The Effect of Inhalation Aromatherapy with Lemon Balm (Melissa officinalis) Essential Oil on Sleep Quality in Mothers of Preterm Infants in the Neonatal Intensive Care Unit (A Randomized Clinical Trial Study)
Abstract
Aim
The present study was to investigate the effect of inhalation aromatherapy with the lemon balm (Melissa officinalis) essential oil on sleep quality in the mothers of preterm infants admitted to the neonatal intensive care unit (NICU).
Background
Preterm infants and their hospital care are among the stressful events encountered by mothers. As maternal sleep disturbances are one of the frequent disorders at this stage, developing some measures to support mothers has been high on the list.
Methods
This two-group randomized clinical trial (RCT) was conducted on 50 mothers of preterm infants at the 28-32 weeks of pregnancy, completing the Pittsburgh Sleep Quality Index (PSQI) as the data collection tool. The study samples were initially randomized into two groups, viz., intervention and control. Afterward, the mothers in the intervention group received inhalation aromatherapy with the lemon balm essential oil by 5-7 drops on their face masks twice a day for two weeks. Then, sleep quantity and quality were assessed during the one- and two-week intervals following the intervention. The data were further analyzed using descriptive and inferential statistics.
Results
In total, 50 mothers of preterm infants were investigated in this study. The overall score of sleep quality in the mothers in the intervention group within the one- and two-week intervals at the post-intervention stage indicated a significant decrease, as compared with those in the controls (p<0.001). Moreover, the overall score of sleep quality for two weeks after the intervention compared with the one-week interval significantly dropped in the intervention group, as compared with the control one (p<0.001).
Conclusion
It was concluded that inhalation aromatherapy with lemon balm essential oil as a complementary medicine could be effective in improving sleep quality in mothers of preterm infants.
1. INTRODUCTION
Preterm birth means the live birth delivered before the completion of the 37 weeks of pregnancy, typically characterized by the gestational age as extremely preterm for not more than 28 weeks, very preterm for 28 to less than 32 weeks, and moderate-to-late preterm for 32 to under 37 weeks [1]. As a global problem, Iran is also one of the countries facing a high prevalence rate of preterm birth [2], with an upward trend of 30% over the past 25 years [3]. Corresponding to the statistics reported by the Ministry of Health and Medical Education within the Iranian government, roughly 1,200,000 infants are born each year, and 7% of such cases are registered as preterm ones [4, 5]. Additionally, the highest rate of admissions to neonatal intensive care units (NICUs) is typically associated with preterm birth [6]. Unquestionably, the parents of preterm infants are almost always in need of much more support [7], so postpartum healthcare services are of utmost importance, and any failure in this respect gives rise to many severe physical and mental complications [8, 9]. Such parents, mostly mothers, are thus subjected to higher levels of stress than those of full-term infants [10], because such mothers must attempt to be in accord with the demanding intensive healthcare services for these infants [11]. As about 28-70% of mothers with preterm infants live through high levels of mental stress [12], developing some measures to support them during hospital care for their infants in the NICU seems to be vital [11]. All through this stressful event, the bulk of mothers are exposed to painful experiences, including some changes in their sleep patterns [13].
Sleep, one of the bare necessities for human survival, has been described as the time to let the body and brain repair and restore, and even reenergize the spiritual, mental, and physical abilities [13, 14]. Disrupted sleep patterns in mothers are thus accompanied by some unpleasant consequences, such as cessation of breastfeeding and reduction in mother-infant attachment. Without enough sleep, the ability to concentrate, judge, and perform daily activities further diminishes, and irritability redoubles. For the postpartum period, mothers are also drawn against numerous sleep disorders, sleep deprivation, and lots of fluctuations in their sleep patterns [13], attributable to some physical changes after childbirth along with hormonal changes, including low levels of progesterone and melatonin, as one of the most striking features of the first year after childbirth. Even though such disorders occur for all, they drastically impact maternal health and functioning. Disturbed sleep patterns and reduced sleep quality after childbirth may thus remain invariable for several weeks or months, and their persistence is likely to bring about countless problems [15, 16].
Thanks to their non-invasiveness, fewer side effects, and popularity, the application of complementary and herbal medicine has drawn much attention among people and scholars [17]. In this vein, a variety of practices, such as music therapy, therapeutic touch, aromatherapy, relaxation techniques, yoga, acupuncture, and the use of medicinal plants, have been advocated as effective methods to handle sleep disturbances [14], although some might have their own limitations. For example, not all patients can play all sports or attend yoga sessions. In the meantime, inhalation aromatherapy has been recognized as an alternative with fewer restrictions and higher practicality [7]. In this technique, oils and essential oils are typically utilized to improve health status and cure some diseases. The general rule here is that once an aromatic plant scent is inhaled, its molecules travel across the olfactory system, and then transferred to the limbic system, wherein an emotional response is given to the stimulation created in this line [18]. Among innumerable aromatic plants, lemon balm (Melissa officinalis), belonging to the mint family, has been widely exploited in traditional medicine, tracing back to over 2000 years ago. This medicinal perennial has been thus investigated in numerous studies for its therapeutic benefits [18, 19]. It is native to the eastern and western Mediterranean region of Asia and distinguished in Iran, being extensively cultivated in Tehran, Golestan, West Azerbaijan, Lorestan, and Kermanshah provinces, whose fresh or dried leaves are typically used for medicinal purposes [8]. This aromatic plant is applied in different forms, i.e., essential oil, sweat, ointment, and powder, which have their own sedative-anxiolytic properties [10]. Relieving stress, inducing sleep, and improving mood [20, 21], anxiety, and depression [22, 23] have been accordingly reported as the positive effects of this medicinal plant. In addition, aromatherapy with lemon balm may be applicable in mild depression, as highly recommended by Ibn Sina, a preeminent philosopher and physician of the Muslim world in Iran [1]. Lemon balm can be stored for a very long time with no side effects reported to date [11]. Of note, one technique to prepare the essential oil of medicinal plants is water distillation via a Clevenger apparatus, as a simple, ancient method. Thus, the highest amount of essential oil extracted from lemon balm is typically obtained by this method, in which the desired plant is directly placed in a distillation flask inside water, and then about two-thirds of its volume is filled with water, and heated. The produced water vapors contain essential molecules, which are liquefied after traveling through refrigerant pipes, and collected in the receiving container [24, 25].
Since aromatherapy in the postpartum period has been reported to be effective in improving the physical and mental condition and facilitating the interaction of mothers and babies [26] and sleep quality [12] and considering the fact that every year, a large number of premature babies in the first days need to be hospitalized in the neonatal ward. Furthermore, this issue separates the mother and the baby from each other and affects their quality of life, because problems related to insomnia are common problems of women in the post-partum period and these problems are felt more strongly in mothers with premature babies, therefore, due to the lack of similar research in Iran, it seems that a study should be conducted with the aim of the effect of inhalation aromatherapy with the lemon balm (Melissa officinalis) essential oil on sleep quality in the mothers of preterm infants admitted to the neonatal intensive care unit (NICU).
2. MATERIALS AND METHODS
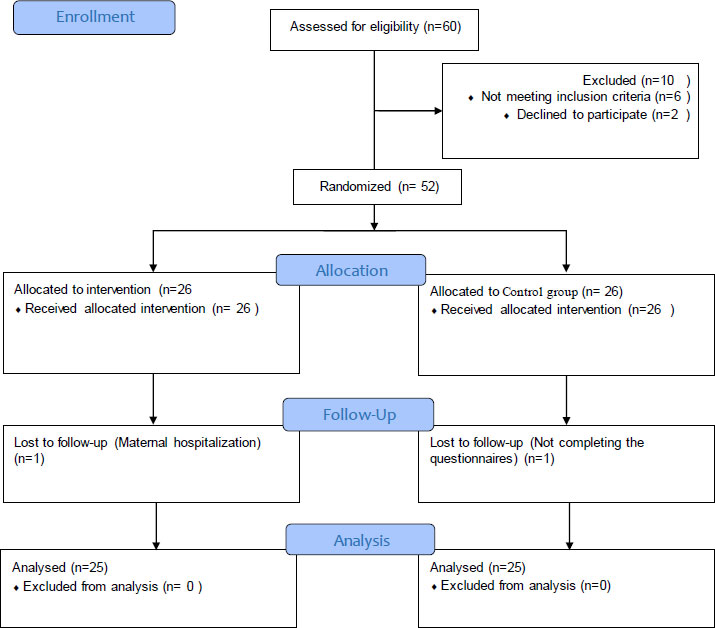
This two-group randomized clinical trial (RCT) was conducted on the mothers of preterm infants hospitalized at Imam Reza Hospital and Umm Al-Banin Hospital, and teaching medical centers affiliated to Mashhad University of Medical Sciences, Mashhad, Iran. Using G* Power 3.1.92, and considering the effect size (0. 86) Dehghan et al. 2023 [25] determined the error level (5%), the power (80%) the attrition rate (20%), and the size (intervention = 25 and control = 25). At the beginning of sampling, 60 mothers were invited to the study, 6 people were not eligible to enter the study, and two mothers did not complete the consent form. During the research, a mother was admitted to the women's department in the intervention group. In the control group, one mother did not complete the forms at the end of the study and was excluded from the study. A flow diagram describing mother selection is shown in Fig. (1).
In the control group, one mother did not complete the forms at the end and was excluded from the study. The inclusion criteria were signing informed consent forms by the mothers for their inclusion in the intervention, being at the 28-32 weeks of pregnancy, suffering from no chronic physical and mental illnesses, olfactory disorders, allergies, cold, and low sleep quality (endorsed by the Pittsburgh Sleep Quality Index (PSQI) that with examining
seven components of sleep, and the questions related to examining each component are scored from 0 to 3 and finally based on 0-21 Obtaining a total score in the total range It is judged that a total score of 5 or more indicates inadequate sleep quality), having access to phones for making calls, as well as taking no sedative and hypnotic drugs. On the other hand, the exclusion criteria were unwillingness to continue the trial for any reason, infant death, and during the intervention, the neonatal should be discharged from the hospital with personal consent. Accordingly, the mothers terminating their pregnancy at the 28-32 weeks of pregnancy, with infants admitted to the NICU, were selected for the initial interview using the hospitalized infant file. The interview was conducted during the first 48 hours of the mother’s presence in the NICU in terms of meeting the inclusion criteria, according to the sample selection form. Once ensuring that the conditions were met, the informed consent was taken. The mothers were also checked for their depression using the Edinburgh Postnatal Depression Scale (EPDS). After obtaining a score indicating no depression (a score less than 13), the mothers were placed in the intervention or control groups by selecting them as members of the statistical population and using drawing for their random assignment.
The randomized blocking approach was used to divide the mothers into two groups. This study involved two arms: A: intervention, Group B: control. Quadruple blocks were established and numbered accordingly: AABB (1), ABAB (2), ABBA (3), and BBAA (4). Randomization was then conducted using the random number table method via the website http//www.graphpad.com/quickcalcs/index .cfm. Numbers between 1 and 4 were generated (e.g., 1, 4, 3, and so on). Subsequently, the arms allocation list was determined based on the previously generated random numbers (BABAAA BBBBAA--...), continuing until the desired sample size of 52 participants was reached for each arm.
The mothers’ information was further evaluated based on the demographic characteristics form. In this study, the lemon balm essential oil was prepared by water distillation via a Clevenger apparatus as a simple, ancient method. For this purpose, the desired plant was directly placed in the distillation flask inside water, and then about two-thirds of its volume was filled with water and heated. The produced water vapors comprised of the essential oil molecules, which were liquefied after passing through refrigerant pipes, and collected in the receiving container. The essential oil obtained was further augmented to 5.1% with olive oil as the base. Afterward, 5-7 drops of this product were poured on a face mask, and the mothers in the intervention group were asked to wear it twice a day for 20-30 minutes each time and inhale the scent. Notably, the control group received no intervention. Once again, sleep quality in mothers from both study groups was assessed at the end of the first and the second weeks after the initial interview. To monitor the implementation of this procedure, the researcher made daily phone calls or had face-to-face meetings with the study samples. Although no side effects had been already cited in previous research for the lemon balm essential oil, the samples were followed up in order to reduce the possible complications.
The PSQI, a standardized self-rated questionnaire, was administered as the data collection tool in this study, whose reliability had been previously confirmed in numerous studies and implemented by Lee et al. [26]. The reliability of the Iranian version of this questionnaire was also measured via the test-retest reliability by 88%, and its content validity was reviewed and established by Peyvandi et al. [6]. To check the internal consistency of the PSQI, its internal correlation coefficient was recalculated in this study with Cronbach’s alpha coefficient of 84%. The questionnaire could thus help assess sleep quality based on seven components, including changes in sleep quality (item 9), sleep latency (the sum of item 2 and the first part of item 5), sleep duration (item 4), sleep efficiency (some percentages of items 1, 3, and 4), sleep disturbance (the sum of items in line five), daytime dysfunction due to sleepiness (the sum of items 7 and 8), and overall sleep quality, where the items related to each part could be scored from 0 to 3, and judged from 0-21 with reference to the overall score, viz., 5 or so, representing low sleep quality. In this part, the demographic characteristics of the study samples were also compared in both groups, and the homogeneity of these variables was examined. First, the normality of the quantitative variables was established using the Shapiro-Wilk test. Furthermore, the independent-samples t-test was applied to compare both study groups in respect of normal quantitative variables, and the Mann-Whitney U test was utilized for the non-normal and rank ones. Furthermore, the nominal variables were compared in both groups using the Chi-square test and the Fisher’s exact test. The main variable, i.e., sleep quality, was compared in the study samples in the intervention and control groups, namely, the comparison between the pre-intervention stage, one week later, and two weeks after the intervention. For the intragroup comparisons of the three stages, namely, before, one week later, and two weeks after the intervention, the repeated measures analysis of variance (ANOVA) was employed to find the normal variables, and the Friedman test was exploited for the non-normal ones. All statistical analyses were completed at the significance level of 95%.
3. RESULTS
The data taken from 50 mothers of preterm infants in the NICU were analyzed in this study. Maternal age, gestational age, EPDS score, birth weight, birth length, infant head circumference, and the one- and five-minute Apgar scores were also found to be homogeneous in both intervention and control groups (p>0.05). The demographic characteristics of the study samples are illustrated in Table 1.
The overall sleep quality for the initial interview with the mothers in the intervention group was 6.8±2.4, and that was 8.7±2.8 in the controls (p=0.007). These values within the one-week interval after the intervention were equal to 3.0±1.4 and 8.5±3.1 in the intervention and control groups, respectively (p<0.001). The overall sleep quality, two weeks after the intervention completion, was also 1.2±0.6 in the intervention group and 8.5±0.3 in the control one (p<0.001). As well, the overall sleep quality during the one-week interval after the intervention dropped by -3.8±1.8 and -0.2±2.4 in the intervention and control groups, respectively, as compared with those at the pre-intervention stage (p<0.001). Moreover, these values decreased by -5.6±2.0 in the intervention group and -0.2±2.8 in the controls two weeks after the intervention, as compared with those before the intervention (p<0.001). The overall score of sleep quality within the two-week interval after the intervention compared with the one-week interval accordingly diminished by -1.8±1.1 in the intervention group and -0.0±1.5 in the control one (p<0.001) (Table 2).
The study results revealed a statistically significant difference in the intervention group at three stages, viz., before, one week later, and two weeks after the intervention. The changes in the overall score of sleep quality in the intervention group at the pre-intervention stage, one week later, and two weeks after the intervention were also significant (p<0.001). The repeated measures ANOVA outcomes further showed that the variations in the overall score of sleep quality during the pre-intervention stage, one week later and two weeks after the intervention, were not significant in the control group (p=0.786) (Table 3).
| Variables | Intervention Group | Control Group | Test Results |
|---|---|---|---|
| Mean±Standard Deviation | Mean±Standard Deviation | ||
| Maternal age (year) | 28.4±6.3 | 29.0±5.6 | t=-0.3, df=48, p=0.741 Independent-samples t- test |
| Gestational age (week) | 29.3±1.3 | 30.1±1.4 | Z=-2.0, p=0.091 Mann-Whitney U test |
| EPDS score | 8.5±2.9 | 7.8±3.6 | t=0.8, df=48, p=0.417 Independent-samples t- test |
| Birth weight (g) | 1188.24±239.743 | 1287.75±245.57 | t=-1.369, df=39, p=0.178 Independent-samples t- test |
| Birth length (cm) | 36.0±4.52 | 37.52±4.35 | Z=-1.111, p=0.273 Mann-Whitney U test |
| Infant head circumference (cm) | 27.30±2.26 | 27.60±2.20 | t=-0.347, df=48, p=0.730 Independent-samples t- test |
| One-minute Apgar score | 5.70±1.6 | 6.5±1.5 | Z=-2.1, p>0.05 Mann-Whitney U test |
| Five-minute Apgar score | 7.7±1.1 | 8.1±1.0 | Z=-1.2, p=0.219 Mann-Whitney U test |
| Intervention Group | Control Group | Intergroup Test Results | |
|---|---|---|---|
| Mean±Standard Deviation | Mean±Standard Deviation | ||
| Initial interview | 6.8±2.4 | 8.7±2.8 | Z=-5.7 p<0.001 Mann-Whitney U test |
| One week after intervention | 3.0±1.4 | 8.5±3.1 | Z=-6.3 p<0.001 Mann-Whitney U test |
| Two weeks after intervention | 1.2±0.6 | 8.5±3.0 | Z=-5.1 p<0.001 Mann-Whitney U test |
| Difference between the one-week interval and pre-intervention stage | -3.8±1.8 | -0.2±2.4 | Z=-5.8 p<0.001 Mann-Whitney U test |
| Difference between the two-week interval and pre-intervention stage | -5.6±2.0 | -0.2±2.8 | Z=-4.2 p<0.001 Mann-Whitney U test |
| Difference between two-week interval and one-week interval after intervention | -1.8±1.1 | -0.0±1.5 | Z=-1.111 p=0.273 Mann-Whitney U test |
| Intragroup test results | Chi-square=48.6 df=2 p<0.001 Friedman test |
F=0.1 df=2.48 p=0.786 Repeated measures ANOVA |
| Sleep Components | Groups | Before Intervention | One Week After the Intervention | Two Weeks After the Intervention | Intragroup p-value* |
Intergroup p-value** |
|---|---|---|---|---|---|---|
| Changes in sleep quality | Intervention | 1.4±0.6 | 0.9±0.4 | 0.1±0.3 | p<0.001 | p<0.001 |
| Control | 1.5±0.8 | 1.4±0.9 | 1.5±0.9 | p=0.751 | ||
| Sleep latency | Intervention | 1.7±0.9 | 0.4±0.6 | 0.1±0.3 | p<0.001 | p<0.001 |
| Control | 2.0±1.1 | 1.6±0.9 | 1.5±0.9 | p=0.015 | ||
| Sleep duration | Intervention | 0.7±0.9 | 0.9±0.6 | 1.0±0.4 | p=0.056 | p=0.728 |
| Control | 1.3±1.0 | 1.6±0.8 | 1.7±0.7 | p=0.086 | ||
| Sleep efficiency | Intervention | 0.5±0.7 | 0.1±0.3 | 0.0±0.0 | p<0.001 | p=0.40 |
| Control | 0.9±0.8 | 0.7±0.9 | 0.9±0.9 | p=0.139 | ||
| Sleep disturbance | Intervention | 1.3±0.5 | 0.3±0.5 | 0.0±0.0 | p<0.001 | p<0.001 |
| Control | 1.7±0.9 | 1.6±0.9 | 1.5±0.7 | p=0.416 | ||
| Daytime dysfunction due to sleepiness | Intervention | 1.2±0.7 | 0.4±0.5 | 0.0±0.0 | p<0.001 | p<0.001 |
| Control | 1.4±0.9 | 1.5±0.9 | 1.3±0.8 | p=0.465 | ||
| Overall score of sleep quality | Intervention | 6.8±2.4 | 3.0±1.4 | 1.2±0.6 | p<0.001 | p<0.001 |
| Control | 8.7±2.8 | 8.5±3.1 | 8.5±3.0 | p=0.786 |
4. DISCUSSION
The effect of inhalation aromatherapy with the lemon balm essential oil on sleep quality in the mothers of preterm infants was investigated in this study in two intervention and control groups, 25 people in each one, for two weeks. Seven components were correspondingly assessed using the PSQI. With regard to the changes in sleep quality, there were improvements in the intervention group at the end of the first and second weeks following the intervention completion, while no variation was observed in the controls. For sleep latency, the intervention group also experienced an increase at both assessment stages, but a slight improvement was seen in the control group, which was not predictable on account of the mothers’ fatigue while taking care of their preterm infants. Sleep duration in both groups was slightly lower at the end of the first and second weeks due to the continuous care of their preterm infants during hospitalization. This upgraded the mothers in the intervention group at the end of the first and second weeks, while no change was spotted in the controls. The mean±standard deviation of sleep disturbance in the mothers of the intervention group also reduced at the end of both assessment stages, but there was a slight change in the control group at the end of the one- and two-week intervals after the intervention. In terms of daytime dysfunction due to sleepiness, the mothers in the intervention group showed much better improvement within the one- and two-week intervals after the intervention, while no significant change was observed in the control group. The overall score of sleep quality further dwindled one week after the intervention in the mothers in the intervention group, but there was no decrease in the controls. Two weeks after the intervention, sleep quality in the mothers in the intervention group improved, but there was no difference in the controls. In general, the results showed that inhalation aromatherapy with the lemon balm essential oil boosted overall sleep quality in the study samples. According to Farag and Mills (2003), investigating the effect of combined valerian and lemon balm supplements on insomnia in the United States, sleep latency had lessened, and sleep duration had elevated [27], which were in line with the results in the present study in terms of sleep latency, but not for sleep duration. Cerny and Schmid (1999), in their investigation in Switzerland, also reflected on the efficacy and tolerability of oral valerian supplemented with lemon balm on mild sleep disorders in healthy people and concluded that sleep quality had improved by taking the desired capsules [28], which was consistent with the study results with regard to improvements in sleep disturbance and overall sleep quality. Additionally, Julien et al., in their study at Martino Hospital in Geneva, Italy, examined the effect of lemon balm on the treatment of mild-to-moderate anxiety disorder and sleep disturbance in women and men aged 18-70 and concluded that lemon balm could reduce sleep disorders by 42% and insomnia by 35% [29], which were in agreement with the results of the present study. Likewise, Chen et al. (2015) explored the effectiveness of lavender tea on maternal sleep quality after preterm birth in Taiwan, showing that the participants in the intervention group had reached better sleep quality as compared with the controls [8], which was consistent with the present study considering the same statistical populations. In this vein, Lee et al. (2004) evaluated the effects of inhalation aromatherapy with eucalyptus and lavender essential oils on sleep quality in 51 mothers, using post-tests on the sixth and 60 days after childbirth. The study findings did not establish any significant difference between the mean sleep duration and the mean number of awakenings before the intervention. Following the intervention, no significant difference had been also reported between sleep duration, number of awakenings, and satisfaction with sleep quality in both groups. Despite the application of inhalation aromatherapy for mothers after childbirth, this technique could have no effect on sleep quality in the long term [30], which was in conflict with the present study, measured in the short term with a positive effect.
CONCLUSION
The study results were close to those confirming the effect of inhalation aromatherapy with lemon balm essential oil; however, it is suggested to investigate its effect as combined with other supplements in the long term and even in the oral form. The effect of spraying this essential oil in the mother’s room should also be investigated in further research.
LIST OF ABBREVIATIONS
| RCT | = Randomized Clinical Trial |
| PSQI | = Pittsburgh Sleep Quality Index |
| EPDS | = Edinburgh Postnatal Depression Scale |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was part of the thesis approved by Mashhad University of Medical Sciences, Mashhad, Iran, with contract code no. 951450 and the project code no. IRCT2017012532190N1, archived in the Iranian Registry of Clinical Trials (IRCT) and the Research Project Archives of the School of Nursing and Midwifery affiliated with Mashhad University of Medical Sciences, Mashhad, Iran.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
In terms of ethical considerations, the present study was ethical in two respects: first, all the participants volunteered to participate in the study, and secondly, keeping in mind the principles of confidentiality and secrecy, participants were assured that all information would remain confidential and that the results would be reported in a general manner.
STANDARDS OF REPORTING
CONSORT guidelines have been followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author [T.S] upon reasonable request.
FUNDING
This research was done with the financial support of Mashhad University of Medical Sciences.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors hereby would like to extend their sincere gratitude to the Vice-Chancellor’s Office for Research at Mashhad University of Medical Sciences, Mashhad, Iran, the respected personnel of Imam Reza Hospital and Umm al-Banin Hospital in the city of Mashhad, Iran, as well as all mothers who kindly contributed to this research.


