All published articles of this journal are available on ScienceDirect.
An Evaluation of The Syphilis Screening Program Among Pregnant Women In Gaborone Clinics, Botswana: A Five Year Retrospective Analysis
Abstract
Background:
Syphilis in pregnancy is a public health problem mainly in developing countries. If untreated, it can lead to pregnancy and fetal complications. Nation-wide screening at antenatal care is an important intervention for early detection and treatment to prevent complications.
Objective:
The aim was to evaluate the proportions and trends in the syphilis screening program of pregnant women who were attending the 15 public health care facilities in Gaborone Botswana during the period 2004 and 2008.
Method:
We conducted a cross-sectional study in the antenatal care facilities in Gaborone. Data was obtained from the antenatal registers from 7th to 25th September 2009 using a structured data collection sheet. We recorded the number of pregnant women registered for antenatal care, those screened and those not screened for syphilis. The SPSS 14.0 for windows software was used for data analysis.
Results:
The overall trends in the proportions of pregnant women screened for syphilis from 2004 to 2005 increased from 87.2% (95% CI, 86.4-88.0) to 89.7% (95% CI, 89.0-90.4), compared to the 2005 to 2006 estimates that showed a declined from 89.7% (95% CI, 89.0-90.4) to 79.0% (95% CI, 77.9-80.1). Seventy five percent of the clinics showed rising trends in the proportions of pregnant women screened for syphilis from 2004-2008.
Conclusion:
There were marked variations in the trends among pregnant women screened and those not screened for syphilis in the clinics around Gaborone. The overall trend was an increase screening coverage in the years 2004-2008. There is a need to investigate the factors associated with these variations.
1. INTRODUCTION
Syphilis is a sexually transmitted infection caused by the spirochete Treponema palladium, and is considered a serious public health challenge if left untreated. In pregnancy, this major public health problem is preventable and treatable, to the benefit of especially the resource constrained countries [1]. Untreated active syphilis infection causes adverse outcomes in 50-80% of pregnancies surviving past 12 weeks gestation. In order to avert these adverse outcomes, routine antenatal screening and penicillin treatment for this infection are highly recommended as part of the comprehensive antenatal care [2, 3].
Syphilis screening involves collection of blood sample for serological tests, for diagnosis and monitoring of response to treatment. There are two types of serological tests for syphilis, viz non-treponemal or reagin tests and treponemal antibody tests. The non-treponemal tests (RPR, VDRL) are non-specific as they measure the reagin (mixture of IgG and IgM) in the patient’s serum. They are relatively accurate, can be titrated and quantified. It needs to be noted that high reactivity titers in non-treponemal serological tests usually indicate early active infection [2]. In theory, titer values of less than 1:8 obtained in non-treponemal tests should be confirmed with a specific treponemal test – especially in communities with low rates of syphilis (RPR positivity rates ˂ 5%) [2].
The treponemal antibody tests are specific serological tests for syphilis infection, e.g. Fluorescent treponemal antibody-absorption (FTA-ABS) test, Treponema pallidum hemagglutination assay (TPHA), Treponema pallidum ELISA test (TP-ELISA). They are of little importance in monitoring responses to therapy since they remain positive for life, even after successful treatment intervention [2].
The FTA-ABS test is usually positive in approximately three weeks following the infection as opposed to non-treponemal tests and TPHA which become positive in about six weeks following the infection. Consequently, the FTA-ABS test has traditionally been used to detect early syphilitic infection with a high sensitivity (85-100%) in all stages of the disease, while TPHA test is used to detect later stages of the infection [3].
In sub-Saharan Africa, a review of national antenatal screening programs showed that 17 out of 22 countries in the continent incorporate syphilis screening as part of the routine antenatal care, of which, only 38% of pregnant women were actually screened [1]. A study in Tanzania, demonstrated that out of 2256 pregnant women eligible for syphilis screening over 4 months, only 970 (43%) were documented to have had an RPR test, among them144 (15%) were sero-reactive [4]. In the same country, a retrospective cohort study showed that 16.8% of 22,180 pregnant women attending antenatal clinics had not been screened for syphilis at the time of delivery. However, 1809 out of 3724 (16.8%) were later screened at the delivery; among them, 144 (8.0%) tested RPR positive [5].
In 2004-2005, 71 (13%) of 546 women coming for a repeat antenatal care visit in Botswana had not been screened for syphilis [6]. The national guidelines of Botswana stipulate that screening for syphilis with non-treponemal tests such as VDRL or RPR is mandatory in the first and third trimesters of pregnancy. The decision to adopt this guideline was informed by the findings of 2007 Botswana sentinel surveillance that showed high syphilis prevalence by districts in the range from 0.4% to 16.7%, but more commonly above 3.0% among antenatal attendees [7]. Non-treponemal tests are 60-90% sensitive for the diagnosis of primary, latent and late syphilis, but almost 100% sensitive for secondary syphilis [2].
The aim of the study was to evaluate the syphilis screening program amongst registered pregnant women attending public antenatal clinics by determining the trends in the overall proportion of pregnant women screened and those not screened for syphilis, as well as trends by facilitating the proportion of pregnant women screened and not screened for syphilis from 15 public primary care facilities in Gaborone, Botswana.
1.1. Significance of the Study
An overview of literature shows paucity of information on proportions of pregnant women screened and not screened for syphilis amongst antenatal clinics attendees in Gaborone, Botswana. Most studies reviewed did not yield data on exploration of proportions of registered pregnant women not screened for syphilis, because this category of women is not routinely used to monitor the antenatal syphilis screening program. It is hoped that information generated from this study would be helpful to inform national health policies and strategies to further strengthen the antenatal syphilis screening program in Gaborone, Botswana.
1.2. Ethical Considerations
Approval for this study was obtained from the University of Liverpool and the Ministry of Health, Botswana (PPME 13/18/1 PSIV {50}). Permission to collect data from the district was obtained from the District Health Team (DHT) of the Gaborone City Council, Botswana. The approved data collection sheet was based on the study objectives and all details linking the data to any patient were removed.
2. MATERIALS AND METHODOLOGY
2.1. Study Design
This was a descriptive cross-sectional study based on antenatal care records of pregnant women screened and not screened for syphilis in 15 clinics in Gaborone Botswana from 2004-2008.
2.2. Study Setting
This study was conducted in all the 15 public antenatal care facilities in Gaborone, Botswana. All the facilities providing routine antenatal care were included in order to attain a representative sample of each study site. The sites were coded as follows-BH1, BH2, BH3, Block 6, Block 8, Block 9, Bontleng, BTA, Extension 2, Extension 14, Extension 15, Sebele, Phase 2, ONC and G-west. We later excluded G-west from the study site as we could not access the clinic antenatal register.
All the study sites also offer undifferentiated primary care services irrespective of age, gender and socioeconomic background to the people of Gaborone and its surrounding communities. The practice profile encompasses preventative, promotive, curative and rehabilitative health care delivery.
2.3. Data Source & Data Collection
We sourced data directly from the antenatal register of each study site and data collection was from 7th to 25th September 2009 using a structured data collection sheet approved by the research and ethics committee of the Ministry of Health, Botswana. The study sites were visited in turns for data collection. The following variables were extracted from the antenatal register of each clinic - number of pregnant women registered for antenatal care, number of pregnant women screened and those not screened for syphilis per year from 2004-2008.
2.4. Reliability and Validity
The uniformity of the recording keeping systems of the recorded data was checked to ensure its validity. This was done through comparing the data collected from the antenatal registers at each clinic site with that of central statistics office at District Health Team to detect any disparities. Reliability was ensured by consistently using the approved data capture sheet throughout the data collection process. We consistently used the clinic code for each study site to prevent cross-transposition of data among the study sites and to enable data checking. Data were extracted from the antenatal registers of each clinic and thereafter double entered manually by two trained data clerks into the approved data sheet and the two sheets were compared by the researchers in order to rectify any disparity.
2.5. Data Analysis
Information collected on the data capture sheet was summarized per year and by clinic, 2004-2008. For ease of data analysis we produced a table. The full dataset were entered, edited and cleaned using SPSS 14.0 for windows software, then exported to Microsoft Excel for statistical analysis. All variables used in our study were categorical data and descriptive statistics were used. Descriptive statistics were obtained from baseline frequency tables created in a Microsoft Excel spreadsheet. The overall trend and trends by clinic in the proportions of registered pregnant women screened and those not screened for syphilis per year were calculated. Specifically, proportions screened were calculated as the total number of pregnant women screened for syphilis divided by the total number of pregnant women registered for antenatal care per year and by clinic per year for 2004-2008. Proportions not screened were calculated as the total number of pregnant women not screened for syphilis divided by the total number of pregnant women registered for antenatal care per year and by clinic per year for 2004-2008. To highlight the shortfall in the proportion of the pregnant women who were screened for syphilis, we projected the table depicting those who were not screened per health facility over the period of five years, 2004-2008. Finally, 95% confidence interval was determined for each proportion calculated.
3. RESULTS
3.1. Overall Trend in the Proportion of Registered Pregnant Women Screened and Not Screened for Syphilis
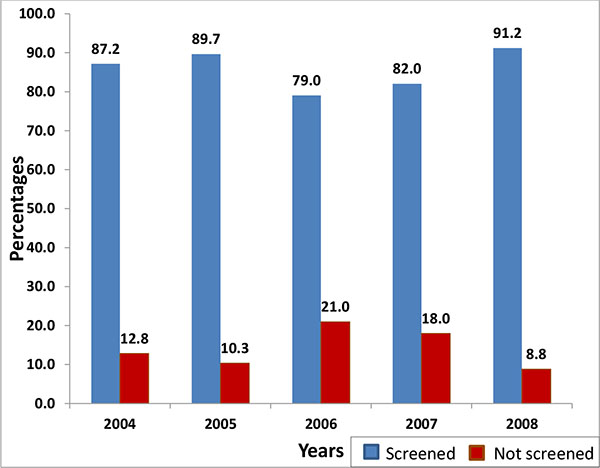
A total of 31,221 pregnant women registered for antenatal care over the five years period, of whom, 26,875 (86.1%; 95% CI, 85.7-86.5) and 4,346 (13.9%; 95% CI, 13.5-14.3) were screened and not screened for syphilis, respectively. Of the 6418 registered pregnant women in 2004, 5594 (87.2%; 95% CI, 86.4-88.0) were screened, which increased in 2005, to 5775 (89.7%; 95% CI, 89.0-90.4) out of 6442 registered pregnant women. In 2006, the proportion of registered pregnant women screened for syphilis reduced to 4490 (79.04%; 95% CI, 77.9-80.1), which increased again in 2007 and 2008 to 4903 (82.0%; 95% CI, 81.0-83.0) and 6113 (91.2%; 95% CI, 90.5-91.9), respectively. The fluctuations are demonstrated in Table 1 and Fig. (1) below.
| Year | Number registered for ANC | Number (proportion) screened for syphilis n (%; 95% CI) |
Number (proportion) not screened for syphilis n (%; 95% CI) |
|---|---|---|---|
| 2004 | 6418 | 5594 (87.2; 86.4-88.0) | 824 (12.8; 12.0-13.6) |
| 2005 | 6442 | 5775 (89.7; 89.0-90.4) | 667 (10.3; 9.6-11.0) |
| 2006 | 5681 | 4490 (79.0; 77.9-80.1) | 1191 (21.0; 19.9-22.1) |
| 2007 | 5977 | 4903 (82.0; 81.0-83.0) | 1074 (18.0; 17.0-19.0) |
| 2008 | 6703 | 6113 (91.2; 90.5-91.9) | 590 (8.8; 8.1-9.5) |
| Total | 31221 | 26875 (86.1; 85.7-86.5) | 4346 (13.9; 13.5-14.3) |
Of the 31, 221 pregnant women who registered for antenatal care (ANC) over the period of five years (2004-2008), 4, 346 (13.9%; 95% CI, 13.5-14.3) were not screened for syphilis.
3.2. Trend by Clinic the Proportion of Registered Pregnant Women Not Screened For Syphilis
There were different trends by health facility in the proportions of registered pregnant women not screened for syphilis. Only two clinics, BH 1 (except in 2005) and Phase 2 (except in 2006) demonstrates a gradual reduction in the proportions of pregnant women not screened for syphilis from 2004-2008. However, the rest of the clinics show marked variations in the proportions of registered pregnant women not screened for syphilis from 2004-2008 (Table 2).
| Year | 2004 | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|---|
| Clinic | Proportion not screened n (%; 95% CI) |
Proportion not screened n (%; 95% CI) |
Proportion not screened n (%; 95% CI) |
Proportion not screened n (%; 95% CI) |
Proportion not screened n (%; 95% CI) |
| BH 1 | 29/348 (8.3; 5.4-11.2) |
32/353 (9.1; 6.1-12.1) |
16/324 (4.9; 2.6-7.3) |
18/367 (4.9; 2.7-7.1) |
11/351 (3.1; 1.3-4.9) |
| BH 2 | 66/571 (11.6; 9.0-14.2) |
41/524 (7.8; 5.5-10.1) |
59/532 (11.1; 8.4-13.8) |
78/272 (28.7; 23.3-34.1) |
55/300 (18.3; 13.9-22.7) |
| BH 3 | 61/602 (10.1; 7.7-12.5) |
32/618 (5.2; 3.5-7.0) |
167/645 (25.9; 22.5-29.3) |
133/742 (17.9; 15.1-20.1) |
61/738 (8.3; 6.3-10.3) |
| Blk. 6 | 38/419 (9.1; 6.4-11.9) |
31/492 (6.3; 4.2-8.5) |
114/365 (31.2; 26.5-36.0) |
93/601 (15.5; 12.6-18.4) |
26/450 (5.8; 3.6-8.0) |
| Blk. 8 | 20/290 (6.9; 4.0-9.8) |
13/386 (3.4; 1.6-5.2) |
64/337 (19.0; 14.8-23.2) |
60/425 (14.1; 10.8-17.4) |
14/395 (3.5; 1.7-5.3) |
| Blk. 9 | 268/1097 (24.4; 21.9-26.9) |
206/872 (23.6; 20.8-26.4) |
254/755 (33.6; 30.2-37.0) |
215/777 (27.7; 24.6-30.9) |
135/1265 (10.7; 9.0-12.4) |
| Ext. 2 | 29/306 (9.5; 6.2-12.8) |
21/322 (6.5; 3.8-9.2) |
55/229 (24.0; 18.5-29.5) |
56/298 (18.8; 14.4-23.2) |
23/184 (12.5; 7.7-17.3) |
| Ext. 14 | 27/407 (6.6; 4.2-9.0) |
27/394 (6.9; 4.4-9.4) |
49/313 (15.7; 11.7-19.7) |
51/329 (15.5; 11.6-19.4) |
28/317 (8.8; 5.7-11.9) |
| Ext. 15 | 47/378 (12.4; 9.1-15.7) |
59/406 (14.5; 11.1-17.9) |
68/216 (31.5; 25.3-37.7) |
43/204 (21.1; 15.5-26.7) |
13/358 (3.6; 1.7-5.5) |
| Bontleng | 28/399 (7.0; 4.5-9.5) |
21/409 (5.1; 3.0-7.2) |
68/345 (19.7; 15.5-23.9) |
71/336 (21.1; 16.7-25.5) |
56/524 (10.7; 8.1-13.4) |
| ONC | 73/735 (9.9; 7.7-12.1) |
69/715 (9.7; 7.5-11.9) |
79/738 (10.7; 8.5-12.9) |
112/730 (15.3; 12.7-17.9) |
73/728 (10.0; 7.8-12-2) |
| Sebele | 24/83 (28.9; 19.2-38.7) |
08/123 (6.5; 2.1-10.9) |
25/117 (21.4; 14.0-28.8) |
14/107 (13.1; 6.7-19.5) |
07/112 (6.3; 1.8-10.8) |
| BTA | 47/453 (10.4; 7.6-13.2) |
39/477 (8.2; 5.7-10.7) |
82/376 (21.8; 17.6-26.0) |
75/453 (16.6; 13.2-20.0) |
44/479 (9.2; 6.6-11.8) |
| Phase 2 | 69/330 (20.9; 16.5-25.3) |
68/351 (19.4; 15.3-23.5) |
91/389 (23.4; 19.2-27.6) |
55/336 (16.4; 12.4-20.4) |
44/502 (8.8; 6.3-11.3) |
According to table II, in 2004, the proportion not screened for syphilis was highest amongst pregnant women from Sebele clinic 28.9% (95% CI, 19.2-38.7) than those from Block 9 clinic 24.4% (95% CI, 21.9-26.9) and lowest amongst pregnant women from Extension 14 clinic 6.6% (95% CI, 4.2-9.0). In 2005 and 2006, the proportion not screened for syphilis ranged from lowest 3.4% (95% CI, 1.6-5.2) in Block 8 clinic to highest 23.6% (95% CI, 20.8-26.4) in Block 9 and from lowest 4.9% (95% CI, 2.6-7.3) in BH 1 clinic to highest 33.6% (95% CI, 30.2-37.0) in Block 9 clinic respectively. The proportions not screened for syphilis ranged from 4.9% (95% CI, 2.7-7.1) in BH 1 clinic to 28.7% (95% CI, 23.3-34.1) in BH 2 clinic for 2007, in comparison with 2008 proportions that ranged from 3.1% (95% CI, 1.3-4.9) in BH 1 clinic to 18.3% (95% CI, 13.9-22.7) in BH 2 clinic. Therefore, it can be stated that almost all the clinics showed no trend in the proportions of pregnant women not screened for syphilis from 2004-2008.
Table 2 shows trends by health facility the proportion of pregnant women not screened for syphilis over the period of five years, 2004-2008. In 2006 and 2007, almost all the clinics (except BH 2, Bontleng and ONC clinics) recorded a decline in the proportion of pregnant women not screened for syphilis in comparison with previous years (2004 and 2005) and 2008.
3.3. Summary of the Study Findings
The overall trends in the proportions of pregnant women screened for syphilis from 2004 to 2005 increased from 87.2% (95% CI, 86.4-88.0) to 89.7% (95% CI, 89.0-90.4), when compared with the 2005 to 2006 estimates that showed a declined from 89.7% (95% CI, 89.0-90.4) to 79.0% 95% CI, 77.9-80.1). However, there was a significant inclined in the proportions of pregnant women screened for syphilis from 82.0% (95% CI, 81.0-83.0) in 2007 to 91.2% (95% CI, 90.5-91.9) in 2008.
Trends by clinic showed a proportion of pregnant women not screened for syphilis ranging from 6.6% {95% CI, 4.2-9.0} (Extension 14) to 28.9% {95% CI, 19.2-38.7} (Sebele) in 2004, 3.4% {95% CI, 1.6-5.2} (Block 8) to 23.6% {95% CI, 20.8-26.4} (Block 9) in 2005, 4.9% {95% CI, 2.6-7.3} (BH 1) to 33.6% {95% CI, 30.2-37.0} (Block 9) in 2006, 4.9% {95% CI, 2.7-7.1} (BH 1) to 28.7% {95% CI, 23.3-34.1} (BH 2) in 2007, and 3.1% {95% CI, 1.3-4.9} (BH 1) to 18.3% {95% CI, 13.9-22.7} (BH 2) in 2008. Lowest proportions of registered pregnant women not screened for syphilis were consistently noted at BH 1 clinic from 2006 to 2008, while Block 9 and BH 2 clinics consistently recorded highest proportions from 2005 to 2006 and from 2007 to 2008 respectively. About one fourth (3 out of 14) of the clinics showed a rising trends in the proportions of pregnant women screened for syphilis from 2004-2008. The overall picture is that, the majority of the clinics demonstrated no trend in the proportions of pregnant women screened and not screened for syphilis from 2004-2008.
4. DISCUSSION
This section describes the results of our study in relation with the literature reviewed. It also illustrates the public health implications of the results, implications for policy and practice as well as strengths and limitations of this study. As far as the researchers are aware, this study is the first in the country to show a comparison of pregnant women screened and not screened for syphilis as at the time of data collection in 2009.
4.1. Overall Trends in the Proportion of Pregnant Women Screened and Not Screened for Syphilis
In this study, the proportions of pregnant women not screened for syphilis over a 5 years period (2004 to 2008) remains very high in the range from 8.80% to 20.96% and an average just above 10.00%. The problem with patients not screened is that it may lead to an underestimate of the prevalence of syphilis. It also represents an enormous missed opportunity to reduce adverse pregnancy outcomes including congenital syphilis, increased infant and maternal mortalities.
The reasons for the above finding is unclear; but may include factors identified in other studies relating to other sexually transmitted infections (e.g. chlamydia and gonorrhoea) such as lack of reagents at the laboratory, screening results either not retrieved from the laboratory or not documented and long laboratory turn-around times from blood collection to getting results [8], late attendance of pregnant women for antenatal care [9], health care providers’ unawareness of the need to identify and treat syphilis early in pregnancy and thus not prioritising syphilis screening, lack of trained laboratory staff and poor socio-economic status rendering travelling of women from remote areas difficult [10]. This finding suggests an urgent need to conduct periodic supervision and evaluation of the extent of accomplishment of national guidelines in all antenatal clinics in Gaborone, Botswana.
The finding of high percentage (i.e. slightly more than one tenth) of registered pregnant women receiving antenatal care not screening for syphilis in our study is consistent with the study conducted among 536 pregnant women in the Moshi municipality in Tanzania, which reported a 10.6% proportion of pregnant women not screened for syphilis [8]. A cross-sectional study conducted locally in Botswana by Ramoren and Rahman among 703 antenatal care attendees at 13 health facilities in Gaborone, between October 2000 and February 2001 reported a rate of 13% among pregnant women not screened for syphilis. This was the same area where our study was conducted. A similar finding with our survey which came four years later may be an indication that there has been no improvement in the screening rate in the clinics around Gaborone. Furthermore, the high proportion of pregnant women not screened for syphilis in this area could be a reflection of underperformance of the antenatal care system in the country. There was an increase in the proportion of pregnant women not screened for syphilis from 2005 to 2006 in comparison with previous years (2004 and 2005) and 2008 (Table 1 & Fig. 1). The possible reasons advanced above could again be the explanation for this finding [8].
There was an improvement in the syphilis screening program in 2008 with a decline in the proportion of pregnant women not screened for syphilis in all the 14 primary care facilities. This was mostly likely due to corrective measures emanating from the lesson learnt from the 2007 Botswana sentinel surveillance that demonstrated high prevalence of syphilis by districts in the range from 0.4% to 16.7% among pregnant women [7]. The recommended interventions included mandatory syphilis screening with non-treponemal tests (VDRL OR RPR) in the first and third trimesters per index pregnancy, increasing awareness of syphilis screening program among health care workers especially antenatal care providers, promoting community based health education programs on early antenatal care including early syphilis screening among pregnant women, and the adoption of syndromic approach of managing sexually transmitted infections, including syphilis [7].
4.2. Trends by Health Facility the Proportion of Pregnant Women Not Screened for Syphilis
This study confirms high variations in the trend by clinic the proportions of pregnant women not screened for syphilis in the range from 3.13% at BH 1 to 33.64% at Block 9, but more commonly above 10% especially at Sebele, BTA, BH 2,BH 3, Phase 2, Block 6 and 8, Extension 2, Extension 15 and Bontleng. In a previous study on syphilis prevalence in the clinics around Gabarone, the syphilis prevalence rate was found to be high at Sebele, Bontleng, BTA and Block 8 clinics [7]. This is probably due to the variation in the geographical location of the clinics (some in mainly rural, others in more urban areas) which exposes the pregnant women in different socio-economic environments [11]. However, all pregnant women attending public antenatal clinics must be screened during 1st and 3rd trimesters or at the time of delivery (for women who missed 3rd trimester screening), in line with the Botswana national guidelines on VDRL or RPR tests [12]. Furthermore, reactive VDRL/RPR cases must be treated with penicillin, issued with contact slip(s) for partner notification and treatment of sexual partner [13].
4.3. Public Health Implications of this Study
Public health impact of the infection on pregnancy outcomes among unscreened women cannot be underestimated since inadequate antenatal care is an important barrier to the reduction of syphilis prevalence, prevention of pregnancy wastages and congenital syphilis. This impact may be reduced by increasing public awareness on the significance of syphilis screening, and the risks of the infection in pregnancy if not detected and treated early [14].
4.4. Strengths and Limitations
The main strength of our study was that it aimed to examine trends in proportions of pregnant women screened and those not screened for syphilis, which is an important and previously under-studied area in Botswana. The study numbers were large enough to produce a representative sample size. Validation of data was achieved by comparing data collected from the antenatal registers at each clinic site with that of central statistics office at District Health Team and there was little or no difference in numbers. Furthermore, the study included all the clinics providing antenatal care around Gaborone. The study limitation could emanate from possible errors in data entry, given the vast number of patients involved in the study. Also, we did not factored-in parity and nationality of registered pregnant women not screened for syphilis, as these were not pre-conceived as part of the data to be collected during study design. The study reports on data collected in 2009. There is need for studies to be conducted in the similar area to compare current data with the data reflected in this study.
4.5. Recommendations
The authors suggest promotion of earlier antenatal care attendance, preferably during the 1st trimester and each clinic should be encouraged to use the IEC materials to demonstrate the existence of syphilis screening and treatment. Also, rapid on-site screening in line with WHO recommendations, prompt treatment and improved partner tracing are important goals for pregnant women, health care providers and policy makers (13). There is a need to re-emphasize syphilis screening during first and third trimesters because women with non-reactive results in early pregnancy may be sero-reactive during late pregnancy or at the time of delivery [13]. This can be incorporated into the existing prevention of mother to child transmission of HIV (PMTCT) program in the country, targeting both syphilis and HIV prevention in pregnancy. Finally, we recommend a nationwide study that will factor-in parity and nationality of pregnant women receiving antenatal care in all primary care centers in the country.
CONCLUSION
This study showed variations in the trends and proportions of pregnant women screened and those not screened for syphilis in the clinics around Gaborone. However, high proportions of registered pregnant women not screened for syphilis demonstrated in this study may under-estimate syphilis prevalence rates in the city and the country at large. Hence, there is need to put measures in place to trace the pregnant women attending antenatal care in the clinics who default on syphilis screening. Further studies are needed to establish the underlying factors for the occurrence of non-screening among the pregnant women.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Approval for this study was obtained from the University of Liverpool and the Ministry of Health, Botswana (PPME 13/18/1 PSIV {50}). Permission to collect data from the district was obtained from the District Health Team (DHT) of the Gaborone City Council, Botswana.
HUMAN AND ANIMAL RIGHTS
No Animals/Humans were used for studies that are base of this research.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors thank the District Health Team (DHT) of the Gaborone City Council, Botswana for availing the data used in this study. This study was conducted in partial fulfillment of the requirements for the award of the Masters of Public Health (MPH) degree to the first author at the University of Liverpool, United Kingdom.


