All published articles of this journal are available on ScienceDirect.
The Determinants of Delayed Diagnosis and Treatment Among Malaria Patients in Myanmar: A Cross-Sectional Study
Abstract
Background:
This cross-sectional study was conducted to assess the determining factors for delayed diagnosis and treatment among malaria patients in Myanmar.
Methods:
The sample comprised 220 respondents diagnosed with malaria last year, living in the upper, middle, and lower part of Myanmar. In 2017, data were collected through interviews and analyzed using percentage, mean, standard deviation, and the chi-square test.
Results:
The results affirmed that most of the respondents were in the working age group and of low educational level. They also had poor knowledge and perception of malaria, and more than half of the respondents visited health centers or volunteered for their first treatment of choice. Most respondents received little social support for malaria. There were significant associations between age, sex, education, marital status, occupation, and delayed diagnosis and treatment (p < 0.05). Knowledge and perceptions of malaria, health-seeking behavior, and low social support on malaria services were also significantly associated with delayed malaria diagnosis and treatment (p < 0.05).
Conclusion:
According to the findings, appropriate strengthening of cooperation and collaborations among different sectors upon diagnosis, coverage of treatment services, interventions to increase community awareness, effective communication, behavioral changes, and improved capability of the village health volunteers are evidently needed.
1. INTRODUCTION
Malaria is still a public health problem in over 100 countries [1]. Africa is the most endemic area; Southeast Asia follows as the second-highest place in terms of endemicity, morbidity rates, and mortality rates [2]. Despite the global decline in the number of malaria cases and associated deaths from 2000 to 2015, an estimated 214 million people were diagnosed with malaria and around 438,000 deaths were reported globally, most of which occurred in countries with a great malaria burden and where healthcare systems are weak [3]. Malaria is a public health concern due to (i) changing meteorological characteristics, (ii) the influx of migrant workers who seek employment opportunities in development projects such as mining, plantations, major constructions, and road-building, (iii) delayed diagnosis seeking behavior of patients, and (iv) multi-drug resistance [4]. The prevalence of clients who seek diagnosis and treatment more than 24 hours after the onset of symptoms is 79.4%, while delay caused by providers delayed was only 1.3% [3]. Apart from the cost only for having diagnosis and treatment of malaria, almost 80% of the total expenses were indirect costs associated with seeking treatment [5]. These costs act as a barrier for poor people to assess proper health services and can cause a delay in treatment seeking and increase self-medication practices. Without proper treatment, the delay may tend to develop severe complications and deaths within one week of onset of fever [5]. In meantime, most patients seek their first treatment at drug shops (18%), Markets (15%), private clinic (16%) and Quack (1%) [6].
Myanmar is still considered to have a significant number of reported malaria cases as compared to South East Asian Countries although effective treatment milestones have been achieved in recent years. In 2016, 291 out of 330 townships in Myanmar are malaria endemic and the percentage of the population in those areas is 76.34%. Both mortality and morbidity rate have been reduced from 2011 to 2016. However, there were 105,178 confirmed malaria cases and 21 deaths reported and are one of the highest morbidity rate and mortality rate among the countries in the SEARO region in 2016 [7]. Moreover, since 2009, available data have suggested the emergence of artemisinin resistance in five regions and states of Myanmar, that is in relation to all the currently using three first-line artemisinin-based combination therapy -ACTs (artemether-lumefantrine, artesunate-mefloquine and dihydroartemisinin-piperaquine) [3, 4, 8, 9]. The true magnitude of the malaria problem might be much higher (the majority behaves either self-medication or seeking care in the private formal or informal sectors like general practitioners or quacks) [10, 11]. Nevertheless, according to the World Health Organization (WHO), Greater Mekong Sub-region (GMS) strategies and government committees have been launched to eliminate malaria in Myanmar by the year 2015-2030 [11]. The WHO also encouraged that all malaria suspected clients should have access to early diagnosis by either microscopy or Rapid Diagnosis Tests (RDT) and treatment facility as early as possible. The ideal time is within 24 hours from the onset of symptoms to halt the risk of serious complications and forward transmission [12].
| Characteristics | n | (%) |
|---|---|---|
| Delayed Diagnosis | ||
| 24 hr - 48 hr | 74 | 33.6 |
| 48 hr - 72 hr | 59 | 26.9 |
| > 72 hr | 87 | 39.5 |
| Delayed Treatment | ||
| 24 hr - 48 hr | 72 | 32.7 |
| 48 hr - 72 hr | 54 | 24.5 |
| > 72 hr | 94 | 42.8 |
| Characteristics | Types of Delayed Diagnosis | p-value | Types of Delayed Treatment | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| 24-48 hr | 48-72 hr | >72 hr | 24-48 hr | 48-72 hr | >72 hr | |||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |||
| Age in years | ||||||||
| 15 - 35 | 54 (42.5) | 35 (27.6) | 38 (29.9) | 0.001* | 52 (40.9) | 31 (24.4) | 44 (34.6) | 0.009* |
| >35 | 20 (23) | 24 (25.3) | 49 (51.7) | 20 (21.5) | 23 (24.7) | 50 (53.8) | ||
| Sex | ||||||||
| Male | 41 (29.5) | 33 (23.7) | 65 (46.8) | 0.016* | 41 (29.5) | 28 (20.1) | 70 (50.4) | 0.005* |
| Female | 33 (40.7) | 26 (32.1) | 22 (27.2) | 31 (38.3) | 26 (32.1) | 24 (29.6) | ||
| Education | ||||||||
| Low education | 36 (21.1) | 50 (29.2) | 85 (49.7) | < 0.001* | 34 (19.9) | 45 (26.3) | 92 (53.8) | < 0.001* |
| High education | 38 (77.6) | 9 (18.4) | 2 (4.1) | 38 (77.6) | 9 (18.4) | 2 (4.1) | ||
| Marital status | ||||||||
| Single | 39 (51.3) | 16 (21.1) | 21 (27.6) | < 0.001* | 39 (51.3) | 15 (19.7) | 22 (50) | < 0.001* |
| Married | 35 (24.3) | 43 (29.9) | 66 (45.8) | 33 (22.9) | 39 (27.1) | 72 (50) | ||
| Occupation | ||||||||
| Forest related work | 27 (23.1) | 29 (24.8) | 61 (52.1) | <0.001* | 27 (23.1) | 25 (21.4) | 65 (55.5) | < 0.001* |
| Non-forest related work | 47 (45.6) | 30 (29.1) | 26 (25.2) | 45 (43.5) | 29 (28.2) | 29 (28.2) | ||
| Monthly family income | ||||||||
| < 200,000 Kyats | 20 (27.8) | 19 (26.4) | 33 (45.8) | NS | 19 (26.4) | 18 (25) | 35 (48.6) | NS |
| > 200,000 Kyats | 54 (36.5) | 40 (27) | 54 (36.5) | 53 (35.8) | 36 (24.3) | 59 (39.9) | ||
| Live near forested area (< 1mile) | ||||||||
| Yes | 15 (33.3) | 11 (24.4) | 19 (42.2) | NS | 13 (28.9) | 12 (26.7) | 20 (44.4) | NS |
| No | 59 (33.7) | 48 (27.4) | 68 (38.9) | 59 (33.7) | 42 (24) | 74 (42.3) | ||
| Experiences in health related field | ||||||||
| Yes | 1 (100) | 0 (0) | 0 (0) | NS | 1 (100) | 0 (0) | 0 (0) | NS |
| No | 73 (33.3) | 59 (26.9) | 87 (39.7) | 71 (32.4) | 54 (24.7) | 94 (42.9) | ||
| Previous attempt of malaria | ||||||||
| Yes | 3 (50) | 2 (33.3) | 1 (16.7) | NS | 3 (50) | 2 (33.3) | 1 (16.7) | NS |
| No | 71(33.2) | 57 (26.6) | 86 (40.2) | 69 (32.2) | 52 (24.3) | 93 (43.5) | ||
| Characteristics | Types of Delayed Diagnosis | p-value | Types of Delayed Treatment | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| 24-48 hr | 48-72 hr | >72 hr | 24-48 hr | 48-72 hr | >72 hr | |||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |||
| Knowledge | ||||||||
| Low | 38 (21.6) | 52 (29.5) | 86 (48.9) | <0.001* | 37 (21.1) | 46 (26.1) | 93 (52.8) | <0.001* |
| High | 36 (81.8) | 7 (15.9) | 1 (2.3) | 35 (79.5) | 8 (18.2) | 1 (2.3) | ||
| Health seeking behavior | ||||||||
| Low | 3 (2.7) | 36 (32.1) | 73 (65.2) | <0.001* | 3 (2.7) | 30 (26.8) | 79 (70.5) | <0.001* |
| High | 71 (65.7) | 23 (21.3) | 14 (13.0) | 69 (63.9) | 24 (22.2) | 15 (13.9) | ||
| Overall perception on malaria | ||||||||
| Poor | 33 (19.6) | 51 (30.4) | 84 (50.0) | <0.001* | 33 (19.6) | 44 (26.2) | 91 (54.2) | <0.001* |
| Good | 41 (78.8) | 8 (15.4) | 3 (5.8) | 39 (75) | 10 (19.2) | 3 (5.8) | ||
| Social support | ||||||||
| Low | 32 (18.6) | 55 (32.0) | 85 (49.4) | <0.001* | 32 (18.6) | 48 (27.9) | 92 (53.5) | <0.001* |
| High | 42 (87.5) | 4 (8.3) | 2 (4.2) | 40 (83.3) | 6 (12.5) | 2 (4.2) | ||
Since 2000, the Myanmar Medical Association-Malaria (MMA-Malaria) project began with the support from the Ministry of Health and Sports (MoHS), Vector Borne Disease Control (VBDC) team and WHO to promote an effective prevention against malaria and provide accessible quality diagnosis and standard treatment of malaria to the poor in endemic and high risk townships. According to the 2016 project data, 72% of malaria patients were delayed (>24 hours after onset of symptoms) in seeking diagnosis and treatment. It is still an issue to be addressed by any effective intervention [13]. Early accessible to health service in a timely manner is essential to strengthen case-based surveillance and other interventions [11]. However, one of the major gaps is the lack of formative behavioral research conducted. This study aimed to investigate the determinants of delayed diagnosis and treatment of malaria patients in Myanmar by tracking the background information of malaria patients. Based on the patient’s record of the MMA-Malaria project, delay in diagnosis and treatment of malaria patients in the previous year 2016 was traced for data collection [13].
2. MATERIALS AND METHODS
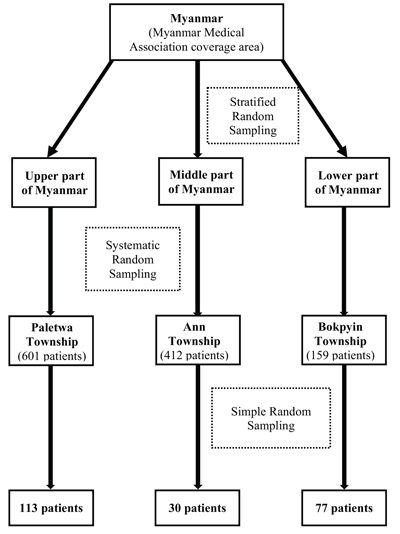
MMA-Malaria project in Myanmar has been implemented in 19 malaria endemic townships around the country. The study sites were divided into three parts, namely an upper, middle and lower part, by using stratified random sampling. One MMA's township was sampled from each part by using simple random sampling. Based on this strategy, Paletwa township (Chin state) in the upper part of Myanmar, Ann township (Rakhine State) in the middle part of Myanmar and Bokpyin township (Tanintharyi Division) in the lower part of Myanmar were selected for inclusion in the study. In each of these three townships, villages are scattered at a significant distance from one another. Thus, roads connecting the villages were often impassable, especially in the rainy season. Geographically, Paletwa township lies on a hilly region, Ann township is located on a flatland, and Bokpyin township is in a coastal area.
The population of interest for the study were malaria-positive patients residing in the selected three townships located in malaria-endemic areas in Myanmar, who were diagnosed during the 12 months preceding the study and who elected to delay diagnosis and standard treatment. According to the 2016 carbonless patients register, in Paletwa, Ann and Bokpyin, there were 761, 543 and 188 malaria positive cases, respectively. Based on the MMA-Malaria Project's data for 2016, 601, 412 and 159 of these cases pertained to patients that delayed seeking care and treatment in Paletwa, Ann and Bokpyin, respectively. Next, systemic random sampling was used to select from these groups a sufficient number of adults (aged 18 or older) (Fig. 1). The sample size for each township was calculated by using the formula; nv = (nc / Nt)*Nv where, nv is the number of samples for each township, nc denotes the total sample size available for the study, Nt is the total number of malaria patients residing in the three townships that delayed seeking treatment, and Nv is the number of such patients in each township. Based on this calculation, 220 individuals were recruited for the present study.
The questionnaire used as a data collection tool was first developed in English and was subsequently translated into Myanmar language. It consisted of six parts, respectively pertaining to general characteristics and disease exposure, knowledge on malaria, health-seeking behaviors, perceptions of malaria, social support for malaria services, and delayed diagnosis and standard treatment of malaria patients. The questionnaire was checked for content validity by an advisory team at Mahidol University, Bangkok, Thailand, as well as by three experts working in the related field. These individuals provided input on the questionnaire correctness, validity, and language clarity. Cronbach's alpha coefficient was calculated to test the questionnaire reliability. Index of Item-Objective Congruence (IOC) was also calculated, yielding 0.778. In addition, a pilot study was conducted with 30 residents of one township from each study zone to assess the smoothness of interview process.
Six educated data collection assistants were selected and underwent a one-day training course, as a part of which they learned how to collect data and control the quality of data. Before collecting the data, field assistants obtained the list of preselected malaria patients’ household addresses. After brief instruction, respondents were asked to fill the informed consent form. After data collection, data was entered and analyzed into the computer by using epi-data and Statistical Package for the Social Sciences (SPSS 22) for quantitative data analysis. Descriptive statistics (mean, standard deviation, minimum, maximum, and percentage) were calculated for the data pertaining to general participant characteristics, knowledge on malaria, health-seeking behavior, perception of malaria, and social support for malaria services. To determine the association between the constructed variables, the chi-squared test was used.
3. RESULTS
Majority of the respondents were delayed more than 72 hours. The respondents who got delayed diagnosis and treatment for more than 72 hours were (39.5%) and (42.8%), respectively (Table 1). The age ranged between 15 - 62 years, the mean age was 34.15 ± SD 10.6. Majority of the respondents (57.7%) were the young age group (18 - 35 years) and 42.3% were older age group (>35 years). Male to female ratio was 1.72:1.00, (63.2%) and (36.8%), respectively. Majority of the respondents finished low education level (primary/ secondary school) (77.7%) followed by 22.3% of high school and above. Two-thirds of the respondents were married (65.5%). Regarding their occupations, more than half of the respondents had forest-related occupations such as agriculture, rubber tapping, migrant, bamboo cutting, and mining workers. More than two-thirds (67.3%) of the respondent's family income were more than 200,000 kyats (˜135USD) per month. Nearly 80% of respondents lived more than one mile away from the forested area. Almost all of them had no experience of working in a health-related field and they had never suffered from malaria before 2016.
For the associations, there were found that factors significantly associated with delayed diagnosis were age (p = 0.001), sex (p = 0.016), education (p < 0.001), marital status (p < 0.001), occupation (p < 0.001) while no significant associations with income, living areas, health-related working experience and previous attempt of malaria. Respondents aged more than 35 years old delayed for diagnosis more than 72 hours for (51.7%), meanwhile, those aged 35 years and lower delayed for diagnosis more than 72 hours for (29.9%). From the result, the older aged group were higher degree delayed than the younger aged group. Male respondents delayed for diagnosis more than 72 hours for (46.8%) and female respondents were (27.2%), the degree of delayed was higher in male respondents than female. The respondents who had low education delayed for malaria diagnosis more than 72 hours for (49.7%), meanwhile, those who had high education delayed for diagnosis more than 72 hours for (4.1%). According to the result, low educated respondents were higher degree delayed than high educated respondents. Respondents who are single delayed for diagnosis more than 72 hours for (27.6%) and respondents who are married delayed for diagnosis more than 72 hours for (45.8%). As the result, the degree of delayed was higher in married than single respondents. Forest-related workers delayed for diagnosis more than 72 hours for (52.1%), meanwhile, nonforest related workers have delayed diagnosis more than 72 hours for (25.2%). The degree of delayed was higher in forest-related workers than other type of occupation.
There were associations between independent variables and delayed treatment of malaria. It was found that factors significantly associated with delayed effective treatment were age (p = 0.009), sex (p = 0.005), education levels (p < 0.001), marital status (p < 0.001) and occupation (p < 0.001). Respondents aged more than 35 years old delayed treatment more than 72 hours for (53.8%), meanwhile those aged 35 years and lower delayed treatment more than 72 hours for (34.6%). From the result, older aged group were higher degree delayed than the younger aged group. Male respondents delayed for treatment more than 72 hours for (50.0%) and female respondents delayed for treatment more than 72 hours for (29.6%). The degree of delayed was higher in male respondents than female. The respondents who had low education delayed treatment more than 72 hours for (53.8%), meanwhile who had high education were delayed treatment more than 72 hours for (4.1%). According to the result, low educated respondents were higher degree delayed than those who had high education. Respondents who are single delayed treatment more than 72 hours for (29.0%) and respondents who are married delayed treatment more than 72 hours for (50.0%). As the result, the degree of delayed was higher in married than single respondents. Forest-related workers delayed treatment more than 72 hours for (55.5%), meanwhile, nonforest related workers delayed treatment more than 72 hours for (28.2%). The degree of delayed was higher in forest-related workers than others type of occupation (Table 2).
In addition, there were associations between knowledge on malaria (p < 0.001), perception on malaria (p < 0.001), care-seeking behaviors (p < 0.001), social support on malaria services (p < 0.001) and delayed seeking diagnosis and the delayed treatment at p < 0.05 level. For overall knowledge of malaria, most of the respondents had a low level of knowledge (80.0%), whereas 20% had a high level. The mean score was 8.4 which was 52.5% of the total score. The respondents who had a low level of knowledge on malaria delayed for diagnosis more than 72 hours for (48.9%) and high level of knowledge on malaria delayed for diagnosis more than 72 hours for (2.3%) only, the degree of delayed was higher at a low level of knowledge than a high level of knowledge. The respondents who had a low level of knowledge on malaria delayed treatment more than 72 hours for (52.8%) meanwhile those who had a high level of knowledge on malaria delayed treatment more than 72 hours only for (2.3%). The degree of delayed was higher in respondents who had a low level of knowledge than those who had a high level of knowledge. Respondents who had low health-seeking behaviors delayed for diagnosis more than 72 hours for (65.2%) and respondents who had good health seeking behavior delayed diagnosis more than 72 hours for (13.0%). The degree was higher in the respondents who had low health-seeking behavior than those who had high health-seeking behaviors. Respondents who had low health-seeking behaviors delayed treatment more than 72 hours for (70.5%) and those who had good health seeking behavior delayed treatment more than 72 hours for (13.9%). The degree was higher in the respondents who had low health-seeking behavior than those who had high health-seeking behaviors.
For the overall perception, two third of them had a poor level of perception whereas 23.6% had a high level of perception. The mean score of the overall perception was 32.9 and SD was 6.6, which was (68.5%) of the total score. Regarding overall perception association with delayed diagnosis and treatment, half of the respondents who had poor perception delayed for diagnosis more than 72 hours while those who had good perception delayed for diagnosis more than 72 hours for (5.8%). Most of the respondents (78.2%) got the overall support at a low level and high level (21.8%). The mean score of the overall social support was 13.4, SD±5.7, which was 79.6% of the total scored. Respondents who got low to moderate social support for malaria services delayed for diagnosis more than 72 hours for (49.4%) while those who got high social support delayed for diagnosis more than 72 hours only for (4.2%). The degree was higher in the respondents who got low social support than those who got high social support (Table 3).
4. DISCUSSION
It was divided into two types: delayed diagnosis and delayed treatment; in addition, it was classified using three degrees: (a) 24 - 48 hours, (b) 48 - 72 hours, and (c) more than 72 hours. All of the respondents were mostly delayed in both diagnosis and effective treatment. These delays may be due to respondents’ low knowledge levels and working age group; they could not go to the clinic within 24 hours, and they did not know how to predict malaria by themselves. In addition, most of the respondents lived in either the malaria-endemic area or remote areas, which made it difficult for them to access the health center. The majority of respondents had delays in diagnosis of more than 72 hours because the selected township had poor public transportation and no health centers. Also, the malaria patients did not know the signs and symptoms of malaria and its complications; therefore, patients did not know exactly when they had malaria. Delayed malaria diagnosis and delay in effective treatment were the worst in Paletwa Township because the township was in a hilly region, and travel was difficult. The previous study in Wa region, Myanmar found that 87.5% of respondents were delayed in malaria treatment because of low family income and distance from health facilities [14]. Another study in the endemic area of rural Myanmar showed that 84.2% of respondents were delayed in seeking malaria treatment, and only a few were not delayed in seeking effective treatment within 24 hours after the onset of the first symptoms of malaria [15].
Delay times were longer in older age groups compared with younger age groups because most of the older respondents were dependent on the family, and they could not go to clinics by themselves. In addition, the older villagers relied on traditional medicine and trusted spiritual and traditional beliefs. The degree of delay for younger age groups was not high, but they were also delayed; the younger groups thought that they had high immunity and that malaria would, therefore, resolve naturally, so they did not go to health centers within 24 hours. These respondents were also in the working age groups, so they could not go to health centers easily when they were working, especially if they were working in the forest. This was similar to the previous study in Myanmar and the Cambodian border area in 2013, which found that the respondents over 30 years of age were more likely to delay than the other age groups [16]. Regarding gender, two-thirds of the respondents were male. Most of them were forest-related workers and, thus, they were more prone to infection and to delayed diagnosis and treatment. Most male respondents had low education levels, and they did not know the severity and complications of malaria; therefore, they self-medicated and did not go to health centers within 24 hours. One of the studies in Myanmar showed that male respondents more often delayed treatment than females [15]. Another study in Mae Ramat district, Tak Province, Thailand (located in the Thailand - Myanmar border area) showed that the number of male respondents who were delayed was predominantly higher than female respondents; therefore, males might be a high-risk group for contracting malaria, and most of them were delayed in malaria diagnosis and effective treatment [17].
The study, however, observed that more than two-thirds of them had low levels of education (i.e., illiteracy, primary and secondary school), and the results showed that the lower the knowledge level, the more prolonged the delay in diagnosis and effective treatment. This may have been because most of the respondents who had low education levels did not attend to the health education section, and they were not interested about health information provided by the government or MMA or some other NGOs. Marital status was also associated with delays in malaria diagnosis and effective treatment. Married respondents were 1.89 times more likely than single respondents to delay diagnosis and treatment. The married respondents thought that fevers with chills and rigors were not important, and they were more focused on their families and their economic status, so they relied on self-treatment and traditional healers. The 2015 study in rural Myanmar similarly found that most of the respondents (75.2%) were married and were 1.41 times more likely to delay than others [15]. Regarding occupation, most respondents were forest-related workers, and they were more delayed in the diagnosis and effective treatment because they did not know they were more prone to infection. These workers had difficulty with transportation, and they could not easily go to health centers when they were getting ill. In addition, their job behaviors were also one of the reasons for delays; they built temporary houses and lived in the forest, and so they did not have easy access to health centers. One of the studies in Thailand in 2001 showed that forest-related workers had negative health-seeking behavior and more delays in diagnosis and treatment than other occupations (e.g., seller, street vendor, or employee of government) [17].
Other remaining variables (e.g., monthly family income, living near forested areas, experience in health-related fields, and previous illnesses with malaria) were not associated with delayed malaria diagnosis and effective treatment. This was a similar finding to that of the 2015 study in rural Myanmar, which showed no association between income and delayed malaria treatment [15]. As to income of the respondents, more than two-thirds of them earned more than enough money to afford to go to clinics; however, they delayed because of the unavailability of health-care personnel. Moreover, their work, families, and social activities might also have led to delayed diagnosis and effective treatment. Another variable, disease exposure, was not associated with delayed diagnosis and effective treatment because almost all (i.e., nearly 100%) of the respondents were not experienced in health-related fields, and they had not suffered from malaria before 2016.
This study found an association between knowledge of malaria and delayed malaria diagnosis and treatment; however, the results showed that more than half of the respondents had low levels of knowledge, and only a few respondents had higher levels of knowledge about malaria. The respondents who had low levels of knowledge about the disease were more likely to have delayed diagnosis and treatment. The previous study in Myanmar found the similar result, that 56.1% of respondents had poor knowledge so that they went to informal health center including traditional healers and quacks and treated after 72 hours from the onset of symptom started [15]. This was also similar to a study in Mae Sot district, Tak province, Thailand which showed that there was a significantly positive correlation between knowledge on malaria and treatment seeking behavior [18]. The respondents in this study have several choices as seeking treatments for illness. This study found that more than half of them chose health center and volunteer. Some of them still chose traditional healer and quacks. However, all of the respondents delayed more than 24 hours, even they choose correct health services. This may be due to the availability of volunteers that they also go to work for their income, thus sometimes they are not in the village when the patients need [19]. In addition, the respondents thought that the cost for malaria diagnosis and treatment is expensive, difficult to find health care personal and distance barrier. Drug vendors sell fake drugs or ineffective drugs, which the respondents can easily buy so that they do not want to go health center. The previous study in Myanmar showed that health-seeking behavior and services accessibility were associated with delayed in malaria treatment [15]. Also, a study in Myanmar described that roles of assigned village health volunteers are questionable and need to be strengthened [19].
Regarding the perception, there was an association between perception and delayed malaria diagnosis and effective treatment in this study. This result implied that the respondents who had poor perception went to clinic later than the respondents who had a good perception of malaria. Interestingly, 5.8% of respondents went to the clinic more than 72 hours and had a good perception on malaria. The reason might be due to civil war especially in Paletwa township, respondents had good perception but they cannot go to health center at the time of illness. It was similar to the previous study in Zanazibar in 2013, which showed that there was an association between perception and seeking malaria treatment [20]. Contrastively, the study done in Tak province, Thailand in 2007 found no association between them and showed different result compare to this study [17]. There was an association between social support on malaria services and delayed malaria diagnosis and effective treatment. Half of the respondents had low social support for malaria services. Less than 30% of the respondents got support all the time from family, friends, community and volunteers but more than half of them got support sometimes. Most of the respondents never got final support from all of the social support on malaria services. Therefore, they did not go to malaria services within 24 hours and they went to health center or volunteer when it is more severe. Some rural areas where people have low income were presented that villagers do not want to pay for malaria service. This may lead to delayed in malaria diagnosis and effective treatment. One of the previous studies in Myanmar showed that respondents who can afford for the treatment also significantly associated with seeking malaria treatment and 1.54 times more less likely to delay than those who cannot afford [15]. Difficulty in transportation is another problem in villages; transportation was not convenient and difficult to access, most of the respondents used their own vehicles to get malaria services. Some respondents lived far away from the malaria services, thus, patients do not want to go to health care center and they more preferred to choose the nearest place for malaria services.
5. LIMITATIONS OF THE STUDY
This study provides a list of the factors influencing the delayed diagnosis and treatment of malaria in Myanmar. The findings were limited since the study population was rather selective, as it was only conducted among the respondents who lived in malaria-endemic area and were present at the time of data collection. This study was conducted based on the answers from the respondents and hence, there was a possibility of recall bias. This study did not investigate the details of previous experience about the illness and its complications. The patients who were infected with malaria and emerged successful in both diagnosis and the effective treatment of the disease were not included in this study. This study was based on the medical record of MMA and may have missed a few patients from other projects or government hospitals. These may contain a recall bias in the respondents’ memories as there were problem in recalling the affecting factors to a delay in seeking treatment for malaria during the last year and it depends on the severity of the illness.
CONCLUSION
In this study, the problems, needs, types and degree of the delay in malaria diagnosis and its treatment were explored. New interventions or approaches should be introduced and implemented to fill these gaps. For provider sectors’ recommendations, the national malaria treatment guideline should be updated and distributed among service providers from the government, NGOs, INGOs and private clinics in all areas, especially in remote areas. In terms of medical management by the Myanmar Government, the medical licensing system should be enhanced to ensure that the private clinics could be held to maintain the standard, which could dictate the quality of services and control the cost. For village health volunteers, the updated guideline must be provided to them to be able to deliver quality diagnosis and standard treatment guidelines and to disseminate proper health messages to the patients. The active case detection should be promoted to find out missing or asymptomatic malaria cases. From a community point of view, they should be encouraged to participate in health activities such as health education, community health talks etc.
As the study design is just a quantitative study, a mixed method such as qualitative and quantitative methods should also be conducted with in-depth interview or focus group discussion to explore more information and the causes that effect on delayed diagnosis and treatment. In order to get reliable and meaningful results, the larger sample size would represent the malaria patients of all parts of Myanmar. The previous experience of illness, complications of illness, cultural and psychological factors should also be addressed in the future researches.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
The data collection was carried out with the approval of the Ethical Committee from Mahidol University, Bangkok, Thailand (Reference: COA. No. MUPH 2017-053).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
ACKNOWLEDGEMENTS
Declared none.


