RESEARCH ARTICLE
Assessment of Risk Factors and Medication Use for Infectious Vaginitis Among Females of Reproductive Age Visiting Maternity Hospital of Pokhara, Nepal
Prasanna Dahal1, *, Sita Jhendi1, Chham Maya Pun2, Laxman Maharjan1
Article Information
Identifiers and Pagination:
Year: 2017Volume: 10
First Page: 140
Last Page: 147
Publisher ID: TOPHJ-10-140
DOI: 10.2174/1874944501710010140
Article History:
Received Date: 22/04/2017Revision Received Date: 21/06/2017
Acceptance Date: 11/07/2017
Electronic publication date: 31/08/2017
Collection year: 2017

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Vaginitis is one of the most common gynecological problems in females especially in their reproductive ages and poses significant clinical consequences if left untreated. The study aims to assess the risk factors and medication used for its management in reproductive-aged females with vaginitis visiting maternity hospital of Pokhara, Nepal.
Methods and Materials:
A prospective cross-sectional study was carried out on females of age group 15-49 years, diagnosed with infectious vaginitis for the period of two months. Assessment was made based on clinical profile, questionnaire and personnel interview. Descriptive statistics was used for analyzing the results of the study.
Results:
A total of 130 patients were enrolled in the study. Most patients were literate, married and from rural area. Bacterial and fungal infections were common cause for vaginitis representing 56% and 22% respectively. The study shows that the 70% females with infectious vaginitis had a practice of using plain cloth napkins, during their menstruation period and 35% had previous infection in reproductive organ, also risk factors such as pregnancy, use of oral contraceptive, recent antibiotics/steroid use, sexually transmitted disease (STD) and diabetes were commonly present in females with infectious vaginitis. The most frequently (75%) prescribed drug was topical antibacterial –antifungal agents. Metronidazole, cefpodoxime and ciprofloxacin were mostly prescribed among antibiotics whereas fluconazole and clotrimazole were among antifungals.
Conclusion:
The study recommends need of awareness and educational programs concerning reproductive health and hygiene for females in these areas. Prescribing trend shows slight discrepancy from standard treatment guidelines for vaginal infections.
1. INTRODUCTION
Vaginal infection is one of the most common gynecological problems. Approximately 5-10 million offices visits per year are attributed to vaginitis [1, 2]. The most common diseases associated with vaginal infection involve bacterial vaginosis, vulvovaginal candidiasis, and trichomoniasis, which may often also infect in combination [3]. Generally, bacterial vaginosis are associated with a significantly increased risk of pelvic inflammatory disease, post-abortion uterine infection, breast abscess, cervical intraepithelial neoplasia, and posthysterectomy cuff infection [4]. Similarly, Candida albicans is responsible for most episodes of vulvovaginal candidiasis; a very common condition that affects up to 75% of women at least once in their lifetime [5]. Trichomoniasis is the most common non-viral sexually transmitted disease, caused by the parasitic protozoan Trichomonas vaginalis with an estimated 170 million cases occurring worldwide each year [6]. Various studies have revealed that frequent etiology of vaginitis involves imbalances in the normal flora or pH of the vagina, unhygienic practices, improper care during menstruation, pregnancy, diabetes, broad-spectrum antibiotic use, immunodeficiency, frequent douching, diaphragm use, oral contraceptives pill use and occasionally, hormonal and allergic factors [1, 3, 7, 8]. Many studies suggest that oral and topical antibiotics such as metronidazole, tinidazole, clindamycin as the stronghold available therapy for the treatment of bacterial vaginosis and trichomoniasis and antifungals such as fluconazole, clotrimazole, itraconazole are effective in vaginal candidiasis or combined therapy in mixed infection cases [2, 4, 5]. In Nepal, studies related to infectious genital diseases and their risk factors in females are still lacking. With this consideration, this study aims to assess the probable risk factors contributing vaginitis and types of medication prescribed for its treatment in reproductive-aged females visiting one of the maternity hospitals of western Nepal.
2. METHODS AND MATERIALS
The health facility based prospective, observational and descriptive type of study was conducted in maternity child friendship hospital, Pokhara, Nepal from August 2014 to September 2014. The target population consisted of reproductive-aged females with age group between 15 to 49 years, who were diagnosed with infectious vaginitis. Given that the study was carried out in one location only; the sample size was determined based on the number of reproductive-aged females, diagnosed with infectious vaginitis who visited the outpatients department of maternity child friendship hospital during the study period. A random sampling method was used to select the women using the hat and draw procedure to reduce bias. Inclusion criteria include females with age group between 15 to 49 years, diagnosed with infectious vaginitis who were attending outpatients department of maternity hospital and who were not cognitively impaired. We excluded females with cognitive impairment and those who did not give their consent freely.
All relevant clinical information such as patients’ demographics, complains on admission, diagnosis, types of infection and drug prescribed for vaginitis were recorded in suitably design data collection form whereas data on socio-economic variables and risk factors were collected by semi-structured questionnaire based on literature study. Questionnaire includes information regarding patients’ income, occupation, education status, chief complains along with risk assessment indicators such as presence or absence of STD, previous infection on reproductive organs. Diabetes, pregnancy, oral contraceptive use and information concerning sexual hygiene etc. were filled and signed by patients. Research was approved from the Department of Pharmacy, Sunsari Technical College. Permission was obtained from the maternity child friendship hospital through letters written to the hospital administration explaining the goals and the importance of the research and asking for permission to collect data. Before the participants were selected for the study, a brief explanation was given on the goal of the research with basic clarifications about the purpose of the research. Written consent was taken from all the patients who agreed to participate in the study. Participants were informed that the research was strictly for academic purposes and participants’ rights such as the right to confidentiality, right to autonomy and freedom from harm were ensured.
2.1. Statistical Analysis
Collected data were entered in the Microsoft excel spreadsheet (MS office 2007) at the end of the research and computer was secured using a password to secure participant’s information and prevent unwanted access. Descriptive statistics were performed. Analysis of baseline characteristics of study participant were made using univariate chi-square test and with tests of significance being (p < 0.05). Pearson chi square test was used to determine the association of risk factors, symptoms and drugs in relation to types of infections. Percentages were taken in round figures to the nearest integer value while presenting data.
3. RESULTS
A total of 130 patients were assessed in the study. Almost half of them i.e. 49% were of age group of 25-35 years while the mean age of patients was found to be 33 ± SD 8.98 years. Among the total patients, majority of them were married (85%) and from rural areas (75%), however 88% were literate ranging from primary schooling to post- graduate studies. Out of total literate patients, 44% had literacy status lower than higher secondary education level. A large group of patients (76%) were unemployed. Majority of the patients who were employed worked in the private sector. Furthermore, large number of patients had low income status. The details of demographic and socio-economic profile of patients are shown in Table 1.
| Details |
Number (%) (N=130) |
X2 | df | p-value | |
|---|---|---|---|---|---|
| Age group | 15-25 25-35 35-45 45-49 |
24 (19%) 64 (49%) 25 (19%) 17 (13%) |
41.877 | 3 | <0.001 |
| Marital status | Married Unmarried |
110 (85%) 20 (15%) |
62.308 | 1 | <0.001 |
| Area | Rural Urban |
97 (75%) 33 (25%) |
31.508 | 1 | <0.001 |
| Literary status | Illiterate Literate |
16 (12%) 114 (88%) |
73.87 | 1 | <0.001 |
| Employment status | Unemployed Employed |
99 (76%) 31 (25%) |
35.569 | 1 | <0.001 |
|
Family income/ month (in NRS) (1 US $~100NRS) |
Below 5,000 5,000-10,000 10,000-15,000 Above 15,000 |
11 (8%) 18 (14%) 48 (37%) 53 (41%) |
40.646 | 3 | <0.001 |
Among 130 vaginitis cases, 73 (56%) of patients were diagnosed with bacterial vaginitis, 28 (22%) had fungal infection, 3 (2%) were infected with trichomoniasis, 20 (15%) have mixed type infection and 6 (5%) cases were due to other causes like allergies or hormonal. Patients with infectious vaginitis complained of multiple symptoms; most of them includes itching/soreness of genital organ, discharge from genitals often accompanying with unpleasant odor, burning micturition, discomfort during intercourse where as 20.76% of patients complained of other symptoms like dysmenorhoea, irregular menstruation, frequent urination, backache, lower abdominal pain as shown in Table 2. However, distribution of symptoms do not dependent on the types of infection (P > 0.05) (Fig. 1).
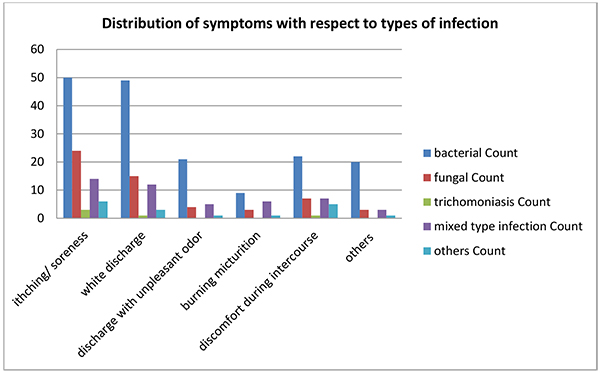 |
Fig. (1). Distribution of symptoms with respect to types of infection. |
| Symptoms | Number (N=130) | Percentage |
|---|---|---|
| Itching/soreness | 97 | 75% |
| Discharge from genitals | 80 | 62% |
| Discharge with unpleasant odor | 31 | 24% |
| Burning micturition | 19 | 15% |
| Discomfort during intercourse | 42 | 32% |
| Others | 27 | 21% |
This study found that 70% of patients had a practice of using cloth napkins (washed, sundried and reusable type) during their menstruation period and 46 (36%) of them had previous infection in reproductive organ; however, habit of daily cleanliness of reproductive organ was found in 100% patients with varied instance and frequency. Several behavioral and biologic risk factors associated with infectious vaginitis predicted in this study are shown in (Table 3 and Fig. 2). Statistical analysis showed that the distribution of individual risk factors was independent of the types of infections i.e. p > 0.05.
| Factors |
Number (N=130) |
Percentage |
|---|---|---|
| Practice of using cloth napkins during menstrual period | 91 | 70% |
| Previous infection of reproductive organ | 46 | 36% |
| Sexually Transmitted diseases | 19 | 15% |
| Oral contraceptive use | 16 | 13% |
| Recent antibiotics/steroid use | 15 | 12% |
| Pregnancy | 15 | 12% |
| Diabetes | 6 | 5% |
| *Cleanness of reproductive organ | 130 | 100% |
* frequency of cleanness of reproductive organ –out of 130 patients cleanness of reproductive organ (vagina) represent as follows:1 time/day -33(25%), 2 time/day -63(49%), more than 2 time/day -34(26%)
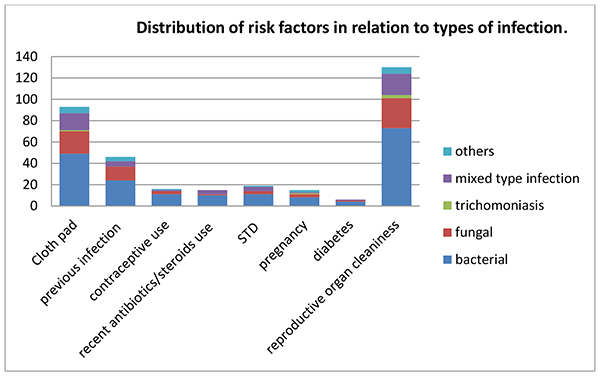 |
Fig. (2). Distribution of risk factors in relation to types of infection. |
Drug prescribing trends depicted that topical antibacterial-antifungals in gel/ointment/tablet forms for local application (clotrimazole / metronidazole / lactic acid bacillus often in mixed form) were the most frequently prescribed drugs i.e. 75% for the treatment of vaginitis followed by metronidazole 33%. Least prescribed drugs were itraconazole and doxycycline representing 7% and 5%, respectiveiy. Prescription of drugs such as cefpodoxime, metronidazole, fluconazole, topical antibacterial-antifungals, secnidazole, cetirizine, clindamycin and itaconazole was significant depending upon the types of infection (p <0.05). Antibiotics were prescribed higher in the cases of bacterial infection and antifungals were mainly prescribed in cases of fungal infection where as both the antibiotics and antifungals were prescribed in suspected mixed infection cases. Topical agents and antihistamines were prescribed in majority of cases of vaginitis irrespectives of types (Fig. 3). Types of medication prescribed for the treatment of infectious vaginitis are shown in Table (4).
| Drugs |
Number (n=130) |
Percentage of cases | X2 | df | P-value |
|---|---|---|---|---|---|
| cefpodoxime | 30 | 23% | 22.940 | 4 | <0.001 |
| ciprofloxacin | 24 | 19% | 3.526 | 4 | 0.474 |
| metronidazole | 43 | 33% | 50.186 | 4 | <0.001 |
| fluconazole | 35 | 27% | 66.237 | 4 | <0.001 |
| Topical antibacterial-antifungal agents | 97 | 75% | 13.947 | 4 | 0.007 |
| secnidazole | 11 | 9% | 9.973 | 4 | 0.041 |
| cetirizine | 35 | 27% | 19.274 | 4 | 0.001 |
| tinidazole | 9 | 7% | 4.490 | 4 | 0.344 |
| cefixime | 11 | 9% | 2.345 | 4 | 0.673 |
| doxycycline | 6 | 5% | 6.907 | 4 | 0.141 |
| clindamycin | 17 | 13% | 10.229 | 4 | 0.037 |
| itraconazole | 9 | 7% | 15.974 | 4 | 0.003 |
| mupirocin | 9 | 7% | 5.374 | 4 | 0.251 |
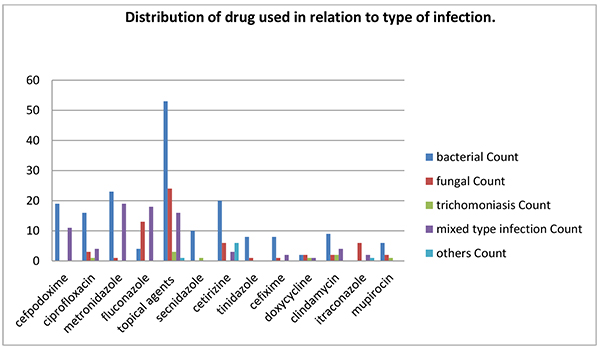 |
Fig. (3). Distribution of drug used in relation to type of infection. |
4. DISCUSSION
Genital infection is a wide spread problem among females of reproductive age. Similar study for assessing prevalence and risk factors on sexually active females carried out by Mascarenhas et al. [1] in Brazil, and Bhalla et al. in India [9] also signify that adolescent and women of child bearing age were more affected by infectious vaginitis. In our study, high cases of infectious vaginitis were observed in married women than unmarried females during the study period. This may be due to effects of factors such as altered menstrual status, hormonal changes, sexual activity, contraceptive use and pregnancy in females of these age groups which may have contributed for higher risk of vaginal infection. Similar finding has been reported by Nzomo et al. [10] in their study conducted in Kenya. Majority of the patients were from rural area and unemployed with low family incomes. These outcomes clearly indicate that the disease prevalence is higher in population with low socioeconomic status. The results were similar to the study conducted by Balamurugan and Bendigeri at Karnataka, India [11].
The study shows that bacterial and fungal were common types of infections followed by trichomoniasis. These findings correlate with the epidemiological findings provided by Tempera in the review on vaginal infections, illustrating that microorganism responsible for vaginal infection includes bacterial vaginosis ranging from 40-50%, and vulvovaginal candidiasis from 20-35%, and trichomoniasis from 5 to 20%, which may often demonstrate as mixed infection [3]. Laxmi et al., in their review on infectious vaginitis inform that bacterial vaginosis has been found to be more common among the women of reproductive age group [8]. A similar finding was obtained in a range of other studies [9, 10]. In our study, itching/soreness of genital organ was most frequent complaint of females with vaginitis followed by discharge from genitals accompanying with unpleasant odor, burning micturition, discomfort during intercourse. This finding contradicts with studies conducted by Balamurugan et al. [11] and Nadan et al. [12] in Karnataka and Uttar Pradesh, India, where vaginal discharge was the most common reported symptom by reproductive-aged females.
In Nepal, adolescent and women particularly of rural areas mostly use the plain old cloth napkins which are washed, sundried and reused multiple times for subsequent cycles rather than hygienic disposable pads available in market. Though limited studies support the opinion that unhygienic menstrual management practice corresponds to increased risk of bacterial vaginosis [13, 14]; our study reflects that majority of females with infectious vaginitis had the habit of using cloth napkins. This may have contributed to vaginitis due to the verity that reused cloth pads may not be well sanitized because cleaning may be often done without soap and with unclean water especially by people with low socio-economic groups and rural areas. Furthermore, factors such as social taboos and restrictions compel females in drying cloth pad indoors, away from sunlight and open air which may result in unsettled bacterial or fungal contamination. This finding coincides with the opinions of some studies related to menstruation hygiene in India [11, 15]. History of previous infection was the second most common risk factor for vaginitis. This re-occurrence might be the outcome of either improper medication or previously unrecognized complication or may be due to repetitive use of contaminated cloth pad [2]. Other risk factors that we observed with vaginosis were pregnancy, use of contraceptive, recently antibiotics/steroid use, sexually transmitted disease, diabetes, and hygienic issues. This result coincides with findings obtained by Mascarenhas et al. in Brazil [1]. The explanation regarding its basis for contributing vaginitis includes that pregnancy may cause behavioural, environmental and hormonal change, and reduce the immunity to fight infections [6]; diabetes increases glucose levels in vaginal secretions and body secretions and alters host defense which may increase risk for infection; recent antibiotics and steroid use may weaken body immune system; multiple partners may increase risk transmitting STD and infections, sexual intercourse and ejaculation are also very strong immuno-suppressive agents and can harm local immune response, oral contraceptives can change the vaginal flora, pH and estrogen level which may contribute to infections [3, 7].
Furthermore, infectious vaginitis has significant clinical consequences if left untreated. The cause of infection must be treated appropriately to prevent recurrence and emergence of any multidrug organisms and knowledge about the various causes of infectious vaginitis, their diagnostic and treatment modalities is very essential for the practitioners for effective management of various vaginal infections. Antibiotics usually recommended for bacterial vaginosis are metronidazole, clindamycin and tinidazole [8]. In our study, highly prescribed drug (75%) was topical antibacterial-antifungal agents (Drug composition contains clotrimazole, metronidazole, lactic acid bacillus often in mixed form). Use of topical therapies in the treatment of bacteria vaginosis are known to be effective and associated with fewer side effects than systematic medication [2]. Combination of clotrimazole, metronidazole and lactic acid bacillus in single dosage form was prescribed for both symptomatic and asymptomatic vaginitis and plays in effective role in eradication of bacterial, fungal or mixed infection vaginitis. Clotrimazole is a broad spectrum anti-fungal drug. Metronidazole tablet was the second most commonly prescribed drug. Metronidazole is used to treat bacterial as well as trichomoniasis infection of the vagina [4]. Until now Metronidazole and clindamycin are regarded as the mainstay of therapy in the treatment of bacterial vaginosis [16]. Recently tinidazole is also used as an alternative. Tinidazole, an antimicrobial agent initially used for Trichomonas vaginalis infections has also been shown to be effective for bacteria vaginosis. Available data suggest that tinidazole has a role in special populations particularly for refractory or relapsing bacteria vaginosis [16, 17]. In our study, cefpodoxime, cefixime and ciprofloxacin were also used in remarkable number of cases of infectious vaginitis. Cephalosporins are considered as safer alternatives during pregnancy. In one recent study, these drugs have shown high drug sensitivity profile against bacteria causing vaginal infection [18]. Ciprofloxacin and other floroquinolones also have proven clinical benefits in case of aerobic vaginitis although contraindicated in pregnancy [19]. However, Van Schalkwyk et al., in their recent study review several systematic reviews, randomized control trials/controlled clinical trials, and observational studies for screening and management of vulvovaginitis and suggested metronidazole, tinidazole and clindamycin for initial treatment of bacterial vaginosis and tricomoniasis whereas, systemic/ or topical azoles are recommended for the treatment of vulvovaginal candidiasis [5]. Similar recommendation is made by the Center of Disease Dontrol and Prevention, USA in their recent treatment guidelines of sexually transmitted diseases [21]. Cetirizine is an antihistamine mostly used in combination of other antibacterial or antifungal in patients who do not respond to single therapy and is highly effective in cases of allergic and itching [20]. Topical and oral antifungal azoles (fluconazole, itraconazole) are effective in the treatment of vulvovaginal candidiasis or fungal infection [4, 8].
CONCLUSION
Bacterial and fungal infections are the most common cause of infectious vaginitis. The study shows that use of old cloth napkins during menstruation period has potential contribution towards infectious vaginitis for which further case control study with large sample is recommended. Besides, risk factors such as previous vaginal infection, pregnancy, use of oral contraceptive, recent antibiotics/steroid, STDs, and diabetes were also seen remarkably linked with females having infectious vaginitis. Metronidazole, cefpodoxime, ciprofloxacin, clindamycin were mostly prescribed among antibiotics whereas systemic and topical azoles were prescribed among antifungals. Prescribing trend shows slight discrepancy from standard treatment guidelines for vaginal infections. The study recommends the need of creating awareness and organizing educational programs concerning reproductive health and hygiene for females in these areas.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research approval was provided by the institution "Sunsari Technical College”.
HUMAN AND ANIMAL RIGHTS
No Animals/Humans were used for studies that are base of this research.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We would like to express our sincere thanks to all the medical and non-medical staffs of Maternity Friendship Hospital, Pokhara.
REFERENCES
| [1] | Mascarenhas RE, Machado MS, Coste Silva BF, et al. Prevalence and risk factors for bacterial vaginosis and other vulvovaginitis in a population of sexually active adolescents from Salvador, Bahia, Brazil. Infect Dis Obstet Gynecol 2012; 2012 378640 |
| [2] | Carr PL, Felsenstein D, Friedman RH. Evaluation and management of vaginitis. J Gen Intern Med 1998; 13(5): 335-46. |
| [3] | Tempera G. Vaginal infections: Epidemiology and risk factors. Luglio-Agosto Giorn. It Ost Gin 2005; 27: 7-8. |
| [4] | Rein MFl. Diagnosis and treatment of infectious vaginitis. J Clin Outcomes Manag 1999; 6(4): 45-54. |
| [5] | van Schalkwyk J, Yudin MH, et al. Infectious disease ccmmittee. Vulvovaginitis: Screening for and Management of Trichomoniasis, Vulvovaginal Candidiasis, and Bacterial Vaginosis. J Obstet Gynaecol Can 2015; 37(3): 266-74. |
| [6] | Nelson DB, Macones G. Bacterial vaginosis in pregnancy: Current findings and future directions. Epidemiol Rev 2002; 24(2): 102-8. |
| [7] | Thulkar J, Kriplani A, Agarwal N, Vishnubhatla S. Aetiology and risk factors of recurrent vaginitis and its association with various contraceptive methods. Indian J Med Res 2010; 131: 83-7. |
| [8] | Lakshmi K, Aishwarya JR, Chitralekha S, Menezes GA. Review on infectious vaginitis. Res J Pharm Biol Chem Sci 2013; 4(3): 679-88. |
| [9] | Bhalla P, Chawla R, Garg S, et al. Prevalence of Bacterial Vaginosis among women in Delhi, India. Indian. J Med Res 2007; 167-72. |
| [10] | Nzomo J, Waiyaki P, Waihenya R. Bacterial Vaginosis and correlates in women of reproductive age in Thika, Kenya. Adv Microbiol 2013; 3: 249-54. |
| [11] | Balamurugan SS, Bendigeri N. Community-based study of reproductive tract infections among women of the reproductive age group in the urban health training centre area in Hubli, Karnataka. Indian J Community Med 2012; 37(1): 34-8. |
| [12] | Nandan D, Gupta YP, Krishnan V, Sharma A, Misra SK. Reproductive tract infection in women of reproductive age group in Sitapur/Shahjahanpur District of Uttar Pradesh. Indian J Public Health 2001; 45(1): 8-13. |
| [13] | Baisley K, Changalucha J, Weiss HA, et al. Bacterial vaginosis in female facility workers in north-western Tanzania: Prevalence and risk factors. Sex Transm Infect 2009; 85(5): 370-5. |
| [14] | Das P, Baker KK, Dutta A, et al. Menstrual hygiene practices, WASH access and the risk of urogenital infection in women from Odisha, India. PLoS One 2015; 10(6): e0130777. |
| [15] | Narayan K, Srinivasa D, Pelto P, Veerammal S. Puberty rituals reproductive knowledge and health of adolescent schoolgirls in south India. Asia Pac Popul J 2001; 16: 225-38. |
| [16] | Menard JP. Antibacterial treatment of bacterial vaginosis: Current and emerging therapies. Int J Womens Health 2011; 3: 295-305. |
| [17] | Dickey LJ, Nailor MD, Sobel JD. Guidelines for the treatment of bacterial vaginosis: Focus on tinidazole. Ther Clin Risk Manag 2009; 5(3): 485-9. |
| [18] | Narayana-Swamy N, Ramalingappa P, Bhatara U. Antimicrobial sensitivity pattern of microorganisms isolated from vaginal infections at a tertiary hospital in Bangalore, India. Int J Med Students 2015; 3(1): 34-43. |
| [19] | Vaginitis A. Abnormal vaginal flora that is distinct from bacterial vaginosis. Medical diagnostic laboratories bulletin. (online). 2012. Available at: https://www.mdlab.com/forms/TechBulletin/Aerobic_Vaginitis.pdf |
| [20] | Neves NA, Carvalho LP, Lopes AC, Cruz A, Carvalho EM. Successful treatment of refractory recurrent vaginal candidiasis with cetirizine plus fluconazole. J Low Genit Tract Dis 2005; 9(3): 167-70. |
| [21] | Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines. Centers of disease control and prevention. MMWR Recomm Rep 2015; 64: 69-75. |









