Risk Factors Associated with Malignant Lung Nodules in Smokers with Coal Worker’s Pneumoconiosis: An Exploratory Case-control Study
Abstract
Background
Benign lung nodules (LN) in coal worker’s pneumoconiosis (CWP) may be indistinguishable from lung cancer (LC) on radiography. There is a lack of validated LN risk calculators and LN management guidelines for CWP patients.
Objective
We sought to identify characteristics predictive of LC in LN detected in smokers with CWP.
Methods
An exploratory case-control study was conducted between 2015 to 2020. All adult ever-smokers with radiographic-proven CWP and LN, which were biopsied, were included. Multivariable logistic regression models were used to quantify adjusted associations between demographic and radiographic characteristics.
Results
Of the 29 eligible patients, 15 (52%) had biopsy-proven LC and 14 (48%) had benign LN. Solid LN increased the odds of LC by 21.6 times (p=0.17). Patients with radiographic emphysema were 2.21 times more likely to have a malignant LN (p=0.51). LN spiculation was associated with a higher risk of LC (OR=1.73, p=0.72), as was the presence of a solitary LN (OR=9.35, p=0.13). Multiple LN was found to be negatively associated with LC (OR=0.18, p=0.36). Family history of LC, pack-years of smoking, and exposure to silica and/or coal were not found to be predictive of malignancy (OR≤1, p>0.05).
Conclusion
Solid and spiculated LN associated with emphysema and multiple LN was found to be correlated with a higher risk for LC in CWP ever-smokers. No statistically significant association was found due to the small number of patients. This study highlights unique LN features conferring a higher risk of LC among smokers with CWP. Larger, prospective, multicentric studies should be conducted to confirm these findings.
Clinical Trial Registration
The clinical trial registration number approved by the Institutional Review Board, West Virginia University, was #2109411710.
1. INTRODUCTION
Lung cancer is the second most common cancer diagnosed in both men and women in the United States (U.S.), with an incidence of approximately 230,000 cases annually [ 1]. The leading risk factor for the development of lung cancer is tobacco smoking, followed by age, environmental and radiation exposure, co-existing lung diseases, family history, and ethnicity [ 2]. Coal miners represent a unique subgroup of manual workers with a higher exposure rate to several mediators of lung cancers, including respirable silica, coal dust, radon, and diesel exhaust [ 3]. Furthermore, the prevalence of smoking among coal miners was as high as 56.3 to 66.3%, as reported in cross-sectional studies conducted in Turkey and China [ 4, 5]. Interestingly, the association between lung cancer and coal dust exposure has been less clear. A historical cohort study reported lower lung cancer risk in coal miners [ 6]. This data has been disputed in more recent epidemiological studies showing a positive correlation between the risk of lung cancer among smokers with coal worker’s pneumoconiosis (CWP) [ 7, 8].
CWP is a distinct entity within the spectrum of coal mine dust lung disease, which includes disease manifestations like silicosis, dust-related diffuse fibrosis, and chronic obstructive pulmonary disease. The hallmark of CWP is the radiological presence of rounded and irregular lung opacities of variable sizes as well as distribution [ 9, 10]. With ongoing exposure and/or time, these nodules (classically less than 3cm in size) may enlarge into lung masses (opacities larger than 3cm) or may coalesce to form progressive massive fibrosis (PMF). Histologically, lung lesions seen in CWP and PMF are benign. Coal macules of CWP represent collections of carbon-laden macrophages. PMF is a severe form of CWP characterized by large carbonaceous scars containing dense collagen [ 11]. These lesions may have a necrotic center [ 11].
Long nodules and masses seen in CWP and PMF may be indistinguishable from lung cancer in chest X-rays and computed tomogram (CT) of the chest. Moreover, positron emission tomography (PET) scans are an imperfect discriminatory tool to distinguish malignant from benign lung nodules in CWP as these nodules have an increased fluorine 18-fluorodeoxyglucose (FDG) uptake and high standardized uptake values (SUV). Thus, most benign lesions in CWP are falsely positive on PET and do not correlate with malignancy [ 10]. Unfortunately, this may lead to an excess of unnecessary biopsies and surgical procedures with its attendant risks.
Presently, there is a paucity of clinical guidelines to inform clinicians on approaches to risk-stratified patients in this group to inform best practices in lung nodule management. Existing lung nodule risk calculators, namely Brock University [ 12], Bayesian Inference [ 13, 14], and Mayo Clinic [ 15] models routinely used in clinical practice, were studied and validated in the general population. As these models have not been tested in the CWP population, it is unclear whether these risk calculator models can be applied to CWP patients for the assessment and management of lung nodules. It is crucial to address appropriate patient selection for advanced and/or invasive procedures in the evaluation of lung nodules in patients with CWP to prevent unnecessary complications. The urgency and importance of this issue are underscored in the increasing proportion of U.S. coal miners diagnosed with CWP since 2000 under the Black Lung Surveillance Program [ 3]. The prevalence of CWP among coal miners with a 25-year tenure has now doubled to 7% [ 3]. In this study, we sought to determine unique patient and lung nodule and/or mass characteristics in smokers with CWP with lung nodules with the intent of improving lung cancer screening in smokers with CWP.
2. METHODS
2.1. Study Design and Setting
This retrospective observational exploratory case-control study was conducted at a rural academic center. Characteristics, interventions, and outcomes of adult, ever-smokers with the diagnosis of CWP who had lung biopsies for the evaluation of lung nodules and/or masses were extracted. The study protocol was approved by our organization’s Institutional Board Review (#2109411710) on September 23 rd, 2021. Deidentified data obtained for clinical evaluation was used. The study adhered to the institution’s ethical standards on human experimentation and the Helsinki Declaration of 1975. The study conformed to the “Strengthening the Reporting of Observational Studies in the Epidemiology (STROBE)” guidelines [ 16].
2.2. Participants and Study Size
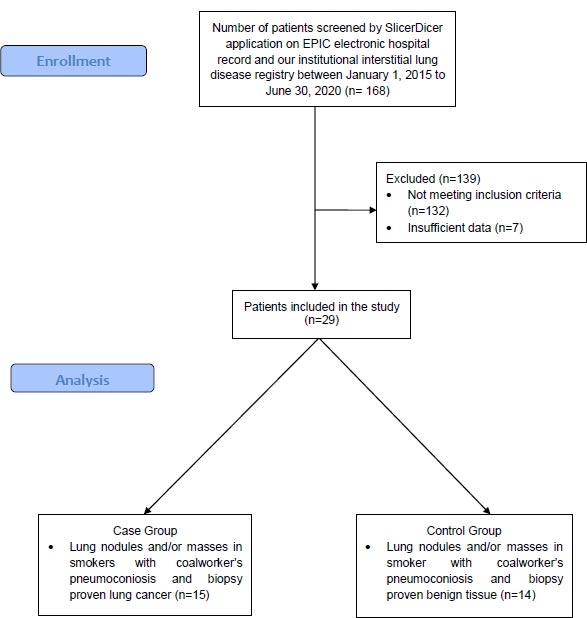
The Slicer Dicer function of EPIC electronic health record and the institution’s interstitial lung disease registry were utilized to identify patients with the diagnosis of CWP between January 1 st, 2015 to June 30 th, 2020. We used the following keywords for patient identification in EPIC: (1) pneumoconiosis, (2) coal exposure, (3) asbestos exposure, (4) silica exposure, (5) unspecified pneumoconiosis, (6) coal worker’s pneumoconiosis, (7) chronic diagnosis, (8) emergency department diagnosis, (9) ‘any time point’ diagnosis, (10) bronchoscopic biopsy, (11) interventional radiology biopsy, (12) CT biopsy, (13) robotic biopsy, (14) lung cancer, (15) lung nodule, (16) lung mass, (17) malignant, (18) benign, (19) smokers, and (20) more than 18 years of age. We excluded 139 patients who did not meet the following criteria: (1) ever-smokers, (2) exposure to either coal, asbestos and/or silica, (3) clinical and radiographic evidence of CWP, and (4) lung nodule and/or lung mass evaluation resulting in lung biopsy. Patients with known lung cancer and/or other solid and/or hematopoietic malignancies at the time of lung biopsy were excluded. After an individual review of all cases by BB, RP, JC, and TA, patients with insufficient clinical data were excluded. A total of 29 patients met all the inclusion criteria of the study, as noted in the “CONSORT Flow Diagram” [ 17] (Fig. 1).
2.3. Selection of Cases and Controls
Between January 1 st, 2015 to June 30 th, 2020, patients aged 18 or more years who were ever-smokers, diagnosed with CWP, had a lung mass and/or lung nodule and had biopsy-proven lung cancer were eligible to be selected as cases. Patients were selected as controls if they were aged 18 or more years who were ever-smokers, diagnosed with CWP, had a lung mass and/or lung nodule, and had biopsy proven benign lung nodule and/or mass.
Family history of lung cancer, smoking history, type of occupational exposure, radiographic presence of emphysema, radiological lung nodule and/or mass characteristics, and pathology report were reviewed and recorded. We specifically identified the size of the nodules and/or masses, their location(s), their appearance, i.e., solid, subsolid, or ground glass, the presence of spiculation, and the quantity of lung nodules and/or masses present on CT chest at the time of lung biopsy performance. Histopathologic evaluation was required to establish malignancy.
2.4. Outcomes
The primary outcome of this case-control study was to identify patient and radiological risk factors associated with lung cancer in patients with CWP, lung nodules and/or masses who are ever-smokers. We compared and analyzed data from cases and control groups to determine the unique characteristics of patients with CWP and lung nodules and/or masses conferring a higher risk for malignancy in the hopes of guiding lung nodule screening in these groups of patients.
2.5. Data Collection
All study records were securely stored in our institution’s network of computers in the outpatient pulmonary office.
2.6. Statistical Methods
All outcome measures and endpoints were analyzed descriptively. Continuous variables were reported in means with standard deviation. Frequencies and percentages were reported for categorical data. Multivariable logistic regression models were used to quantify adjusted associations by calculating odds ratios between several demographic and radiographic characteristics and biopsy-proven lung malignancy. All statistical analyses were performed using R 4.2.1 (R Core Team, Vienna, Austria).
2.7. Bias
This cross-sectional study describes the characteristics of CWP patients who have undergone lung biopsy for malignancy work-up in the rural Appalachian region at a distinct time point. Selection bias was avoided by having four independent reviewers determining the suitability of patients included in the study. Four reviewers conducted independent chart reviews to extract and analyze data. A consensus decision was sought when any disagreements occurred. Information bias may occur in a retrospective study.
3. RESULTS
3.1. Participants
Baseline patient and lung nodule and/or mass characteristics in smokers with CWP are illustrated in Table 1. All 29 patients were included in the final analyses, of which 15 (51.7%) had biopsy-proven lung cancer, and 14 (48.3%) had benign lung nodules. Overall, the age, race, gender, and family history of cancer in both groups were similar. The proportion of heavy smokers, i.e., more than 20 pack-year, was similar in both groups (n=12, 80.0% vs. n=11, 78.5%). Exposure history, as determined by information provided by patients and documentation within medical records, was homogenous in both groups, with the exception of 1 patient (6.7%) in the lung cancer group reporting exposure to asbestos. All patients denied exposure to silica. Three patients (20.0%) reported exposure to both coal and asbestos in the lung cancer group compared to 4 patients (28.6%) in the benign lung nodule and/or mass group. The tenure of exposure was alike in both groups (Table 2).
The most common histopathological finding in benign lung nodules and/or mass was anthracosis (n=8, 57.1%). One patient (7.1%) had a hamartoma, two (14.3%) had inflammatory lung nodules, and three patients (21.4%) had no further characterization of histopathological data documented in the medical records. In patients with lung cancer, the most common histopathological finding was squamous cell cancer (n=7, 46.7%), followed by adenocarcinoma (n=5, 33.3%). A single patient (6.7%) for each category of small cell lung cancer, poorly differentiated carcinoma, and lymphoma was found. Benign lung nodules [(M=25.2 (28.4) x M=21.2 (17.5) mm] were larger than malignant lung nodules [(M=19.3 (15.5) x M=15.7 (10.7) mm] in smokers with CWP. Malignant nodules and/or mass were more often solid in nature (n=13, 86.7%) compared to benign nodules, and mass was solid (n=7,50.0%), subsolid (n=4, 28.6), and ground-glass (n=4, 21.4%), respectively. Upper lobe lung nodule and/or mass was more often malignant (n=10, 50% vs n=9, 39.1%). Both benign and malignant lung nodules and/or mass was similarly present in patients with solitary or multiple synchronous nodules. Malignant lung nodule and/or mass was more often spiculated than benign lesions (n=6, 40% vs. n=4, 28.6%).
| Characteristics | Malignant Lung Nodule (n=15) | Benign Lung Nodule (n =14) |
| Age, median (IQR)
Male, n (%) White, n (%) Radiographic emphysema, n (%) Family history of cancer, n (%) |
70.0 (63.0, 75.0)
15 (100.0) 15 (100.0) 11 (73.3) 13 (86.7) |
65.0 (60.0, 72.0)
14 (100.0) 14 (100.0) 9 (64.3) 10 (71.4) |
| Tobacco smoking (pack-years), n (%)
• < 10 • 10 – 20 • 20 – 30 • 30 – 40 • >40 • Unknown |
2 (13.3)
1 (6.7) 2 (13.3) 3 (20.0) 7 (46.7) 0 |
3 (21.4)
0 1 (7.1) 4 (28.6) 5 (35.7) 1 (7.1) |
| Exposure, n (%)
• Coal • Asbestos • Silica • Multiple |
11 (73.3)
1 (6.7) 0 3 (20.0) |
10 (71.4)
0 0 4 (28.6) |
| Duration of exposure, n (%)
• < 10 • 10 – 20 • 20 – 30 • 30 – 40 • >40 • Unknown |
0
3 (20.0) 1 (6.7) 7 (46.7) 1 (6.7) 3 (20.0) |
0
5 (35.7) 1 (7.1) 6 (42.9) 0 2 (14.3) |
| Histology of nodule/mass, n (%)
• Benign o Anthracosis o Necrosis o Inflammation o Hamartoma o Unknown • Malignant o Small cell cancer o Squamous cell cancer o Adenocarcinoma o Poorly differentiated carcinoma o Lymphoma |
0
0 0 0 0 1 (6.7) 7 (46.7) 5 (33.3) 1 (6.7) 1 (6.7) |
8 (57.1)
0 2 (14.3) 1 (7.1) 3 (21.4) 0 0 0 0 0 |
| Size of nodule/mass (mm), n (%)
• Length, mean (SD) • Width, mean (SD) |
19.3 (15.5)
15.7 (10.7) |
25.2 (28.4)
21.2 (17.5) |
| Nodule/mass appearance, n (%)
• Solid • Subsolid • Ground-glass |
13 (86.7)
1 (6.7) 1 (6.7) |
7 (50.0)
4 (28.6) 3 (21.4) |
| Location of nodule/mass, n (%)*
• Upper lobe • Middle lobe • Lower lobe • Lingula |
n=20
10 (50.0) 5 (25.0) 5 (25.0) 0 |
n=23
9 (39.1) 6 (26.1) 7 (30.4) 1 (4.3) |
| Number of nodules/masses per patient, n (%)
• 1 • 2 • 3 • 4 • 5 • >5 |
3 (20.0)
3 (20.0) 2 (13.3) 3 (20.0) 2 (13.3) 2 (13.3) |
5 (35.7)
3 (21.4) 1 (7.1) 1 (7.1) 0 4 (28.6) |
| • Spiculated nodule/mass, n (%) | 6 (40.0) | 4 (28.6) |
| Characteristics | Adjusted Odds Ratio | p-value | Coefficient | Standard Error |
|---|---|---|---|---|
| Solid lung nodule | 21.60 | 0.174 | 3.07 | 2.19 |
| Solitary lung nodule | 9.35 | 0.127 | 2.24 | 1.46 |
| Emphysema on CT chest | 2.21 | 0.514 | 0.80 | 1.22 |
| Lung nodule spiculation | 1.73 | 0.721 | 0.55 | 1.53 |
| Duration of coal exposure | 1.49 | 0.421 | 0.40 | 0.50 |
| Subsolid lung nodule | 1.27 | 0.160 | 0.24 | 2.63 |
| Size of lung nodule | 1.01 | 0.804 | 0.01 | 0.03 |
| Cigarette smoking pack-years | 1.00 | 1.000 | -0.01 | 0.52 |
| Multiple lung nodules | 0.18 | 0.358 | -1.70 | 1.85 |
| Coal exposure | 0.13 | 0.927 | -2.06 | 22.38 |
| Coal and silica exposure | 0.11 | 0.921 | -2.19 | 22.40 |
| Family history of lung cancer | 0.10 | 0.148 | -2.28 | 1.58 |
3.2. Outcome Data
In smokers with CWP, biopsy-proven lung cancer, in contrast to benign lung lesions, was more likely to occur in solid or subsolid lung nodules and/or mass with OR 21.6 ( p = 0.174) and OR 1.27 ( p = 0.16), respectively. Lung cancer was more likely if the nodule and/or mass were solitary (OR 9.35, p = 0.127) and spiculated (OR 1.72, p = 0.721). The presence of concomitant emphysema in radiographs increased the likelihood of malignant lung nodules and/or masses (OR 2.21, p = 0.514). Prolonged tenure in coal mining was associated with a higher risk for lung cancer (OR 1.49, p = 0.421). Size of lung nodule and/or mass was slightly associated with lung cancer (OR 1.01, p = 0.804). Cumulative tobacco smoking, presence of synchronous multiple lung nodules and/or masses, reported exposure to coal and coal and silica simultaneously, and finally, family history of lung cancer were not predictive of lung cancer in this study with all OR <1 ( p>0.05).
4. DISCUSSION
4.1. Key Results
This study tests the hypothesis that epidemiologic and radiologic features can be predictive of malignancy in the evaluation of lung nodules and/or masses among smokers with CWP. We demonstrated that solitary, solid, subsolid, larger size, and spiculated lung nodules and/or masses are associated with biopsy-proven lung cancer. CWP patients with radiographic emphysema and longer coal mining tenure are more likely to have lung cancer. It is noteworthy that none of these associations demonstrated statistical significance owing to the limited sample size. However, our findings highlight key considerations in the applicability of lung nodule risk calculators and lung cancer screening practices specific to CWP patients.
Lung cancer screening has been advocated since the publication of the National Lung Screening Trial in 2011 to mitigate the risk of advanced-stage lung cancer with a dismal 5-year survival of 20.5% [ 18]. There are several lung cancer screening regimens, including (1) the American College of Radiology Lung Reporting and Data (Lung-RADs) system, the British Thoracic Society (BTS) guidelines, and the American College of Chest Physicians (ACCP) guidelines. The BTS and ACCP guidelines are unique among these screening programs due to the incorporation of crucial patient and exposure risk factors [ 19]. In fact, the BTS and ACCP guidelines outperform the Lung-RADS in terms of their accuracy in detecting lung cancer (BTS: accuracy 87%, sensitivity 80%, specificity 92%; ACCP: accuracy 80%, specificity 84%; Lung-RADS: sensitivity 59%, specificity 93%) [ 19]. This study highlights the importance of integrating individual risk factors in addition to radiological features of lung nodules in lung cancer screening. These screening programs are developed for the general population who are ever-smokers and do not specifically address groups of people with an elevated lung cancer risk due to occupational exposures.
The Brock University cancer prediction equation [ 20] is a risk stratification tool used to assist clinicians in navigating the lung nodule evaluation algorithm. It incorporates patients’ age, gender, family history of lung cancer, presence of emphysema and nodule spiculation, size, type, location, and count. All these features correlate with the findings of this study except for the coal mining tenure. In contrast, the Bayesian prediction model [ 13, 14] includes historical features of malignancy, smoking, and hemoptysis. It distinctly includes factors, such as nodule growth rate, presence of calcification, edge on X-ray and CT chest, and cavity wall thickness. Characteristically, it omits any consideration for occupational exposures. Based on the Brock University model, a risk prediction score in excess of 10% would then entail the utilization of PET scans [ 21]. Based on the FDG uptake and SUV, a lung nodule with high malignancy risk would then be biopsied or alternatively surgically removed [ 21]. The Mayo Clinic model, on the other hand, includes the likelihood of malignancy on PET [ 15]. The absence of a lung nodule risk calculator tool specific for CWP patients may overestimate the risk of lung cancer, hence subjecting CWP patients to invasive procedures with a high false positive rate for lung cancer. This is exemplified in this study, with at least half of CWP ever-smokers having a benign lung nodule (48.3%) following invasive procedures, including lung resections.
Coal mining is a growing industry with approximately 8 million individuals employed all over the world [ 3]. The U.S. contributes up to 30% of the world’s coal reserves [ 3]. The prevalence of CWP among coal miners has been increasing since 2000 in the U.S., distinctly in the central Appalachian region [ 22]. Thus, it has become increasingly critical to address the lack of validated tools for lung nodule risk assessment in CWP patients. One optimistic development is the utilization of magnetic resonance imaging (MRI) of the chest to discriminate lung cancer from benign lung nodules in patients with CWP and PMF. Ogihara and colleagues demonstrated that lung cancer lesions show intermediate to high signal intensity in contrast to PMF lesions, which show a low signal intensity on T2-weighted images [ 23]. PMF lesions had a gradual enhancement compared to lung cancer lesions, which had a more rapid enhancement pattern on MRI [ 23]. Unfortunately, more studies evaluating the usefulness of MRI in differentiating benign from malignant lung nodules are required. In a recent systematic review, PET/MRI was non-superior to PET/CT in detecting lung cancer in lung nodules larger than 10mm [ 24].
4.2. Generalizability and Limitations
This study has several limitations. First, this is a retrospective observational study. All patients included in the study were White and males, mirroring the unique sociodemographic nature of the coal mining industry and the rural West Virginia Appalachia region [ 25]. To improve the external validity of the findings noted in this study, the inclusion of a more ethnically and geographically diverse population would shed light on the risk of lung cancer in lung nodules of ever-smokers with CWP. Second, the retrospective nature of the study may lead to selection bias. The methods section described methods to mitigate these biases. To improve the statistical strength of this study, confounding variables may be controlled by limiting our analyses to a few variables.
CONCLUSION
The evaluation and management of lung nodules and/or masses in smokers with CWP continue to be a challenge for clinicians due to the lack of validated predictive calculators and poorly sensitive imaging tools. These patients are thus more likely to undergo invasive procedures compared to the general population. This study suggests unique patient and nodule and/or mass characteristics in addition to exposure duration conferring a greater risk for lung cancer among smokers with CWP. Further larger, multicenter, and prospective studies are warranted to validate these findings. In the meantime, it is paramount for clinicians to practice individualized medicine when managing suspicious lung nodules and/or masses in patients with CWP.
LIST OF ABBREVIATIONS
| ACCP | = American College of Chest Physicians |
| BTS | = British Thoracic Society |
| CWP | = Coal worker’s pneumoconiosis |
| CT | = Computed tomogram |
| FDG | = Fluorodeoxyglucose |
| MRI | = Magnetic resonance imaging |
| PET | = Positron emission tomography |
| PMF | = Progressive Massive Fibrosis |
| SUV | = Standardized uptake values |
| U.S | = United States |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol was approved by our organization’s Institutional Board Review (#2109411710).
CONSENT TO PARTICIPATE
The informed consent requirement was waived. Only deidentified data obtained for clinical evaluation purposes was used.
STANDARDS OF REPORTING
STROBE guidelines were followed.
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study. The study was conducted in accordance with the institutional ethical standards on human experimentation and with the Helsinki Declaration of 1975.
CONFLICT OF INTEREST
The authors confirmed that there is no conflict of interest related to the manuscript.
AVAILABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials. The data that support the findings of this study are available from the corresponding author, BB, on special request.
FUNDING
None.
ACKNOWLEDGEMENTS
The authors would like to thank Rachel Salyer, PhD, for her assistance and support in reviewing and editing this manuscript. They would also like to thank the West Virginia Clinical and Translational Sciences Institute for their input on the statistical analyses included in this manuscript.


