All published articles of this journal are available on ScienceDirect.
Social Risk Factors Contributing to Anxiety, Depression and Stress among Indian Healthcare Students during Lockdown
Abstract
Background
The increase in mental health disorders among the general population, healthcare workers and students during the pandemic was evident. There are scanty reports regarding the mental health status of students in the health care services from India during the pandemic lockdown. This study aims to find the risk factors of anxiety and stress among these students and to evaluate the adapting mechanisms to alleviate the same.
Methods
A web-based cross-sectional survey was perfomed in students undergoing undergraduate courses in various healthcare services after institutional ethical clearance. The study tool was a pre-validated self-administered questionnaire in the google form. The link was shared in various WhatsApp groups to be shared among students with a brief description of the study after proper content validation.
Results
Of the 527 respondents, 291 (56%) were females, 385 (74%) were in MBBS Courses, and 178 (34%) were from government colleges. Prevalence of anxiety, depression and stress were 372 (70.6%), 360 (68.3%) and 262 (49.7%), respectively. The mean scores of anxiety, depression and stress were 14.33 ± 10.4, 17.24 ± 12.21 and 16.60 ±10.4, respectively. The presence of anxiety, depression and stress was not associated with age, course and year of study, type of Institutions in which they study, socioeconomic status and performance in the recent written examination. There was no association of gender with anxiety and depression, but females had more stress than males (p = .025). Extremely severe levels of anxiety, depression and stress were seen in 158 (30%), 124 (23.5%) and 43 (8%), respectively. A total of 296 (57%) of the students started a new hobby during the lockdown. Students who felt relaxed after talking to their teachers or mentors, students who shared talks with family members and friends, students whose parental fights were less, and students who opened up with parents were less likely to have anxiety and stress.
Conclusion
The prevalence of anxiety, depression and stress in healthcare students from our country was very high. Most of the students needed motivation during the pandemic lockdown. Proper psychological support to students of health care services is a necessity in such a crisis situation.
1. INTRODUCTION
The Coronavirus disease 2019 (COVID-19) pandemic has been stressful for people. A meta-analysis reported stress, anxiety and depression to be high in the general population across the world during this period [1]. Among different professions, students and healthcare professionals were found to experience stress, anxiety, and depression more than others [2]. Varied global herd immunity rates pose ongoing risks. Demographics, socioeconomic factors, and health behaviors impact disease transmission. Understanding these factors is vital for effective responses [3]. Worldwide, many studies suggested that there was an increase in mental health issues among healthcare workers located in a variety of fields and positions during the covid-19 pandemic [4-6]. Furthermore, studies have reported regarding the mental health problems among students during this pandemic [7-9]. A study from India reported more than 80% of participants felt the need for professional help from mental health experts to deal with emotional issues and other psychological issues during the pandemic [10]. The COVID-19 pandemic has also heightened the risk of suicidality among adolescents due to stress, while lockdowns and school closures have exacerbated mental health challenges [11]. The authors believe the mental health state of students of different healthcare services during the lockdown period of the pandemic may be high, for which there are very scarce reports, especially from India [12, 13]. The social risk factors for psychological states may vary from region to region in different parts of the world. A study involving Siberian Indigenous peoples reported declining mental health due to the loss of their cultural values [14]. Thus, it is essential to find out the psychosocial factors affecting the mental health of students who will be in the workforce of the healthcare system in the future in such pandemic-like situations. This study was planned to find the prevalence and the levels of anxiety, depression and stress among the students of health care services during the second lockdown period of the pandemic. The secondary objective was to determine the associated risk factors of anxiety and stress and evaluate the adapting mechanisms to alleviate the same.
2. MATERIALS AND METHODS
This web-based cross-sectional survey was planned during the lockdown period of the COVID-19 pandemic in a medical school of a reputed university in Eastern India after institutional ethical approval (KIIT/ KIMS/ IEC/ 368/ 2020 dated 24.08.2020). The data collection was for a six-week period from 1st September to 15th October, 2020. The study participants were all students undergoing undergraduate courses in health care services (MBBS, BDS, Nursing, BPT/ BPO) anywhere in India. Students aged between 16 to 30 years who gave consent for participation were included in the survey. Non-consenting students and students undergoing post graduate courses were excluded from the study. Students under treatment for any psychiatric illness were also excluded from the study. The study tool was a pre validated self-administered questionnaire in the Google form with six sections. The first section contained a proper explanation of the study objectives and the consent for participation. The second and third sections had the socio-demographic details and twenty-five self-framed questions relating to the cause of anxiety, depression and stress, respectively, during the lockdown period. The choices in all the twenty-five questions in the third section were dichotomous, having responses of either ‘yes’ or ‘no’ (Fig. 1). The fourth and fifth sections contained the questions of DASS21 (Depression, Anxiety and Stress Scale) and three questions related to Kuppuswamy socio-economic status, respectively [15, 16]. The last section contained self-framed questions regarding the changes after the lockdown and the adaptive strategies adopted by students to alleviate their anxiety, depression and stress. Questions like the development of new hobbies, change in food habits, development of substance abuse, seeking mental health advice, increased reading habits, and increased use of social media were the few questions asked in the last section. Few of the questions had dichotomous responses, and others were open-ended questions regarding the type of new hobbies they developed. There were 21 items in the DASS 21 questionnaire with 7 questions, each designed to measure the state of anxiety, stress and depression, respectively. Each question can be reported as 0, 1, 2, 3; Where ‘0’= did not apply to me at all, ‘1’ = applied to me to some degree or some of the time, ‘2’ = applied to me to a considerable degree or a good part of time, ‘3’ = applied to me to very much or most of the time. Scores for anxiety, stress and depression were calculated by summing the scores for relevant items. Scores on DASS 21 need to be multiplied by two to calculate the final scores. Individuals having scores of more than 7, more than 9 and more than 14 were considered to have anxiety, depression and stress, respectively. The Kuppuswamy Socioeconomic Scale included 3 parameters: educational status of the head of families, occupational status and overall aggregate income of the family. Each parameter was further classified into subgroups, and scores were allotted to each subgroup. The total score of the Kuppuswamy Socioeconomic Scale ranged from 3-29, and it classified families into 5 groups: upper class (26-29), upper middle class (16-25), lower middle class (11-15), upper lower (5-10) and lower (< 5) socio-economic class. The content validation of the questionnaire was done by experts and students (sixteen) using a review form after the details of the study were individually explained to them. The questions were modified as per the feedback received from them. The link to the Google form was shared in various WhatsApp groups to be shared among students with a brief description of the study. The link was opened for one and a half months to receive responses.
2.1. Statistical Analysis
All the data were cleaned and analyzed using SPSS version 21. A descriptive analysis of sociodemographic characteristics and associated risk factors in terms of the presence or absence of anxiety, depression and stress was performed. Data were expressed as percentages and 95% confidence intervals. Students with anxiety, depression and stress were classified into mild, moderate, severe and extremely severe groups according to DASS21 cut-off scores. Chi-square was applied to compare the categorical variables between the students with and without anxiety, depression or stress, respectively. Odds Ratio and 95% Confidence Intervals were calculated to find the risk factors of anxiety and stress. The level of statistical significance was set at p < 0.05 for all the analyses.
3. RESULTS
A total of 527 students, mostly 20-22 years of age, replied to the online survey. Among the respondents, the proportion of female students was slightly higher, at 291 (56%) in comparison to males. Three fourth of these, i.e., 385 (74%), were medical students studying MBBS, and nearly half, i.e., 237 (45%), were in the first year of their education. Among these students, 178 (34%) were studying in government colleges. Due to the COVID-19 pandemic, most of the students, i.e., 501 (96%), were residing with their family/relatives (Table 1).
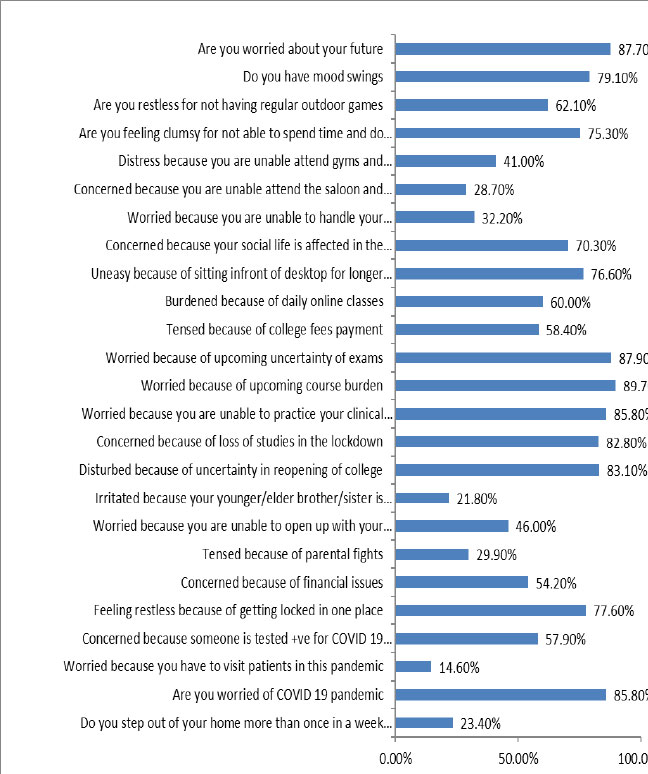
Fig. (1) describes the responses given by the participants to the survey questions as ‘Yes.’ Most of the students were worried regarding their future (88%), upcoming course burden (89.7%), upcoming uncertainty of exams (87.9%), inability to practice their clinical skills/practical (85.8%), loss of studies in the lockdown (82.8%), uncertainty in the reopening of college (83.1%), college fees payment (58.4%) and other financial issues (54.2%). Further, most of the students were burdened because of daily online classes (60.0%) and sitting in front of desktops for longer periods (76.6%). A large proportion of students had mood swings (79.1%), felt restless because of getting locked in one place (77.6%), inability to have regular outdoor games (62.1%), inability to spend time with friends (75.3%), inability to attend gyms and healthcare centers (41.0%) and few were concerned because someone tested positive for COVID 19 in their family, friends, relatives or in locality (57.9%). Most of the students (70.3%) considered that their social life was affected during lockdown. A few of the students also reported that they were worried because they had to visit patients during this pandemic (14.6%). While residing at home, respondents encountered certain issues with family, like the inability to open up with their parents (46.0%), difficulty in handling relationships (32.2%), tension because of parental fights (29.9%) and disturbances from the siblings (21.8%).
| Basic Details |
Frequency n (%) |
Stress n = 262 (49.7%) |
Anxiety n = 372 (70.6%) |
Depression n = 360 (68.3%) |
|---|---|---|---|---|
| Type of Institution | - | - | - | - |
| Government College | 178 (34.1%) | 92(35.1%) | 129 (34.7%) | 121 (33.6%) |
| Private College | 344 (65.9%) | 170(64.9%) | 243 (65.3%) | 239 (66.4%) |
| Course | - | - | - | - |
| MBBS | 385 (73.8%) | 199(76.0%) | 279(75.0%) | 270 (75.0%) |
| BDS | 93 (17.8%) | 42(16.0%) | 59(15.9%) | 63 (17.5%) |
| Nursing | 31 (5.9%) | 15(5.7%) | 24(6.5%) | 17 (4.7%) |
| Others | 13 (2.5%) | 6(2.3%) | 10(2.7%) | 10 (2.8%) |
| Year of Study | - | - | - | - |
| 1st year | 237 (45.4%) | 126(48.1%) | 177(47.6%) | 170 (47.2%) |
| 2nd year | 106 (20.3%) | 44(16.8%) | 72(19.4%) | 63 (17.5%) |
| 3rd year | 91 (17.4%) | 49(18.7%) | 63(16.9%) | 65 (18.1%) |
| 4th Year | 88 (16.9%) | 43(16.4%) | 60(16.2%) | 62 (17.2%) |
| Age Group | - | - | - | - |
| 17 - 19 Years | 87 (16.7%) | 44(16.8%) | 63(16.9%) | 59 (16.4%) |
| 20 - 22 Years | 351 (67.2%) | 183(69.8%) | 246(66.1%) | 247 (68.6%) |
| 23 - 25 Years | 80 (15.3%) | 34(13.0%) | 61(16.4%) | 52 (14.4%) |
| 26 - 28 Years | 3 (0.6%) | 1(0.4%) | 2(0.5%) | 2 (0.6%) |
| >28 Years | 1 (0.2%) | 0(0.0%) | 0(0.0%) | 0 (0.0%) |
| Gender | - | - | - | - |
| Male | 226 (43.7%) | 101(38.8%) | 158(42.8%) | 153 (42.9%) |
| Female | 291 (56.3%) | 159(61.2%) | 211(57.2%) | 204 (57.1%) |
| Living Arrangements | - | - | - | - |
| With Family/Relatives | 501 (96.0%) | 252(96.2%) | 357(96.0%) | 350 (97.2%) |
| Hostel/Flat | 21 (4.0%) | 10(3.8%) | 15(4.0%) | 10 (2.8%) |
| Kuppuswamy Scale (Mean ± SD) | 20.89 ± 5.94 | 20.82 ± 6.01 | 20.86 ± 6.05 | 21.16 ± 5.91 |
| Socio-Economic Class | - | - | - | - |
| Upper | 153 (32.3%) | 73(30.7%) | 107(31.8%) | 110 (33.3%) |
| Upper Middle | 232 (49.0%) | 122(51.3%) | 167(49.7%) | 166 (50.3%) |
| Lower Middle | 60 (12.7%) | 28(11.8%) | 41(12.2%) | 35 (10.6%) |
| Upper Lower | 26 (5.5%) | 13(5.5%) | 19(5.7%) | 17 (5.2%) |
| Lower | 2 (0.4%) | 0(0.0%) | 2(0.6%) | 2 (0.6%) |
| Change After Lockdown | Frequency (%) |
|---|---|
| New Hobbies (Yes) | 296 (56.7%) |
| Change in Food Habits (Yes) | 385 (73.8%) |
| Type of Food Intake | - |
| Comfort Foods | 247 (47.3%) |
| Healthy Food | 275 (52.7%) |
| Substance Use (Yes) | 224 (42.9%) |
| Increase in Reading Habits (Yes) | 186 (35.6%) |
| Increase in Social Media Use (Yes) | 342 (65.5%) |
| Informal Conversation with Teachers/Mentors (Yes) | 100 (19.2%) |
| Feeling Relaxed after Talk with Teacher/Mentor (Yes) | 221 (42.3%) |
| Sought Mental Health Advice (Yes) | 62 (12.2%) |
| Need Motivation (Yes) | 345 (67.9%) |

Table 2 outlines the changed habits of students due to pandemic induced forced lockdown. A total of 296 (57%) of the students acquired a new hobby during the lockdown. A large proportion of the students noticed a change in their food habits. After this change, 275 (53%) of the students preferred to have healthy food. Also, 186 (36%) and 342 (65%) of the students had an increase in their reading habits and social media use, respectively. However, 224 (43%) students had a habit of substance abuse.
The proportion of students with anxiety, depression and stress was 372 (70.6%), 360 (68.3%) and 262 (49.7%), respectively. The mean scores of anxiety, depression and stress were 14.33 ± 10.4, 17.24 ± 12.21 and 16.60 ±10.4, respectively. The mean scores of anxiety, depression and stress were not associated with age, course and year of study, type of Institutions in which they studied, socioeconomic status and performance in the recent written examination. There was no association of gender with anxiety and depression, but girls had significantly more stress than boys (15.76 ± 10.08 vs 17.63 ± 10.54; p = .04).
Fig. (2) gives the number of students having mild, moderate, severe, extremely severe levels of anxiety, depression and stress, respectively. Half of the total students experienced some degree of stress, including 53 (10%), 87 (16%), 79 (15%) and 43 (8%) as mild, moderate, severe and extremely severe, respectively. Among the students having anxiety, 158 (30%) had extremely severe anxiety. A total of 35 (6.6%) students had mild anxiety, 117 (22.2%) had moderate, and 62 (11.8%) had severe levels of anxiety. Of those students who had depression, 55 (10.4%), 108 (20.5%), 73 (13.9%) and 124 (23.5%) had a mild, moderate, severe and extremely severe levels of depression, respectively.
Table 3 compares the social parameters with the presence or absence of anxiety, stress and depression, respectively. Most of these parameters were significantly different in students who had anxiety, stress and depression when compared to the students without anxiety, stress and depression, respectively. The prevalence of anxiety and depression was not affected by gender, but the prevalence of stress was significantly higher in girls than the boys (p = .025). The presence of anxiety, depression and stress was not associated with age, course and year of study, type of Institutions in which they studied, socioeconomic status and performance in the recent written examination.
Students adopted certain activities during the lockdown to deal with their mental disturbances, such as, listening to music (381 (72%)), watching movies and online content (316 (60%)), chatting with friends (282 (53.5%)), spending time on social media (233 (44%)), doing yoga/exercise (190 (36%)) or sharing their experiences with family members (169 (32%)). Some (35%) liked to sit alone and solve their problem. Others liked to cope by cooking new recipes, reading a book or novel, going on a ride and playing indoor/outdoor games or with pets (Fig. 3). Most of the students felt relaxed after talking to a teacher or mentor.
The students with anxiety sought motivation four times more compared to those without anxiety (OR 3.98; 95% CI [2.64 – 5.98]). Students with stress sought motivation three and a half times more compared to students without stress (OR 3.53; 95% CI [2.37-5.26]). Students with depression sought motivation three times more compared to students without depression (OR 3.35; 95% CI [2.25-5]).
Students who felt relaxed after talking to their teachers or mentors, students who shared talks with family members and friends, students whose parental fights were less, and students who were able to open up with parents were less likely to have anxiety and stress.
Furthermore, 32.1% of students coped by talking to their family members, and around 43% of students were engaged in substance abuse as a mechanism of coping. Table 4 describes the effect of one of the positive coping measures with that of negative coping measures on the prevalence of anxiety, depression and stress. The prevalence of anxiety, depression and stress was significantly lower in students who used positive coping mechanisms like talking to their parents than in those who coped using substances.
| Basic Details | Stress | Anxiety | Depression | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Absent | Present | p | Absent | Present | p | Absent | Present | p | |
| Do you step out of your home more than once a week during the pandemic | 71 (27.3%) | 51 (19.5%) | 0.034 | 38 (25.3%) | 84 (22.6%) | 0.501 | 41 (25.3%) | 81 (22.5%) | 0.483 |
| Are you worried about the COVID-19 pandemic | 216 (83.1%) | 232 (88.5%) | 0.073 | 123 (82.0%) | 325 (87.4%) | 0.112 | 133 (82.1%) | 315 (87.5%) | 0.102 |
| Worried because you have to visit patients | 26 (10.0%) | 50 (19.1%) | 0.003 | 8 (5.3%) | 68 (18.3%) | <0.001 | 17 (10.5%) | 59 (16.4%) | 0.077 |
| Concerned because someone tested positive for COVID-19 in your family, friends | 138 (53.1%) | 164 (62.6%) | 0.028 | 69 (46.0%) | 233 (62.6%) | <0.001 | 81 (50.0%) | 221 (61.4%) | 0.015 |
| Feeling restless because of getting locked in one place | 181 (69.6%) | 224 (85.5%) | <0.001 | 97 (64.7%) | 308 (82.8%) | <0.001 | 103 (63.6%) | 302 (83.9%) | <0.001 |
| Concerned because of financial issues | 116 (44.6%) | 167 (63.7%) | <0.001 | 56 (37.3%) | 227 (61.0%) | <0.001 | 68 (42.0%) | 215 (59.7%) | <0.001 |
| Tensed because of parental fights | 49 (18.8%) | 107 (40.8%) | <0.001 | 27 (18.0%) | 129 (34.7%) | <0.001 | 28 (17.3%) | 128 (35.6%) | <0.001 |
| Worried because you are unable to open up with your parents | 79 (30.4%) | 161 (61.5%) | <0.001 | 33 (22.0%) | 207 (55.6%) | <0.001 | 43 (26.5%) | 197 (54.7%) | <0.001 |
| Irritated because your younger/elder sibling is disturbing | 43 (16.5%) | 71 (27.1%) | 0.004 | 22 (14.7%) | 92 (24.7%) | 0.012 | 27 (16.7%) | 87 (24.2%) | 0.055 |
| Disturbed because of uncertainty in reopening of college | 196 (75.4%) | 238 (90.8%) | <0.001 | 108 (72.0%) | 326 (87.6%) | <0.001 | 115 (71.0%) | 319 (88.6%) | <0.001 |
| Concerned because of loss of studies | 201 (77.3%) | 231 (88.2%) | 0.001 | 111 (74.0%) | 321 (86.3%) | <0.001 | 125 (77.2%) | 307 (85.3%) | 0.023 |
| Worried because you are unable to attend your clinical skills | 215 (82.7%) | 233 (88.9%) | 0.041 | 120 (80.0%) | 328 (88.2%) | 0.015 | 132 (81.5%) | 316 (87.8%) | 0.056 |
| Worried because of upcoming course burden | 217 (83.5%) | 251 (95.8%) | <0.001 | 121 (80.7%) | 347 (93.3%) | <0.001 | 133 (82.1%) | 335 (93.1%) | <0.001 |
| Worried because of the uncertainty of exams | 210 (80.8%) | 249 (95.0%) | <0.001 | 123 (82.0%) | 336 (90.3%) | 0.008 | 127 (78.4%) | 332 (92.2%) | <0.001 |
| Tensed because of college fee payment | 135 (51.9%) | 170 (64.9%) | 0.003 | 71 (47.3%) | 234 (62.9%) | 0.001 | 83 (51.2%) | 222 (61.7%) | 0.025 |
| Burdened because of daily online classes | 127 (48.8%) | 186 (71.0%) | <0.001 | 70 (46.7%) | 243 (65.3%) | <0.001 | 84 (51.9%) | 229 (63.6%) | 0.011 |
| Uneasy as to sit longer time in front of the desktop | 176 (67.7%) | 224 (85.5%) | <0.001 | 97 (64.7%) | 303 (81.5%) | <0.001 | 110 (67.9%) | 290 (80.6%) | 0.002 |
| Concerned as your social life is affected in the lockdown | 160 (61.5%) | 207 (79.0%) | <0.001 | 83 (55.3%) | 284 (76.3%) | <0.001 | 97 (59.9%) | 270 (75.0%) | <0.001 |
| Worried because you are unable to handle your relationship | 55 (21.2%) | 113 (43.1%) | <0.001 | 31 (20.7%) | 137 (36.8%) | <0.001 | 30 (18.5%) | 138 (38.3%) | <0.001 |
| Concerned because you are unable attend saloon and parlours |
60 (23.1%) | 90 (34.4%) | 0.004 | 38 (25.3%) | 112 (30.1%) | 0.275 | 41 (25.3%) | 109 (30.3%) | 0.246 |
| Distress as you are unable attend gyms & healthcare centers | 94 (36.2%) | 120 (45.8%) | 0.025 | 54 (36.0%) | 160 (43.0%) | 0.141 | 61 (37.7%) | 153 (42.5%) | 0.298 |
| Are you feeling clumsy for not able to spend time with your close friends | 176 (67.7%) | 217 (82.8%) | <0.001 | 103 (68.7%) | 290 (78.0%) | 0.026 | 105 (64.8%) | 288 (80.0%) | <0.001 |
| Are you restless for not having regular outdoor games | 143 (55.0%) | 181 (69.1%) | <0.001 | 78 (52.0%) | 246 (66.1%) | 0.003 | 86 (53.1%) | 238 (66.1%) | 0.005 |
| Do you have mood swings | 174 (66.9%) | 239 (91.2%) | <0.001 | 93 (62.0%) | 320 (86.0%) | <0.001 | 101 (62.3%) | 312 (86.7%) | <0.001 |
| Are you worried about your future | 208 (80.0%) | 250 (95.4%) | <0.001 | 114 (76.0%) | 344 (92.5%) | <0.001 | 127 (78.4%) | 331 (91.9%) | <0.001 |

| - | Present/Absent | Students Coping by Talking to Family Member | Students Coping by Substance Use | X2 | p |
|---|---|---|---|---|---|
| Anxiety | Present | 103 | 170 | 10.145 | 0.001* |
| - | Absent | 66 | 54 | ||
| Depression | Present | 106 | 163 | 4.5 | 0.033* |
| - | Absent | 63 | 61 | ||
| Stress | Present | 73 | 126 | 6.57 | 0.010* |
| - | Absent | 96 | 98 |
| - | Studentswho had Conversations with a Family Member n=169 Mean±SD |
Students with Substance Use n=224 Mean±SD |
t | p |
|---|---|---|---|---|
| Anxiety | 12.37±10.05 | 15.76±10.61 | 3.21 | .0014* |
| Depression | 14.78±11.45 | 18.43±12.40 | 2.99 | .003* |
| Stress | 15.10±10.01 | 17.69±10.37 | 2.49 | .013* |
Table 5 shows the comparison of the total scores of anxiety, depression and stress among students coping with talking to family members and using substances. The total scores of anxiety, depression and stress were lesser in students who coped talking to their family members than compared to those who used substances for coping. These differences were statistically significant.
4. DISCUSSION
The prevalence of anxiety, stress and depression in this study is much higher (70.6%, 68.3% and 49.7%) than in a similar study conducted during the COVID 19 Lockdown by Mishra et al., where the prevalence of anxiety, stress and depression among healthcare students was reported to be 27.7%, 26.2% and 9.7% respectively [14]. Such differences may be due to the reason that the sample population considered in the latter study is from one private institute. In contrast, our study sample includes healthcare students from both private and government institutes throughout India. Whereas another Indian study published before the COVID pandemic reported a higher percentage of anxiety (66.9%), stress (53%) and depression (51.3%) among medical graduates [17]. Still higher prevalence of these conditions seen in our study is due to various social factors due to the lockdown.
The presence of anxiety and stress was not associated with age, course of the study, academic year, type of institution (private vs government) in which they studied, socioeconomic status and performance in the recent written examination, which was similar to another study [18, 19]. In this study, there was no association of gender with anxiety, which was in contrast to the finding of a study among college students in India where females reported more anxiety [20, 21]. The female students in this study reported more stress than males [22], which was contradictory to one of our own studies conducted previously during the normal curriculum of the MBBS course [23]. A higher prevalence of stress among girls during the lockdown might have been because of the increased household chores responsibilities during the lockdown, which is usually more for the girls than the boys in our country.
In this study, around 42%, 38% and 23% of students were having severe to extremely severe anxiety, stress and depression, respectively. While a study from Egypt showed similar prevalence in the extremely severe sub-group, an Indonesian study reported a much lower prevalence of anxiety and stress in this sub-group [24, 25]. Fear of COVID-19, issues in the families, financial crisis, continuous online mode of learning, uncertainties of examination pattern, confinement to one place, no social interactions, etc., were the common contributors to high levels of psychological distress among these students in this study [26].
Students who were able to share with their family members were in contact with their close friends, or were in touch with their mentors or faculty members did not report psychological impact. Previous studies have narrated mentoring and opening up with good friends has a positive impact on mental health [27, 28].
Many of the students developed a new hobby during the lockdown and had a change in food habits, which was similar to a previous study [21]. There was a rise in social media use and a rise in reading habits among students. Many students developed substance use for the first time. A recent study from the US reported a significant increase in alcohol consumption as a coping mechanism due to stress, loneliness, and depression during the pandemic [29].
Similar findings were seen in another study conducted among the general population of India [30]. Listening to music, watching movies and online content, and conversations with friends were the common measures to keep themselves busy. A study from Jordan reported cooking and baking were the most popular methods to improve mental state during the pandemic [31]. Around seventy percent of students agreed that they needed motivation during that period. This study reports twelve percent of the total participants sought psychiatric support for the first time. An Indian study reported similar findings, stating there was a 20% increase in mental health issues seen since COVID-19 [32].
| Parameters | Anxiety OR(95%CI) | Stress OR(95%CI) |
|---|---|---|
| Gender | - | - |
| Male | 0.88(0.6-1.29)* | 0.67(0.47-0.95)* |
| Female | 1.14(0.77-1.67)* | 1.49(1.05-2.11) |
| Worried because you have to visit patients during this pandemic | 3.97 (1.86-8.48) | 2.21(1.28-3.53) |
| Feeling restless because of getting locked in one place | 2.63(1.71-4.04) | 2.57(1.67-3.97) |
| Concerned because of financial issues | 2.63(1.78-3.89) | 2.18(1.54-3.1) |
| Tensed because of parental fights | 2.42(1.51-3.86) | 2.97(2-4.42) |
| Worried because you are unable to open up with your parents | 4.45(2.87-6.89) | 3.65(2.54-5.25) |
| Disturbed because of uncertainty in reopening of college | 2.76(1.72-4.42) | 3.24(1.95-5.37) |
| Concerned because of the loss of studies in the lockdown | 2.21(1.38-3.54) | 2.19(1.36-3.51) |
| Worried because of upcoming course burden | 3.33(1.87-5.9) | 4.52(2.28-8.99) |
| Worried because of upcoming uncertainty of exams | 2.05(1.19-3.52) | 4.56(2.14-8.62) |
| Burdened because of daily online classes | 2.15(1.46-3.16) | 2.56(1.79-3.68) |
| Uneasy because of sitting in front of a desktop for longer periods | 2.4(1.57-3.67) | 2.81(1.83-4.33) |
| Concerned because your social life is affected by the lockdown | 2.61(1.74-3.89) | 2.35(1.6-3.47) |
| Worried because you are unable to handle your relationship | 2.24(1.43-3.5) | 2.83(1.92-4.15) |
| Do you have mood swings | 3.77(2.43-5.86) | 5.14(3.12-8.47) |
| Worried about your future | 3.88(2.27-6.64) | 5.21(2.71-10.02) |
| Those who remained alone & introvert | 2.04 (1.33-3.11) | 1.87 (1.3-2.7) |
| Change in Food Habits (Yes) | 1.96(1.3-2.96) | 1.81(1.21-2.69) |
| Substance Use (Yes) | 1.5(1.01-2.21) | 1.53(1.08-2.17) |
| Parameter | Anxiety Absent OR (95% CI) | Stress Absent OR (95% CI) |
|---|---|---|
| Students who opened up to parents | 4.45 (2.87-6.89) | 3.65 (2.54-5.25) |
| Students who felt relaxed after talking with Teacher/Mentor: | 2.87 (1.94 - 4.24) | 2.14 (1.5-3.05) |
| Families with less Parental Fights | 2.42 (1.51-3.86) | 2.97 (2-4.42) |
| Students who shared talks with family members | 1.94 (1.31-2.86) | 1.47 (1.02-2.13) |
| Students who cooked New Recipe | 1.56 (1.05-2.33) | 1.45 (0.99-2.11)* |
| Students who Chit Chatted with friends | 1.3 (0.89 - 1.89)* | 1.8 (1.28-2.55) |
Factors like age, gender, year of study, course of study, socioeconomic status, and place of living were not the predictors of anxiety and stress in this sample, as reported in many other studies [13, 26, 31, 33]. The risk factors which had an association with the presence of anxiety and stress in this study were apprehension about attending COVID-19 patients, uncertainties of the course burden and examination, financial aspects, family issues, long-term confinement, poor handling of relationships, and lack of regular outdoor games. Different studies have reported similar results as of our study [22, 31, 34, 35].
In this study, students who used substance abuse as a coping mechanism had higher prevalence and higher scores for anxiety, depression and stress compared to the students who had conversations with their family members. Substance abuse is a very common unhealthy coping mechanism that may lead to addiction and exacerbate mental health issues [36, 37]. Support-seeking behavior is a healthier coping mechanism that has a beneficial effect on mental health during stressful situations [38].
5. LIMITATIONS
There are a few limitations in this study. Firstly, the sleep quality of the students has not been considered. Secondly, it is a cross-sectional survey, so the level of psychological impact in different time frames of the lockdown has not been considered. Thirdly, the sample size is less compared to an expected nation-wide survey. However, in this study, the study participants were from different parts of the country, undergoing different healthcare related courses from both government and private colleges (Tables 6 and 7).
CONCLUSION
The prevalence of anxiety, stress and depression in healthcare students from our country was very high. Most of the students needed motivation during the pandemic lockdown. Familial disharmony, financial issues, long duration of online classes, long-term confinement, and fear of infection acquisition by family members were few risk factors for the detrimental mental health status. Most of the students needed motivation during that period. Opening up with mentors/ faculty members, friends and parents was the protective factor for a good psychological state. Proper psychological support from family, friends and teachers is a necessity for students of health care services in such crisis situations in the future. This study is one of its kind, which describes the psychosocial risk factors influencing the common mental health problems among Indian students of health care services during a global health crisis.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus Disease 2019 |
| DASS21 | = Depression, Anxiety and Stress Scale |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Institutional Ethics Committee of KIMS, KIIT University, Bhubaneswar, Odisha, India. Approval Number (KIIT/ KIMS/ IEC/ 368/ 2020 dated 24.08.2020).
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study. The Helsinki Declaration has been followed while conducting research on human subjects in this study.
CONSENT FOR PUBLICATION
Written informed consent has been taken from all the participants for this study.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available in the article. The raw data is available with the corresponding author, [M.M], which can be retrieved on special request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


