RESEARCH ARTICLE
The Influence of Social Media Lifestyle Interventions on Health Behaviour: A Study on Patients with Major Depressive Disorders and Family Caregivers
A. Jattamart1, A. Leelasantitham1, *
Article Information
Identifiers and Pagination:
Year: 2019Volume: 12
First Page: 387
Last Page: 405
Publisher ID: TOPHJ-12-387
DOI: 10.2174/1874944501912010387
Article History:
Received Date: 08/06/2019Revision Received Date: 23/08/2019
Acceptance Date: 13/09/2019
Electronic publication date: 30/09/2019
Collection year: 2019

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: (https://creativecommons.org/licenses/by/4.0/legalcode). This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
The World Health Organisation (WHO) predicts that depression will be the second leading cause of diseases by 2020. If depression is not properly treated, it can develop into a depressive disorder and increase the risk of suicide.Besides biopsychosocial factors, lifestyle is said to be a major cause of this disease and has led to an increase in its prevalence.
Objective:
The objective of this study was to study the intentions of patients with major depressive disorders and family caregivers to change their health behaviour and lifestyle through social media influences.
Methods:
This was a cross-sectional study. Participants were invited to take part in the research and give their informed consent. The sample consisted of 157 patients diagnosed with major depressive disorders, aged 18 years and over, and 110 family caregivers. Data were collected from the questionnaires designed according to the I-Change Model (ICM). Statistical results to confirm causal relationships were analysed based on Structural Equation Modelling (SEM) and by using the SmartPLS 3 software.
Results:
Patients and family caregivers were questioned about their perspectives on health matters and the influence on their motivations and intentions to change patients’ health behaviour and lifestyle, particularly social media interventions. The patients received information and counselling about health matters, health awareness, motivation and their intentions to change their health behaviour. The family caregivers were presented with the same information and counselling to motivate them to influence the depressive patients’ intentions to change their health behaviour.
Conclusion:
It is possible that lifestyle interventions on social media can influence the intention to change health behaviour in both patients and caregivers. However, if the patient lacks interest in participating in the treatment and does not have a good relationship with the clinician or provide relevant information to the experts; this can be an obstacle to changing their health behaviour. Therefore, future research should be conducted to ascertain which interventions are appropriate for patients and to study the long-term effects of any risks from using social media in patients with major depressive disorders.
1. INTRODUCTION
The World Health Organisation (WHO) predicts that by 2020, depression will be the second most common illness in the world and a major cause of disability-adjusted life year (DALY) – one DALY can be thought of as one year loss of the healthy life. Depression is predicted to be a major mental health problem in the population of Thailand [1]. According to a report of Adjaye-Gbewonyo, Rebok [2] that confirms the impact of depression on the DALY of the older adult population. If it is not properly treated, it can develop into a depressive disorder and patients can suffer from depressive moods, which can lead to chronic impairments [3]; it can also increase the risk of suicide [4].
Clinical Practice Guidelines of Major Depressive Disorders begin with screening and case-finding (as shown in Section 1.1 Pre-Diagnosis) in order to isolate people at risk or in the early stages of treatment as soon as possible. Once found, the risk population undergoes diagnosis by a psychiatrist (as shown in Section 1.2 Diagnosis) to find the cause and explain the abnormalities of the disease in patients. After that, it describes the treatment process which aims to make no residual symptoms through medication and various forms of therapy including health behaviour interventions (Section 1.3 Lifestyle Intervention with Major Depressive Disorder (Post-Diagnosis)), which is a tool used to reduce problems and obstacles to the treatment of diseases. However, another important issue is the change in health behaviour that is described in Section 1.4. This can help to reduce the health risk behaviours of those people who are in the risk groups identified in Section 1.1, and who can be supported by the treatment procedures described in Section 1.3. Therefore, the research is interested in conceptual modelling of behaviour modification to obtain a new model to explain the acceptance of lifestyle interventions using social media, with the intention of changing health behaviours from the perspective of depressed patients and family caregivers.
1.1. Pre-Diagnosis
Pre-Diagnosis explains the screening and evaluation of clinical results from risk populations to proceed with disease diagnosis process which uses tools to screen for depression. The currently depression screening is used in conjunction with digital platforms and online media especially in social media that found relationship between using social media and health has received considerable attention. People with health problems and general users use social media to promote health and increase their knowledge of particular conditions. This is known as Health Information-Seeking Behaviour (HISB) [5]. Instead of direct inquiries from experts, young users tend to show HISB [6]. They also share their experience of certain diseases and promote mental health through sharing advice on mental health problems [7], increasing their social support network [8]. HISB is influenced by motivation, awareness, and perceptions of health and behaviour [9] and is indicative of how personal characteristics play a role in promoting health.
With regard to people at risk of mental health problems, there is evidence that social media and information technology can be used to quickly assess and screen high-risk patients for treatment and follow-up. The evaluation and screening of high-risk patients is done by a group of medical personnel who assess symptoms based on user-generated content (UGC) obtained from patients [10]. Such content helps the professionals predict levels of mental illness and its prevalence by using artificial intelligence to develop a user-level mental model [11]. This model uses text-mining technology to examine the text on web posts, web blogs, micro-blogs, forums, bulletin board systems or other media [12] and can serve as a screening channel for depression [13]. This also helps to assess the risk of depression in pregnant women who are at risk by examining the content posted by users on platforms and testing it with a tool designed for depression screening (The Edinburgh Postnatal Depression Scale (EPDS)). Women with an EPDS score of 13+ are more likely to post words related to mental health conditions [14]. Therefore, this shows that digital platforms and social media may be used to assess the risk of depression.
1.2. Diagnosis
From the effects of the depressive disorder described above when explaining the cause of the disease, it is found that there are complex causes that can help to understand the risk factors for the disease. This will support those involved in treatment with regard to understanding and explaining the patient’s disorder. That is why specialists develop biopsychosocial models to help in the search for factors related to the treatment process [15] which are caused by biological issues such as stress, gene abnormalities, abnormal neurotransmitters [16] [17], psychological influences (personality, behaviour) [18, 19] and social factors (social and environmental support) [20-22]. Lifestyle can also be a major cause of the disease. Treatment [23] includes: 1) improving the quality of diet which can help to reduce the risk of depression by 35% [24], 2) introducing an exercise programme after a CES-D assessment [25] and 3) improving sleeping patterns, because insomnia is a major problem for depressed patients as it affects the brain structure and neurogenesis [26].
In addition, there are reports that confirm the relationship between depression and physical illness. This includes a longitudinal study of the relationship between depressive symptoms and Coronary Heart Disease (CHD), which is the number one cause of death in the world population, which confirms that depression can predict CHD [27], or a report that shows that in the case of patients with depression, 18-27% have or will have prostate cancer [28]. However, depression can be prevented and cured. For this reason, the mental health service should pay attention to the treatment and prevention of depression by educating and adjusting behaviours in such a way as to reduce risk factors for disease and disease severity.
Previous research has found that the relationship between the use of social media in a patient group helped the patients to participate in the treatment process [29], worked as a medium to share information and allowed them to comment on mental health service providers [30, 31] and to develop a health service system through social media [32, 33]. It is also used as a tool to communicate and exchange useful information between different medical groups [34, 35] based on ethical requirements, privacy laws, confidentiality and professional codes of practice [36]. It also includes the use of Behavioural Intervention Technologies (BITs) comprising web-based interventions, mobile technologies, social media (discussion groups, social networking), virtual reality and web-based games [37], all of which are used in the process of behavioural and psychological intervention. This includes cognitive and affective methods that support behavioural, physical and mental health while also tracking their long-term effects. It has also been found to be effective in face-to-face therapy [38].
Online intervention in health behaviour is a strategy for improving the sustainable treatment of patients with the goal of correcting problematic behaviour that is a barrier to the treatment of disease and optimal health and well-being [39]. This is important for the development of public health. It also helps to reduce travel restrictions, such as the cost of transporting medical supplies and access to people in remote areas [40, 41]. Studying online intervention in health behaviour is challenging for researchers and those involved in learning about the social psychology factors, behaviour, and the process of behavioural change in individuals and various groups because it is difficult to know when online health behaviour interventions have occurred.
1.3. Lifestyle Intervention with Major Depressive Disorder (Post-Diagnosis)
Online health behaviour interventions are used as a tool to prevent problems and reduce the obstacles to the treatment of diseases in people with mental illnesses. Internet-based studies on the effect of depression in adolescent mothers tested the intervention behaviour using variables based on the Theory of Planned Behaviour (TPB) and found that it affects the attitudes and perceptions, and controls the intention to improve health behaviour [42]. Compared to controlled interventions, internet interventions including psychoeducation websites and websites offering cognitive behaviour therapy, have been shown to help reduce levels of depression using the Centre for Epidemiologic Studies Depression Scale (CES-D) [43]. Evaluating the characteristics of Technology-Based Interventions (TBIs) effect on anxiety, depression, and health-related quality of life in patient groups with prostate cancer, the results indicated that the patient group controlled by the TBI platform had a reduced level of depression [28]. Facebook supports changing the health behaviour of depressed patients [44] and has used interventions including Facebook groups to support lifestyle interventions for weight loss and physical activity in patients with serious mental illnesses. Various studies confirm the use of Facebook as a tool to support lifestyle interventions for weight loss in those who are obese and have mental illnesses [44]. Therefore, we can conclude that social media in the form of Internet Support Groups (ISGs), resources and discussion groups can be used to promote health behaviour [37].
These findings show that changes in health behaviour that focus on the lifestyle of patients with mental health disorders are integrated within social media, and can influence depressed patients’ attitudes, perceptions, and intentions to access health care. However, there is little evidence to show that social media has an impact on changes in health behaviour and there are no studies on the factors that are directly related to the behavioural modification process of a person's health. In addition, there are no studies on interpersonal relationships which have an important role in interventions to change personal health behaviour both in face-to-face and online therapy [45]. Any evaluation of the treatment processes requires information from the family caregiver, which has also been lacking.
| Model / Theory | Definition | Constructs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Information | Environment | Awareness | Motivation | Barriers | Action | ||||||
| Perception | Cues to Action | Attitude | Social Influence / Subjective Norm | Self-Efficacy / Behavioural skills | Intention | Behaviour | |||||
| Health Belief Model (HBM) [46] | Studies the relationship between the health behaviours of individuals and medical and public health services. Considers relevant factors as 1) perceived susceptibility, 2) perceived severity, 3) perceived threat, 4) perceived benefits and barriers, and 5) cues to action. | - | - | / | - | - | - | - | / | - | / |
| Protection Motivation Theory (PMT) [48] | Used to evaluate health information awareness that leads to prevention methods. The related factors are: 1) perceived severity, 2) perceived susceptibility, 3) response efficacy and 4) self-efficacy. | - | - | / | - | - | - | / | - | / | / |
| Social-Cognitive Theory (SCT) [47] | Used to study behavioural changes resulting from learning, by observing or imitating. The relevant factors are 1) personal, 2) environment, and 3) behaviour. | - | / | - | - | - | - | - | - | - | / |
| Theory of Reasoned Action (TRA) [49] | Used to study changes in personal behaviour considering the rational actions caused by, 1) attitude toward behaviour, and 2) subjective norm. | - | - | - | - | / | / | - | - | / | / |
| Theory of Planned Behaviour (TPB) [50] | Used to study changes in behaviour of individuals resulting from intentions that lead to behaviours caused by, 1) attitude, 2) subjective norm, and 3) perceived behavioural control. | - | - | / | - | / | / | - | - | / | / |
| Attitude-Social influences- Self-Efficacy (ASE-model) [51] | Used to describe various health behaviours. The relevant factors are, 1) attitude, 2) social influence and 3) self-efficacy. | - | - | - | - | / | / | / | - | / | / |
| Information Motivation Behavioural skills theory (IMB) [52] | Used to study the changing behaviour of individuals by considering information, motivation and behavioural skills that result in changes in the behaviour of individuals. | / | - | - | - | / | / | / | - | - | / |
Currently, there are many concepts and theories that try to explain the health behaviour and give importance to the cognitive perspective of the people who are affecting the behavioural change. Therefore, it is important to consider using these concepts and theories in accordance with the objectives being studied. The cognitive perspective for describing health behaviour is shown in Table 1. However, there are limitations to using these concepts and theories in cases where the behaviour is complex, as can be seen from using the Health Belief Model (HBM) [46] and Social-cognitive Theory (SCT) [47]. They do not include a study on the factors that cause motivation (social influence, self-efficacy/behavioural skills, attitude), or the information and intention that affect behaviour. Protection Motivation Theory (PMT) [48], the Theory of Reasoned Action (TRA) [49], the Theory of Planned Behaviour (TPB) [50] and the Attitude-Social influences-Self-Efficacy model (ASE-model) [51] do not explain the information, environment and barriers that affect the intention and behaviour of individuals. Therefore, when studying health behaviour it is important to consider the factors that influence the cognitive perspective of the person under study.
1.4. I-Change Model
The I-Change Model (ICM) addresses the limitations of the behavioural models (Theory of Planned Behaviour (TPB), Attitude-Social Influence-Self-efficacy (ASE)) [50] and improves the ability to explain the factors that influence the health behaviour modifications which are a result of compre- hensive intentions to predict future changes in health behav- iour. The factors related to health behaviour modification include: 1) Predisposing factors related to demographic characteristics such as behavioural, psychological, biological, social and cultural (in which previous research found differences in the demographic characteristics which affected the variability in the use of social media) [53], 2) Information factors related to health counselling and information, 3) Awareness factors related to awareness of good health and appropriate practices of individuals based on knowledge, action cues and risk perceptions, 4) Motivation factors concerning attitudes, social influences and self-efficacy to practice various behaviours, 5) The intention to support behavioural change which is the main factor in predicting future behaviour modification, 6) Ability factors involved in planning for future behavioural changes 7) Barriers that restrict behavioural change and 8) Behavioural state which modifies that behaviour (Fig. 1).
The ICM was introduced as a conceptual framework to predict smoking cessation behaviour which was influenced by helpful tailored advice, personal motivation and psychological intervention [54-56]. It has been used to study the psychosocial factors that predict eating in moderation, resulting from an awareness of the risk behaviour of individuals [57]. It has also been used to study the skills and knowledge of nurses and provide them to pregnant women and their partners who are concerned about alcohol consumption during pregnancy [58]. In addition, ICM has been used to study behavioural interventions that explore motivation and changes in the risk behaviour of people with Familial Hypercholesterolemia (FH) based on a control group and an intervention group. The researchers found that it was helpful to improve awareness of the risk of disease by increasing knowledge and risk perception, and also by increasing motivation to encourage health behaviours which help reduce the risk of cardiovascular diseases [59]. It has also been used in web-based interventions to promote Physical Activity (PA) in adults with Type 2 diabetes by integrating it with the factors that influence behavioural change. A study was carried out to assess the effectiveness and acceptance of its use and it was found that it is important to develop and tailor web-based interventions and evaluate the ability to use it before implementation [60]. Although the ICM has been used in extensive study on health behaviours, it was only used to explain the opinions and the direction of the relationship between the variables studied (as shown in Table 2). Therefore, there is a need to explain the relationships more clearly. This led to the study on the intention ‘to go to bed’, for example which resulted from personal awareness and motivation. It explains the causal relationship between external and internal variables (or between latent variables) to test the consistency of the model and the theory applied. ICM was previously introduced to study the awareness and motivation to predict the intention of ‘bedtime’ in the form of a structural equation model based on the red frame [61] (Fig. 1). It has also been used to integrate with the information–motivation–behavioural skills model (IMB) to predict the motivation to use condoms during sexual intercourse in the form of a structural equation model based on the blue frame [62] (Fig. 1).
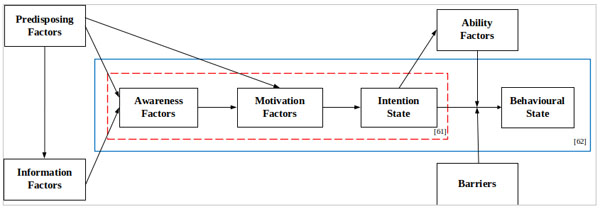 |
Fig. (1). I-Change Model [50]. |
| Behavioural Change | ICM factors | Statistical Analysis | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Predisposing | Information | Awareness | Motivation | Intention | Barriers | Ability | Behavioural | ||
| Smoking cessation | / | - | / | / | / | - | / | / | Multivariate linear regression analyses, multivariate and univariate regression analyses [54]. |
| Smoking prevention | / | - | / | / | / | - | / | / | Multilevel logistic regression analyses [55, 56]. |
| Eating in moderation | / | - | / | / | / | - | - | - | Logistic regression analysis, independent samples t-tests, crosstab analyses and multiple linear regression analysis [57]. |
| Lifestyle intervention | / | - | / | / | / | - | / | - | Multiple linear and logistic regression analysis [59]. |
| Aerobic physical activity | / | / | / | / | / | - | / | / | Evaluating Web-based intervention [60]. |
| Alcohol consumption in pregnancy | / | / | / | / | / | - | / | - | Descriptive statistic [58]. |
| Going to bed early | / | - | / | / | / | - | - | - | Pearson correlations and Structural Equation Modelling (SEM) [61]. |
| Condom use | / | - | / | / | / | - | - | / | Bivariate correlations and Structural Equation Modelling (SEM) [62]. |
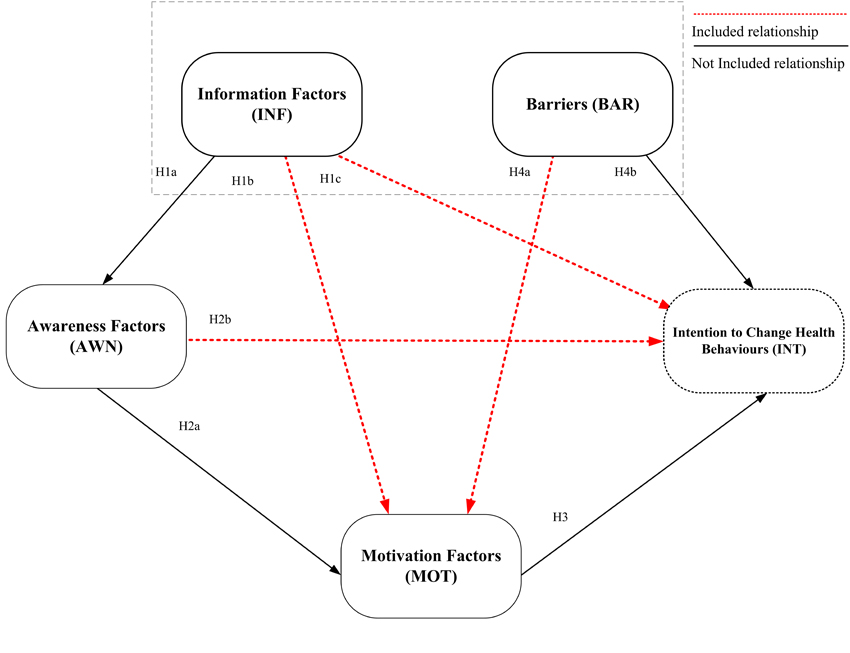 |
Fig. (2). Proposed SMLI model based on the I-change model. |
It can be seen that the ICM has been used to describe the online health behaviour interventions of patients. It can help us to understand the psychosocial factors that influence comprehensive behavioural changes. However, the ICM was not used in previous research to study social media and the health behaviour interventions of depressed patients. There was no acknowledgement of interpersonal relationships or how social media interventions changed health behaviour. Therefore, it is necessary to ascertain if there is any consistency between the ICM variables and the social media health behaviour interventions in the form of structural equations. This can help us to understand the psychosocial factors that influence appropriate behavioural changes.
1.5. The Research Study
The purpose of this study is to ascertain the influence of Social Media Lifestyle Interventions (SMLI) on health behaviour from a study on patients with major depressive disorders and family caregivers and to confirm any consistencies between the ICM and SMLI in the form of a structural equation model.
2. MATERIALS AND METHODS
2.1. Conceptual Model
The main objective of this research is to predict the intentions of patients to change their health behaviour resulting from the acceptance of SMLI. It uses the social media classification criteria of Grajales III and Sheps [36] which focuses on the popular social networking and media sharing sites and Microblogs (Facebook, Instagram, YouTube, Twitter and Line) that use health care interventions. The ICM framework is used to explain the intentions that lead to the most predictable behaviour [63] and to focus on the factors that influence cognitive perspectives and changes in health behaviour. Factors tested include Information Factors (INF), awareness factors (AWN), motivation factors (MOT), barriers (BAR), and Intention to Change Health Behaviours (INT). Fig. (1) shows that intention is primarily responsible for ability factors and behavioural state to predict future behaviour changes. Therefore, in order to monitor future behaviour changes, it is first necessary to understand the intentions of the person. As this is a cross-sectional study, it does not explain the ability factors and behavioural states. In addition, further studies based on the ICM include the relationship between INF and MOT, INF and INT, AWN and INT and the relationship between BAR and INT. The proposed SMLI model based on the I-change model is shown in Fig. (2).
2.2. Hypotheses
The relevant factors of ICM are described as follows:
The predisposing factors related to demographic characteristics are 1) behavioural factors (lifestyle, eating behaviour, health status, smoking behaviour) [64], 2) psychological factors (personality), 3) biological factors (gender, genetic), and 4) Social and cultural factors (price of cigarettes, policies) [65]. Previous studies found that differences in age, gender, status, relationship, and health problems affect the perception and behaviour of individuals using social media both positively and negatively [66, 67].
Information factors are 1) Messages (content suggestion, content type and the quality of information that affects feelings and awareness of health), 2) Channels (this relates to the channel used to receive health information) and, 3) Sources, (relates to the sources from which the health information is obtained). Regarding the relationship between the content on social media, it was previously found that when the content creators and readers have a close relationship, the emotional responses and feelings are more effective [68]. This includes information from health professionals which is acceptable to most readers [69]. The form of the content (likes, comments/poll votes, and views) also influences participation of the readers [70]. Therefore, this study examines the information and advice about participating in secret groups and seeking health information from social media lifestyle interventions. For this reason, the following hypotheses are proposed:
- H1a: Information factors have a positive influence on awareness factors in changing the behaviour of patients' health as a result of accepting social media lifestyle interventions.
- H1b: Information factors have a positive influence on motivation factors in changing the behaviour of patients' health as a result of accepting social media lifestyle interventions.
- H1c: Information factors have a positive influence on intentions to use social media to change the behaviour of patients' health as a result of accepting social media lifestyle interventions.
Awareness factors are related to awareness of good health and appropriate practices and are evaluated from 1) knowledge related to behaviour that causes health hazards [71], 2) cues to actions related to what induces people to change their behaviour (price, personal satisfaction) [61, 72] and 3) risk perceptions from experiencing unwanted side effects and the severity of danger or illness when performing inappropriate behaviour [57]. Therefore, this study examines the information and advice given about the awareness of a proper lifestyle after joining a secret group, and about seeking health information from social media lifestyle interventions. Therefore, its hypotheses are as follows:
- H2a: Awareness factors have a positive influence on motivation factors in changing the health behaviour of patients as a result of accepting social media lifestyle interventions.
- H2b: Awareness factors have a positive influence on patients' intention to change health behaviour as a result of accepting social media lifestyle interventions.
Motivation factors assess the advantages and disadvantages of behaviour change and consist of 1) attitude, which is the measure of a person's attitude toward behaviour change, 2) social influence, this is whether a person in a society or social support encourages the change in behaviour and, 3) self-efficacy, which is an assessment of the perception of difficulty or ease in changing the behaviour [73, 74]. Therefore, this study explains the motivation to change health behaviour when joining a secret group and when seeking health information from social media lifestyle interventions. Therefore, its hypothesis is as follows:
- H3: Motivation factors have a positive influence on patients' intentions to change health behaviour as a result of accepting social media lifestyle interventions.
In this study, barriers refer to the behaviour modification limitations assessed by participation in treatment and communication relationships and by providing useful information to experts regarding the treatment [75].
- H4a: Barriers influence motivation factors in changing patient’s health behaviour as a result of accepting social media lifestyle interventions.
- H4b: Barriers influence patients' intentions to change health behaviour as a result of accepting social media lifestyle interventions.
Intention factors refer to the intention to support that behavioural change. This is measured by the current response of the person to changing the behaviour in various ways, including giving advice to others, the intention to act on their own or the intention to use the advice given [64, 76]. This study focuses on the intention to change the health behaviour of patients by using SMLI. The proposed hypotheses of the study are shown in Table 3.
The proposed hypotheses of the study are shown in Table 3.
2.3. Participants
This is a cross-sectional study using purposive sampling based on the characteristics of the sample of patients who met the criteria and objectives of the research. It consisted of patients diagnosed with mild and moderate levels of a major depressive disorder. Patients with severe levels of a depressive disorder were eliminated from the study. All the patients were assessed by a nine-question assessment tool (9Q scale) [77]. 157 patients over the age of 18 years and who were able to read and write in Thai language and 110 family caregivers were selected. Data were collected from a hospital in Thailand during the period July 2018 to January 2019. The research process was approved by The Centre of Ethical Reinforcement for Human Research, Mahidol University, Thailand (MU-CIRB 2018/058.0503). Individuals were invited to participate in the research. The purpose of the study was clarified by a research assistant who gave out information sheets to the participants and assured them that any information collected would be confidential. The questionnaire issued to the respondents did not contain any identifiable information. Participants were told that they could withdraw from the research at any time and that the questionnaires would be destroyed after the project was completed [78]. All the participants in the research project gave their informed consent.
2.4. Measurement Instrument
The questionnaire was designed based on the ICM theory framework and consisted of six parts: Part 1: predisposing factors of the participants; Part 2: information factors; Part 3: awareness factors; Part 4: motivation factors; Part 5: barriers factor and Part 6: factors related to the intention to change the behaviour. It was measured and evaluated according to the Likert 5 criteria: Level 1 (strongly disagree) to 5 (strongly agree) and was divided into two sets. Questionnaire series 1: Collect data from the patients before starting the questionnaire. The clinical psychologist or psychiatric nurse assessed their readiness to complete the questionnaire using the Thai Mental State Examination (TMSE) form [79]. After talking with the patients, the clinical psychologist or psychiatric nurse wrote out their responses to assess them and prevent them from being asked any questions that may stimulate their condition and to assess the situation prior to the questionnaire phase by interviewing one person at a time for no more than 15 minutes at a time. Questionnaire series 2: Collect information from related individuals with experience of caring for patients for at least six months. Both the patients and family caregivers were asked the same questions, as shown in Table 4.
2.5. Data Analysis
The analysis of causal relationships was carried out using the partial least squares structural equation model (PLS-SEM) which uses a variance-based structural equation model (variance-based SEM). Testing was carried out using the SmartPLS software V.3.2.8 [82] to test the concept of education in each factor. PLS-SEM in the SmartPLS software does not operate under restrictive assumptions about data distribution since it is non-parametric and is effective in predicting the relevant elements to be used to test the theory [83, 84]. For example, it has been used to study the following; the behaviour of social media users [85], the leadership behavior of employees for information systems security [86], education [87] and business studies [88] including the study on health behaviours with a view to prevent diseases [89] and the impact on mental health problems [90]. PLS-SEM can analyse the results of measurement models and structural models simultaneously. It is suitable for testing small and medium samples [91] and can provide results for the accuracy of the content and the accuracy of the classification with Composite Reliability (CR) and average variance (AVE) statistics [92]. For these reasons, PLS-SEM is the most suitable model for this study. The results of the PLS-SEM analysis of the patient and family caregiver information are presented in the form of measurement and structural models.
3. RESULTS
3.1. Descriptive Statistics
The random sampling of 186 depressive patients produced 157 complete data sets (14 were screened out, nine were unqualified, and six were incomplete). Of 139 family caregivers, 110 had complete data (15 were unqualified and 14 were incomplete). The demographic characteristics of the participants are listed in Table 5.
3.2. Measurement Model
After the examination of the quality of variables according to the criteria described in a study [93] and the list of questions in the first set of questionnaires (patients), it was found that all the Composite Reliability (CR) values were between 0.875-0.896 (with the value not less than 0.7). Cronbach's α values were between 0.757-0.848, and these values were in accordance with the value which was not less than 0.7. The Average Variance Extracted (AVE) values were between 0.568-0.780 (with the value not less than 0.5). The results of the quality of the variables and the questions from the list of questionnaires in set 2 (family caregivers) found that the Composite Reliability (CR) value was between 0.879-0.919, and Cronbach's α value was between 0.770-0.897. The Average Variance Extracted values (AVE) were between 0.647-0.813 as shown in Table 6.
The questions used in the measurement of quality questionnaires passed all the weight values criteria. According to the criteria, the values not less than 0.7 showed reliability of the questions used in the measurement. The first set of questionnaires (patients) had a weight between 0.730-0.968 and the second questionnaire (family caregiver) had a weight between 0.72-0.907. Fornell-Larcker [94] criteria were also used to evaluate the relationship between the variables in the form of a diagonal matrix, which found that the square roots of the AVEs in each construct (bold letters) were greater than the values in the horizontal row and corresponding rows. This indicated that the variables were categorical (Discriminant Validity), as shown in Tables 7 and 8.
3.3. Structural Model
This study examined the fit of the model before testing with path coefficient significance based on the structural model and criteria set by Hair Jr and Hult [93], and Henseler and Hubona [95]. It was evaluated using the Stone-Geisser Q2 process of blindfolding. For the Awareness Factors (AWN) (Q2=0.026), Motivation Factors (MOT) (Q2=0.088) and Intention to Change Health Behaviours (INT) (Q2=0.245), the result was greater than 0, indicating that the construct is relevant in accordance with the predictive relevance of the model. The value of the standardised root mean square residual (SRMR) was measured - the acceptable criteria must be lower than 0.08 (and was 0.077 for our model). The suitability of the model was assessed based on the value of Goodness-of-Fit (GoF) which was 0.37. This passed the acceptable criteria (which must be higher than 0.36) [96]. All this indicates that the model is a good fit.
The testing of the structural model from the resampling of patient data using the bootstrap method for the 5,000 list generated an approximate estimation for increasing confidence by analysing the relationship between the constructs [93]. The multicollinearity tests with the VIF values found that the causal variables do not correlate above the threshold of 3.3 [93]. When considering the value of the path coefficients, the p-value and t-value corresponded to the t-value which was higher than 1.96 (significance level=5%), 2.58 (significance level=1%), and 3.29 (significance level =0.1%) [93]. This means that hypothesis H1a is accepted: Information Factors (INF) have a positive influence on Awareness Factors (AWN) at a significance level of 0.01 (β = 0.224, t=2.899); H1b is accepted: Information Factors (INF) have a positive influence on the Motivation Factors (MOT) at a significance level of 0.05 (β = 0.178, t=2.318); H1c is accepted: Information Factors
| Hypothesises | Factors | ||||
|---|---|---|---|---|---|
| Information Factors | Awareness Factors | Motivation Factors | Barriers | Intention Factors | |
| H1a | / | / | - | - | - |
| H1b | / | - | / | - | - |
| H1c | / | - | - | - | / |
| H2a | - | / | / | - | - |
| H2b | - | / | - | - | / |
| H3 | - | - | / | - | / |
| H4a | - | - | / | / | - |
| H4b | - | - | - | / | / |
| Construct | Items | Survey Item | References |
|---|---|---|---|
| Predisposing Factors | - | Gender, age, education, experience of social media usage, social media platform used and total time per day (hours). | Adapted from [80] |
| Information Factors (INF) | INF1 | ‘Advice from experts, friends and relatives makes me interested in joining a secret group and in seeking health information and lifestyle interventions through social media.’ | Adapted from [71, 74, 81] |
| Information Factors (INF) | INF2 | ‘Advice from other participants on social media influences my health behaviour.’ | Adapted from [71, 74, 81] |
| INF3 | ‘Joining a secret group and seeking health information from social media interventions allowed me to share lifestyle experiences such as food menus, exercise methods and sleeping patterns, which is useful to other participants.’ | ||
| INF4 | ‘Joining a secret group and seeking health information and interventions on social media have allowed me to get information and advice on how to live healthier including helpful food menus, exercise and getting enough sleep.’ | ||
| Awareness Factors (AWN) | AWN1 | ‘I perceive the benefits of joining a secret group and seeking health information for depressive diseases by seeking lifestyle interventions on social media that will encourage good health behaviour.’ | Adapted from [58, 61, 71, 72] |
| AWN2 | ‘I acknowledge that joining a secret group and seeking health information about depressive diseases by interacting on social media helps me to contact and exchange information with other participants.’ | ||
| AWN3 | ‘I perceive that I can find health and lifestyle information such as food menus, exercise methods and sleeping patterns by participating on social media.’ | ||
| AWN4 | ‘I can learn to join a secret group and seek health information about depressive diseases by quickly interacting on social media.’ | ||
| AWN5 | ‘Joining a secret group and seeking health information will help stimulate me to improve my healthy behaviour.’ | ||
| AWN6 | ‘My personal technology preferences made me interested in joining a secret group and seeking health information by interacting on social media.’ | ||
| Motivation Factors (MOT) | MOT1 | ‘I think that joining a secret group and seeking health information about depressive diseases is beneficial for my health habits.’ | Adapted from [72, 73, 74, 76, 81] |
| MOT2 | ‘The support from experts, friends and relatives contributed to my decision to use secret groups and to seek health information about depressive diseases by interacting on social media.’ | ||
| MOT3 | ‘Experts, friends and relatives have encouraged me to use secret groups and seek health information about depressive diseases by interacting on social media.’ | ||
| MOT4 | ‘I think it is easy to use secret groups and seek health information about depressive diseases by interacting on social media.’ | ||
| MOT5 | ‘I think I will get the right information and be safe when using secret groups and seeking health information about depressive diseases while interacting on social media.’ | ||
| Barrier (BAR) | BAR1 | ‘I cooperate with and follow the advice of experts on the use of secret groups and seeking health information about depressive diseases when interacting on social media.’ | Adapted from [75] |
| BAR2 | ‘I cooperate with experts by providing information related to treatment.’ | ||
| Intention to Change Health Behaviours (INT) | INT1 | ‘I accept the guidelines for the development of a lifestyle intervention model on social media to change health habits both in the form of secret groups and in finding health information about depression.’ | Adapted from [54, 81] |
| Intention to Change Health Behaviours (INT) | INT2 | ‘I am ready to change my health habits during the next six months to help develop a lifestyle intervention programme using social media.’ | Adapted from [54, 81] |
| INT3 | ‘I intend to change my health behaviour in the next six months if there is a development programme of intervention on social media.’ |
| Characteristics | Patients (n=157) | Family Caregivers (n=110) | ||
|---|---|---|---|---|
| Number | Percentage | Number | Percentage | |
| Gender | ||||
| Male | 36 | 22.9 | 31 | 28.7 |
| Female | 121 | 77.1 | 77 | 71.3 |
| Age (years) | ||||
| 18-25 | 35 | 22.3 | 7 | 6.5 |
| 26-35 | 77 | 49.0 | 34 | 31.5 |
| 36-45 | 39 | 24.8 | 45 | 41.7 |
| 46-55 | 6 | 3.8 | 22 | 20.4 |
| Education level | ||||
| High school or less | 21 | 13.4 | 13 | 12 |
| College | 71 | 45.2 | 50 | 46.3 |
| BA or higher | 65 | 41.4 | 45 | 41.7 |
| Experience of using Social media (hours) | ||||
| Less than 1 year | 15 | 9.6 | 21 | 19.4 |
| 1-3 years | 51 | 32.5 | 33 | 30.6 |
| 3 years and above | 91 | 58.0 | 54 | 50 |
| Social Media Platforms used | ||||
| 152 | 96.8 | 99 | 91.7 | |
| 28 | 17.8 | 22 | 20.4 | |
| 25 | 15.9 | 12 | 11.1 | |
| Line | 151 | 96.2 | 69 | 63.9 |
| YouTube | 89 | 56.7 | 87 | 80.6 |
| Total time per day (hours) | ||||
| Less than 1 hour | 6 | 3.8 | 7 | 6.5 |
| 1-3 hours | 78 | 49.7 | 14 | 13 |
| 3-5 hours | 31 | 19.7 | 78 | 72.2 |
| 5 hours and above | 42 | 26.8 | 9 | 8.3 |
| Construct | Composite Reliability (> 0.70) |
Cronbach's α (> 0.70) |
AVE (> 0.50) | |||
|---|---|---|---|---|---|---|
| Patients | Family Caregivers | Patients | Family Caregivers | Patients | Family Caregivers | |
| Information Factors (INF) | 0.889 | 0.879 | 0.833 | 0.819 | 0.667 | 0.647 |
| Awareness Factors (AWN) | 0.888 | 0.919 | 0.848 | 0.897 | 0.568 | 0.655 |
| Motivation Factors (MOT) | 0.876 | 0.918 | 0.825 | 0.888 | 0.586 | 0.692 |
| Barrier (BAR) | 0.896 | 0.897 | 0.757 | 0.770 | 0.742 | 0.813 |
| Intention to Change Health Behaviours (INT) | 0.875 | 0.894 | 0.826 | 0.823 | 0.780 | 0.738 |
| Patients | ||||||
|---|---|---|---|---|---|---|
| Construct | Items | INF | AWN | MOT | BAR | INT |
| Information Factors (INF) | INF1 | 0.804 | 0.162 | 0.165 | -0.049 | 0.334 |
| INF2 | 0.852 | 0.184 | 0.211 | 0.003 | 0.324 | |
| INF3 | 0.831 | 0.203 | 0.269 | 0.067 | 0.283 | |
| INF4 | 0.779 | 0.184 | 0.183 | 0.037 | 0.291 | |
| Awareness Factors (AWN) | AWN1 | 0.130 | 0.756 | 0.373 | 0.222 | 0.379 |
| Awareness Factors (AWN) | AWN2 | 0.182 | 0.753 | 0.194 | 0.061 | 0.315 |
| A | AWN3 | 0.203 | 0.755 | 0.325 | -0.031 | 0.297 |
| AWN4 | 0.107 | 0.744 | 0.290 | 0.084 | 0.269 | |
| AWN5 | 0.193 | 0.784 | 0.264 | 0.022 | 0.304 | |
| AWN6 | 0.200 | 0.730 | 0.264 | 0.104 | 0.310 | |
| Motivation Factors (MOT) | MOT1 | 0.282 | 0.470 | 0.762 | 0.025 | 0.366 |
| MOT2 | 0.203 | 0.270 | 0.787 | 0.104 | 0.413 | |
| MOT3 | 0.135 | 0.231 | 0.779 | 0.254 | 0.289 | |
| MOT4 | 0.148 | 0.195 | 0.757 | 0.187 | 0.373 | |
| MOT5 | 0.171 | 0.243 | 0.742 | 0.023 | 0.323 | |
| Barrier (BAR) | BAR1 | 0.054 | 0.115 | 0.176 | 0.968 | 0.257 |
| BAR2 | -0.074 | 0.058 | 0.030 | 0.789 | 0.130 | |
| Intention to Change Health Behaviours (INT) | INT1 | 0.250 | 0.374 | 0.448 | 0.225 | 0.816 |
| INT2 | 0.435 | 0.389 | 0.388 | 0.151 | 0.904 | |
| INT3 | 0.277 | 0.311 | 0.366 | 0.253 | 0.863 | |
| Family Caregivers | ||||||
| Construct | Items | INF | AWN | MOT | BAR | INT |
| Information Factors (INF) | INF1 | 0.764 | 0.229 | 0.262 | 0.173 | 0.220 |
| INF2 | 0.828 | 0.099 | 0.287 | 0.168 | 0.174 | |
| INF3 | 0.893 | 0.198 | 0.341 | 0.252 | 0.253 | |
| INF4 | 0.724 | 0.177 | 0.194 | 0.172 | 0.079 | |
| Awareness Factors (AWN) | AWN1 | 0.287 | 0.832 | 0.190 | 0.186 | 0.145 |
| AWN2 | 0.130 | 0.802 | 0.187 | 0.064 | 0.168 | |
| AWN3 | 0.220 | 0.863 | 0.168 | 0.076 | 0.113 | |
| AWN4 | 0.083 | 0.744 | 0.108 | -0.051 | 0.034 | |
| AWN5 | 0.165 | 0.843 | 0.196 | 0.192 | 0.052 | |
| AWN6 | 0.090 | 0.765 | 0.159 | 0.106 | 0.111 | |
| Motivation Factors (MOT) | MOT1 | 0.331 | 0.232 | 0.833 | 0.278 | 0.419 |
| MOT2 | 0.326 | 0.119 | 0.846 | 0.365 | 0.403 | |
| MOT3 | 0.326 | 0.064 | 0.863 | 0.252 | 0.390 | |
| MOT4 | 0.250 | 0.147 | 0.857 | 0.290 | 0.460 | |
| MOT5 | 0.188 | 0.352 | 0.754 | 0.175 | 0.355 | |
| Barrier (BAR) | BAR1 | 0.198 | 0.110 | 0.295 | 0.897 | 0.258 |
| BAR2 | 0.237 | 0.137 | 0.304 | 0.907 | 0.276 | |
| Intention to Change Health Behaviours (INT) | INT1 | 0.238 | 0.139 | 0.459 | 0.263 | 0.841 |
| INT2 | 0.272 | 0.162 | 0.413 | 0.258 | 0.889 | |
| INT3 | 0.092 | 0.045 | 0.381 | 0.241 | 0.846 | |
| Patients | |||||
|---|---|---|---|---|---|
| Construct | INF | AWN | MOT | BAR | INT |
| Information Factors (INF) | 0.817 | ||||
| Awareness Factors (AWN) | 0.224 | 0.754 | |||
| Motivation Factors (MOT) | 0.255 | 0.385 | 0.766 | ||
| Barrier (BAR) | 0.018 | 0.107 | 0.146 | 0.883 | |
| Intention to Change Health Behaviours (INT) | 0.255 | 0.385 | 0.466 | 0.146 | 0.862 |
| Family Caregivers | |||||
| Construct | INF | AWN | MOT | BAR | INT |
| Information Factors (INF) | 0.778 | ||||
| Awareness Factors (AWN) | 0.041 | 0.788 | |||
| Motivation Factors (MOT) | 0.066 | 0.118 | 0.849 | ||
| Barrier (BAR) | 0.164 | 0.287 | 0.019 | 0.830 | |
| Intention to Change Health Behaviours (INT) | 0.196 | 0.096 | 0.155 | 0.009 | 0.878 |
The sampling of the data from the family caregivers used the 5,000 bootstrap method and a multicollinearity examination with VIF values. This found that the causal variables do not correlate above the threshold of 3.3 [93]. The results show that the following hypotheses are accepted H1b: Information Factors (INF) have a positive influence on Motivation Factors (MOT) at a significance level of 0.01 (β = 0.257, t=2.707); H3: Motivation Factors (MOT) have a positive influence on Intention to Change Health Behaviours (INT) at a significance level of 0.001 (β = 0.419, t=4.450); and, H4a: Barriers (BAR) have a positive influence on Motivation Factors (MOT) at a significance level of 0.01 (β = 0.253, t=2.792). The results reject Hypotheses H1a, H1c, H2a, H2b and H4b because INF does not have a positive relationship with AWN and INT, AWN does not have a positive relation with MOT and INT and BAR does not have a positive relation with INT. The results are shown in Table 8 and Fig. (3). The results of checking the model fit according to the criteria of Hair Jr and Hult [93], and Henseler and Hubona [95] found that the value of Stone-Geisser Q2 for AWN (Q2=0.024), MOT (Q2=0.121) and INT (Q2=0.162) was relevant and predictive of the model. The value of the standardised root mean square residual (SRMR) was lower than 0.08 (0.076 for our model) and the value of the goodness-of-fit (GoF) was equal to 0.70 which indicates that the model is a good fit [96]. The results are shown in Table 9 and Fig. (4).
The linear relationship between the exogenous and endogenous variables is presented in the form of a measure- ment model and shows the relationship between the variables and the structural model, which describes the causal relation- ship between the variables and also examines the predictive relevance of the models with the Stone-Geisser Q2 values, a standardised root mean square residual (SRMR) and goodness-of-fit (GoF) values. This confirms that the models presented in this study can be applied to the data studied. In addition, in this study, a new relationship is found between Information Factors (INF) and Motivation Factors (MOT) and between Information Factors (INF) and Intention to Change Health Behaviours (INT). The results are shown in Tables 3 to 8.
4. DISCUSSION
This study is the first to predict that the intention to change health behaviour is influenced by social media lifestyle interventions from the perspective of depressed patients and family caregivers by analysing PLS-SEM. The psychosocial factors relate to the intention of the person based on the ICM. The majority of patients were female (77.1%), and Facebook was the most popular social media platform (96.8%) followed by Line (96.2%). The results of the study (shown in Fig. 3) indicate that the views of the depressed patients are mostly consistent with the hypotheses. Only hypothesis H4a does not find a relationship between Barrier and Motivation Factors. This explains that participation in treatment and communication relationships between clinician and patient does not affect the motivation to change health behaviour arising from social media interventions.
The relationship between Information Factors (INF) has a significant positive influence on Awareness Factors (AWN), Motivation Factors (MOT) and Intention to Change Health Behaviours (INT), as shown in Fig. (3) which is in agreement with previous studies. This explains how individuals receive information and advice about health and how it affects their motivation [97] to participate in activities [44]. Additionally, the source of information or a close relationship with experts affects the users' acceptance [68, 69]. When a person is more aware of and is motivated in accessing information about health, it is more beneficial to health [98]. Therefore, information plays an important role in raising awareness and motivation and can also predict the intention to change health behaviour. However, to be clear, elements such as information, factors, messages, channels, and sources of factors, all affect awareness, motivation, and predictions of Intention to Change the Health of patients with major depressive disorders who accept social media interventions.
With regard to the Awareness Factors (AWN) in Fig. (3), there is a significant positive influence on Motivation Factors (MOT) and Intention to change health behaviours (INT). This finding is supported by a previous study that explains that people should be aware that being healthy is an important factor in terms of increasing motivation when it comes to adjusting their health behaviour and that awareness can relate to knowledge and perceptions risk [57]. It shows that awareness of good health and the negative health effects of social media interventions can greatly affect the motivation to change health behaviour and also contribute to the intention to change the health behaviour of depressed patients who accept interventions from social media.
From Fig. (3), it can be seen that Motivation Factors (MOT) have a significant positive influence on Intention to Change Health Behaviours (INT) of depressive patients in accepting intervention from social media.
| Hypotheses | Relationship | Patients (n= 157) | Family Caregivers (n= 110) | Supported | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | p-value | t- value | VIF | β | p-value | t- value | VIF | |||
| H1a | INF -> AWN | 0.224 | 0.004** | 2.899 | 1.000 | 0.222 | 0.051 | 1.956 | 1.000 | Patients |
| H1b | INF -> MOT | 0.178 | 0.020* | 2.318 | 1.053 | 0.257 | 0.006** | 2.707 | 1.105 | Patients, Family Caregivers |
| H1c | INF -> INT | 0.248 | 0.000*** | 3.532 | 1.092 | 0.057 | 0.472 | 0.720 | 1.187 | Patients |
| H2a | AWN -> MOT | 0.333 | 0.000*** | 5.029 | 1.065 | 0.122 | 0.215 | 1.240 | 1.060 | Patients |
| H2b | AWN -> INT | 0.233 | 0.002** | 3.212 | 1.202 | 0.017 | 0.856 | 0.181 | 1.079 | Patients |
| H3 | MOT -> INT | 0.288 | 0.000*** | 3.632 | 1.233 | 0.419 | 0.000*** | 4.450 | 1.248 | Patients, Family Caregivers |
| H4a | BAR -> MOT | 0.107 | 0.224 | 1.216 | 1.012 | 0.253 | 0.004** | 2.792 | 1.071 | Family Caregivers |
| H4b | BAR -> INT | 0.169 | 0.013* | 2.498 | 1.026 | 0.141 | 0.137 | 1.488 | 1.151 | Patients |
According to the results of studies on health behaviours, people who are aware and have healthy attitudes will have an increased level of motivation which plays an important role in the Intention to Change Health Behaviour [13, 79, 99]. On the other hand, if a person lacks motivation to have good health behaviour, it is an important factor when it comes to changing such poor health behaviour habits. The results show that the level of motivation plays an important role in an individual’s intention to change their health behaviour. Therefore, we suggest that the awareness and attitude of patients towards good health should be promoted in order to create incentives for changing their health behaviours. This will lead to the intention to change health behaviours by accepting intervention in living with regard to social media. In addition, when a patient does not participate in treatment and lacks a good relationship with experts, it can affect the treatments given [75] and can hinder the intention to change health behaviours caused by accepting interventions from social media.
Fig. (4) provides the views of the family caregivers and indicates how they play an important role in promoting the patient's well-being [100]. Information Factors (INF) have a significant positive correlation with the statistics for Motivation Factors (MOT) which is consistent with the study by Walthouwer and Oenema [57]. This explains how information and health advice are important for behaviour modification and how obtaining information or advice about the benefits of accepting and interacting with social media tends to motivate patients to have good health behaviour. The more the patients accept to have a better attitude towards health behaviour, the greater the incentive to change the behaviour by accepting social media interventions [61]. Motivation Factors (MOT) have a significant positive relationship with the Intention to Change Health Behaviours (INT) of patients with depression who accept social media interventions.
The main obstacle to motivating people to change health behaviour is when they are not interested in participating in the treatment and lack good relationships with the experts. Therefore, family caregivers can help by encouraging patients to become interested in participating in treatment and act as mediators in communication with experts and patients. On the other hand, the assumptions in H5 are not supported in the study results from the caregiver's perspective, which may be due to the caregiver working with patients who lack awareness of good health [57]. The hypothesis does not relate to the Intention to Change Health behaviour of patients with depression who accept social media intervention.
Finally, the results show that accepting social media interventions has benefits for patients in supporting their participation in treatment by creating guidelines for online self-help in clinical practice [101]. This also benefits the experts in reducing the limitations of face-to-face therapy, such as access to travel information, costs, transportation time, medical supplies and getting access to people in remote areas [40] [41]. It also helps to solve the problems of psychiatrists and psychosocial staff in Thailand [1] and improve the treatment processes. Therefore, if in future there is a lifestyle-based social media intervention programme developed based on this model, it should focus on providing information and advice to patients about the benefits of accepting social media lifestyle interventions. It should raise awareness and promote the results of living a proper lifestyle and use incentives to encourage participants to change their health behaviour through interactions on social media. Increasing the intention to change is important for predicting the changing behaviour of the patient and improving health [8, 45].
5. LIMITATIONS
This study had several limitations. It was based on a sample group from a hospital who were invited to take part and therefore lacked diversity. The demography was also limited to one area. In addition, the depressed patients were not separated into groups of various severity (mild, moderate and severe depression). This could reflect the differences in the patients' responses. Therefore, the results of this study cannot be said to explain the intentions of complicated depressed patients. In addition, there should be a study on the intention to change health behaviours in various forms (sleep, eating or exercise) because the results of this study only explain the overall health behaviour.
Future studies should also include a long-term follow-up of the patients who show an intention to change their health habits. It can show how their plans develop and how their behaviour changes. Moreover, the long-term effects of the risks of using social media by depressed patients both in terms of their privacy and the unreliability of information should be studied [8]. In particular, personal comments on social media are a cause for concern, especially for people with mental health disorders.
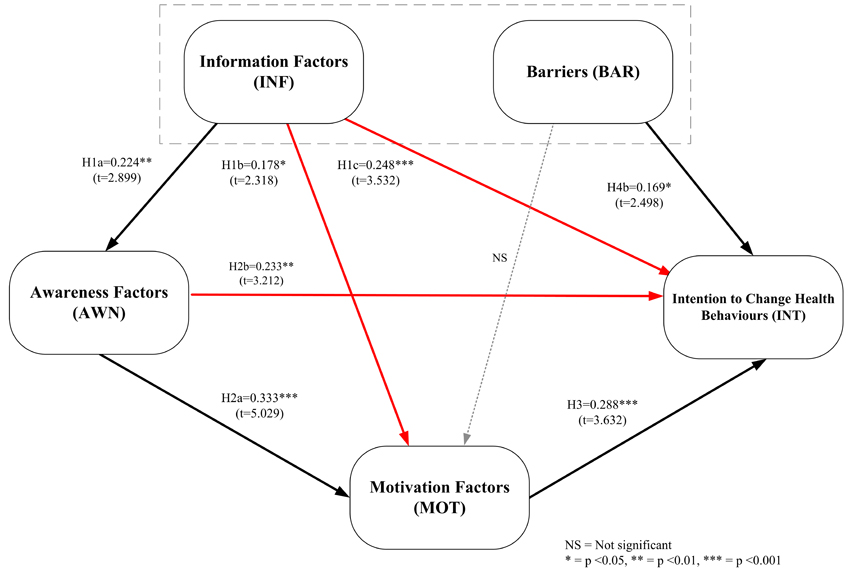 |
Fig. (3). Results of the proposed SMLI model for patients. |
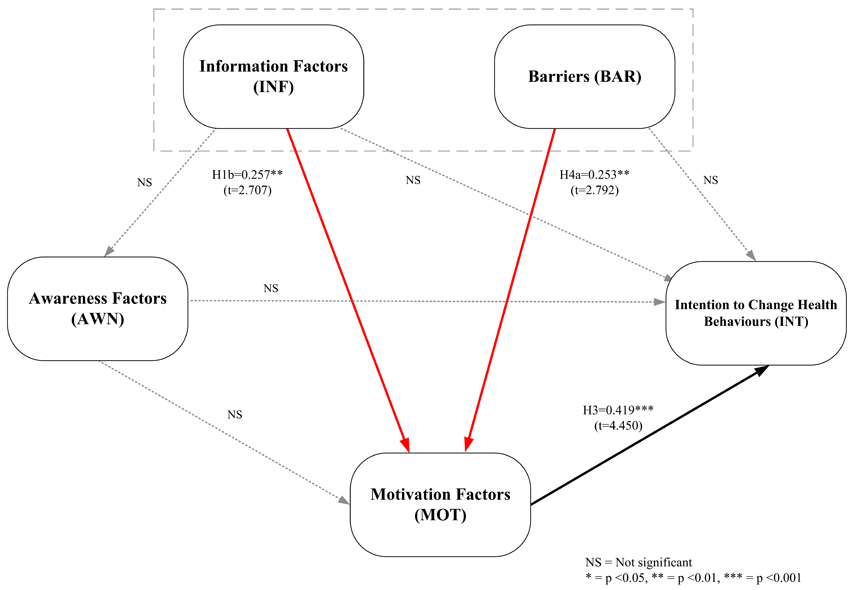 |
Fig. (4). Results of the proposed SMLI model for family caregivers. |
CONCLUSION
The findings from this study show how it is possible to use social media to intervene in lifestyle and create a willingness to change health behaviour from the perspective of depressed patients and family caregivers which covers the psychosocial factors of the I-Change Model. Information and awareness are important factors that increase the patient’s motivation level and can predict that persons intention to change their health behaviours. However, if the patient lacks interest in participating in treatment and does not have a good relationship with a clinician, he/ she tends not to change health behaviours by accepting social media interventions. Therefore, interventions in patients who use social media should focus on providing advice and raising awareness of a proper lifestyle. They can also focus on organizing activities for patients to engage in the long term, as well as encouraging good relationships between experts and patients.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This research was approved by the Centre of Ethical Reinforcement for Human Research, Mahidol University, Thailand (MU-CIRB 2018/058.0503).
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Written consent from all the participants in this study was obtained before publication.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
The study is supported by the Rajamangala University of Technology Rattanakosin for PhD scholarship. (Contract number  001/59)
001/59)
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to thank all the participants in this study; psychiatrist, clinical psychologist and staffs at the hospital; The Centre of Ethical Reinforcement for Human Research, Mahidol University, Thailand.









