All published articles of this journal are available on ScienceDirect.
Effects of Smoking Electronic Cigarettes on Pulmonary Function and Environmental Parameters
Abstract
Objectives:
Our study aims to evaluate whether the active use of the electronic cigarette (e-cig) can determine adverse effects on the respiratory function of healthy workers and whether potentially dangerous pollutants are released in the air.
Methods:
Thirty healthy workers (seventeen men and thirteen women, age range 27-37) were included in the study. Immediately before and after a 5-minute smoking session performed in two different days (first-day e-cig, second-day tobacco cigarette [t-cig]), they underwent spirometry evaluation. Furthermore, environmental particle monitoring was performed during the experimental procedure (i.e. before, during and after active smoking).
Results:
Our study showed slight reductions in the main pulmonary function data both after active e-cig and t-cig smoking. Changes in the main respiratory parameters were significantly different than baseline after 1 minute from e-cigarette smoking (3,95 vs 3,91 lt for FEV:P=0,03; 0,84 vs 0,83 for FEV1/FVC ratio:P=0,008; 4,23 vs 3,99 lt/min for FEF25-75%: P=0,03) but not after 15 minutes from active e-cigarette smoking, whereas after t-cig smoking, there was a significant drop in the 15 min value of FEV1(P=, FEF25-75% (P=0.01) and the FEV1/FVC ratio (P=0.007).
Regarding environmental exposure, the e-cig smoking was associated with the transient release of particles with a diameter < 1 micron which dropped to baseline after 5 minutes, whereas in the case of t-cig, the particles persisted for 60 min.
Conclusion:
In this study, the active use of e-cig for a short time caused similar, although less pronounced effects as tobacco smoke on the pulmonary function. Similarly, the particles released in the environment had lower concentration and persistence than those of t-cig. These data suggest that e-cig may potentially be dangerous for active smokers and the environment. Long-term studies seem warranted to discover the health effects of active and passive exposure to e-cig.
1. INTRODUCTION
Both active and environmental tobacco smoking may cause relevant changes in respiratory function [1], and also many diseases sometimes even fatal [2-6] These effects seem to be due to several harmful substances and carcinogens released after the combustion process that underlies the operation of traditional cigarettes. The e-cigs have therefore been proposed in recent years both as a safe alternative to t-cigs and as an aid for smoking cessation [7].
These new devices are in fact reminiscent in design and use gestures to conventional cigarettes, diverging for substances in their liquid pocket which are released through a process of vaporization [8-14], in place of the combustion process of t-cigs.
The absence of tobacco and combustion process would suggest the absence of typical releasing of toxic substances found in tobacco smoke, and therefore the lack of adverse health effects. However, many issues are causing concern for public health, such as the risk of backsliding the habit of tobacco smoking for ex-smokers, to start smoking cigarette for young people, and to lead to nicotine addiction. The risk may be higher for young people given the easy retrieval of these items through the Internet market [15].
In recent years, several studies focused on the possible effects on the health of smokers and non-smokers caused by e-cigs.
Irritation of the mucous membranes, nausea and vomiting, increased sweating and dizziness [16], as well as increased cotinine in saliva [17], in urine [18] and serum [19] of consumers, with probable minor cardiovascular effects, have been reported [20].
Other studies have speculated that, because of ease in the flow of nicotine into the bloodstream following dermal contact or through the gastrointestinal tract, the overthrow of 5 ml of e-liquid on the skin can cause severe poisoning or even death, especially in children if they accidentally touch or swallow the nicotine-containing solution present in the pocket of e-cigs, especially when it is not kept in secured containers. Moreover, the solutions of the e-cigs may contain sensitizing chemicals, such as benzyl alcohol and limonene. Indeed, allergic contact dermatitis and allergic reactions following skin contact, have been reported [21-23]
Research on the respiratory function of e-cig smokers reported an increase in pulmonary resistance and impedance associated to a decrease in exhaled nitric oxide immediately after smoking, as well as non-significant reductions of FEV1/FVC ratio [19].
Pollutants released in the environment may change according to the composition of the liquid, type and age of the e-ig, the length of the puff, puff interval, age, sex and health status of the smoker [24-26]. A comparison of the substances released into the environment after e-cig use with those issued by t-cig, shows that in the steam released from e-cigs, similar substances, albeit at lower concentrations, as released by tobacco smoke can be detected [27-34]
Other studies focused on the size and status of released particles, showing that e-cigs are able to generate an aerosol of fine and ultrafine particles [25, 35, 36], although, once again, at lower concentrations in comparison to the environmental contamination of tobacco smoke. These studies, however, have not defined unambiguously the nature of the aerosol generated, particularly with regard to the characterization of particle size. This is of primary interest regarding the possibility of input and interaction in the different sections of the airways of subjects exposed.
The aim of our study was, therefore, to assess whether the active use of e-cig from healthy subjects can cause short-term effects on lung function, and whether these effects are different from those associated to a similar exposure to tobacco smoke.
Another purpose of our study was to investigate the possible impact on the health of non-smokers by evaluating the environmental pollution resulting from the use of e-cigs and t-cigs, by monitoring the time course of the concentration of particles released in confined spaces, in order to contribute to produce data for regulatory purposes in the workspace.
2. METHODS
2.1. Participants
Thirty healthy non-smoker volunteers (17 man and 13 women) were enrolled, of mean age 32.6 ± 2.75 years (range 27-37 years); average Body Mass Index (BMI) was 23.2 (range, 18 - 28.7). Patients who had one or more of the following conditions were excluded from the study: chronic bronchopulmonary diseases in the acute phase, respiratory allergies, respiratory symptoms, acute or chronic diseases regarding the cardiovascular system, liver, kidney or urinary system, cancer, autoimmune or immunodeficiency conditions.
Similarly, those who were not enrolled in the study were subjects presenting contraindications to the execution of the spirometric test such as pregnancy, recent abdominal surgery, thoracic or ocular episodes of hemoptysis, myocardial infarction (within 3 months) or unstable angina, thoracic aneurysm, pneumothorax, oral pain exacerbated from the mouthpiece, dental implants misplaced, dementia or confusion, language difficulties.
We also excluded those from the study subjects reporting previous spirometric changes and using drugs acting on the pulmonary tract (bronchodilators, corticosteroids, other drugs used for diseases of the airways such as anti-leukotrienes, theophylline, etc.) .
Ex-smokers were excluded for ethical reasons, because the study could lead to a relapse in tobacco smoke .
All subjects avoided alcohol during the preceding 4 hours, abstained from heavy physical activity and from eating during the preceding 2 hours.
2.2. Experimental Design
Each participant underwent, in different days, a 5min session of active e-cig or t-cig smoking. Therefore, all participants performed in different sessions both e-cig (first session) and T-cig (second session).
For e-cigarette smoking protocol, volunteers were asked to perform 15puff of nicotine-containing e-liquid (mean concentration 18mg/ml). During each session, three spirometric evaluations were performed: At baseline (before smoking), within 1 min and after 15 min from smoking. Each evaluation was conducted in accordance with the statement ERS / ATS 2005 with regard to the fulfillment of the criteria for acceptability and reproducibility of the tests. According to those criteria, an adequate test requires a minimum of three acceptable FVC manoeuvres. Repeatability is achieved when the difference between the largest and the next largest FVC is less than 0.150 L and the difference between the largest and next largest FEV1 is less than 0.150 L.
The results were expressed as a) the onset of obstruction, b) changes in the FEV1/FVC ratio, c) changes in FEV1, d) changes in FEF25 -75.
Finally we evaluated the extent of environmental pollution induced by e-cig or t-cig smoking, and its temporal variation during the subsequent 60 minutes.
2.3. Active Smoking Protocol
The e-cig model was a popular model EGO P (L) with manual start; the liquid used, the aroma of Latakia tobacco containing nicotine 1.8% (18 ml / L), propylene glycol, glycerol, vegetable flavorings, and deionized water .
The volunteers were asked to smoke the electronic cigarette over 5-minutes time (the same time required for volunteers smoking a traditional cigarette), performing 15puff.
The used t-cig had a composition equal to 0.6 mg of nicotine, tar 8 mg and carbon monoxide (CO) 9 mg.
2.4. Lung Function Study
Before starting the lung function test, weight and height were measured for each participant. All subjects in the study were asked to perform a full ventilatory inspiratory and expiratory maneuver, both slow and forced acquisition of curves with volume-time and flow-volume . The measurement of lung volumes and flows and their possible variations was assessed using a the flow-based spirometer (SensorMedics, Vmax 229) according to the guidelines of the ATS (American Thoracic Society) ERS (European Respiratory Society) in 2005. Disposable mouthpieces with filter type Microgard II Carefusion were used. The measured values include: Forced Vital Capacity (FVC) ; forced expiratory volume in the first second (FEV 1 or FEV) ; Index Tiffenau (FEV1/FVC) ; Peak Expiratory Flow (PEF) ; forced expiratory flow at 25% of FVC (FEF25%); forced expiratory flow at 50% of FVC (FEF50%) ; forced expiratory flow at 75% of FVC (FEF75%); forced expiratory flow between 25% and 75% of FVC (FEF25 -75%) . At last, three consecutive trials were performed for each subject.
Obstruction was diagnosed in subjects with FEV1/VC below the Lower Limits of Normal (LLN) calculated according to the ECCS or in subjects showing a change in FEV1>20% compared to baseline.
For the simple purpose of our study, no sample size study was conducted before. The data were analyzed with STATA 9 statistical package.
2.5. Protocol for the Environmental Impact Study
For the environmental exposure assessment, we adopted the technique of emission assessment of nanoparticles (Nanoparticle Emission Assessment Technique, NEAT) suggested by NIOSH . For this purpose, two devices are concomitantly used.
- Measurement of the concentration of airborne dust with the use of Optical Particle Counter (OPC) model AEROTRAK 9306 of TSI: the appliance, of portable type, being a six -channel measurement (count), with a flow rate of 0, 1 CFM (2.83 liters / min); the number of particles in the size ranges as 0,3 - 0,5 - 1.0 to 3.0 - 5.0 to 10 m with 0.3 micron sensitivity (from 0.3 micron to 10 mM) ;
- Measurement of the concentration of airborne dust every second with Condensation Particle Counter (CPC) P- Trak Ultrafine Particle Counter Model 8525 TSI: The device measures the number of particles smaller than 1 micron and therefore provides guidance on the presence of nanoparticles .
Evaluation was performed at baseline, during active smoking and for 60 minutes thereafter. All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Policlinico Tor Vergata.
3. RESULTS
Complete spirometry data are shown in Table 1. A significant decrease in comparison to baseline was observed in tobacco smokers in FEV1 1 and 15 minutes after t-cigarette smoking (P=0,005 and P=0,05). The ratio FEV1/FVC and FEF 25-75% also varied significantly from baseline (P=0,045 and P=0,015 respectively) in both cases at 1 and 15-minutes evaluation. In e-cigarette smokers, a significant decrease in FEV1 was observed 1 minute after smoking (3,55 vs 3,51 P=0,033) but not at 15-minutes spirometry (3,55 vs 3,53; P=0,36). Furthermore, a significant fall in FEV1/FVC ratio (0,84 vs 0,83; P=0,008) and in FEF 25-75% (4,33 vs 3,99 lt/min; P=0,000) was observed after 1 minute from the e-cigarette smoking. After 15 minutes from the exposure, a persistent decrease in FEF 25-75% but not in FEV1/FVC ratio was observed. Paired sample ANOVA test was used for statistical evaluation.
| Mean | Diff | S.D. | S.E | 95% C.I. | P | |||
| Lower | Upper | |||||||
|
Smoking Tobacco |
FEV1 Baseline FEV1 post 1 min |
3,53 3,48 |
0,04 | 0,10 | 0,028 | 0,01 | 0,08 | 0,00 |
| FEV1 Baseline FEV1 post 15 min |
3,53 3,51 |
0,02 | 0,054 | 0,016 | 0,01 | 0,04 | 0,05 | |
| FEV1/VC Baseline FEV1/VC post 1 min |
82,2 81,7 |
0,5 | 1,28 | 0,38 | 0,98 | 1,02 | 0,04 | |
| FEV1VC Basale FEV1/VC a 15 min |
82,2 81,0 |
1,2 | 1,16 | 0,35 | 0,75 | 1,68 | 0,01 | |
| FEF25 - 75Baseline FEF25 -75% post 1 min |
3,45 3,38 |
0,06 | 0,13 | 0,04 | 0,01 | 0,11 | 0,01 | |
| FEF25 -75Baseline FEF25 -75post 15 min |
3,45 3,31 |
0,14 | 0,14 | 0,04 | 0,08 | 0,12 | 0,00 | |
| Smoking E-cigarette |
FEV1 Baseline FEV1 post 1 min |
3,55 3,51 |
0,04 | 0,11 | 0,02 | 0,00 | 0,09 | 0,03 |
| FEV1 Basale FEV1 a 15min |
3,55 3,53 |
0,02 | 0,14 | 0,03 | -0,03 | 0,07 | 0,36 | |
| FEV1/VC Basale FEV1/VC a 1min |
82,1 81,6 |
1,03 | 2,00 | 0,37 | 0,29 | 1,78 | 0,01 | |
| FEV1/VC Baseline FEV1/VC post 15 min |
82,1 81,5 |
0,40 | 2,49 | 0,46 | -0,53 | 1,33 | 0,39 | |
| FEF25 -75 Baseline FEF25 - 75 post 1 min |
3,44 3,3 |
0,23 | 0,31 | 0,06 | 0,12 | 0,35 | 0,00 | |
| FEF25 -75 Baseline FEF25 - 75 post 15 min |
3,44 3,35 |
0,09 | 0,32 | 0,06 | 0,02 | 0,25 | 0,03 | |
3.1. Study of Environmental Contamination
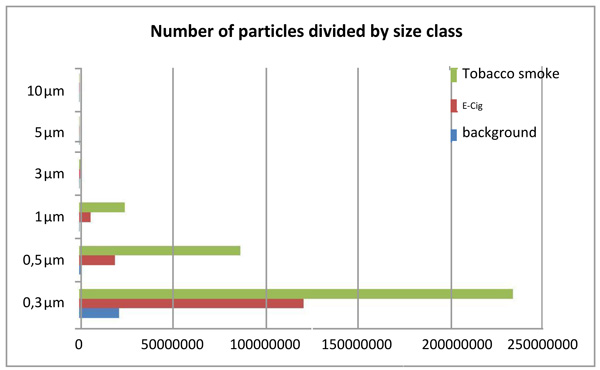
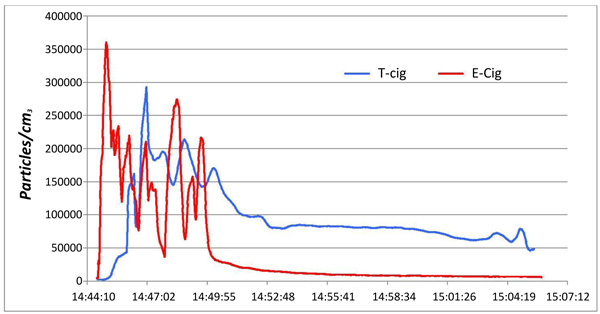
The number concentration of airborne particles of different size and the time course concentration are shown in Figs. (1 and 2). During the session for the detection of tobacco smoke, the average concentration of particles in the bottom of the room was 2443pp/cm3, while those measured during and after smoking, it was 42645 pp/cm3 (range 2310 – 500000 pp/cm3).
The corresponding value for the e-cigarette session was 49690pp/cm3 (range 5040-500000pp/cm3).
The concentration of the particles released by e-cig dropped to baseline levels in about 5 minutes, whereas the particles released by t-cig lasted for about 30 min (Fig. 2).
4. DISCUSSION
To our knowledge, only few studies evaluated the lung function changes related to e-cig exposure and the consequential impact on the indoor air quality in the workplace based on the evaluation of air pollutants produced comparatively by both tobacco and e-cigarette smoking task. In our study, 5 minutes of the use of e-cigarette caused a significant decrease in airflow when measured with flow-volume spirometry. The spirometry results regarding active e-cigarette smoking are partially consistent with the others published studies [19, 23]. In our study, we found no significant onset of obstruction patterns in the exposed healthy volunteers (when defined by a FEV1/VC ratio under low limits of normality - according to ATS/ERS statement 2005) and non-significant changes in FEV1 (defined as a fall in the parameter >20% of baseline value) in the e-cig group. On the other hand, we observed a uniform trend of a significant worsening of all respiratory parameters after 1 minute but not after 15-minutes from active e-cigarette smoking task and a persistent decrease in FEF25-75%. This parameter has been shown to be more sensitive than FEV1 and FEV1/VC ratio in predicting the development of clinically evident airflow obstruction associated with air pollution, although a potential weakness may be represented by its relatively high day-to-day variability [37-41].
It should be noted that the changes we observed in the airflow, even if statistically significant, may be too small to be clinically relevant for healthy people. We cannot exclude, however that the situation might be different for susceptible subjects. According to previous studies, we hypothesize that the decrease in the airflow is attributable to the acute increase of airflow resistance due to small airway narrowing depending on both mucosal edema, smooth muscle contraction or local secretions. This hypothesis is supported also by the findings of our study that showed airflow changes immediately after the smoking task (1 minute), suggesting an immediate response typically related to muscles response.
Regarding the changes in FEV1, no subject showed a fall of this parameter greater than 20% from baseline after smoking t-cig or e-cig. This result may be related to the relatively low doses used in our study design. Of note, a difference in FEV1 baseline values was observed between the first (e-cigarette) and the second (T-cigarette) session. This is probably due to spontaneous inter-day oscillation in this parameter in healthy subjects. Anyway, this fact had no influence on the results, which were based on the difference in FEV1, FEV1/FVC ratio and FEF 25-75% recorded before and after smoking.
In 2013, Flouris et al. [19] claimed that studies regarding the relationship between exposure to e-cigarette smoking and the onset of respiratory acute effects were flawed due to lack of proper control group and of controlling the influence of recent smoking. In our study, the control group was represented by the same population exposed to 5 minutes e-cig smoking. The changes we evidenced in the e-cig exposure were quantitatively similar to that evidenced after tobacco smoking. In our experience, this is the first study evidencing small airways flow changes after e-cigarette smoking. Although chronic obstructive lung disease is a long-term process, even small exposure to toxic pollutants can stimulate the tissue reaction contributing to the late effects. This fact must be considered carefully when defining public health policies or when planning medical or occupational regulation.
As far as the environmental evaluation is concerned, the results of our study are consistent with those obtained by other studies, which reported that emissions of fine and ultrafine particulate matter from traditional cigarettes and electronic equipment are greater than those present in the first session of smoking [25, 36].
Further studies have shown how aerosol generated by the electronic cigarette falls within the particle size of 250-450 nm, similar to the range of traditional cigarettes [36].
The results obtained from our observations thus show how environmental tobacco smoke can pollute a closed environment for a long time even after smoking, as opposed to the electronic cigarette.
Surely, the use of electronic cigarettes with different dose of nicotine or used for a longer time could give different results. Variables such as aeration of the environment, the size of the room, the temperature, the number of smokers or the type of cigarette used may have an influence.
Although the health effects of the exposure to the concentrations used in our study are not clear, in our opinion the findings of our work must be carefully considered in the evaluation of environmental control strategies regarding the use of the e-cigarette in indoor workplace.
It might be appropriate to investigate the dynamics of indoor pollution to highlight the possible need to suggest measures such as bans or restrictions on the use of e-cig in certain well-identified areas where adequate ventilation and air circulation are guaranteed.
CONCLUSION
The active use of the electronic cigarette by healthy subjects leads to worsening of the main parameters of ventilatory function after 5 minutes exposure. These changes are smaller than that observed after exposure to tobacco smoke.
Both types of cigarettes showed measurable albeit different effects on air quality in confined spaces.
The health effects of long-term active and passive exposure to e-cigarette need to be assessed.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
The protocol was approved by the Ethics Committee of Policlinico Tor Vergata.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2008.
CONSENT FOR PUBLICATION
All subjects gave their informed consent for inclusion before they participated in the study.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


