All published articles of this journal are available on ScienceDirect.
Health-Related Quality of Life and Associated Factors Among People Living with HIV /AIDS Following ART Clinic in Jimma University Specialized Hospital, Southwest Ethiopia: A Facility- Based Cross-Sectional Study
Abstract
Background:
HIV care of people living with HIV /AIDS (PLWH/A) is critical for fruitful HIV inhibition, treatment and provision of quality of life. The goal of Anti-Retroviral Therapy (ART) is to suppress viral replication, lessen morbidity and death, and improve patients’ quality of life. The quality of life of HIV/AIDS patients is not well appraised in the study area beforehand. Therefore, this study assessed the health-related quality of life and associated factors among people living with HIV /AIDS followed by ART Clinic in Jimma University Specialized Hospital, Southwest Ethiopia.
Methods:
We used facility based cross-sectional study design and 351 samples selected by systematic random sampling from Jimma University Specialized Hospital ART clinic in March-2014. Data were collected through interviewer-administered questionnaires and analyzed by using SPSS version 20.0 software. Descriptive analysis (frequency and percentage) was calculated. Bivariate and multivariate analyses were used to identify associated factors. The association between the explanatory and dependent variables was assessed at p-value of less than 0.05. The results were presented in a narrative form, tables and graphs.
Results:
From the total respondents, 143 (40.7%) of them have low quality of life in general. Of these, 238 (67.8%) of them had low psychological domain, 136 (38.7%) had low physical domain and 223 (63.5%) low social domain. The age ≤ 39 years (AOR = 2.381 [95% CI = 1.238, 4.579]), Currently employed (AOR= 3.509 [95% CI = 1.900, 6.482]), current CD4 count ≥ 250 cell/ml (AOR = 2.663 [95% CI = 1.363,5.203]), current WHO Stage I-II (AOR = 4.772 [95% CI = 2.308, 9.865]), good general health condition (AOR = 2.609 [95%CI = 1.372, 4.961]), no comorbidity (AOR = 7.737 [95% CI = 4.146, 4.438), friendly social relationship (AOR = 5.395 [95% CI = 2.781, 10.467]), other persons reminded their drugs took time (AOR = 3.363 [95% CI = 1.629, 6.943]) and drunk alcohol (AOR = 1.915[95% CI = 1.039, 3.529]) were identified as the predictors of health related quality of life.
Conclusion:
Findings of this study indicate that the significant number of participants exists on low-level- of health related quality of life in general. The age, occupation, current CD4 count level, current WHO stage status, general health conditions, comorbidity conditions, status of their social relations, their conditions due to lack of support, reminder of drugs taking time, and alcohol drinking status have been observed to have a statistically significant association with their health-related quality of life status.
1. BACKGROUND
HIV/AIDS continues to spread worldwide and is one of serious health challenges. Although much of the news on AIDS is encouraging, the challenges become continued. Globally, there were 36.7 million people living with HIV in 2015, which increased up to 33.3 million in 2010 because of continuing new infections; people are living longer with HIV than the general population. However, 1.1 million people died of AIDS in 2015. There were about 2.1 million new infections reported in 2015 or about 5,700 new infections per day. An estimated 32.1 million adults aged 15-49 years worldwide are living with HIV [1, 2]. Around two million children are living with HIV, with 110,000 AIDS-related deaths reported and 150,000 new infections among children in 2015 [3].
Sub-Saharan Africa, the hardest hit region, is home to nearly 70% of people living with HIV but only about 13% of the world’s population [4]. The sub-region of Eastern and Southern Africa is home to more than half (52%) of all people living with HIV, as well as more than half of the children living with HIV (56%) [5]. Ethiopia has a large and very vulnerable population; there is more than half million (671,941) HIV positive population, with 14,405 new HIV infections and 24,813 deaths reported in 2016 [6].
The goal of antiretroviral therapy (ART) is to suppress viral replication, reduce morbidity and mortality, and improve quality of life (QoL) [7]. The global coverage of ART increased from 2% of people living with HIV in 2000 to 40% in 2014. In the WHO African Region, 41% [38–46%] of people living with HIV were able to access life-saving medicines in 2014. Globally, more than 18 million people were receiving antiretroviral treatment in mid-2016 [8].
Health-related quality of life (HRQoL) is a multidimensional construct showing an individual's or a group's perceived physical, social and mental domains functioning over time. It goes beyond the direct measures of population health, life expectancy, and causes of death, and focuses on the impact that health status has on the quality of life [9, 10]. According to the World Health Organization (WHO), QoL is defined as an individuals’ perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns. This definition considers individuals’ satisfaction with their physical, psychological, social relationships, environment, and spiritual aspects of their life [11].
Clinicians and public health officials have used HRQoL and well-being to measure the effects of chronic illness, treatments, and short- and long-term disabilities. The measure of health outcomes would begin to assess the population’s health not only on the basis of saving lives, but also in terms of improving the quality of lives [12].
The measures of Quality of life (QoL) present an opportunity to evaluate interventions from the perspective of the patient [13]. The major challenge in Ethiopia and other resource-limited settings in Africa is lack of information on HRQoL of populations affected by HIV/AIDS. Moreover, the quality of life of HIV/AIDS patients is not well - known and has not been well assessed in the study area previously. Therefore, this study assessed the health-related quality of life and associated factors among people living with HIV /AIDS following ART Clinic in Jimma University Specialized Hospital, Southwest Ethiopia.
2. METHODS
2.1. Study Setting and Participants
A facility-based cross-sectional study was conducted in Jimma University Specialized Hospital ART clinic from March 1 to 30, 2014. Jimma University Specialized Hospital (JUSH) is one of the oldest public hospitals in the country. It was established in 1937 by Italian invaders for the service of their soldiers. Geographically, it is located in Jimma city that is located at 357 km from Addis Ababa [14]. JUSH is the teaching and referral hospital that has around 450 beds and more than 750 empolyees as both supportive and professional staff. It provides services for approximately 9000 inpatient and 80000 outpatient attendances a year. JUSH ART clinic pioneered the use of antiretroviral drugs in Ethiopia in 2002. The clinic currently gives follow-up service for about 6260 HIV/AIDS patients. On average, 50 - 100 patients were observed to visit the clinic on a day. The follow-up appointments were being given to patients in every one to two months. The clinic staffed with internist, senior health officer and nurses who were trained in specific HIV/AIDS disease patient cares [15].
2.2. Sample Size Determinations and Sampling Techniques
The sample was determined by single population proportion formula using EPI Info 7.1.0.6 version was applied with an assumption of the level of confidence of the study being 95%, sampling error tolerated 5%, proportion of poor quality of life 56.4% [20] and 5% non-response rate. Since the total population were 6260 that was less than 10,000, the population correction formula was used. Finally, 372 sample sizes were calculated.
Study participants were selected by using the systematic random sampling technique. There were a total of 6260 patients registered for ART care in the hospital. Per day, high turnover of patients was observed as approximately 130 patients were observed to attend the PLWHA clinic each day. To finish data collection within one month, every day around 18 study participants were recruited. Therefore, every 7th patient attending the clinic was involved in an interview until the required sample of 372 was recruited. As patients attended the clinic on a monthly basis and above, no patients included twice during the recruitment period. The study includes adult patients above the age of eighteen years old due to ethical issues.
2.3. Data Collection Instruments and Methods
The questioners were adapted from related literatures [17-29]. The questioners assessed mainly socio-demographic factors like age, educational status, occupation, marital status, etc; disease related care factors like CD4 count, WHO stage, length of treatment, general health condition, etc and social relationship related factors such as reminder of drugs, with whom they live, self-care status, etc; moreover also questions that help us to measure their physical activities and psychological freedom, freely thinking, interpretation, etc. Data were collected both by Afan Oromo and Amharic questionnaires. Five BSc nurses working in JUSH ART clinic who could speak both Amharic and Afan Oromo were collected the data by face-to-face interview. One BSc nurse who works at JUSH ART clinic was assigned as the supervisor at the time of data collections to supervise the overall data collection conditions including technical activities. The patients were interviewed after they received the service they required from the ART clinic.
2.4. Data Quality Assurance
The questionnaires were pre-tested on 5% of the sample in Jimma town, Shanan Gibe Hospital on HIV positive patients who started HAART drug treatment at ART clinic before the actual data collections and amendment were made accordingly. Language experts translated the questioners into two local languages (Ahmaric and Afan Oromo) and then back to English to make sure the consistency of the questionnaires, then correction were done accordingly. The data collectors and supervisors were trained on data collection tools and procedures for one day. On top of this, supervisors were follow data collectors. Both supervisors and investigators also checked for clarity and completeness of the collected data in every day during the period of data collections.
2.5. Data Processing and Analysis
Before data entry, questionnaires were checked for completeness. Data was entered into Epidata version 3.0 and then exported to SPSS version 20.0 for further analysis. Descriptive methods of statistical analysis, percentage, frequency and mean were calculated. The mean was calculated by computing different questions and depending on the calculated mean results, the variables under study were dichotomized into good quality of life and poor quality of life. Bivariate logistic regression analysis will be used to identify associations between variables. The variables that had a p-value ≤ 0.3 have an association with another similar research and variables that are suspected to have an association with study variables were transferred to multiple logistic regression models. The possible effects of confounders were controlled through multivariate logistic regression analysis to identify the predictor of the study variables. The association between the explanatory and dependent variables was assessed at a p-value of 0.05. The variables that shown p-value < 0.05 were considered as statistically significant variables in the final model. The degree of association between independent and dependent variables was assessed using adjusted odds ratio with 95% confidence interval. The findings were presented in the form of narratives, cross-tabulations, tables, pie charts and graphs.
3. RESULTS
3.1. Socio-demographic Characteristics
Three hundred seventy-two study participants were sampled and only 351 of them participated in the study with the response rate of 94.35%. The female respondents were more accounting for 228(65%). Most of the participants273 (67.5%) aged less than 40 years Concerning their marital status, unmarried were dominant accounting for 152 (43.3%) followed by 99 (28.2%) married and 69 (19.7%) divorced. Majority of the study participants were of primary school 143 (40.7%) followed by secondary school 104 (30.5%). Depending on the ethnicity and religion, Oromo and Muslims account for 42.7% and 29% respectively. Based on occupations, 247 (70.4%) of them were employed (Table 1).
| Variables | Alternatives | Frequency | Percentage (%) |
|---|---|---|---|
| Age of the respondent | 1. ≤ 39 years | 237 | 67.5 |
| 2. ≥ 40 years | 114 | 32.5 | |
| Sex of respondents | 1. Male | 123 | 35 |
| 2. Female | 228 | 65 | |
| Marital status | 1. Single | 152 | 43.3 |
| 2. Married | 99 | 28.2 | |
| 3. Widowed | 31 | 8.8 | |
| 4. Divorce | 69 | 19.7 | |
| Educational level | 1. No formal education | 70 | 19.9 |
| 2. Grade: 1-8 | 143 | 40.7 | |
| 3. Grade: 9-10 | 104 | 30.5 | |
| 4. 10+, certificate and above | 31 | 8.8 | |
| Ethnicity | 1. Oromo | 153 | 43.6 |
| 2. Amhara | 96 | 27.4 | |
| 3. Tigre | 18 | 5.1 | |
| 4. Dawuro | 34 | 9.7 | |
| 5. Yem | 36 | 10.3 | |
| 6. Other* | 14 | 4 | |
| Religion | 1. Muslim | 102 | 29.1 |
| 2. Orthodox | 181 | 51.6 | |
| 3. Protestant | 68 | 19.3 | |
| 4. Others** | 13 | 3.6 | |
| Occupation | 1. Currently employed | 247 | 70.4 |
| 2. Currently not employed | 104 | 29.6 | |
| Income of respondents | 1. ≤ 500 ETB | 253 | 72.1 |
| 2. 501 - 1000 ETB | 48 | 13.7 | |
| 3. ≥ 1001 ETB | 50 | 14.2 |
3.2. Clinical Conditions of Participants
Majority of respondents, 248 (70.7%) had a CD4 count less than < 250 cell/ml when they started taking ART to follow up clinic services. During the data collection time, half 178 (50.8%) of the respondents had greater than 250 cell/ml CD4 count. Three forth, 283 (80.6%) of the participants were at stage I - II of WHO classification. Regarding opportunistic infections prophylaxes, majority 233 (66.4%) of them were taking prophylaxes. Moreover, 247 (70.4%) of them were found on good general health condition. Compared to the last year, 273 (77.8%) of them were better now than a year in relation to health status (Table 2).
| Variables | Alternatives | Frequency | Percentage |
|---|---|---|---|
| CD4 count when ART started | 1. < 250 cell/ml | 248 | 70.7 |
| 2. ≥ 250 cell/ml | 103 | 29.3 | |
| CD4 count currently | 1. < 250 cell/ml | 73 | 20.8 |
| 2. ≥ 250 cell/ml | 278 | 79.2 | |
| WHO stage at start | 1. Stage I - II | 286 | 81.5 |
| 2. Stage III - V | 65 | 18.5 | |
| Current WHO stage of HIV | 1. Stage I - II | 283 | 80.6 |
| 2. Stage III- V | 68 | 19.4 | |
| Vests clinic for health seeking | 1. Yes | 285 | 81.2 |
| 2. No | 66 | 18.8 | |
| Discontinuation of OI prophylaxes | 1. Yes | 233 | 66.4 |
| 2. No | 118 | 33.6 | |
| How long they stayed on treatment | 1. < 2 years | 143 | 40.7 |
| 2. ≥ 2 years | 208 | 59.3 | |
| General health condition | 1. Good | 247 | 70.4 |
| 2. Poor | 104 | 29.6 | |
| Faced body pain in last 4 weeks | 1. Not faced | 217 | 61.8 |
| 2. mild pain | 103 | 29.3 | |
| 3. severe pain | 31 | 8.8 | |
| Healthy as any body | 1. Yes | 223 | 63.5 |
| 2. No | 128 | 36.5 | |
| Compared to last year how they rate their health status | 1. better now than a year | 273 | 77.8 |
| 2. worse now than a year | 78 | 22.2 | |
| Can perform any physical exercise | 1. yes | 215 | 61.3 |
| 2. No | 136 | 38.7 | |
| Have attended health education | 1. Yes | 287 | 81.8 |
| 2. No | 64 | 18.2 |
3.3. Quality of Life of the Participants
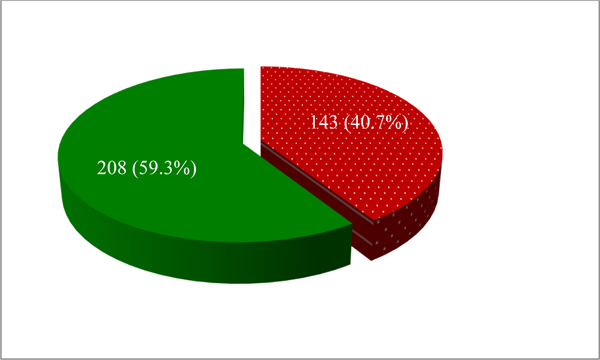
From all participants, 143 (40.7%) of them had low quality of life in general (Fig. 1). When assessed by different domains of quality of life, 238 (67.8%) of them had a low psychological domain, 136 (38.7%) had a low physical domain and 223 (63.5%) social domain (Fig. 2).
3.4. Factors Associated with Health-related Quality of Life
In binary logistic regression analysis, age, sex, occupation, income, CD4 count currently, current WHO stage of HIV, general health condition, how long they stayed on treatment, their health status compared to the last year, having comorbidity, self-care status, relationship with community, facing negative consequence due to lack of support, drinking alcohol and cigarettes smoking have a statistical association with their quality of life status.
The independent variables that had a p-value ≤ 0.25 in binary logistic regressions were moved into multiple logistic regression models. After analysis; age, occupation, current CD4 count level, current WHO stage of HIV, general health condition, comorbidity status, relationship with community, a reminder of drugs and alcohol drinking status of the respondents have a statistically significant association with patients’ quality of life. In further elaborations; patients that aged ≤ 39 years were around two times more likely to have a high quality of life when compared with those aged above 40 years (AOR = 2.381 [95% CI = 1.238, 4.579]). Those respondents that have occupations were 3.5 times more likely to have a high quality of life when compared with those who have no jobs (AOR= 3.509 [95% CI = 1.900, 6.482]). Patients that have current CD4 count ≥ 250 cell/ml were around three times more to have a high quality of life as related to with their counterparts (AOR = 2.663 [95% CI = 1.363,5.203]). The participants that exist on a good level of general health condition were 2.6 times more to have a high quality of life compared to their opposite(AOR = 2.609 [95%CI = 1.372, 4.961]). Moreover, the respondents who were recently at WHO stage I – II were around 5 times more than their complements to have a high quality of life (AOR = 4.772 [95% CI = 2.308, 9.865]). Those patients who had no comorbidity were around eight times more likely to have a high quality of life when compared with those who had comorbidities with other diseases (AOR = 7.737 [95% CI = 4.146, 4.438). In addition, respondents those who had friendly social relations were five times more likely to have a high quality of life as compared to those faced discriminations (AOR = 5.395 [95% CI = 2.781, 10.467]). Also, the participants those not faced any negative consequence related to lack of support were around three times more to have a high quality of life (AOR = 2.987 [95% CI = 1.498, 5.956]). Likewise, participants, those have other persons who remind them when drugs taking time reached were three times more likely to have a high quality of life as compared to those participants who remind the drugs taking time by themselves (AOR = 3.363 [95% CI = 1.629, 6.943]). Finally, the participants who did not have alcohol drinking behaviors were 2 times more likely to have a high quality of life as compared to their equivalents (AOR = 1.915[95% CI = 1.039, 3.529]) (Table 3).

| Independent Variables | Alternatives | Quality of Life | P-values | COR [95%C.I] | AOR [95%C.I] | ||
|---|---|---|---|---|---|---|---|
| Low | High | COR | AOR | ||||
| Age of respondents | ≤ 39 years | 83 | 154 | .027 | .009 | 1.670 (1.060 - 2.630) | 2.381 (1.238 - 4.579) |
| ≥ 40 years | 54 | 60 | 1.00 | 1.00 | |||
| Sex of respondents | Male | 32 | 87 | .001 | .148 | 2.248 (1.390 - 3.635) | 1.573 (0.852 - 2.904) |
| Female | 105 | 127 | 1.00 | 1.00 | |||
| Marital Status | Single | 61 | 91 | .397 | .868 | 0.941 (0.558 - 1.585) | 0.914(0.317 - 2.638) |
| Married | 37 | 62 | .277 | .932 | 1.445 (0. 814 - 2.565) | 1.049 (0.346 - 3.177) | |
| Divorce | 24 | 45 | .199 | .035 | 1.478 (0. 680 - 3.212) | 3.453 (1.092 - 6.919) | |
| Widowed | 15 | 16 | 1.00 | 1.00 | |||
| Educational level of respondents | No education | 28 | 42 | 1.00 | |||
| Primary (1-8 | 67 | 79 | .415 | 0.786 (0.441 - 1.402) | |||
| Secondary (9-10 | 39 | 67 | .668 | 1.145 (0.616 - 2.129) | |||
| Post-secondary (10+) | 9 | 20 | .403 | 1.481 (0.590 - 3.720) | |||
| Occupation of respondents | Currently employed | 79 | 168 | .000 | .000 | 3.403(2.112 - 5.482) | 3.509 (1.900 - 6.482) |
| Currently not employed | 64 | 40 | 1.00 | 1.00 | |||
| Average monthly income | ≤ 500ETB | 111 | 142 | 1.00 | 1.00 | ||
| 501- 1000ETB | 18 | 30 | .414 | .680 | 1.303 (0.690 - 2.458) | 0.841 (0.369 - 1.918) | |
| ≥ 1001ETB | 14 | 36 | .040 | .493 | 2.010 (1.033 - 3.910) | 0.731(0.298 - 1.794) | |
| CD4 count when ART started | < 250 cell/ml | 73 | 100 | 1.00 | |||
| ≥ 250 cell/ml | 70 | 108 | .584 | 0.888 (0.580 - 1.359) | |||
| CD4 count currently | < 250 cell/ml | 47 | 26 | 1.00 | 1.00 | ||
| ≥ 250 cell/ml | 116 | 162 | .001 | .004 | 2.373(1.431 - 3.935) | 2.663 (1.363 - 5.203) | |
| WHO stage at start | Stage I-II | 122 | 164 | .127 | .769 | 1.559(0.881 - 2.757) | 0.894 (0.422 - 1.893) |
| Stage III-IV | 21 | 44 | 1.00 | ||||
| Current WHO stage of HIV | Stage I-II | 100 | 183 | .000 | .000 | 3.148(1.816 - 5.455) | 4.772 (2.308 - 9.865) |
| Stage III-IV | 43 | 25 | 1.00 | 1.00 | |||
| General health condition | Good | 85 | 162 | .001 | .003 | 2.403 (1.506 - 3.836) | 2.609 (1.372 - 4.961) |
| Poor | 58 | 46 | 1.00 | 1.00 | |||
| Discontinuation of OI prophylaxes | No | 99 | 134 | .349 | 1.243(0.789 - 1.958) | ||
| Yes | 44 | 74 | 1.00 | ||||
| Compared to last year how they rate your health | Better now than a year | 101 | 172 | .008 | .863 | 1.987 (1.195 - 3.304) | 1.066 (0.514 - 2.212) |
| Worse now than a year | 42 | 36 | 1.00 | 1.00 | |||
| How long they stayed on treatment | < 2 years | 46 | 97 | 1.00 | 1.00 | ||
| ≥ 2 years | 97 | 111 | .007 | .091 | 1.843 (1.182 - 2.873) | 1.677(0.920 - 3.057) | |
| Have any Clinical symptoms for HIV | Yes | 82 | 125 | 1.00 | |||
| No | 61 | 83 | .606 | 1.120(0.727 - 1.726) | |||
| Comorbidity Conditions | Yes | 85 | 52 | 1.00 | 1.00 | ||
| No | 58 | 156 | .000 | .000 | 4.397 (2.781 - 6.952) | 7.737 (4.146 - 4.438) | |
| Self-care status | Low | 154 | 81 | 1.00 | 1.00 | ||
| High | 38 | 78 | .033 | .738 | 1.658 (1.041 - 2.640) | 1.114 (0.591 - 2.100) | |
| Community relation with HIV patients | Friendly | 98 | 138 | .001 | .000 | 2.953(1.797 - 4.852) | 5.395 (2.781 -10.467) |
| Discrimination | 87 | 28 | 1.00 | 1.00 | |||
| Faced any negative consequence of lack of support | Yes | 23 | 62 | 1.00 | 1.00 | ||
| No | 120 | 146 | .004 | .002 | 2.216 (1.296 - 3.787) | 2.987 (1.498 - 5.956) | |
| Currently with whom they living | With another person | 129 | 173 | .065 | .119 | 1.864 (0.963 - 3.608) | 2.048 (0.831 - 5.047) |
| Alone | 14 | 35 | 1.00 | 1.00 | |||
| Reminder of drugs | Self | 106 | 169 | 1.00 | |||
| Other person | 37 | 39 | .113 | .001 | 1.513(0.907 - 2.522) | 3.363 (1.629 - 6.943) | |
| Drinks alcohols | Yes | 61 | 52 | 1.00 | 1.00 | ||
| No | 82 | 156 | .001 | .037 | 2.232 (1.414 - 3.523) | 1.915 (1.039 - 3.529) | |
| Being cigarette Smoker | Yes | 48 | 49 | 1.00 | 1.00 | ||
| No | 95 | 159 | .040 | .324 | 1.640 (1.022 - 2.629) | 1.371 (0.732 - 2.568) | |
| Khat chewing | Yes | 35 | 54 | .753 | 1.082 (0.662 -1.769) | ||
| No | 108 | 154 | 1.00 | ||||
4. DISCUSSION
This study assessed the health-related quality of life and associated factors among people living with HIV /AIDS following ART Clinic in Jimma University Specialized Hospital, Southwest Ethiopia. Accordingly, from all participants, 143 (40.7%) of them have a low quality of life in general. When assessed by different domains of quality of life, 238 (67.8%) of them have a low psychological domain, 136 (38.7%) have a low physical domain and 223 (63.5%) social domain, respectively.
The age of respondents, those aged less than 39 years is more likely to have good health related quality of life as this finding, as they are the youngest and they can care for themselves independently. Regarding their occupation, employed respondents have good health-related quality of life and this can be happen since they can support themselves financially as they engage themselves with work that can make them to forget about their disease and more in social relationship at work which has a great contribution for quality of life.
Moreover, those respondents with their current CD4 count level above 250 cell/ml and being at WHO Stage I-II currently have a high quality of life than their counterpart. This is because of their health status is not further deteriorated by the disease and it has a direct relationship with their general health conditions. likewise, having comorbidity with other diseases and having good social relations. If they had an additional disease, it can further damage their health and they end up with having a poor quality of life. Meanwhile, lack of support and lack of reminder of drugs taking time and alcohol drinking behaviors are the predictors of the status of health-related quality of life. This shown that supporting HIV/AIDS patienthas a great contribution to the improvement of their quality of life.
Similar to this study finding, the study conducted ne in Irish presented that average level of HIV-infected people had health-related quality of life [16]. Another study conducted in Central Karnataka, India revealed that the quality of life was rated as poor by 26% of the study subjects and 27% of the subjects are dissatisfied with their overall health status. Quality of life score was the highest in the environmental domain and lowest in social relationships domain, which were much lower than this study [17]. Likewise, the studies conducted in Bangladesh revealed that majority of the respondents were with low Quality of Life (QoL) in all the domains of HQoL. The proportion of respondents with low QoL was the highest in the domain of social relationship (64.6%) followed by psychological domain (59.8%) and physical domain (58.5%) [18].
Furthermore, the study conducted in Nigeria showed that the psychological health and physical health domains were similar and but the social domain was very low [19]. Also, the study condcuted e in Felege Hiwot Referral Hospital, Bahir Dar, North West Ethiopia has shown that the proportion of respondents with low health-related quality of life in all domains was 56.4% [20].
Similar to this study finding, the study conducted in Northeastern region of Brazil and also in Belgium has shown that male gender, having a paid occupation, income per capita, a longer time since diagnosis, having been stigmatized and adherence to treatment were predictors associated with a quality of life [21, 22]. Another study conducted in Southern Brazil and Nigeria on the same title exposed that low quality of life was associated with being female, age < 40 years, having low education levels, low socioeconomic class, unemployment, not having a stable relationship, signs of anxiety and depression, abuse or addiction of psychoactive substances, lack of perceived social support, comorbidities, HIV related hospitalizations and a CD4+ cell count less than 350, which contradict and resemble with these study findings in some variables [19, 30].
Likewise, the study conducted in Irish, China and Uganda on similar topic revealed that general health, symptoms of HIV, co-morbidities, social support, employment, age, gender, educational level, alcohol intake, CD4 count and HIV-complications had an independent association with physical and psychological domain of quality of life that directly contributed for general quality of life [20, 31, 32]. Another study conducted in Iran at a different place by different time with similar focus publicized that gender, marital status, level of education, CD4+ count, and clinical stage of the disease had a significant effect on the quality of life of the patients [17, 24, 25].
Moreover, findings of the study conducted in the USA and other review studies revealed that comorbidity, limitations in activities, and victimization are significant risk factors for decreased physical and mental health-related quality of life. Social support and self-efficacy serve as protective factors although social support is only significant with mental health-related quality of life [33, 34].
Similarly, a study conducted in Coastal South India and Bangladesh has shown that the quality of life was high among males, younger patients, married participants, and pateints with variables such as higher socioeconomic status, longer duration of ART, elf-motivation to take ART, stage of HIV, absence of opportunistic infection and higher CD4 count [26, 27, 35].
Likewise, the study conducted in Felege Hiwot Referral Hospital, Bahir Dar and in Mekelle Town, Ethiopia reflected that unemployment, gender, poor adherence and being ambulatory were found to have a statistically significant association with health-related quality of life [20, 36].
5. STRENGTHS AND LIMITATIONS
This study data were collected by their caregivers and no discomfort was observed related to their confidentiality of information which can decrease the social desirability bias. Since, the study focused on only one hospital, these findings cannot be generalized to the entire population of the regions. Since the data were collected only by quantitative methods, it does not address the information that can possibly be addressed by qualitative methods. Therefore, in future, it is better if both qualitative and quantitative methods of data collections are considered.
CONCLUSION
Overall, a significant number of HIV/AIDS patients exist on the low level of health-related quality of life. The age, occupation, current CD4 count level, current WHO stage status, general health conditions, comorbidity conditions, status of their social relations, their conditions due to lack of support, reminder of drugs taking time, and alcohol drinking status have a statistically significant association with health-related quality of life of patients.
LIST OF ABBREVIATIONS
| AIDS | = Acquired Immunodeficiency Syndrome |
| AOR | = Adjusted Odds Ratio |
| ART | = Antiretroviral therapy |
| CI | = Confidence interval |
| COR | = Crude Odds Ratio |
| HAART | = Highly active antiretroviral therapy |
| HIV | = Human Immune Deficiency Virus |
| HRQoL | = Health-related quality of life |
| JUSH | = Jimma University Specialized Hospital |
| OI | = Opportunistic Infections |
| PLWHA | = People Living with HIV/AIDS |
| QoL | = Quality of life |
| WHO | = World Health Organization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Before the data collection, Ethical clearance and approval were obtained from the Ethical Review Committee of College of Public Health and Medical Sciences, Jimma University to conduct this research by taking verbal consent from the participants. Permission was obtained from Jimma University Specialized Hospital to conduct the study.
HUMAN AND ANIMAL RIGHTS
No animals/ humans were used for the studies that are basis of this research.
CONSENT FOR PUBLICATION
Prior to questionnaires administered, the aims and objectives of the study were clearly explained to the participants and oral informed consent was obtained from each study participants since written consent was not feasible and practiced for survey study. Confidentiality was ensured throughout the execution of the study. The names of participants were not asked and a code was used instead of their name. Participants have been informed that their participation was voluntary and that they can withdraw from the study at any time if they wish to do so. The participants were also informed as their involvement was based on volunteer participation or refusing to participate had no link with the services they received.
AVAILABILITY OF DATA AND MATERIALS
The datasets that used in this study for analysis and other information are currently with corresponding author and principal investigator. Therefore, they can provide the data if requested.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
FUNDING
This study was done by Jimma University financial support received by Tamiru Tesfaye. However, the funder had no role in overall activities in the study such as; in the study design, data collection and analysis. Finally, the funder had no role in the decision to publish, or preparation of the manuscript for publication.
AUTHORS' CONTRIBUTIONS
TT is the principal investigator. TT, TB and AA conceived and designed the study. JD assisted the design of the study. TT and JD analyzed the data and interpreted the results. TT and JD prepared and critically reviewed the manuscript. All authors have read and approved the manuscript.
ACKNOWLEDGEMENTS
We would like to acknowledge Jimma University for supporting this study financially. Our thanks also extended to Jimma University specialized Hospital manager and Staff for their cooperation. In addition, our heartfelt thanks also extended to study participants who shared their priceless time to give information. Again, we acknowledge data collectors for their full commitment during data collections. Last but not the least, our gratitude extends to our families, friends and colleagues for all their support and encouragement during the conduction of this study.
DISCLOSURE
“Part of this article has previously been published in HIV positive sero-status disclosure and its determinants among people living with HIV /AIDS following ART clinic in Jimma University Specialized Hospital, Southwest Ethiopia: a facility- based cross-sectional study, Archives of Public Health 76.1 (2018): 1.”


