All published articles of this journal are available on ScienceDirect.
Training and Evaluation of Community Health Workers (CHWs): Towards Improving Maternal and Newborn Survival in an Urban Setting in KwaZulu-Natal, South Africa
Abstract
Background:
In South Africa, Community Health Workers (CHWs) are a key component of community outreach teams as part of Primary Health Care (PHC) re-engineering. Although the value of CHW programs has been increasingly recognized, published evaluations of CHWs’ training programs are rare. This study documents the training and evaluation of CHWs on maternal and neonatal care towards improved maternal-newborn survival in an impoverished urban setting in KwaZulu-Natal, South Africa.
Methods:
Using a descriptive study design, CHWs were trained to do home visits, assess and support the mother to settle in well at home post-discharge, check on babies’ warmth, cord care, breastfeeding, basic hygiene, size of the baby if underweight and advise on Kangaroo mother care. They were also trained to check if the mothers were given the Road to Health card and to inquire about the immunization and subsequent follow-up visits to the PHC, and encourage mothers to adhere to their follow up dates at PHC clinics. Pre-and post-test scores, shadow visits, and spot checks were used to evaluate their performance.
Results:
Generally, CHWs (n=47) from all three PHC clinics performed well. Overall, the highest post-test score among the PHC CHWs was 72% and the lowest was 50%. On average during shadow visits 67% CHWs were rated as good, 2% were rated as poor, and most CHWs received the highest score at 92% during spot checks.
Conclusion:
CHWs demonstrated social commitment and purpose in the short term observed. The evaluation of the training of CHWs revealed that most demonstrated the necessary skills for referrals to prevent complications, caring for newborns and their mothers at home immediately after discharge from health care centers. CHW upskilling training on maternal-newborn services should be prioritized in the most affected areas.
1. INTRODUCTION
Maternal, neonatal and child (MNC) deaths are a major public health problem in low and middle-income countries (LMIC). In sub-Saharan Africa, the causes of death differ substantially from one country to another [1, 2]. In South Africa, the causes of MNC deaths are multifactorial and health facility oriented problems, such as poor transport facilities; health care provider failed to follow protocol resulting in poor initial assessment and recognition/diagnosis .and delay in referring patients. There are also patient-oriented problems, such as delay in seeking medical help, lack of antenatal care (ANC) visits or infrequent ANC attendance, and lack of adherence to nutrition and immunization programs [3].
These challenges have led the South African government to initiate re-engineering of primary health care (PHC) to make a significant difference to maternal, newborn and child health (MNCH) especially in impoverished communities [4]. Community health workers (CHWs), also known as community caregivers, lay health workers, village health workers or community health promoters are a key component of community outreach teams as part of PHC re-engineering [5]. These cadres of health workers are close to communities, both geographically and socially since they are chosen from within affected communities. They act to strengthen the health system by bridging the gap between health facilities and communities [6, 7].
Elsewhere the use of CHWs has been associated with improved health care access, prenatal care, pregnancy, and birth outcomes as well as reduced health care costs [6-11]. As opposed to the past where CHWs were regarded as unpaid, lightly trained members of the community who focus mainly on health education and provide basic treatments, to date CHWs are increasingly envisioned as a trained and paid corps who give advice and treatments and implement preventive measures [12].
However, their potential is hampered by the lack of integration and conflict with health professionals, insufficient recognition and community support, knowledge retention problems, and inadequate supervision [10]. Furthermore, although the value of CHW programs has been increasingly recognized, published evaluations of CHWs’ training programs are rare. This is in spite of the fact that assessing performance of the community-based health workers has been a major concern for health authorities since Alma Ata [13, 14]. In South Africa, evidence shows that nationally, CHWs have low levels of education [15].
On the basis of the new, expanded and dynamic idea of CHWs as a subsystem within the formal health-care system, CHWs need focused tasks, adequate training, and supervision [6, 11, 12, 16, 17]. With appropriate support and sufficient training, CHWs can potentially play a pivotal role in strengthening health systems since more specifically, they are an important resource for implementing interventions targeting reductions of maternal, newborn and child deaths, by tracking women throughout their pregnancy while simultaneously promoting appropriate maternal and newborn care practices [8, 10, 16]. The aim of this paper is to report on the training and evaluation of CHWs for improving maternal and neonatal health towards improving maternal-newborn survival in an impoverished peri-urban setting in KwaZulu-Natal, South Africa.
2. METHODS
2.1. Study Setting And Design
The population of Umlazi where a study was conducted, live in a peri-urban area composed of approximately a million people. Umlazi is situated south of Durban in the province of KwaZulu-Natal in South Africa. The area is characterized by overcrowding, formal and informal settlements, and a high rate of unemployment. EThekwini district, of which Umlazi is part, has a high antenatal (ANC) HIV prevalence 41.6% [17]. In KwaZulu-Natal neonatal mortality rate is around 23/1000 live births and the infant mortality rate is around 56/1000 live births [18]. There is also a high rate of Tuberculosis infections in adults as well as children due to overcrowding [17]. The area has ten PHC centers of which three are open twenty- four hours each day including weekends, the rest work eight hours daily excluding weekends. There is one regional hospital where all the above-mentioned clinics refer to their complicated patients for further management and care [17].
The study used a descriptive study design using both qualitative and quantitative methods by employing a phenomenological approach for the former and using the latter for the evaluation. We explored the effect of training CHWs to promote birth preparedness and utilization of maternal and newborn health (MNH) services, towards the improved survival of mothers and their newborn. Phenomenological research will not necessarily provide definitive explanations or impact but raises awareness and increases insight about the phenomena by describing learned experiences and the comprehension of the activities or events [18]. The study, in addition, used a quantitative method (pre/post questionnaires) to evaluate the results of the training workshops that were implemented and to evaluate the results of the shadow visits and spot checks undertaken at household level.
2.2. Recruitment And Selection of CHWs
A total of 47 CHWs were recruited from the three purposefully selected PHC centers, Clinic A (n=12), Clinic B (n=25) and Clinic C (n=10). The criteria were to purposefully select PHC centers that have a high workload as this affects the utilization rate and quality of the services. Three of the selected clinics open each day for twenty-four hours. These PHCs have a very high workload with an average catchment population per clinic greater than 60 000 [17].
Selected CHWs were already working as community caregivers in the selected catchment areas. The professional nurses in charge of each clinic allocated the CHWs to the study for training in MNH. They had grade 12 qualifications (a term used to refer to the final year of high school), and were employed by the Department of Health (DOH) and trained as generalist CHWs based on the PHC training package, which identifies twelve roles that are to be performed by the CHWs working in PHC [5].
These include home-based care, counseling, support and stress relief, health promotion and education at a household level, referral to relevant departments, supporting home-based projects, liaison between DOH and the community, mobilization against diseases and poor health through campaigns and word of mouth, etc., directly supervised treatment support i.e., (DOTS for Tuberculosis), screening of health-related clinic cards for compliance or default, assessment of health status for all family members and giving advice, weighing infants and babies and recording this in the child’s ‘Road to Health’ card and providing information and counseling to support the prevention of mother to child transmission (PMTCT) of HIV/AIDS [5].
2.3. Course Structure and Content
The training was done to enable and enhance the necessary skills to support and care for pregnant women and their babies throughout their pregnancy and post-delivery. CHWs were divided into three groups per three sessions over a three-day period. The training focused on equipping CHWs with skills and knowledge to assist pregnant mothers and their babies pre and post-delivery at their homes in the first month of life. The CHWs were trained to conduct home visits during pregnancy and after delivery. The aim of the visits was to promote birth preparedness and utilization of (MNH) services. This included knowledge of newborn danger signs for referrals. The training was also meant to enhance a good working relationship with the Community Advisory Group (CAG) in the area and the Partner Defined Quality (PDQ) structures, which comprise community members and health facility staff.
PDQ is a methodology to improve the quality and access to health services with the involvement of communities in defining, implementing and monitoring the quality improvement process [19]. The model focuses on strengthening the link between the community and primary health care services with the aim to empower all parties. It focuses on:
- Planning, and designing health programmers involving the community
- Exploring process together
- Bridging the gap between the PHC clinic and community to strengthen the continuum of care
- And lastly, working in partnership to sustain the delivery of quality health care
The methods used in the training sessions included lectures, reading, presentation and discussions, demonstrations, and individual and group exercises. This included role-plays where trainees practiced home visits and counseling skills on each other in groups. There were also simulated home visits exploring different scenarios (at both community and household level) that the trainees were likely to encounter.
The training manual was developed based on the UNICEF and WHO training materials [20]. The study investigator with extensive experience in counseling, breastfeeding promotion, PMTC, neonatal and childcare, conducted the training. The pre-test was carried out before the actual training to determine their knowledge of MNH. The training was divided into 26 sessions covering three broad areas (1) home visits (support and care), (2) child feeding practices and (3) postnatal care at a community level (Table 1). In addition, CHWs were also trained on the CAG and PDQ’ roles and their responsibilities and activities in their community. They were also encouraged to attend meetings of the CAG and PDQ structures.
2.4. Evaluation of the Training of CHWs
The training was carried over three days. A pre-test assessment was made and after the training, each CHW took a post-test in order to measure how much CHWs had learned since the beginning of the training. The pre-test and post-test assessments were conducted by the trainer, an experienced midwife specializing in maternal, pediatrics and neonatal care with extensive experience in community engagement, and the results of both tests were shared with individual CHWs. Thirty- six questions were used in the pre- and post-test assessments and each correct answer were given a score of 1, and there was no negative marking. The performance of CHWs was evaluated over a one-month period. The aim was to measure the level of knowledge through the pre-test scores before the training. The post-test scores were used to assess the level of understanding, and assimilation as well as comprehension post-training.
| Sessions | Topics |
|---|---|
|
1 2 3 4 5 6 7 8 9 |
Home visits (support and care) Purpose of the CHW visit Importance of understanding the basics of ANC Recruitment of pregnant women Purpose of CHW visit Interpersonal skills communication Targeting clinic visits for pregnant women Applying counseling to real life Interview guide and process of home visiting Practicing home visits by doing role-plays |
|
10 11 12 13 14 15 16 16 17 18 |
Child feeding practices Counseling to support appropriate and safe baby feeding Breast milk and importance of breastfeeding Helping mother position herself before putting the baby to the breast Attachment of baby to the breast. Expressing breast milk Practicing exclusive breastfeeding Baby feeding for HIV positive women Teaching about safe formula feeding as well as its common difficulties Common baby feeding difficulties Applying counseling skills to different baby feeding methods |
|
19 20 21 22 23 23 24 |
Postnatal care at a community level Understanding of the importance of the continuum of care Introduction to neonatal care (importance of community home-based care for mothers and newborn babies) Care for eyes, umbilical cord and skin Observe for maternal depression Know how to observe for danger signs and refer early to a health facility Understand maintenance of body temperature of small babies (Community kangaroo care) Importance of bonding |
Shadow visits were used to evaluate the performance of CHWs during home visits. The trainer shadowed (accompanied) CHWs during their home visits to see how they do their job in order to and give feedback and guidance after the visit. The quantitative rating of the shadow visits was based on (1) How the CHW introduced the study, (2) body language, (3) listening skills, response to questions, (4) use of simple and clear language, (5) giving relevant study information, (6) making an appointment for the next visit, (7) concluding the visit and saying goodbye. The evaluation included spot checks with pregnant women and new mothers post-training to evaluate their satisfaction with the service provided and the competency of CHWs. The evaluation also included assessing their skills in community mobilization and sensitization, to stimulate demand for MNH services.
The performance of CHWs during shadow visits based on the seven questions was rated from 1 - very poor, 2 - poor, 3 - needs improvement, 4 - good and 5 - excellent. The rating of the spot checks was based on (1) client satisfaction, (2) punctuality of CHWs following appointment, (3) provision of study information and (4) CHWs spending at least 45 minutes with each study participant during the visit. Frequencies (n) and percentages (%) were used to summarize pre and post-test score, shadow visits and spot checks by PHCs catchment areas (clinic A, B, and C).
3. FINDINGS
A total of 80 pregnant women in their 20-40 weeks trimester were recruited to participate in the study. Their ages ranged from 20 to 42 years. The majority were single (96%), and were mostly unemployed (80%) and the rest were in part-time employment.
3.1. Evaluation and Performance of CHWs
3.1.1. Pre And Post Test Scores
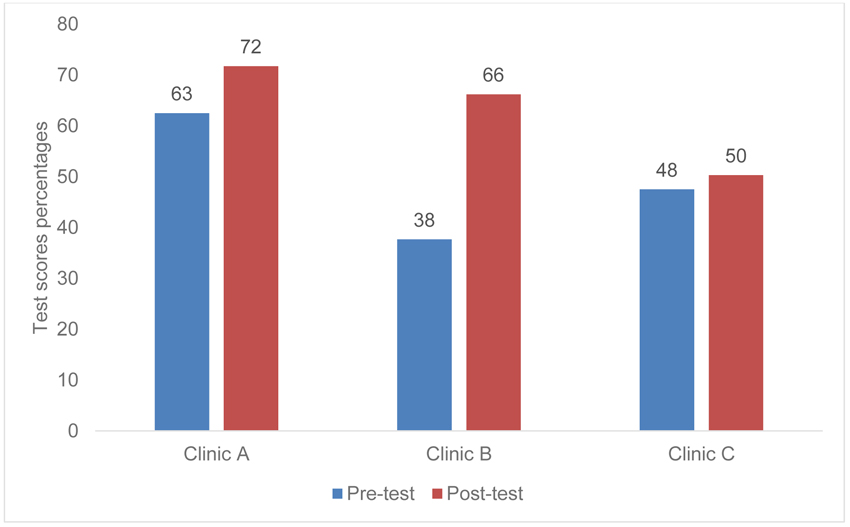
On average CHWs received post-training test scores of 63%. Overall, the highest CHW post training test score was 72% from clinic A and the lowest was 50% from clinic C (Fig. 1). On average CHWs’ knowledge of MNH improved from 63.0% pretraining to 72% post training in Clinic A and from 38% pretraining to 66% post training in clinic B and from 48% pretraining to 50% post training in Clinic C.
3.1.2. Shadow Visits
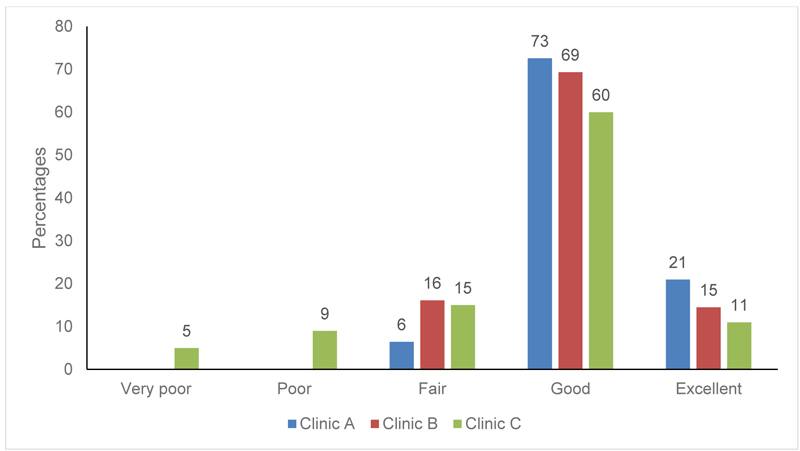
Out of 46 households visited, 7 household had relocated and 39 shadow visits were successfully conducted. On average, 67% CHWs were rated as good, and on this rating, CHWs from Clinic A received 73%, those from Clinic B received 69% and those from Clinic C received 60% (Fig. 2). This meant that CHWs had good communication skills, that is, good use of verbal and non-verbal communication (friendly, responsible and respectful),including active listening.
3.1.3. Spot Checks
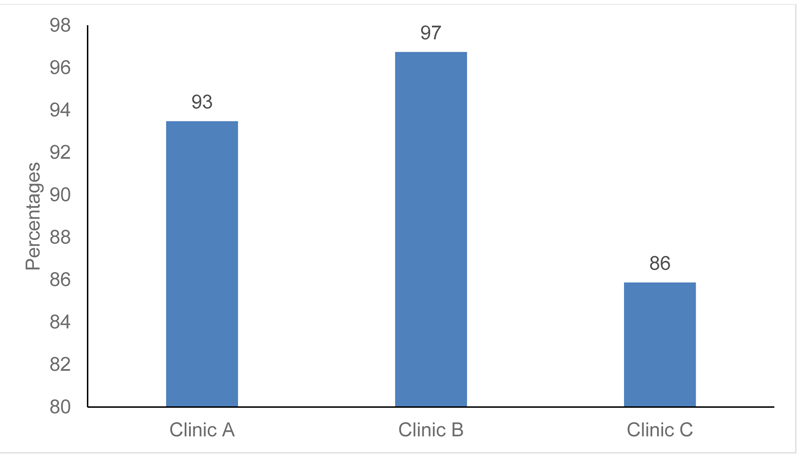
Out of the 39 valid households visited on average, the majority of CHWs received the highest score at 92%. The highest rating was received by CHWs from Clinic B (97%) followed by Clinic A (93%) and Clinic C (86%) (Fig. 3). This suggests that the CHWs had acquired a solid foundation of knowledge and skills for MNC. CHWs in this role are typically used to do referrals, promote breastfeeding and child nutrition, family planning, immunization, and other behaviors linked to mother and child health. Most importantly, these scores indicate that CHWs are trusted by the community-especially the mothers.
3.2. Future Supervision
All participants were given certificates of attendance at the end of the training. Following the completion of the training and one month of observations through shadow visits and spot checks, there was an official hand over to the facility-based trained professional nurses who are in charge of community outreach teams. The trained CHW were part of community outreach teams employed by the DOH and supervised by the professional nurses. Future refresher training was discussed and planned with the professional nurses so that they could feature them in their in-service training plans.
4. DISCUSSION
In recognition of the value of CHWs to the country’s healthcare system, since 2011 the South African government has been gradually integrating CHWs into structured ward-based outreach teams [5]. However, few studies have assessed the effect of training of CHWs. Moreover, training programs vary in their goals, target populations and intended outcomes [7, 8, 16, 17].
This study documents the training and evaluation of CHWs on MNC towards improving maternal-newborn survival in order to inform and guide future training for CHWs on MNH. They were recruited and trained to support and care for pregnant women and their babies before and after birth. A pre- and post-test was administered to evaluate the knowledge and skills that they had gained during the training. Although there was an overall improvement, CHWs from one of the PHCs performed poorly. Consequently, the topics covered in the initial training were revisited at a refresher training just before fieldwork began. Following the training, the observation period of a month was in line with the neonatal period which is the first month of life which is usually a critical time, especially the first twenty-four hours which is often characterized by a high neonatal mortality rate [3, 21]
The observations during the shadow visits and spot checks indicated that the training of CHWs was effective as they successful recruited pregnant women and instituted referrals to avert complications, and followed up newborns and their mothers at home immediately after discharge from health care centers. Basically, they effectively applied the study protocol by doing two ANC visits in each recruited household, followed by a postnatal visit at home within 24-48 hours, followed by visits at 3-4 days, 10-14 days, and the last visit at 3-4 weeks. Babies that were born prematurely were offered two extra visits as they needed more care. In such instances, kangaroo care was discussed during visits and mothers were shown how to keep their babies warm. They also encouraged mothers in their infant feeding choices. However, mixed feeding was discouraged and exclusive breastfeeding encouraged.
These results confirm that CHWs provide a critical link between communities and the health system by bridging the gap between health facilities and the surrounding communities [7, 8, 11, 18]. Evidence shows that CHWs have been instrumental in reducing maternal and neonatal mortality rates through making referrals for emergency obstetric care, and undertaking home visits after the birth, and of their presence at-home births [22-24], They also promote vaccination uptake, breastfeeding and education on infectious disease [25-27].
However, the shadow visits and the spots checks also showed that the performance of CHWs from the selected PHCs varied. Consequently, refresher training was planned to be carried out by their community outreach supervisors. It was also agreed that refresher training would be informed by emerging issues and the need for improvements. The maternal and neonatal component that was the focus of this study was additional to a number of areas in which CHWs were trained. It has been shown that while the standardized training of CHWs as generalist health workers is ideal, program-specific training is much more effective as it ensures that core knowledge and skills are effectively relayed [7, 8, 11].
5. LIMITATIONS
Some participants had relocated which made it impossible to locate them. The relatively short study period (one month) limited the follow up with the mothers. In addition, the study had no control arm, and evaluated the training outcomes through pre- and post-tests, shadow visits during home visits and spot checks with pregnant women. Therefore, improvement in maternal and newborn survival could not be measured. Furthermore, the small sample size weakens the power of statistical significance. Generalisability was not possible given the relatively small study sample and catchment area. Nevertheless, this study provides valuable insights into the implementation of the CHW strategy focusing on the utilization of MNH services, and adds to the general body of knowledge on the training of CHWs towards improved MNH.
CONCLUSION
CHWs demonstrated social commitment and purpose in the short term observed. CHWs demonstrated that they had acquired competencies on how to conduct visits during pregnancy and after delivery to care for the mothers and their babies including the knowledge of newborn danger signs for referrals. During shadow visits and spot checks, CHWs also demonstrated their skills on community mobilization and sensitization to stimulate demand for MNH services. This work demonstrated that one way of improving the health of newborn babies and their mothers is by utilizing CHW’s from their own community with relevant training for supporting pregnant women, mothers, and their newborns. Consequently, the study recommends that the CHW upskilling training on maternal-newborn services should reach more impoverished communities to fill in the gaps between communities and health facilities especially where there is a shortage of midwives or obstetricians.
LIST OF ABBREVIATIONS
| ANC | = Antenatal care |
| ART | = Antiretroviral therapy |
| BREC | = Biomedical Research Ethics Committee |
| CAG | = Community Advisory Group |
| CHW | = Community Health Workers |
| DOH | = Department of Health |
| DOT | = Directly Observed Therapy |
| HIV | = Human Immunodeficiency Virus |
| LMIC | = Low and Middle Income Countries |
| MNC | = Maternal Neonatal Care |
| MNCH | = Maternal Neonatal Child Health |
| NDOH | = National Department of Health |
| PDQ | = Partnership Defined Quality |
| PHC | = Primary Health Care |
| WHO | = World Health Organization |
| UNICEF | = United Nations International Children’s Emergency Fund. |
AUTHORS’ CONTRIBUTIONS
TN conceptualised, conducted training and evaluation of CHWs has and drafted the manuscript. MT and MM supervised the study and made significant intellectual input. All authors reviewed and approved the final draft.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This work was approved by the Biomedical Research Ethics Committee (BREC) of the Discipline of Public Health, School of Nursing and Public Health Medicine, University of KwaZulu-Natal (BREC REF NO: BF081/17).
HUMAN AND ANIMAL RIGHTS
No humans/ animals were used for the studies that are basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article belongs to the University of KwaZulu-Natal and are currently being use for the PhD of the lead author. This data will be shared on request from the lead author upon completion of her PhD.
FUNDING
The work was funded by the College of Health Sciences (CHS) scholarship at the University of KwaZulu-Natal.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGMENTS
We would like to thank all the CHW’s for their participation in the training. Thank EThekwini district manager and PHC managers for providing training venues. The project would not have been possible and successful without the participation of mothers and their babies.


