All published articles of this journal are available on ScienceDirect.
Obstetrics Outcome after a Nutritional Health Education Program for Pregnant Females at Zagazig University Hospitals; An Interventional Study
Abstract
Background:
Nutrition during pregnancy is an important element for the pregnant women and their developing fetus, they must take enough calories and nutrients to provide the essential requirements for both themselves and their fetus and to prevent complications of abnormal weight gain in pregnancy.
Objectives:
To determine the effect of the nutritional health education program on changing knowledge, attitude, and practice towards a healthy lifestyle during pregnancy, obtaining optimal weight gain and consequently its effect on maternal and fetal outcomes.
Subjects and Methods:
An interventional study (pre-post test), in Zagazig university antenatal care outpatient clinic was conducted.
Subjects' Criteria:
135 pregnant females in the first trimester aged 18-35 years who did not have any chronic medical disorder with Body Mass Index between 18.5 and 24.9 kg/m2 were enrolled.
Methods:
Data collection was done using a semi-structured questionnaire about females’ socio-demographic characteristics, obstetric, family and clinical history. Health education sessions were applied to the pregnant females and their knowledge, attitude, and practice about healthy nutrition were assessed before and after the intervention. Ultrasound was performed, maternal and fetal outcomes were detected.
Results:
This study was conducted on 135 pregnant females from whom 9 cases had excluded at the time of delivery due to the detection of ultrasound abnormalities and 16 women were dropped out during the follow-up period. After the nutritional education program, the proportions of adequate knowledge, attitude, and practice were increased from (28.2% to 77.3%), (8.2% to 75.5%) and (32.7% to 77.3%) respectively (p-value <0.001). There was a statistically significant higher cesarean section, Intra and post-partum complications (85.7%vs 42.9%p<0.001), (71.4% vs17.2% p<0.001) and (25.7%vs7.1% p=0.008) [Odds (95% C.I); 8 (6.7-11.3), 12.1(11.7-13.9) and 4.5(1.2-8.7)], higher neonatal weight and neonatal blood glucose (p<0.001& 0.009) in over-weight versus optimal weight gain groups respectively.
Conclusion:
The intervention was effective in increasing pregnant females’ knowledge, attitude, and practice towards healthy nutrition during pregnancy, obtaining optimal weight gain and improving maternal and fetal outcomes.
1. INTRODUCTION
Nutrition in pregnancy has a good influence on subsequent maternal and offspring health, low intake increase the risk of preterm delivery and low birth weight [1] while the excess intake is associated with having larger babies and postpartum weight retention [2]. Moreover, adequate nutrition during pregnancy is important for the development of the placenta, for a healthy delivery and future lactation [3]. The recommended weight gain for obese women during pregnancy is up to 6.8 kilograms; for the overweight women, the gain would be from 6.8 to 11.2 kgs, and for the normal-weight women, between 11.2 to 15.9 kgs [3]. Maternal obesity during pregnancy is a widespread problem which is related to several comorbidities for both mother and child [4]. Excessive Gestational Weight Gain (GWG) increases maternal risks for preeclampsia, gestational diabetes, Caesarean section and weight retention post-partum with associated long-term health consequences [1] and also, fourfold increased risk of large-For-Gestational-Age (LGA) infants [2]. Although the nutritional health education intervention plays a significant role in improving maternal and fetal outcomes through improving knowledge, attitude and practice, little reports on these issues were available before. So the objectives of this study were to improve maternal and neonatal outcomes through raising knowledge, attitude, and practice of pregnant females towards a healthy lifestyle and obtaining optimal weight gain using nutritional health education programs.
2. MATERIALS AND METHODS
2.1. Study Design and Settings
An interventional study (pre-posttest) was conducted in the Antenatal Care Clinic of Obstetrics and Gynecology Department at Zagazig University Hospitals in the period from May 2017 to June 2019.
2.2. Target Group
Pregnant females in the first trimester had visited the Antenatal Care Clinic at Zagazig University Hospitals, aged 18-35 years, nonsmokers, primigravida, take no medication and did not have any chronic medical disorder with Body Mass Index (BMI) between 18.5 and 24.9 kg/m2 were enrolled in this study.
2.3. Sample Size
Was calculated through the Open-EPI (version 3.01), according to the following data: Assuming that the knowledge of pregnant females about healthy nutrition during pregnancy was changed from 9% before intervention to 31% after intervention, the power of precision was 80%, and the confidence interval was 95%, and the sample size was 112 pregnant women. Twenty percent (23 women) were added to overcome the drop-out rate so the total number was 135 pregnant females.
2.4. Sample Technique
A systematic random selection of the sample population from all pregnant women was carried out. The total number of registered women was 570 and we needed a sample size of 135 so we took every 4th women (K-interval) beginning by the 5th one who was chosen by lottery. Nearly sample collection had persisted for seven months.
2.5. Data Collection
All study participants had an individual face-to-face interview and filled the questionnaires to collect socio-demographic data about their age, level of education, income, residence, sources of health information and service delivery [5]. Their family history of obesity and clinical data were detected. We compared women's knowledge, attitude and practice about healthy food, supplements, iron, calcium, effect of anemia and obesity on pregnancy before and after the intervention by the (pre) and the (posttest), also we measured the difference in body weight, fasting blood glucose, blood pressure, and urine analysis.
After the intervention, Ultrasonography was done at the time of birth to detect any unexpected indications for cesarean section. Mode of delivery and intra-partum complications (prolonged, obstructed and precipitate labor, shoulder dystocia, labor and anesthetic complications) were assessed, Neonatal weight and blood glucose at birth were measured and the follow up period persisted 24 hours postpartum to detect any atonic complications in the form of postpartum hemorrhage and traumatic complications in the form of traumatic injury to the genital tract.
2.6. Fieldwork
2.6.1. During the First Session
The nutritional education session was done for each woman individually by health education message using posters and booklets in a face to face interview for 20 minutes and covered;
- 1- Knowledge about healthy foods, the importance of calcium and iron intake, the importance of folic acid and supplementation intake, the foods that decrease absorption of iron, the causes of anemia during pregnancy, also knowledge about ideal gestational weight gain and consequences of abnormal weight gain was illustrated.
- 2- Attitude and practice: A positive attitude about the importance of getting enough calcium, iron, folic acid, and supplementation during pregnancy was supported.
- 3- Definition of obesity in pregnancy, its risk factors (modifiable and non-modifiable) and complications.
2.6.2. Follow up Monthly Visits Along the Pregnancy Period
Were done as one session per month at the antenatal care unit by the researcher and ranged in time from 15 to 20 minutes for each, the females were taught about the healthy balanced diet, habits and follow up of their weight gain was done. Weekly contact through mobile devices and Facebook page was done to ensure adherence to the healthy lifestyle and facilitate communication.
2.6.3. Activities During the Last Visit Before Delivery
- 1- Ultrasound was done to assess the fetal conditions and to exclude any indication of cesarean section (mal-presentation and fetal abnormalities).
- 2- Maternal body weight, blood pressure, fasting blood glucose, urine analysis, convulsion and deciding mode of delivery were determined.
2.6.4. The Pregnant Women Were Followed Until 24 Hours After Delivery
To detect any intra or post-partum complications (atonic complications in the form of postpartum hemorrhage and traumatic complications in the form of traumatic injury to the genital tract), detect neonatal weight and blood glucose.
2.7. Data Management
The collected data were entered, checked and statistically analyzed using the SPSS program (Statistical Package for Social Science) version 23.0 (SPSS Inc., Chicago, IL, USA). For the statistical calculations, data coding was done, and qualitative data were represented as frequencies and percentages. Chi-square test (χ2), Fischer exact test and McNemar test were carried out for testing the association between the qualitative data. Quantitative data were presented as mean, SD and median. Continuous variables were checked for normality by using Shapiro-Wilk test (sig) and Q-Q plot and compared using the independent t-test, paired t-test and Wilcoxon signed-rank test. Binary regression analysis was conducted to identify the predictors of maternal outcomes. The test results were considered significant when p-value ≤ 0.05.
2.7.1. Scoring of Socio-Economic Status
- The socio-economic level was classified into low, moderate and high levels depending on the calculated score (39).
- · A score of less than 50% was considered (low) ≤ 19.5
- · A score from 50% to less than 75% was considered (moderate) = 19.6 - 29.25
- · A score equal to 75% or more (high) was considered ≥ 29.25
- . This is an updated scale delivered from El-Gilany et al. for assessing the Egyptian socioeconomic status [5].
2.7.2. Scoring of Knowledge, Attitude, and Practice
The total knowledge score about healthy food types, the importance of calcium and vitamin D, iron, folic acid, and supplementation intake were 23,18, 21,16 and18 respectively. The scores of knowledge about anemia and weight gain in pregnancy were 34 and16. So the total score of all items of knowledge about healthy nutrition during pregnancy was 146, total attitude, and practice scores towards the importance of healthy foods and habits were 12 and 8.
2.7.3. Adequacy Levels of Knowledge, Attitude, and Practice
The cutoff point was (70%) [6], whereas score ˃ 70% was considered as adequate, while ≤ 70% was considered as inadequate knowledge, attitude and practice levels.
2.7.4. Weight Gain Classification
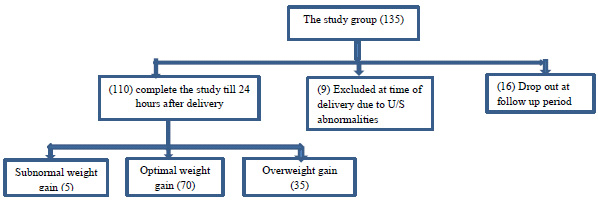
According to the Institute of Medicine [(IOM), 2009] [7], the pre-pregnancy normal-weight women with BMI from (18.5 to 24.9) were classified according to their gestational weight gain at the end of pregnancy as follow; (subnormal weight gain) for women with gestational weight gain <11.2 kg, (optimal weight gain) for women with gestational weight gain from 11.2 to 15.9 kg and (overweight gain) for women with increased gestational weight gain >15.9 kg. (Fig. 1)
3. RESULTS
3.1. Socio-Demographic Characteristics of the Studied Group
The age of the studied group was 27.1±4.4 (ranged from 20-37 years old), about half of them (48.2%) were of low social class, and 40.9% had a positive family history of obesity (mainly first degree relatives). After the intervention, about sixty percent of the study group (63.6%) had optimal weight, and 31.8% had overweight, while only 4.5% had subnormal weight gain (Table 1).
3.2. Knowledge, Attitude and Practice Improvement After the Nutritional Health Education Program
There was a statistically significant improvement in total knowledge, attitude, and practice scores of pregnant females about healthy lifestyle during pregnancy from {median (interquartile range), (53(33-125), 3(0.0-11) & 4(2-7)} before the health education sessions to 127(44-146), 11(1-12) & 6(3-8) respectively after the intervention. With statistically significant higher adequacy levels of knowledge, attitude, and practice after than before the intervention (77.3%, 75.5% and 77.3%), (28.2%, 8.2% and 32.7%) respectively (p-value <0.001) (Table 2).
| Variables | The Studied Group(110) | |
|---|---|---|
|
Age (years): mean ± SD (Range) median |
27.1±4.4 (20-37) 26 |
|
| Variables | NO(110) | % |
|
1- Education of the females Illiterate Read and write Primary Preparatory\secondary High |
12 16 8 50 24 |
10.9 14.5 7.3 45.5 21.8 |
|
2-Occupation of the females Working Housewife |
34 76 |
30.9 69.1 |
|
3- Residence Rural Urban |
78 32 |
70.9 29.1 |
|
4- Income Not enough Enough Enough and more |
56 54 0.0 |
50.9 49.1 0.00 |
|
5- Social class Low Moderate High |
53 45 12 |
48.2 40.9 10.9 |
|
6- Family history of obesity No First degree relatives Second degree relatives |
65 32 13 |
59.1 29.1 11.8 |
|
7- Weight gain after the intervention Subnormal weight gain Optimal weight gain Overweight gain |
5 70 35 |
4.5 63.6 31.8 |
| Variables | Pre intervention | Post intervention | p-value |
|---|---|---|---|
|
-Total Knowledge score Median (interquartile range), |
53 (33-125) |
127 (44-146) |
0.001**^ |
|
-Total attitude score Median (interquartile range), |
3 (0.0-11) |
11 (1-12) |
0.001**^ |
|
-Total practice score Median (interquartile range), |
4 (2-7) |
6 (3-8) |
<0.001**^ |
|
Total Knowledge adequacy NO (%) |
31 (28.2) | 85 (77.3) | <0.001**^^ |
| Total adequacy of positive attitude NO (%) | 9 (8.2) | 83 (75.5) | <0.001**^^ |
| Total practice and healthy habits well done NO (%) | 36 (32.7) | 85 (77.3) | <0.001**^^ |
3.3. Characteristics of the Subnormal Weight Gain Group
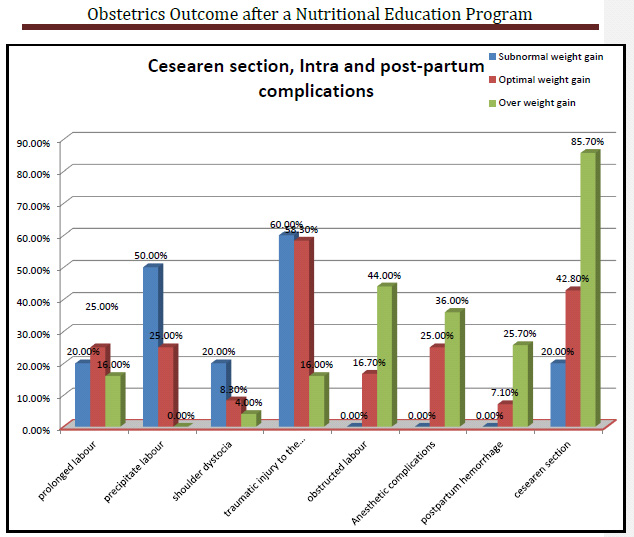
Concerning the five subnormal weight gain females, weight gain was 9±1.6 ranging from 7-11kg, the adequate levels of knowledge, positive attitude, and healthy practice were 60.0%, 20.0% and 0.00% respectively. All of them (100.0%) had normal fasting blood glucose and blood pressure levels and no one (0.0%) had neither convulsion nor proteinuria. Twenty percent of them had cesarean sections and the majority of them (80.0%) had intrapartum complications mainly traumatic injury to the genital tract (60.0%) followed by precipitate labor (50.0%) then prolonged labor and shoulder dystocia (20.0%) with no postpartum complications among them (Fig. 2).
3.4. Binary Logistic Regression for Prediction the Role of Knowledge, Attitude and Practice Improvement on Gestational Weight Gain
For detection of the effective change in knowledge, attitude, and practice as explanatory (independent) factors for the gestational weight gain as a dependent factor in the studied group, Binary logistic regression proved that practice followed by attitude then knowledge were highly statistically significant explanatory variables for optimal gestational weight gain after the intervention [Odds (95% C.I); 9.1 (8.5-10.2), 6.7(2.8-9.3) and 4.5(2.7-8.6)] respectively (P-value <0.001) (Table 3).
3.5. Maternal and Neonatal Outcomes After the Intervention
Concerning maternal outcome, there was a statistically significant lower maternal weight gain, BMI, fasting blood glucose, and presence of proteinuria in optimal than over-weight gain group (14.3±0.9 vs 21.3±2.8), (23.1±2.3 vs 27.1±1.4), (1.4% vs 14.3%) and (0.00% vs 5.7%) with (P-value < 0.001, 0.001, 0.007 and 0.04) respectively. But regarding blood pressure and convulsions, there was no statistically significant difference between both groups (p-value 0.07 and 0.15) respectively (Table 4)
| Variable | Regression coefficient | S.E^ | Wald test | p-value | Odds (C.I 95%)^^ |
|---|---|---|---|---|---|
| Knowledge | 2.2 | 0.65 | 11.5 | 0.001** | 4.5(2.7-8.6) |
| Attitude | 0.05 | 0.01 | 14.6 | <0.001** | 6.7(2.8-9.3) |
| Practice | 2.3 | 0.6 | 15.2 | <0.001** | 9.1(8.5-10.2) |
| Items | Optimal weight gain (N=70) |
Over weight gain (N=35) |
p-value^ | |
|---|---|---|---|---|
|
Weight gain (kg) mean ± SD (Range) |
14.3±0.9 (11.5-15.6) |
21.3±2.8 (16.7-25) |
0.001** | |
|
-BMI (kg/m2) mean ± SD (Range) |
22.3±0.3 (18.8-24.9) |
27.1±1.2 (25-29.8) |
<0.0001** | |
|
-Neonatal weight (grams) mean ± SD (Range) |
3611±400 (2150-4050) |
4102±501 (2200-4950) |
<0.0001** | |
|
-The Neonatal blood glucose level at birth mean ± SD (Range) |
121±7 (110-130) |
128±13 (105-140) |
0.009* | |
|
-Fasting blood glucose (mg/dl) Normal Abnormal |
NO (%) | NO (%) | p-value^^ | OR (C.I 95% |
| 69 (98.6) 1 (1.4) |
30 (85.7) 5 (14.3) |
0.007* | 11.5 (8.3-14.2) |
|
|
-Blood pressure Normal Abnormal |
69 (98.6) 1 (1.4) |
32 (91.4) 3 (8.6) |
0.07 | 1.4 (0.6-1.9) |
|
-Convulsions Absent Present |
70 (100.0) 0.0(0.00) |
34 (97.1) 1(2.9) |
0.15 | NA |
|
- Proteinuria Absent Present |
70 (100.0) 0.0 (0.00) |
33 (94.3) 2 (5.7) |
0.04* | NA |
In regard to neonatal outcome, there was a statistically significant increased neonatal birth weight and blood glucose level at birth (4102±501 vs 3611±400) gm. and (128±13 vs 121±7) (p-value <0.001 and 0.009) respectively in an over-weight gain group than optimal weight gain in (Table 3).
Cesarean section, intra-partum complications and post-partum hemorrhage were statistically significantly higher in over-weight gain group than optimal weight gain one (85.7% VS 42.9%), (71.4% VS 17.2%), and (25.7% VS 7.1%) [Odds (95% C.I); 8 (6.7-11.3), 12.1(11.7-13.9) and 4.5(1.2-8.7)] (P-value <0.001, <0.001 and 0.008) respectively (Fig. 2).
4. DISCUSSION
Nutritional counseling is a cornerstone of the prenatal care for all women during pregnancy as a woman’s nutritional status not only influences her health, but also pregnancy outcomes and the health of her neonate [8].
Abnormal GWG, whether excessive or inadequate, is associated with a series of maternal and neonatal complications, and even life-threatening diseases [9]. Excessive GWG is associated with maternal postpartum weight retention, obesity, abnormalities in maternal prenatal blood glucose level, hypertension during pregnancy, cardio-metabolic problems. While regarding neonates, it causes macrosomia and later childhood obesity [10]. While poor maternal weight gain during pregnancy is associated with SGA infants if mothers does not gain more than 20 pounds, miscarriage, preterm births, LBW infants and gastroschisis [11].
This study included 135 pregnant women in the 1st trimester of pregnancy attending the antenatal care clinic at Zagazig University Hospitals. We measured their body weights, FBG, blood pressure, and urine analysis. Nutritional education was applied and the pregnant females were followed up till 24 hours after delivery. At the time of delivery, all women had Ultrasonography to exclude any fetal abnormalities (mal-presentation was detected in 5 cases, three women had macrocosmic infants, and one woman had cephalo-pelvic disproportion, and so these nine women were excluded from the final statistical analysis).
The present study showed statistically significant improvement in total knowledge score of pregnant women about their healthy nutrition during pregnancy, this attributed to the health education intervention, and this finding was inconsistent with Girard & Olude [12] who conducted meta-analyses for the effect of NEC on maternal, neonatal and infant health outcomes including gestational weight gain, maternal anemia, birth-weight, and preterm delivery and they reported that nutritional education resulted in an improvement of the nutritional knowledge, also similar results by Fallah et al. [6], who found significant increase in the awareness level of pregnant women about healthy nutrition from 3% before the intervention to 31% after the nutritional education intervention (P < 0.001). However, the current results were in contrast with some Turkian studies which found that NE did not provide women with adequate knowledge about nutrition during the pregnancy [13]. This contrast between the current study and the studies which did not have effect might be due to the fact that more positive outcomes could be gained if the nutritional education was given by a dietitian (nutritional health care practitioner), not by midwives, this justification was supported by studies carried out in USA which stated that as a result of the nutritional education provided by a dietitian, unhealthy food consumption was decreased, and healthy food consumption were increased during the pregnancy period [14].
Regarding the attitude and practice of pregnant women towards healthy nutrition during pregnancy, the current study demonstrated a statistically significant improvement. This finding was in concomitant with Aşcı and Rathfisch [15], who found that the lifestyle interventions had a significant effect on improving the pregnant females' attitude in the form of increased calcium, magnesium, iron, zinc, and vegetable intake. Also, the NE programs conducted by Dunneram and Jeewon [16] had been effective in positive behavior modification measured in terms of eating patterns and health quality. The pregnancy-specific healthy dietary practice of the pregnant women increased from 46.8% to 83.7% after the nutritional education sessions applied by Zelalem et al. [14].
Regarding the increased adequacy levels of knowledge, attitude and practice, the significant improvement in this study coincide with Zelalem et al. [14], where the proportion of pregnant women with proper knowledge, attitude and practice towards nutrition during pregnancy increased from 53.9 to 97% and another study revealed that the percent of the pregnant women who had correct information after the intervention was 78.6% [17].
After the intervention, about sixty percent of the studied group (63.6%) had an optimal weight gain, (31.8%) had over-weight gain, while only 4.5% had subnormal weight gain. This good outcome regarding gestational weight gain was statistically significantly explained by the improvement in practice, attitude, and knowledge respectively supported by Walker et al. [18], who found that the traditional face to face delivery of weight management interventions during pregnancy succeeded in obtaining optimal weight gain.
Considering weight gain and maternal complications, the present study was in agreement with Fallah et al. [6], which concluded that 41%, 28%, 26%, and 5% were normal, overweight, obese and underweight respectively depending on BMI. Only 1% had abnormal blood pressure, diabetes and nephropathy, also, the present study coincided with Whitaker et al. [19], whose study concluded that 79% of the pregnant women were within the normal range, 9% below and 11% above.
The statistically significant decrease in C.S, intra and post-partum complications, the decreased neonatal birth weight and blood glucose level among the optimal weight gain group in this study were similar to the results of Stang and Huffman [20] who concluded that lifestyle interventions which modify gestational weight gain might reduce the risk of poor pregnancy outcomes such as gestational diabetes, gestational hypertension, large for gestational age, and macrosomia, as well as lower the risk of significant postpartum retention. Consistently, Denison et al. [21], noted that obese pregnant women were at increased risk of complications, such as shoulder dystocia (OR 2.9, 95% CI 1.4–5.8), gestational diabetes, pre-eclampsia, Venous Thromboembolism (VTE), prolonged labor, and anesthetic complications. Also, Fukami et al. [22], reported that the risk factors for postpartum hemorrhage were fetal macrosomia (over 4000 g), pregnancy-induced hypertension, severe vaginal or perineal lacerations and all these factors can be caused if the maternal gestational weight gain was over 15 kg. Such high weight gain significantly increased the incidence of PPH compared with women showing less than 10 Kg weight gain during pregnancy. Finally, Butwick et al. [23], found an increased risk of postpartum hemorrhage which was atonic as a result of less postoperative movement and more congested vessels among over-weight gain pregnant women.
CONCLUSION
The nutritional education program was effective in increasing the pregnant females’ knowledge, attitude, habits, and practice towards healthy nutrition during pregnancy, obtaining optimal weight gain and improving maternal and fetal outcomes.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The official permission was taken from Zagazig University, Faculty of Medicine, obstetrics and gynecology department. Institutional Review Board (IRB) of the Faculty of Medicine, Zagazig University, Egypt, approved the study protocol (No. 3168).
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
The title and objectives of this study were explained to the participants to ensure their cooperation and informed consent was obtained.
AVAILABILITY OF DATA AND MATERIALS
Data is available from the corresponding author on request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to thank all the staff members of the Community Medicine Department, Obstetrics and Gynecology Department and Pediatric Medicine Department who helped us complete this work. Also, the authors are very grateful to all included women for their valuable contribution to this work.


