REVIEW ARTICLE
Systematic Review on Public Health Problems and Barriers for Sex Workers
Leshata Winter Mokhwelepa1, Mxolisi Welcome Ngwenya1, Gsakani Olivia Sumbane1, *
Article Information
Identifiers and Pagination:
Year: 2024Volume: 17
E-location ID: e18749445264436
Publisher ID: e18749445264436
DOI: 10.2174/0118749445264436231119172400
Article History:
Received Date: 18/07/2023Revision Received Date: 17/09/2023
Acceptance Date: 03/10/2023
Electronic publication date: 02/04/2024
Collection year: 2024

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background
The phenomenon of healthcare and social struggles among sex workers in communities of South Africa is a critical concern. Sex workers are often stigmatised, discriminated against, and violated. This study stems from the observation that sex workers experience daily healthcare and social challenges due to their line of work. This involves prejudice and stigma from the general public and medical professionals. Despite government efforts to raise the calibre of healthcare services, some healthcare systems remain problematic.
Objective
The study intended to critically review the publications on public health problems and barriers faced by sex workers.
Methodology
The systematic review methodology was used in the investigation. Identification of the problem, literature search, data evaluation, data analysis, and presentation were the five stages of the systematic review that were carried out. The following electronic databases were used to conduct a thorough search of the literature from 2013 to 2022: CINAHL, Medline, PubMed, JStore, and Embase. The search phrases included “sex workers,” “health problems,” “barriers,” “experiences,” “challenges,” “Mental Health,” and “systematic review”. Studies that were published prior to 2013 did not focus on the challenges, barriers, and social and health problems of sex workers and were not reported in English were excluded. Following the critical review evaluation, 30 studies were selected for this study out of a total of 85 studies. The categories were constructed using Creswell's Tesch method of data analysis.
Results
The analysis yielded two themes and seven subthemes: (1) public social problems that sex workers must navigate, including violence, criminalisation of sex work, stigma, prejudice, and linguistic and cultural hurdles, (2) high rates of HIV and STIs, a lack of comprehensive knowledge of reproductive and health issues, problems with mental health, and challenging access to care are some examples of the complexity of public healthcare.
Conclusion
A multipronged approach, including legal reform, destigmatisation, and increased access to healthcare and social support services, is required to address the healthcare and social struggles of sex workers.
1. INTRODUCTION
Sex workers are considered to be disease carriers and reservoirs, which restricts their ability to get medical care [1]. The physical and mental health of sex workers is at risk due to numerous interrelated causes [2]. Treatments focusing on a single risk factor are less likely to address complex health inequities caused by stigma, human rights violations, violence exposure, unwanted births, HIV, and other STIs [3]. The health outcomes of sex workers are influenced by personal, social, communal, and governmental factors [4]. One illustration of these problems at several levels is the increased risk of HIV and other STIs among sex worker clients who refuse to wear condoms [5]. The participation of sex workers in healthcare is hampered by stigma and prejudice from healthcare professionals, and physical and sexual abuse is also prevalent [6].
In low-income sub-Saharan countries like Zimbabwe, sex workers had higher rates of HIV infection compared to all women of reproductive age [7]. This conclusion is supported by a study by Maphosa that found that the prevalence of HIV and STI among sex workers in the specific area is more than twenty times higher than the prevalence of HIV in the general population [8]. Accessing HIV and AIDS services can be challenging for sex workers in Zimbabwe, according to reports. Receiving accurate, suitable, and pertinent therapy is significantly hampered by the challenges of admitting sexual orientation [9]. In Zimbabwe, various barriers prevent sex workers from receiving sexual healthcare, such as challenges in finding care. The criminal code in Zimbabwe, which classifies sex work as a crime, restricts sexually active people from sharing information about their jobs and medical requirements to receive treatments like Pap testing and breast cancer screenings [10]. In a single overnight raid with the code “Operation Zvanyanya,” the police captured fifty-three women, which was a high number, according to a report written by Zimbabwean lawyers for human rights. While the women were in police custody, they were denied sanitary pads and attacked with baton sticks by the police [11]. Additionally, condoms are used to prove sex workers' involvement in sex work if they carry them [12].
Previous studies have suggested that women in the sex industry may be more susceptible to mental illnesses, particularly mood disorders, suicidal ideation, and post-traumatic stress disorder [13]. Some Chinese studies suggest that factors at the partner and individual levels, such as age, self-stigma, and sexual coercion, may be associated with less favourable research findings in mental health. On the other hand, research from New York, Australia, Mexico, and other US cities shows links between prior trauma and anxiety, melancholy, and post-traumatic stress disorder symptoms [14]. According to themes of qualitative research conducted in Vancouver and looking at the experiences of transgender sex workers, transgender sex workers experience severe health and social injustices, including trauma and violence, which are connected to socio-structural factors like transphobia, criminalisation, and stigma [15].
Sex workers experience stigmatisation, criminalisation, abuse, and other societal injustices. Every person has the right to be treated fairly by the law and free from torture and cruel treatment. The person's selling of sex has no bearing on these rights. On a worldwide basis, sex workers nonetheless continue to experience disproportionately high rates of violence and other human rights violations. Between 45 and 75% of women encounter physical, sexual, or both sorts of abuse at work throughout their lifetimes, according to a comprehensive study from 2014 [16]. Many times, during discussions about the use of condoms, sex workers are subjected to physical and sexual abuse by clients and predators posing as clients [17]. The rights of sex workers are violated, and their chance of getting HIV and other STDs is increased [16]. Thus, to manage and control sex workers, their intimate partners also use violence against them [5], including threatening to report them to the police. A Lancet investigation found that the places where some aspects of sex work are illegal are also the places where sex workers' rights are most frequently violated [5]. The prevalence of underreporting and infrequent criminalisation of violence against sex workers is high [16]. In some cases, it is done by the police, exacerbating trauma and making it much more difficult for sex workers to receive justice and medical attention. The leading causes of violence against sex workers are criminalisation, contemporary stigma, discrimination, and social marginalisation [4]. These structural problems impact health outcomes and access, increasing physical and mental health risks. Due to the criminalisation of sex work, police can harass and threaten sex workers, extort money through fines or other means, seize their condoms, assault them, and use the prospect of arrest to force them into performing sexual acts. Numerous scenarios have documented each of these misuse [18, 19]. Sex workers claim that such harsh police techniques are a stand-in for enforcing sex laws worldwide.
Sex workers frequently experience stigma and prejudice, which harms their health, safety, and well-being [20]. Due to social perceptions that consider sex work as immoral, illegal, or fundamentally exploitative, it is frequently stigmatised. The stigma associated with this condition can result in discrimination, such as denial of fundamental rights and services, social marginalisation, harassment, and violence [20]. Due to stigma and prejudice, sex workers may encounter considerable obstacles when getting health treatments, such as HIV testing and treatment. This could result in higher HIV transmission rates [21]. Additionally, out of concern for discrimination, sex workers could be hesitant to seek medical attention, which results in treated health issues. As a result, this review aims to examine and analyse the complicated issues that sex workers face in their personal and professional lives. This study revealed three gaps: a lack of social support, legal protection, and inadequate access to healthcare. By investigating the legal frameworks that exist in various nations and analysing the effects of criminalisation on sex workers, as well as by identifying barriers to sex workers' access to healthcare services and developing recommendations to improve access to healthcare services, including sexual and reproductive health services, as well as by examining the social stigma and isolation faced by sex workers and developing strategies to reduce stigma and increase social support, the study will address these gaps.
2. LITERATURE REVIEW METHODOLOGY
The literature review is a comprehensive study and interpretation of literature that addresses a specific topic [22]. The literature review aims to cultivate a robust knowledge base to conduct research studies [23]. A systematic review approach was adopted to synthesize evidence on the complexities of the life of sex workers in terms of health care and social context [24]. This systematic review protocol followed the steps, namely: (i) the research question formulation, where the general purpose and review questions are explicitly stated; (ii) the literature search, which uses a thorough and repeatable search strategy to collect data; (iii) quality assessment, where the methodological quality and relevance of selected literature are appraised; (iv) data extraction and analysis, which includes data abstraction, comparison, and synthesis; and (v) the presentation of results, where the interpretation of the findings is presented.
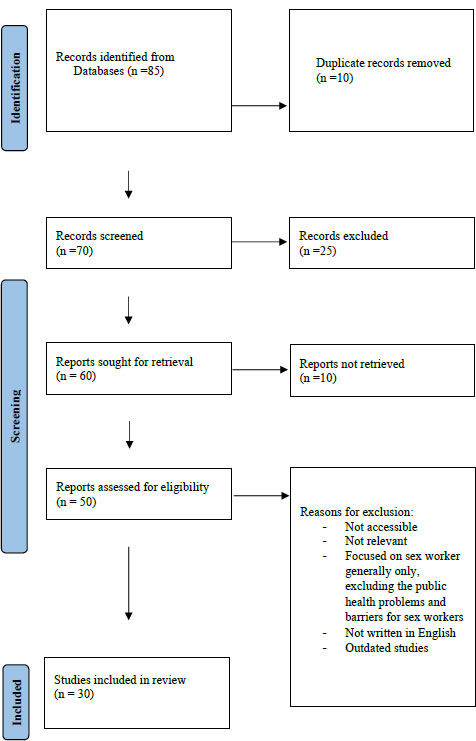 |
Fig. (1). Prisma flow diagram describing the systematic review process. |
2.1. Research Question Formulation
The focus topic, purpose, and research questions for the review are defined during the problem identification phase [25, 26]. This in-depth analysis sought to educate readers on the difficulties faced by sex workers in the medical and social fields. The research issue in this study stems from the observation that sex workers experience daily healthcare and social challenges due to their line of work. This involves prejudice and stigma from the general public and medical professionals. Despite government efforts to raise the calibre of healthcare services, some healthcare systems remain problematic [27]. Sex workers become reluctant to go to clinics for full body screening and testing of infectious diseases, and their chances of receiving health education are inhibited. Furthermore, the authors have observed that such behavior of judging sex workers by most healthcare workers persists in healthcare institutions and leaves them more vulnerable to mental illness. Therefore, this review seeks to explore and describe the public health problems and barriers faced by sex workers. In addition, it further develops guidelines to address the health care and social struggles faced by sex workers. This systematic review analyses current research on what is currently known about sex workers’ healthcare and social challenges and finds areas of the literature that still require research.
The review question, therefore, is as follows:
2) What are the public health problems and barriers for sex workers?
2.2. Literature Search
The healthcare of sex workers and social battles in South African communities are the main topics of this review, which included all peer-reviewed publications that had been published. The initial search was conducted using electronic databases, such as CINAHL, MEDLINE, PubMed, JSTORE, and Embase, and then the search terms discovered in the article titles and abstracts were analysed. Second, articles in all the chosen databases were searched using the indicated keywords and index terms. The final search strategy included the keywords “health problems,” “health care concerns,” “sex workers,” “social challenges,” sex workers,” “health problems,” “barriers in sex workers,” ” sex workers experiences,” ” sex workers challenges,” “mental health of sex workers” and “systematic review”.’ Studies were considered if they were published in English between 2013 and 2022. From the initial search, eighty-five articles were chosen as samples. The authors independently examined the studies to examine if they satisfied the inclusion requirements. The study comprises publications that address the challenges, experiences, perceptions, barriers, and social and health problems of sex workers, as well as those that focus on the systematic review methodology and published in English between 2013 and 2022. After removing duplicates and checking titles and abstracts, fifty studies that might be pertinent were discovered. After full-text reads, twenty papers were eliminated, primarily because they contained duplicates. The final sample for this systematic analysis consisted of thirty papers. The explanatory flow chart in Fig. (1) illustrates the entire screening process.
2.3. Quality Assessment
Primary sources were rigorously assessed for quality at the data review stage, utilising methods for evaluating quality criteria [26]. The reviewers and authors undertook a critical analysis. Both theoretical and empirical reports made up the final thirty papers. Authors, publication year, design, and method were tabulated for each paper. Using a three-point scale with the options of high, low, or not reported from Moagi, Van Der Wath, Jiyane, and Rikhotso, the authors used a modified set of six criteria [28] and on the scale, the authors quantified high as 2 points, low as 1 point, and no report was quantified as 0 points. A sum of quality between 0-4 was regarded as poor, 5-8 as fair, and 9-12 as good. Moreover, the study was comprised of 56,7% of good quality studies and 43,3% of fair quality studies for quality appraisal of the studies. Assessing the goals and objectives, study design, research techniques, theoretical framework, constraints, and implications were significant aspects of the six criteria for methodological rigour. Most of the articles reviewed in this study were of good quality. Table 1 shows the evaluation of the publications. To minimise the risk of bias, the authors independently evaluated the selected studies and a meeting was set to reach a consensus on the emerging themes.
| Author(s) | Year | Title | Study Design | Research Methods | Population (n) | Quality Appraisal | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Objectives | Study Design | Research Methods | Theoretical Framework | Limitations | Implications | Sum of Quality | ||||||
| Slabbert, M., Venter, F., Gay, C., Roelofsen, C., Lalla-Edward, S., and Rees, H. | 2017 | Sexual and reproductive health outcomes among female sex workers in Johannesburg and Pretoria, South Africa: Recommendations for public health programs | Retrospective analysis | Quantitative study | (n = 1830 | 2 | 2 | 2 | 0 | 2 | 2 | 10 |
| Puri N, Shannon K, Nguyen P, Goldenberg SM | 2017 | Burden and correlates of mental health diagnoses among sex workers in an urban setting. | Open, prospective design | Quantitative study | n=692 | 2 | 2 | 2 | 0 | 2 | 2 | 10 |
| Beattie, T. S., Smilenova, B., Krishnaratne, S. and Mazzuca, A. | 2020 | Mental health problems among female sex workers in 1 and middle-income countries: A systematic review. | Systematic review and meta-analysis | Systematic review | n= 1046 | 2 | 0 | 2 | 0 | 2 | 2 | 8 |
| Sou, J., Shannon, K., Li, J., Nguyen, P., Strathdee, S., Shoveller, J. and Goldenberg, S.M. | 2015 | Longitudinal research findings in an urban Canadian setting on the structural causes of migrant sex workers' inconsistent usage of condoms with customers. Diseases Caused by Sexual Contact. | Experimental research design | Longitudinal quantitative research | n= 685 | 2 | 2 | 2 | 0 | 2 | 2 | 10 |
| Benoit, C., McCarthy, B. and Jasson, M. |
2015 | Stigma, sex work, and substance use: A comparative analysis. Sociology of Health and Illness. | Cross-sectional, experimental and descriptive | Comparative analysis | n= 58 | 2 | 2 | 2 | 0 | 2 | 2 | 10 |
| Deering, KN, Amin, A., Shoveller, J., Nesbitt, A., Garcia-Moreno, C., Duff, P., Argento, E. and Shannon. | 2014 | A thorough analysis of the factors associated with violence against sex workers. | Experimental | Qualitative | n= 28 | 2 | 2 | 2 | 0 | 2 | 2 | 10 |
| Schwartz, SR, Rao, A., Rucinski, KB, Lyons, C., Viswasam, N., Comins, CA, Olawore, O. and Baral, S. | 2019 | HIV-related implementation research: designing for individuals, comparing populations, and considering the context. Acquired immune deficiency syndromes journal. | Descriptive and experimental | Mixed method approach |
1015 | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Aborisade, R.A. | 2019 | Evidence of mistreatment of sex workers by Nigerian police from a qualitative investigation. pp. 405–419 in Police Practice and Research. | Experimental | Qualitative | n= 56 | 2 | 2 | 2 | 0 | 2 | 2 | 10 |
| Shannon, K., Crago, A.L., Baral, SD, Bekker, L.G., Kerrigan, D., Decker, M.R., Poteat, T., Wirtz, A.L., Weir, B., Boily, M.C. and Butler, J. | 2018 | The global reaction to HIV and the unfulfilled obligations for sex workers. | Systemic review and meta-analysis | Quantitative approach | 747 | 2 | 2 | 2 | 0 | 0 | 2 | 8 |
| Shannon, K., Strathdee, SA, Goldenberg, S.M., Duff, P., Mwangi, P., Rusakova, M., Reza-Paul, S., Lau, J., Deering, K., Pickles, M.R. and Boily, M.C. | 2015 | Influence of structural factors on the global epidemiology of HIV among women who work in the sex industry. | Systematic review | Systematic review | n=87 | 2 | 2 | 2 | 0 | 0 | 2 | 8 |
| Decker, M.R., Crago, A.L., Chu, S.K., Sherman, S.G., Seshu, M.S., Buthelezi, K., Dhaliwal, M. and Beyrer, C. | 2015 | HIV burden and impact of human rights violations against sex workers. | Cross-sectional, cohort, experimental | Systematic study. | n=800 | 2 | 2 | 2 | 2 | 0 | 2 | 10 |
| Deering, K.N., Bhattacharjee, P., Mohan, H.L., Bradley, J., Shannon, K., Boily, MCC, Ramesh, B.M., Isac, S., Moses, S. and Blanchard, J., 2013. | 2013 | Southern India's female sex workers are at risk of violence and HIV illnesses caused by sexual contact. | Cross-sectional | Quantitative | n=1219 | 2 | 2 | 2 | 0 | 0 | 2 | 8 |
| Evens, E., Lanham, M., Santi, K., Cooke, J., Ridgeway, K., Morales, G., Parker, C., Brennan, C., de Bruin, M., Desrosiers, PC, and Diaz, X. | 2019 | The experiences of gender-based violence experienced by transgender women, men who have sex with men, and female sex workers in Latin America and the Caribbean were investigated in a qualitative study to guide HIV programming. | Experimental | Qualitative | n=278 | 2 | 2 | 2 | 0 | 0 | 2 | 8 |
| Footer, KH, Silberzahn, BF, Tormohlen, KN, and Sherman, SGS. | 2016 | An empirical examination of policing actions as a structural predictor of HIV among sex workers. | Empirical research design | Qualitative | n=137 | 2 | 2 | 2 | 0 | 2 | 2 | 10 |
| Gu, J., Lau, JT, Li, M., Li, H., Gao, Q., Feng, X., Bai, Y., Hao, C., and Hao, Y. | 2014 | The experiences of gender-based violence experienced by transgender women, men who have sex with men, and female sex workers in Latin America and the Caribbean were investigated in a qualitative study to guide HIV programming. | Analytical research | Qualitative study | n=200 | 2 | 2 | 2 | 0 | 0 | 0 | 6 |
| Lyons, T., Krüsi, A., Pierre, L., Kerr, T., Small, W. and Shannon, K. | 2017 | The experiences of trans sex workers in Vancouver, Canada, are being discussed as we negotiate assault in the context of transphobia and criminalisation. | Empirical analysis | Qualitative study | n=33 | 2 | 2 | 2 | 0 | 2 | 2 | 10 |
| MacLean, S.A., Lancaster, K.E., Lungu, T., Mmodzi, P., Hosseinipour, M.C., Pence, BW, Gaynes, BN, Hoffman, IF, and Miller, W.C. | 2018 | Prevalence and correlates of probable depression and posttraumatic stress disorder among female sex workers in Lilongwe, Malawi. | Cross-sectional | Quantitative | n=200 | 2 | 2 | 2 | 0 | 0 | 2 | 8 |
| Platt L, Grenfell P, Meiksin R, Elmes J, Sherman SG, Sanders T, Mwangi P, Crago AL. | 2018 | A thorough review and meta-analysis of quantitative and qualitative studies on the relationships between sex work laws and the health of sex workers. | Empirical, cross-sectional, experimental | Mixed method research | n=134 | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Smith, A., Tulk, D., Snook, K., Ropson, M., and Giwa, S. | 2020 | Female sex workers’ perceptions of the ability of front-line police officers to ensure their safety in St. John's, Newfoundland, Greenwich social work review. | Experimental | Qualitative | n=4 | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Treloar, C., Stardust, Z., Cama, E. and Kim, J. | 2021 | Rethinking the connection between sex work, stigma, and mental health: an Australian study on sex workers. | Observational research design | Systematic study | n=31 | 2 | 2 | 2 | 0 | 0 | 0 | 6 |
| Davis, S.L., Goedel, W.C., Emerson, J. and Guven, B.S. | 2017 | Punitive laws, critical population size estimates, and global AIDS response progress reports. | Experimental, cross-sectional | Qualitative and quantitative | n=154 | 2 | 2 | 2 | 0 | 0 | 0 | 6 |
| Fitzgerald-Husek A, Van Wert MJ, Ewing WF, Grosso AL, Holland CE, Katterl R, Rosman L, Agarwal A, Baral SD. | 2017 | Measuring the stigma that affects both guys who have sex with men and sex workers (MSM). | Experimental | Systematic review | n=541 | 2 | 2 | 2 | 0 | 2 | 0 | 8 |
| Alemayehu, M., Yohannes, G., Damte, A., Fantahun, A., Gebrekirstos, K., Tsegay, R., Goldberger, A. and Yebyo, H. | 2015 | Prevalence and predictors of sexual violence among commercial sex workers in Northern Ethiopia. Reproductive health. | Cross-sectional | Quantitative study | n=250 | 2 | 2 | 2 | 0 | 0 | 0 | 6 |
| Maseko, S. | 2013 | Sex on Trial: Zimbabwe's criminalisation and moralisation of sexuality. A Journal on African Women's Experiences. | Experimental | Qualitative | n=12 | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Moher D. | 2021 | Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. | Cross-sectional | Systematic review and meta-analysis | n=110 | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Kallio H, Pietilä AM, Johnson M, Kangasniemi M. | 2016 | Systematic methodological review: Developing a framework for a qualitative semi‐structured interview guide. Journal of advanced nursing. | Systematic methodological review | Qualitative analysis | n=2703 | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Beattie TS, Smilenova B, Krishnaratne S, Mazzuca A. | 2020 | Mental health problems among female sex workers in 1ow- and middle-income countries | Cross-sectional | Systematic Review and meta-analysis | n=1046 | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Evens E, Lanham M, Santi K, Cooke J, Ridgeway K, Morales G, Parker C, Brennan C, de Bruin M, Desrosiers PC, Diaz X. | 2019 | Experiences of gender-based violence among female sex workers, men who have sex with men, and transgender women in Latin America and the Caribbean. | Structured-experimental | Qualitative study | n=278 | 2 | 2 | 2 | 0 | 2 | 0 | 8 |
| Porter CM. | 2016 | Revisiting Precede–Proceed: A leading model for ecological and ethical health promotion. | Experimental | Qualitative | n=1000 | 2 | 2 | 2 | 0 | 2 | 0 | 8 |
| Saulle R, Sinopoli A, Baer AD, Mannocci A, Marino M, De Belvis AG, Federici A, La Torre G. | 2020 | Saulle R, Sinopoli A, Baer AD, Mannocci A, Marino M, De Belvis AG, Federici A, La Torre G. | Systematic analysis | Qualitative study | n=27 | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
2.4. Data Extraction and Analysis
During the data analysis, information from primary sources was organised, categorised, and summarised to create an integrated conclusion regarding the study subject being examined [25]. A self-developed data extraction sheet was used to extract the relevant data. It detailed the population being examined, the sex workers contributing variables, the healthcare and social struggles faced by sex workers, as well as the study methodology. The data was then organised and classified utilising a constant comparative method to intergrade and analyse the results. The categories were constructed following Creswell's [29] Tesch method of data analysis:
• A team of three authors familiarized themselves with the literature by going through each article repeatedly to check the accuracy of the literature, which created an opportunity to internalize the data of each article.
• As literature was being read repeatedly, the researchers wrote down a list of some ideas or topics discovered as they went through the literature, also relating the phenomena in columns together with supporting statements.
• The listed topics were then compared with the literature. These topics were then abbreviated for coding. Finally, the researchers revisited the literature and wrote the codes next to the relevant topics in the margin.
• Topics that have a similar meaning were grouped. These help in further categorisation. Then, all statements that addressed each category were put together. Finally, further data reduction was made by grouping categories related to one another.
• The researchers reached a final decision on the abbreviation for each category, called themes. Table 2 below illustrates the categories.
2.5. Presentation of Results
The final stage of the systematic review process was data presentation. To support their findings, the authors provided particular details from each source. From the search's sixty relevant pieces of literature yielded, a sample of thirty (30) articles for the study was chosen and then examined for eligibility. To evaluate the study's quality, 56,7% of the studies were of good quality, and 43,3% were of fair quality. A thorough review of what is known regarding the health and social problems of sex workers was carried out using the data of each study. After a comprehensive study, two main themes and their seven subthemes emerged from the review.
Table 2. Representing the themes and subthemes of the review.
| Themes | Sub-themes |
|---|---|
| 1. Public social problems encountered by sex workers | 1.1. Violence 1.2. Criminalisation 1.3. Stigma and discrimination 1.4. Language and cultural barriers |
| 2. Public health problems encountered by sex workers | 2.1. Elevated risk of HIV and STIs due to inconsistent condom use. 2.2. Lack of comprehensive reproductive health education and information and poor access to healthcare. 2.3. Mental problems resulting from sex work. |
3. RESULTS
Table 2 below illustrates the categories constructed in this study. The categories consist of two themes and seven subthemes. In the evaluated research, the population consisted of many women who are sex workers facing health care and social problems.
3.1. Theme 1: Public Social Problems Encountered by Sex Workers
Daily social challenges exist for sex workers in their line of employment. They encounter societal violence, stigma, discrimination, and criminalisation. Many people have negative attitudes toward sex work and individuals who engage in it since it is seen as immoral or deviant. Repercussions include social marginalisation, stigmatisation, housing discrimination, and employment discrimination. The following factors contributing to social struggles will be discussed as subthemes:
3.1.1. Subtheme 1.1: Violence
Sex workers are at increased risk of violence, including physical assault, rape, and arrest and incarceration, with underreporting and lack of prosecution contributing to a sense of vulnerability and helplessness among sex workers [30, 31, 16]. Similarly, sex workers face a significant risk of violence from clients and the broader community due to the stigmatisation of sex work and the criminalisation of many aspects of the industry [32]. This violence can take many forms, including physical and sexual assault, verbal harassment, extortion, and trafficking, and sex workers may be reluctant to report crimes to the police due to fear of arrest [33]. Sometimes, police officers can also perpetrate physical abuse, particularly in countries where sex work is illegal. These acts of violence can cause severe injuries, leading to long-term physical and mental health problems [34]. Sexual violence is also a significant risk for street sex workers. Clients can force them to perform sexual acts against their will or without using protection, putting them at risk for sexually transmitted infections [35]. Pimps or other individuals may also subject street sex workers to rape or sexual assault [5]. Many sex workers are also vulnerable to human trafficking and forced prostitution, particularly heinous sexual violence. Extreme sexual violence against male, female, and transgender sex workers has been observed, particularly during arrest and custody, and includes gang rape and forced unprotected intercourse [36]. Sixty percent of Adama, Ethiopia, sex workers reported experiencing workplace violence [37]. It was 79% in Mombasa, Kenya, compared to 16% in Hunan, China, and 9% in Karnataka, India, where female sex workers reported work-related violence [38]. This shows how most sex workers experience abuse at work. Pimps, police officers, and people who purchase sex from sex workers are some of the people who commit violent crimes.
3.1.2. Subtheme 1.2: Criminalisation of Sexual Work
Criminalisation is the process by which behaviours and individuals are transformed into crimes and criminals [39]. Criminalisation is a significant barrier to healthcare for sex workers. In many countries, sex work is illegal, which means that sex workers may be afraid to seek medical care for fear of being arrested or prosecuted [40]. This fear can lead to a lack of trust in healthcare providers and a reluctance to disclose sensitive information. Furthermore, criminalisation may make it more challenging for sex workers to obtain medical care, including HIV testing and treatment [41].
Laws that make sex work illegal can make it harder for young people to manage the terms under which sex is sold and deter them from using services out of concern that they would be detained, arrested, or prosecuted [42]. These laws are frequently enforced punitively through the seizure of identity documents and citizenship rights, mandatory or coerced HIV testing, condoms being seized, which are used as evidence of solicitation, and the lack of protection from the workforce [43]. In Kenya, police use the possession of condoms as evidence of sex work, leading to the arrest of the individual and the confiscation of their condoms [5]. In Zimbabwe, a group of sex workers said that their interactions with the police were complex and that they had taken their condoms away, placing them in danger as they tried to make a living [44]. According to a 2013 investigation, approximately 15000 sex workers were housed in facilities dubbed “custody and education centres” [8].
Similarly, a new law in Cambodia that is supposed to combat sex workers has suffered because of sexual exploitation and human trafficking [43]. Police have utilised the law to shut down brothels, moving sex workers to unregulated nightclubs and public places [44]. The ability of female sex workers to negotiate condom use had decreased due to their displacement, which also exposed them to more violence and restricted their access to assistance [45].
3.1.3. Subtheme 1.3: Stigma and Discrimination
The sociologist Erving Goffman defined stigma as a social trait or mark that separates individuals based on socially generated opinions [46]. Stigmas severely diminish the bearer, turning them from a whole and well-liked person to a flawed and dismissed one [46]. Due to shame, this frequently leads to social marginalisation and solitude. Benoit et al. contended that in the case of sex workers, the outcome is frequently a refusal to use health services since the identity of the sex workers is elevated to a significant status. When sex workers seek medical care, attitudes and animosity are frequently present because even healthcare professionals and medical facilities worry about being stigmatised by association [46]. As a result, other residents’ social rights are sometimes denied to sex workers [47]. According to Benoit [7], prejudice is the root cause of structural inequality in society, increasing vulnerability and, to some extent, the weight of avoidable health issues for marginalised groups. Society often views sex work as immoral, illegal, or dirty [47]. This stigma may result in a lack of trust between sex workers and medical professionals. Many sex workers fear judgment, discrimination, or even violence when accessing healthcare [42]. As a result, they may avoid seeking care altogether, even when they need it. Sex work is stigmatised and associated with immorality, leading to discrimination and social isolation and creating a hostile healthcare environment [48].
3.1.4. Subtheme 1.4: Language and Cultural Barriers
Sex workers may also face language and cultural barriers when accessing healthcare. Many sex workers who do not speak the language of the country in which they work may face a severe challenge, making it difficult for them to communicate with healthcare providers [41]. Language barriers can prevent sex workers from fully understanding their health status and treatment options, while cultural differences can lead to misunderstandings or inappropriate treatment [49]. For sex workers, cultural norms can pose considerable obstacles, especially in societies where sex is taboo. This can make it difficult for sex workers to communicate with clients, negotiate their rates, or form positive relationships with non-sex workers [16].
3.3. Theme 2: Public Health Problems Encountered by Sex Workers
Accessing healthcare treatments can be challenging for sex workers because of discrimination on the part of healthcare professionals, a lack of insurance, and a shortage of knowledgeable, understanding doctors. A marginalised minority, sex workers have a difficult time getting access to healthcare. The difficulty in getting healthcare for sex workers results from stigma, discrimination, criminalisation, and lack of resources [49]. These problems could have a severe impact on their physical and mental well-being.
3.3.1. Subtheme 2.1: Elevated Risk of HIV and STIs due to Inconsistent Condom Use
Female sex workers are more likely to contract HIV because of factors like limited condom availability in some settings, the potential for violence, the likelihood that condoms will be confiscated and used as evidence of unlawful conduct, the absence of labour rights and customers who would not use condoms, the high prevalence of HIV infection in the region, and the probability of violence [4]. Therefore, the capacity to negotiate condom use can be reduced using drugs and alcohol, and HIV and hepatitis B and C can be spread using shared injecting equipment [4]. Studies by Shannon et al. have also shown that the prevalence of HIV among sex workers is higher than that of the general population [4]. This is due to a combination of factors, including inconsistent condom use, multiple sexual partners, drug and alcohol use, and exposure to violence [4]. However, a recent assessment indicated considerable regional differences in the pooled prevalence of HIV among women who sold sex, ranging from 6.1% in Latin America to 10.9% in Eastern Europe and 36.9% in sub-Saharan Africa [50]. Few studies have been conducted on other STIs, such as chlamydia and gonorrhoea, but many have examined the prevalence of HIV and syphilis infection among female sex workers [51, 52]. These infections can cause serious long-term health difficulties like pelvic inflammatory disease, ectopic pregnancy, and reproductive problems, raising the risk of HIV transmission. Additionally, compared to older women, younger women who sold sex had considerably higher incidences of gonorrhoea and chlamydia, according to a Chinese study by Chen, Yin, Liang, Wang, Jiang, Liu, and Wang [53].
3.3.2. Subtheme 2.2: Lack of Comprehensive Sexual and Reproductive Health Education, Information, and Poor Access to Healthcare Services
Comprehensive sexual and reproductive health education is essential for sex workers, as it can help them make informed decisions about their sexual health and well-being. However, many sex workers do not receive this education due to various factors, such as social stigma, lack of resources, and limited access to information. Sex workers' health and well-being may be adversely affected by the lack of thorough sexual and health education and services. Without access to health education and services, sex workers can engage in risky sexual behaviours, such as unprotected sex, increasing their risk of contracting STIs and unprotected pregnancies. Therefore, this, in turn, can lead to long-term health complications. A study by Zhang, Temmerman, Li, Luo, and Luchters reported that young people in schools are made vulnerable to HIV if health education on sexuality, sexual behaviour, and risk management, including using condoms and negotiating techniques, is not provided by instructors. In addition, three-quarters of the women selling sex between the ages of 15 and 19 who were questioned said they needed more health information [54].
Socas, Shoveller, Bean, Nguyen, Montaner and Shannon reported that most of the struggles discussed above, such as stigmatisation and criminalisation, contribute to poor access to healthcare services by sex workers [55]. Negative attitudes of healthcare workers can make it difficult for sex workers to seek health, get tested, and be treated for STIs and HIV [56]. This could lead to a high prevalence of AIDS and other STIs, such as chlamydia, gonorrhoea, and syphilis, as they may be hesitant to seek care due to fear of discrimination [16]. Furthermore, many sex workers work in paying jobs without benefits or insurance, making it difficult to afford healthcare. They may also face discrimination when obtaining health insurance or financial assistance [4]. Additionally, sex workers can pay for their healthcare out of pocket, which can be prohibitively expensive.
3.3.3. Subtheme 2.3: Mental Health Problems Resulting from Sex Work
The outcomes of mental health problems among sex workers have been reported in several studies. These outcomes were related to alcohol and drug use, stress, and risk-related work in the sex industry [57]. Most sex workers use drugs and alcohol as a coping mechanism. This causes sex workers to experience more stress as they fear being detained by authorities. On the other hand, sex workers are more likely to be kidnapped and have a greater probability of being raped by their clients, making them more depressed. Depression is a common mental health challenge facing sex workers [58]. The stigma and discrimination associated with their work can cause hopelessness and despair. Lack of social support and isolation can also contribute to depression. Sex workers who experience depression may have difficulty finding motivation to work or may struggle to maintain relationships with clients or others in their personal lives [59]. Anxiety is another common mental health challenge faced by sex workers. Sex workers may experience anxiety about their safety, health, and financial stability [60]. Fear of arrest, violence, or discrimination can also contribute to anxiety. Sex workers who experience anxiety can feel on edge or constantly concerned, making it difficult to focus on their work and leading to avoidance behaviours [59]. Posttraumatic stress disorder is a mental health condition that can develop after exposure to a stressful event. Sex workers are at greater risk of experiencing traumatic events, such as physical or sexual assault, police brutality, or other forms of violence. PTSD can result in nightmares, flashbacks, avoidance behaviours, and hyperarousal, which can interfere with the ability of sex workers to function and perform their work [60]. Suicidal ideation is a severe mental health challenge that sex workers may face. The stigma and discrimination associated with their work and the lack of access to mental health care and support services can exacerbate feelings of hopelessness and despair. Sex workers who experience suicidal ideation may be at risk of self-harm or suicide, which can devastate their personal and professional lives [60].
4. DISCUSSION
In a health and social setting, the study sought to analyse and examine the complicated lives of sex workers critically. This study found that sex workers typically struggle with significant health concerns due to several factors, including the stigma associated with their line of work, limited access to healthcare facilities, and the nature of the profession itself. One of the biggest challenges for sex workers seeking medical care is the stigma and discrimination they encounter. Many medical professionals hold incorrect beliefs about sex work and may be unwilling to treat patients or unintentionally do so. The results are in line with the previous studies. Moreover, the results of the study coincided with the findings of a study by Shannon et al. [61] and Benoit et al. [45], as well as the precede-proceed model by Lawrence Green (1974) that social constructs like stigmatization and discrimination alter the quality of life for sex workers, consequently predisposing them to mental health problems and fear of seeking health care services [62].
Due to this, various health conditions, including STIs, HIV/AIDS, and mental health disorders, are not treated. The reviewed articles also mentioned limited access to healthcare services as a significant health challenge for sex workers. This can be attributed to several factors, including the fact that some nations consider sex work illegal or criminal, the fact that there are not enough resources available, or the places where sex work is done [41]. As a result, access to preventive care and seeking medical attention when necessary is restricted for sex workers, which might worsen their health concerns. However, the nature of sex work itself carries certain health risks, including the possibility of physical harm, sexual assault, and contact with STDs [32]. The survey also revealed that it can be challenging for sex workers to receive medical treatment during regular business hours due to the profession's long hours and unpredictable schedules [4]. Overall, the difficulties that sex workers have access to healthcare highlight the need for policies and services that recognise this community’s particular difficulties and offer access to safe and supportive healthcare services to promote sex workers' health and well-being.
The general population stigmatises and discriminates against sex workers in the social setting. This is due to the widespread perception of sex work as immoral or abnormal, which may lead to negative attitudes toward sex work and individuals who engage in it. The results include social marginalisation as well as prejudice in employment and housing. The fact that sex work is prohibited only makes the social struggle that sex workers face worse [5]. When the research was examined, it became clear from numerous studies that sex workers are subjected to harassment, violence, and arrest by law enforcement, further isolating them from society and reducing their ability to seek legal or medical assistance [31, 16]. The challenges that sex workers face generally demonstrate the need for laws. The Precede-Proceed model proposes that to address the life complexities of sex workers in a social and health context, social constructs like stigmatization and discrimination among society, as well as the healthcare personnel, need to be addressed in order to improve the quality of life for sex workers. Increased incidence of STIs and HIV/AIDS among sex workers can be reduced by addressing the behavior of society and healthcare personnel towards sex workers [62, 63].
5. RECOMMENDATIONS
This comprehensive assessment offers crucial information on the difficulties faced by sex workers in South African communities in terms of healthcare and social challenges. To avoid healthcare and social battles among sex workers, the healthcare and social partners must actively work to eradicate this scourge from society. Addressing the social and medical issues faced by sex workers is a complicated issue that calls for multiple solutions and total commitment from all social and healthcare partners, including government and civil society. Evidence-based programs must be created to address the social and medical issues that sex workers encounter and to construct a theoretical framework. Additionally, there is a need for safety precautions, the beginning of campaigns to lessen stigma and violence, the provision of specialized healthcare services and sensitivity training for healthcare professionals, the development of social support networks, and the encouragement of research projects that consider the perspectives of sex workers.
6. LIMITATIONS
The study was only concerned with the difficulties faced by sex workers in a medical and social setting. The included studies' quality and methodology differed, which could have introduced biases and weakened the validity of the results. Another issue is language bias, which resulted in the omission of critical viewpoints and studies by excluding papers published in languages other than English. The hidden and stigmatised nature of sex work can also lead to underreporting and restricted access to reliable data, affecting the assessment’s thoroughness. In the discussion, methodological limitations were not fully covered. The search methodology may have unintentionally left out a number of pertinent items, which may have impacted the thorough results. Notably, the lack of direct observation as a methodology may have prevented a more complex comprehension of the topic under study.
CONCLUSION
In conclusion, sex workers in South African communities face complex and varied social and health challenges. A multi-pronged strategy, including legal change, destigmatisation, and improved access to healthcare and social support services, will be needed to address these problems. To ensure that sex workers can receive the treatment and services they need to maintain healthy and satisfying lives, healthcare providers and policymakers must collaborate.
AUTHORS’ CONTRIBUTIONS
Leshata Winter Mokhwelepa contributed to the concept and design. Leshata Winter Mokhwelepa, Gsakani Olivia Sumbane, and Mxolisi Welcome Ngwenya participated in the acquisition, analysis, or interpretation of data. Leshata Winter Mokhwelepa and Mxolisi Welcome Ngwenya contributed to the drafting of the manuscript. Gsakani Olivia Sumbane and Leshata Winter Mokhwelepa carried out a critical review of the manuscript for important intellectual content. Leshata Winter Mokhwelepa, Gsakani Olivia Sumbane, and Mxolisi Welcome Ngwenya performed the formal analysis. Leshata Winter Mokhwelepa, Gsakani Olivia Sumbane, and Mxolisi Welcome Ngwenya provided administrative, technical, or material support. All authors have given their approval for the manuscript to be submitted.
LIST OF ABBREVIATIONS
| HIV | = Human Immunodeficiency Virus |
| STI | = Sexually Transmitted Infections |
STANDARDS OF REPORTING
PRISMA guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.
Supplementary material is available on the publisher’s website along with the published article.