Narrative Literature on Breastfeeding Counseling during COVID-19: A South African Case of Primary Healthcare
Abstract
Background
Infant and young child feeding (IYCF) is vital to improve child survival and promote healthy growth and development. However, during the coronavirus-19 (COVID-19) pandemic, access to healthcare facilities or IYCF educational campaigns was limited since the focus was on managing the pandemic. Skin-to-skin contact between mother and child is the core of IYCF guidelines, yet COVID-19 regulations encourage social distancing and separation. The aim of this review was to describe challenges and lessons drawn during the COVID-19 pandemic in the delivery or promotion of IYCF.
Methods
This is a narrative literature review, which does not require seeking any ethical approvals. Publications related to the stated key search items, written in English, were included in this review study. Data was sourced from various sources, such as Scopus/Elsevier, ScienceDirect, and PubMed databases, as well as World Health Organization and United Nations Children's Funds. Search items used included IYCF promotion and services during COVID-19.
Results
A total of 43 publications were included in this review. Findings of the literature showed that there were fears of mother-to-child transmission of COVID-19 and poor feeding practices. The use of IYCF services was also limited.
Conclusion
For future COVID-19 waves and similar pandemics, the social distancing and separation of mother to child should not occur since there is minimal risk of transmission of COVID. Therefore, skin-to-skin contact and overall breastfeeding should be promoted. The IYCF guidelines should be reviewed to focus on personal hygiene practices, such as routine soap use and disinfecting of food preparation areas.
1. INTRODUCTION AND BACKGROUND
Infant and young child feeding (IYCF) is a vital aspect of improving child survival and promoting healthy growth and development [1, 2]. The first two years of a child's life offer a key window of opportunity to ensure survival, growth, and development in order to achieve full potential. This can be done by using the best IYCF practices [3, 4]. The World Health Organization [5] recommends that breastfeeding start within an hour of the baby's birth and be done exclusively for the first six months. Quality and nutritious complementary food should be introduced at six months, with continuation of breastfeeding for at least two years or beyond [6]. About 19% of all under-five mortality can be prevented by feeding babies and young children properly [1, 7]. The world's IYCF practices are subpar [8] and include late breastfeeding initiation, pre-lacteal feeding, early or late introduction of complementary foods, delivering low quality, quantity, and unhygienic complementary food, and bottle feeding [2, 9].
The subpar IYCF practices are associated with factors, such as the mother’s age, illiteracy, unemployment, and a lack of household wealth [10, 11]. The index child's birth order and the hospitals, where babies are delivered, are highly linked to the earliest breastfeeding initiation [12-14]. The practice of a minimum acceptable diet, meal frequency, dietary diversity, and the early introduction of complementary feeding are all linked to maternal education [15, 16]. Prenatal and postnatal visits, maternal age, household wealth status, location, media exposure, and antenatal and postnatal visits are all associated with improved complementary feeding practices [17, 18]. Health educational interventions are purposefully designed activities with the goal of disseminating information to individuals, groups, or communities to improve their life skills and knowledge so they may make better health decisions [19]. It is well-acknowledged that educational interventions can advance public health objectives [20]. They have been used to successfully prevent illnesses and manage medical conditions, as well as to enhance or encourage the adoption of healthy lifestyles, habits, and behaviors [21]. However, during the coronavirus-19 (COVID-19) pandemic, access to healthcare facilities or IYCF educational campaigns was limited since the focus was on managing the pandemic; yet children's health remained important. Infant and young child feeding educational interventions on complementary feeding are regarded as an effective strategy. A review study showed that complementary feeding education reduced the number of caregivers by up to 12% who fed their infants with semi-solid foods before the age of six months [19]. Proper weaning practices include proper timing for initiation of complementary feeding, continuation of breastfeeding after introduction of semisolid foods, hygiene, composition, amount, consistency, and frequency of complementary food, and feeding the infant during or after illness [19, 22]. Health education has improved knowledge, attitude, and behavior, but more women still need to start breastfeeding earlier, give colostrum, practice feeding on demand, and want to continue breastfeeding [23].
Promoting breastfeeding and disseminating information are important tasks for healthcare workers. Primary healthcare facilities still serve as information sources for services that teach parents how to feed their infants and young children. However, during the COVID-19 pandemic, there were regulations, such as lockdowns, social distancing measures, and restrictions on in-person meetings. These COVID-19 laws negatively impacted the delivery of breastfeeding education and support services. The IYCF messages involve breastfeeding and skin-to-skin contact between mother and child [5]. The emphasis on social distancing created fear and anxiety among the general public, including mothers who were still breastfeeding. As a result, breastfeeding problems worsened, considering that proper feeding of infants, such as not exclusively breastfeeding for 6 months and introducing food earlier, was already a problem in developing nations [24].
Existing breastfeeding support groups and sessions had to be discontinued or moved online, which might have made them less accessible to some people, especially those with poor internet access. Especially for those who encountered difficulties or had particular needs, breastfeeding mothers might have faced difficulties due to the lack of specialized help from primary healthcare workers. An Iranian study showed that mothers who belonged to low socioeconomic groups breastfed their infants less than other groups [25]. In South Africa, exclusive breastfeeding is a problem with caregivers providing food to their children earlier than 6 months [26]. These inappropriate feeding practices may increase the chances of malnutrition. The pandemic posed serious challenges in the delivery and/or promotion of IYCF services, resulting in underutilization and bad IYCF practices coupled with fear of not transmitting the pandemic to children. Hence this particular review seeks to describe challenges and lessons drawn during the COVID-19 pandemic in the delivery or promotion of IYCF in preparing for future pandemics and improving practices.
2. MATERIALS AND METHODS
A narrative literature review was conducted for this paper. As a result, conducting this assessment did not require seeking any ethical approvals or authorizations. This narrative literature review involved challenges and lessons from COVID-19 IYCF practices and promotion. This method allowed for the retrieval of existing literature from a variety of sources, and only relevant literature was chosen. In order to avoid selection bias, even literature that contradicted the study was included.
2.1. Database and Searches
The following databases were used to locate literature:
• Biomed, Scopus, Cochrane Library, Web of Sciences, Cumulative Index to Nursing and Allied Health Literature, Embase, Etho Med, Elsevier, Science Direct, PubMed, SciElo, JSTOR and SABINET.
• World Health Organization and United Nations Children’s Funds.
The search engines involved Google Scholar, UL E-Libraries, Chrome, and Google Books.
2.2. Searching of Databases
The search approach involved compiling and summarising current and pertinent literature. The data were searched several times, and duplicates were eliminated. The following key search terms were used:
• Infant and young child feeding during COVID.
• Breastfeeding and COVID-19.
• Complementary feeding and COVID-19.
• Infants and young child feeding services and promotion during COVID-19.
• Dissemination of infant and young child feeding messages during COVID-19.
The screening involved the initial stage, wherein titles and abstracts were reviewed based on eligibility criteria. The follow-up screening was further conducted on included publications for relevance, which were finally recorded. The quality assessment was ensured through the use of an Excel spreadsheet, wherein a customized quality assessment checklist was created, in which data were manually entered. Moreover, the assessment data were recorded in the spreadsheet.
3. RESULTS
A total of 952 publications were identified following the first search using the stated databases. The initial screening process resulted in the elimination of 301 publications for relevance and in accordance with eligibility. The 651 selected publications were further screened, which led to the exclusion of 604 publications, which met the quality assessment for this review. Therefore, a total of 47 publications were cited and referenced in this narrative review.
4. DISCUSSION
The discussion in this review is segmented into sub-headings as follows:
4.1. Infant and Young Child Feeding Services during COVID-19
Breastfeeding practices, which offer several health advantages for both mothers and babies [5], are strongly encouraged and supported through breastfeeding education. Accurate and research-based breastfeeding education became even more important during the epidemic to ensure that parents have the information and abilities to breastfeed successfully. The importance of exclusive breastfeeding for the first six months of a baby's life might be discussed, as well as latch techniques, breastfeeding positions, and overcoming common obstacles [5]. Particularly in difficult situations, this knowledge can empower parents and assist them in making knowledgeable decisions about newborn feeding.
Prior to COVID-19, breastmilk was recognized as the finest type of infant nutrition; therefore, providing appropriate breastfeeding on the first day of life is crucial to the health of the newborn infant and breastfeeding success [27]. The World Health Organization (WHO) [5] further recommends that all infants should start breastfeeding an hour after delivery and solely consume breastmilk for the first six months of their lives. The benefits of these include, among other things, reduced infant mortality and avoiding infections in babies [5]. Additionally, early skin-to-skin contact between the mother and child after birth was advised in the “Ten Steps to Successful Breastfeeding” from the Baby-Friendly Hospital Initiative. Breastfeeding should begin during the first hour of a baby's life. Additionally, it advocated for mothers and infants to live together 24 hours a day, to breastfeed whenever they felt like it, and to avoid giving babies more food or liquids, even water, unless absolutely necessary [28]. The COVID-19 pandemic raised questions and concerns about the transmission of infection from mother to kid.
Few studies on breastfeeding in the context of COVID-19 recommended against skin-to-skin contact, mother-infant separation, and restricted breastfeeding or human milk feeding due to concerns about perinatal and postnatal severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) mother-to-child transmission [29, 30]. However, the American Academy of Pediatrics [31] recommended temporary mother-infant separation and feedings of expressed mother's milk until the woman becomes less contagious to her baby. After the mothers had skin-to-skin contact and breastfed without face masks, a few babies born to COVID-19-positive women later tested positive for SARS-CoV-2 [32-34]. While breastfeeding, it is important to use infection control prevention, including a facemask and hand washing [35]. However, one incident of a newborn getting COVID-19 has been documented while the mother was breastfeeding and wearing a face mask [36]. Ng [35] noted that it is doubtful that SARS-CoV-2 transmission occurs through human milk because only three authors have so far found SARS-CoV-2 in human milk [36-38], while many studies found no SARS-CoV-2 in human milk [30, 39, 40]. During the 2003 SARS outbreak, a mother who contracted SARS-CoV-1 at 19 weeks of gestation was found to contain antibodies against the virus in her milk [35, 41]. The World Health Organization recommends advising the rest of the world on the steps that should be followed and its position on nutrition for infants and young children.
The World Health Organization (WHO) [42] interim guidelines for clinical care of COVID-19 indicate that mothers with suspected or confirmed COVID-19 infection should be encouraged to commence and continue breastfeeding because the advantages outweigh the potential hazards of transmission. These WHO recommendations, which are identical to those for maternal influenza infection, encourage breastfeeding while the mother takes infection control precautions [35, 43]. Furthermore, WHO also agreed to the conclusion that breastfeeding and skin-to-skin contact should start at birth and that mothers with suspected or confirmed COVID-19 should not be separated from their newborns. However, these should be done while taking precautions to avoid spreading the virus to her infant, primarily through contact with the mother's infectious respiratory secretions [35]. According to the WHO's recommendations for Infection Prevention and Control (IPC), mothers with suspected, probable, or confirmed COVID-19 should get guidance from healthcare workers regarding droplet and contact precautions when coming into contact with their child [35]. According to United Nations International Children's Emergency Fund [44], mothers who are quarantined at home and who have COVID-19 that is either suspected or confirmed need to be instructed to use good respiratory hygiene when feeding their infants. Before preparing or eating food, caregivers should make sure they adhere to the recommended hygienic procedures, such as regular cleaning and sanitizing of the areas where food is prepared. In communities where eating at a common bowl or feeding children by hand is common, it is preferable to use the child’s own plate and spoon to avoid transmission [44].
4.2. Counselling Mothers with COVID-19 Infection for Breastfeeding
According to the World Health Organization [45], counselling is a well-focused, time-limited, and targeted practice that uses interaction to help people address their concerns and respond effectively to specific obstacles in order to create new coping mechanisms. This includes supporting, protecting, and encouraging breastfeeding as well as providing appropriate complementary feeding nutrition when it comes to feeding newborns and young children, respectively. In the context of COVID-19, healthcare providers (HCPs) must provide mothers with the guidance, counselling, and breastfeeding education necessary for successful breastfeeding. Despite the fact that lockdowns and restrictions have made it difficult to access physical healthcare facilities for suitable guidance. The HCPs were unprepared for the pandemic and lacked the requisite in-service training on infant and young child feeding in the context of COVID-19. All levels of HCPs engaged in infant care and breastfeeding support should be aware of the foundations of COVID-19 and breastfeeding. They must be educated on the options available to the mother, as well as the advantages and disadvantages of each [35]. The crucial in-service training will assist HCPs in providing greater guidance to the general public.
Counselling can be carried out in person, over the phone, or through a videoconference while wearing personal protection equipment (PPE). The first meeting should ideally occur during antenatal care or before the child's delivery once the mother has been diagnosed with COVID-19 [35]. However, due to the wide range of COVID-19 presentations, HCPs may come into a number of circumstances, such as a woman who is only a carrier of the illness or who has a proven, suspected, or pre-symptomatic infection. There is even a rising argument for systematic screening of obstetric patients admitted for labor despite maternal symptomatology [44]. The HCPs should review the mother's options and provide a suitable visual aid. The five steps of counselling are: 1) establishing a rapport, (2) gathering information, (3) defining the problem, (4) discussing possible solutions, and (5) closing the contact by summarizing the decision-making and possible follow-ups [35].
The mother and HCPs must establish a rapport before the mother may trust them. Recognize that in addition to her regular concerns as a new parent, the woman may additionally be worried and fearful about breastfeeding her infant while infected with the COVID-19 virus [35]. Throughout the information-gathering process, HCPs should be supportive and start with open-ended questions before moving on to specific clarifying questions and specific COVID-19 questions, such as those about exposure history, current health status, the results of swab tests, knowledge of COVID-19 and breastfeeding, and similar history for other household members. HCP may ask the mother about her prior breastfeeding experience and expectations [35]. The problem needs to be defined before a solution can be reached. Both HCPs and the mother should agree on the actual problem.
The HCPs should close the contact by affirming and respecting the mother's decision regarding her infant's feeding. The HCPs should clarify that although existing data points to the safety and health of breastfeeding in COVID-19 for the mother's child, more research may become available in the future. Additionally, HCPs ought to point the mother in the direction of trustworthy informative sources, including the WHO, CDC, and national guidelines [35], or social media platforms, including mainstream media programs and follow-ups.
4.3. Dissemination of Infant and Young Child Feeding Messages
Fig. (1) shows alternative platforms for the distribution of infant and young child feeding messages. They include social media, SMSs, mainstream media, pamphlets distribution, YouTube channels, posting at shops, street meetings observing pandemic regulations, and Zoom platforms.
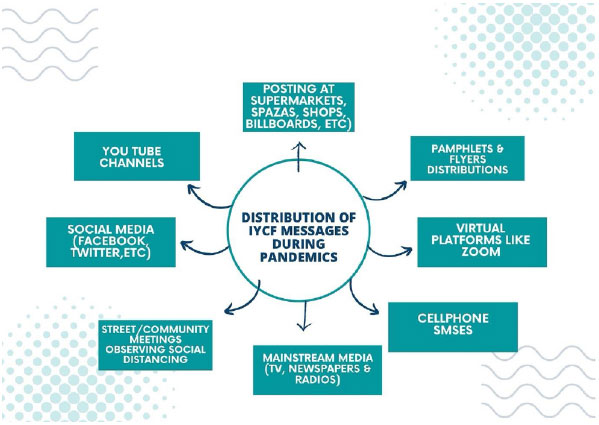
Due to the disruption in routine service delivery at healthcare facilities and community outreach during the lockdown, innovative and practical approaches to inform the public about infant and young child nutrition are required [45]. The provision of individual and group counselling at medical institutions and community platforms was subjected to limitations under COVID-19. Therefore, virtual platforms should be used to disseminate information to families on breastfeeding and complementary feeding behaviours. The education can be provided at important periods, such as when the mother and child are released from the hospital facility or while changing from exclusive BF to timely complementary feeding [46]. Information can be disseminated using a variety of platforms, including mobile technology, social media, traditional media (radio, TV, newspapers), cell phone messages, community announcements, and postings on important stores that are open for business (e.g., supermarkets, food shops). For continued assistance, mothers might also be led to YouTube or other video channels. Message distribution can be redesigned based on the context; other means, for example, in a population where the use of social media can be a challenge due to limited internet access, different methods can be utilised.
Virtual platforms have made breastfeeding education and support services more widely accessible and reachable, allowing people from various geographical places to use them. It might not, however, completely match the individualized services offered in in-person interactions [47]. Some tasks, like watching a breastfeeding session or performing a physical assessment, could be difficult to do virtually. Therefore, it is crucial to regularly assess the efficiency of online resources for breastfeeding education and look into cutting-edge tactics to increase their efficiency [47].
CONCLUSION
The COVID-19 laws have an impact on breastfeeding support and education. For future COVID-19 waves and similar pandemics, the social distancing and separation of mother to child should occur since there is minimal risk of transmission of COVID-19; therefore, skin-to-skin contact and overall breastfeeding should be promoted. Hygiene precautions are critical and must be observed both during and after a pandemic. It is recommended that IYCF guidelines be reviewed in order to focus more on personal hygiene practices, such as routine soap use and disinfecting of food preparation areas. Healthcare providers should continue to receive training on new or updated recommendations for feeding infants and young children for the best possible implementation. In case of future epidemics involving lockdown and movement limitations, it is necessary to use a range of cutting-edge programs, such as social media and focused programs on mainstream media, for accurate information on infant and young child feeding. Similarly, efforts should be made to promote these messages to marginalized communities. Even once the restrictions are lifted, these strategies could be used to improve or augment the fight against child malnutrition.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


