All published articles of this journal are available on ScienceDirect.
Neuromuscular Functional Assessment in Low Back Pain by Surface Electromyography (SEMG)
Abstract
Background:
Low back pain is a major occupational health issue and a leading cause of disability globally. Significant differences in Surface Electromyography (SEMG) have been reported between persons with Low Back Pain (LBP) and normal, healthy controls. Many studies reveal that when the trunk is in full flexion there is an electrical silence in back muscles referred to as “flexion-relaxation phenomenon.” It is often absent in individuals reporting LBP and particularly chronic LBP. There are several SEMG measures that describe this phenomenon.
Objective:
To evaluate muscle activity in acute and chronic LBP and the usefulness of quick and reliable procedures to demonstrate abnormal electromyographic activity of the spine erector muscles.
Methods:
We evaluated 40 subjects aged 25-65 years. For each participant, a clinical history regarding the presence of chronic or acute LBP was collected. Each subject was evaluated with SEMG measures of spine erector muscles during standing and prone position (for acute LBP), and flex-extension movement (for chronic LBP subjects). Superficial potential was recorded and compared between groups.
Results:
In all three procedures, differences were identified in the surface electromyographic activity between the healthy controls and the one affected by LBP.
Conclusion:
The study of normal and pathologic electromyographic patterns could be a valid means to support in an objective way the presence/absence of acute and chronic LBP.
1. INTRODUCTION
Low Back Pain (LBP) is a major public health issue and a leading cause of disability in the Western world [1]. The costs related to this disease are comparable to those related to chronic illness such as diabetes and cardiovascular disease [2-4]. Costs related to loss of productivity and home care are estimated to be eight times higher than the direct costs for diagnosis and treatment [5, 6]. Although the diagnosis of LBP is mainly clinical, several instrumental procedures have also been applied in order to reach an objective classification of the pathology in relation to the costs that a diagnosis of LBP entails. Surface Electromyography (SEMG) is a method of detecting myoelectric signals from superficial muscle, carried out by means of the electromyograph, an electromedical instrument, that has evolved in recent years thanks to many clinical applications in the rehabilitative medical field [7].
In scientific literature, the relationship between the pre-sence of LBP and SEMG outcomes is well established [7, 8]. Studies show that in patients with local acute pain there is increased electromyographic activity, specifically of para-vertebral muscles [9, 10]. Similarly, SEMG is useful in detecting a reduction of neuromuscular endurance and expression of increased fatigue in chronic LBP [11]. One of the most studied methods for the evaluation of LBP through SEMG is the analysis of the modification of the flexion-relaxation pattern [7, 12-16]. On these premises, surface electromyography has been recently proposed as a possible objective method for biomechanical risk assessment in industrial activities [17], such as the biomechanical overload of the upper limb, the hand and the carpal tunnel [18-20]. Indeed, SEMG might be a complementary investigation to clinical-anamnestic evaluation in the field of occupational medicine.
The electromyographic survey might allow evaluating, in a non-invasive, gesture-specific and inexpensive way, functional neuromuscular problems characterized by high level of motor and postural engagement that can typically be difficult to evaluate for occupational physician especially regarding the consequences on the ability to work [21]. Despite these potential applications, protocols for the identification and classification of the various dysfunctions of the paravertebral muscles identified by means of this technique are still lacking. Similarly, the potential for the use of this diagnostic method in the field of occupational medicine is poorly defined especially in subjects affected by LBP.
The aim of our study is to evaluate the procedures for detecting the surface electromyographic activity of the lumbar paravertebral muscles in order to compare electromyographical pattern in subjects aged 18-65 years with acute or chronic LBP.
2. MATERIALS AND METHODS
For this study, the PC based NeuroTrac MyoPlus4 SEMG dual channel portable device Verity Medical Ltd was used.
A calibration system was provided by the supplier. Real-time sEMG data are processed and displayed in software. Data are then converted into force data using individual calibration curves.
We enrolled 40 symptomatic subjects (age range 25-65 years), 20 affected by acute LBP, 8 female and 12 male (mean age 44.80 ± 10.04) and 20 affected by chronic LBP, 9 female and 11 male (mean age 53.35 ± 8.65), and 20 healthy controls (age range 18-65) 10 female and 10 male (mean age 50.35 ± 10.75). Body Mass Index (BMI) was between 19 and 25. For the purpose of this study, acute LBP was defined as acute when starting within the previous 4 weeks from the examination, and chronic when starting before.
We excluded from the study subjects in a poor general health state (due to the presumed loss of muscle tone), patients affected by neuromuscular diseases, scoliosis, and subjects who had been using muscle relaxant drugs that could interfere with electromyographic recording activity.
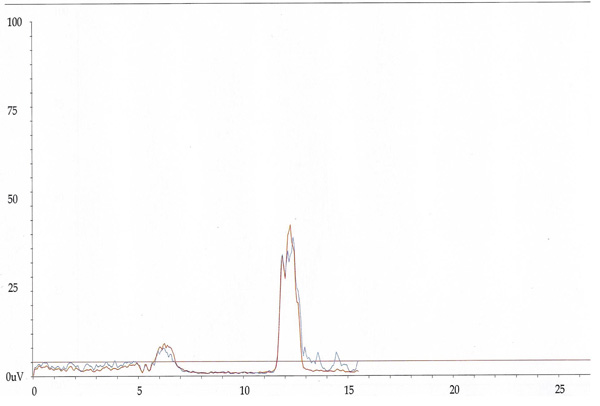
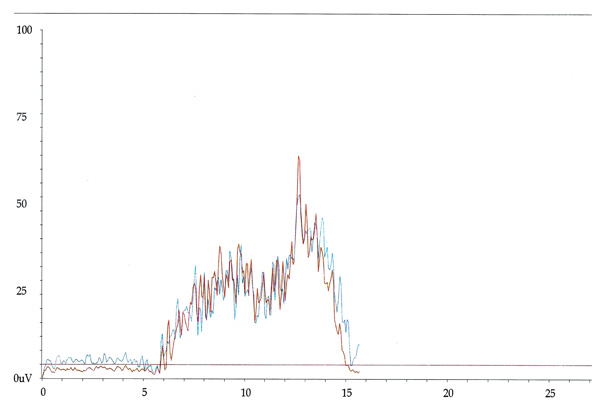
We used a within-subject repeated measures design in symptomatic and healthy subjects. We didn’t perform a comparison between chronic and acute LBP subjects because this is out of the scopes of our work.For each subject, after the correct localization of the lumbar paravertebral muscles (at L3- L4 transverse processes) and after accurate local skin cleansing, the appropriate electrodes were placed bilaterally at a distance of 4 cm from the spine [22]. Patients with acute LBP were evaluated in Prone Position (PP) for 30 seconds and in Standing Position (SP) for 30 seconds, while patients with chronic LBP were studied exclusively during a single flexion-extension movement of the trunk with a total duration of 15 seconds. The control group was evaluated in all three ways. Two channels were used whose visualization, in red for the right-hand haemilate and in blue for the left-hand, was compared. For the patient with acute LBP the mean of the recording in PP was calculated and the average of the recording in SP of each haemilate. Patients with chronic LBP were evaluated starting from the upright position held for 5 seconds, then asked to perform a complete flexion movement of the trunk and holding the position for 5 seconds, and then returning back to the starting orthostatic position that is approximately the timing used in previous studies [12, 22-24]. Examples of electromyographic recordings in one healthy subject and in one patient with chronic LBP are shown in Figs. (1, 2). The ratio between the maximum peak value recorded and the average value of 15 seconds was calculated. T-test was conducted to compare the differences between sEMG ratio recorded for the participant, both in acute LBP (PP and SP) vs. healthy and chronic LBP (FRP right and left side) vs. healthy subjects (Tables 1 and 2).
| – | – | N | Mean | SD | SE |
|---|---|---|---|---|---|
| PP | LBP acute | 20 | 1.590 | 0.8239 | 0.1842 |
| Healthy | 20 | 0.795 | 0.4199 | 0.0939 | |
| SP right side | LBP acute | 20 | 4.635 | 1.0554 | 0.2360 |
| Healthy | 20 | 3.180 | 0.6918 | 0.1547 | |
| SP left side | LBP acute | 20 | 4.915 | 1.6096 | 0.3599 |
| Healthy | 20 | 3.345 | 0.6917 | 0.1547 |
T-test was conducted to test for differences between the healthy control and both the chronic and the acute LBP group data. The criterion selected for statistical significance was set at p < 0.05.
| FRP | – | N | Mean | SD | SE | Sign |
|---|---|---|---|---|---|---|
| Rigt side |
LBP chronic | 20 | 4.795 | 1.8366 | 0.4107 | 0.009 |
| Healthy | 20 | 9.46 | 1.0023 | 0.2241 | ||
| Left side |
LBP chronic | 20 | 4.98 | 1.6574 | 0.3706 | 0.006 |
| Healthy | 20 | 9.2 | 0.9274 | 0.2074 |
| – | N | Min | Max | Mean | SD |
|---|---|---|---|---|---|
| PP | 40 | 0.3 | 3.5 | 1.193 | 0.7607 |
| SP right side | 40 | 1.1 | 7.2 | 3.908 | 1.1483 |
| SP left side | 40 | 1.2 | 9.6 | 4.130 | 1.4585 |
| Mean right side | 40 | 0.8 | 4.1 | 2.550 | 0.8064 |
| Mean left side | 40 | 0.8 | 5.1 | 2.686 | 0.8505 |
| FRP right side | 40 | 2.4 | 10.9 | 7.127 | 2.7772 |
| FRP left side | 40 | 2.2 | 10.7 | 7.090 | 2.5147 |
3. RESULTS
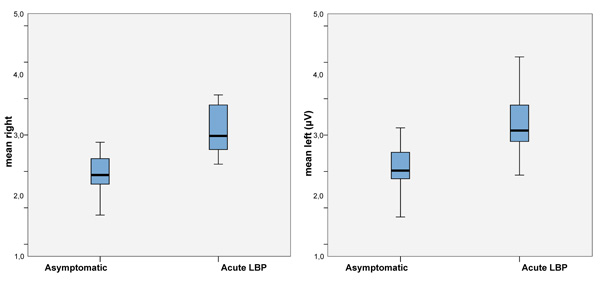
The results of the measurements carried out in the population are shown in Table 3. In all three procedures, significant differences in the surface electromyographic activity between the healthy controls and the one with acute LBP are shown (Table 1 and Fig. 3).
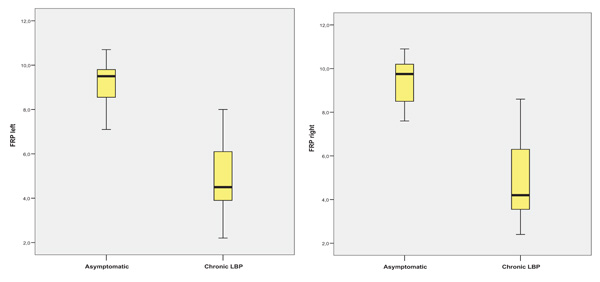
Similarly, the recordings conducted in subjects with chronic LBP showed a significant difference in the side-specific FRP (Flexion-Relaxation Phenomenon) index. The results are shown in Table 2 and Fig. (4).
4. DISCUSSION
In occupational medicine practice, it is important to have an objective evaluation of lumbar pain symptoms in order to evaluate the fitness to work of employees.
In our study, the electromyographic potentials measured in subjects suffering from acute or chronic LBP are significantly different from the values found in healthy control subjects. In healthy subjects, we evaluated PP expecting a threshold value less than 2 μV and a SP threshold value lower than 4 μV. It has been considered appropriate, however, to take into consi-deration at the end of the electromyographic evaluation only the average of the previous values which is always lower than 3 μV in both the hemilates because they are more rep-resentative and less influenced by the individual response. Furthermore, in healthy subjects, the ratio value was always higher than 7 μV in both hemilates. The measurements commonly reported in the literature for Flexion Relaxation Phenomenon (FRR) [24, 25] cannot be compared directly with the ratio adopted in our study given the technical char-acteristics of the electromyograph used in the current study, which provides us with only peak and average peak. Patients with acute LBP have an average of PP and SP values above 3 μV in at least one hemilates and patients with chronic LBP have a ratio value of less than 7 μV. These values are likely to be compatible with an antalgic contracture of the paravertebral muscles, especially in the subjects with acute LBP. In the subjects with chronic LBP, other factors are added, among which the kinesiophobia and a progressive loss of muscle function.Both in subjects with acute and chronic LBP, there is an increase in the difference of values of the two hemilates in each patient, a phenomenon that is also compatible with the adoption of an antalgic posture; moreover, the FRP index is consistently higher in healthy subjects than in those with chronic LBP. In previous studies, FR has been reported to be useful in distinguishing between chronic LBP patients and control subjects [8]. FR deficiency in low subjects affected by chronic low back pain has also been found to be related with self-reported disability [26], pain [27-29], and fear of pain and re-injury [30]. Changes in FR in patients with CLBP patients have been found to be associated with clinical improvement of pain intensity, fear avoidance beliefs [31], and Range-Of-Motion (ROM) [32]. Those outcomes are of interest in evaluating also the work disability of employed subjects, particularly in those involved in heavy weight lifting tasks.
As far as we know, only a few studies were carried out in order to identify with certainty a different response pattern between asymptomatic individuals and those affected by LBP, and results of these studies were not specific for occupational medicine purpose. The implications of this study in the objectivisation of clinical data appear to be potentially large.The main limitations of our study are represented, not only by the relatively limited number of the sample (60 subjects), by also the recording technique such as the low spatial resolution, the possibility of recording only the superficial muscles, the confounding due to the thickness of the subcutaneous fat, the cross-talk of nearby muscles and movement artifacts.As regards the sample size, the results of the statistical analysis seem to be encouraging, however, highlighting a homogeneous behavior of the trend of values in the various groups.Regarding the technical limitations of the method, they are minimized in our study by the selection of the sample (exclusion of obese subjects or strongly overweight and underweight) and by the attention to the execution of the maneuver by the patient.
Although the technique allows a maximum objective relief also through the use of a dedicated software, it requires specific and adequate training both for the peculiar electromyographic patterns and for the discrimination of the clinical variability that in some cases may cause alterations of the same pattern. The interpretation of the operator is therefore fundamental as well as the experience. For example, there are cases in which the patient simulates contractures by voluntarily contracting the muscle, situations that only the trained operator can evaluate with knowledge of the SEMG and its clinical background, especially since scientific studies are lacking. Throughout the study, indicative thresholds for muscle activity have been defined; these emerge from the casuistry examined that, although significant, need expansion. Likewise, studies are deemed necessary to investigate further aspects of electromyographic evaluation specifically in its application in occupational medicine, where there are different conditions depending on the work task.
CONCLUSION
The results of our study show how the SEMG is able to highlight specific patterns and differentiate between the symptomatic subject, the one with LBP and the differential evaluation of patients with acute or chronic backbone. This technique, therefore, represents a valid methodology for the objective acquisition of the functional state of the superficial muscles examined, allowing for accurate identification of the recording patterns characteristic of the different types of lumbar suffering.
In conclusion, we believe that SEMG can be a useful tool in the integration of the clinical-anamnestic data and in the “objectification” of the symptoms, in order to evaluate the work disability. Moreover, it can be helpful for occupational medicine specialist in assessing the clinical improvement of the LBP after treatment for evaluating the fitness for work in these subjects.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
The ethical committee of Tor Vergata Policlinic approved the study with the protocol number “Registro Sperimentazioni 40/18”.
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all the participants prior to data collection.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


