All published articles of this journal are available on ScienceDirect.
Impact of a Health System's Three-Pronged Strategy to Address the Opioid Epidemic in DE, PA, and WV, 2013-2017
Abstract
Background:
In the past two decades, from 1999-2017, more than 700,000 people have died from a drug overdose in the United States. In 2017, more than 68% of the drug overdose deaths involved an opioid, and the opioid death rate was six times higher than in 1999. Although treatable, opioid addiction has significant health consequences; and evidence-based, data-driven models addressing these opioid-related factors remain sparse.
Objectives:
To help stem this epidemic, Highmark Inc., a national health plan as well as the second largest integrated delivery and financing system in America, developed, implemented and evaluated a series of quality management-focused opioid interventions utilizing a three-pronged public health approach. We focused on more effectively managing pain to reduce the need for opioids (primary prevention); when needed, prescribing opioids according to safe prescribing guidelines (secondary prevention); and for those with Opioid Use Disorder (OUD), ensuring access to effective treatment to reduce morbidity/mortality (tertiary prevention) for our members.
Methods:
We deployed a series of evidence-based and data-driven interventions utilizing clinical guidelines, integrated and coordinated infrastructures, and community-based participatory research frameworks within our service areas of Delaware, Pennsylvania, and West Virginia. We examined medical and pharmacy claims for combined data years 2013-2017 by age, product (commercial, diagnosis with OUD), total Opioid prescription (RX) fill rate (per 1,000 members), opioid use by dose (dosage level by Morphine Milligram Equivalents), opioid use by duration (number days of opioid use), rate per 1,000 members diagnosed with OUD, and geography.
Results:
Improvements in total Opioid RX fills, opioid use by dose and duration for members diagnosed with OUD. Over these years, a decrease of 19% of total Opioid RX fills; shorter durations and the majority of these members switched to 7 days or less of opioid use; and a reduction by 13 percentage point of the number of members on higher strength 20+ MMEs opioids resulted.
Conclusion:
These findings may help inform nationwide opioid-focused efforts and set priorities.
1. INTRODUCTION
In the United States, the number of opioid overdoses has reached epidemic proportions [1-3]. In the past two decades (1999-2017), more than 700,000 people have died from drug overdose in the United States [1-3]. In 2017, more than 68 percent of the drug overdose deaths involved an opioid, and the opioid death rate was six times higher than in 1999 [1-3]. The top six states with the highest rates of opioid-related overdose death were West Virginia (WV) (57.8 per 100,000 people), followed by Ohio (OH) (46.3 per 100,000 people), Penn-sylvania (PA) (44.3 per 100,000 people), the District of Columbia (DC) (44.0 per 100,000 people), Kentucky (KY) (37.2 per 100,000 people), and Delaware (DE) (37.0 per 100,000 people). Three of these states (DE, PA, and WV) are within our Highmark Inc. service area [4].
People with Opioid Use Disorder (OUD) are seen with all educational and socioeconomic backgrounds [5,6]. Given that both epigenetics and related social determinants of health are associated with opioid addiction and fatal and non-fatal overdoses, other reported factors may have also played a role [7-12]. These include less-than-optimal legislation; drug industry supply/demand; health policy; safe prescribing practices; quality of data collection; multi-sector partnerships to address the opioid epidemic; monitoring and tracking of drug misuse, abuse, and fraud; provider-focused education and guidance for safe prescribing; and access to and availability of behavioral health services and treatment options, among others [7-12]. Evidence-based, data-driven models addressing these opioid-related factors remain sparse [7-12]. Individuals can become addicted to opioid in as little as five days of exposure [1, 9]. Furthermore, dose and duration of an opioid prescription is linked to the likelihood of a patient being diagnosed with OUD [1,9,13,14].
It is well documented that the rise in opioid overdose deaths involving any opioid is multifactorial [12-14]. Three distinct waves are commonly reported [1]: Wave 1 began in 1990, with a rise in prescription opioid overdose deaths [1,15]. Wave 2 began in 2010, with a rise in heroin overdose deaths. Wave 3 began in 2015, with a rise in synthetic opioid (illicitly-manufactured fentanyl) overdose deaths [1]. Opioids can be prescribed to patients by authorized healthcare practitioners to treat pain, but serious risks and side effects may result [1]. Non-medical use of prescription drugs exists [1,13,16,17], and typically involves a person taking more than the prescribed dose, taking a drug prescribed for another person, or taking a drug obtained illegally or without a legitimate prescription [1,13,17]. More than 12 million people report having misused these medications [12,17]. Health care costs for opioid abusers were eight times higher than for non-abusers [18]. Employees with substance abuse disorder have three times more in health care costs of the average worker, nearly $2,500 in absenteeism [19]. Strategies to prevent opioid misuse, abuse, and diversion may reduce the associated costs due to excessive healthcare utilization [20]. For insured members, the Blue Cross Blue Shield (BCBS) Health Index identifies OUD as the fifth-most impactful condition affecting the health of commercially insured members in America [6]. Given that OUD can be prevented [2], evidence-based strategies are needed to help reduce OUD risk; and to increase access to OUD treatment if the person has developed dependence.
1.1. Health Systems-Level Efforts to Combat the Opioid Epidemic.
Integrated Delivery and Financing Systems (IDFSs) can play a key role in stemming the tide of the opioid crisis because of their ability to control more processes from end-to-end, including alignment of payment and benefit structures [21]. Highmark Inc. (hereinafter referred to as Highmark) was one of the early health systems in the United States to confront the opioid epidemic due to being at the epicenter of the epidemic within its service areas of DE, PA, and WV [4]. Highmark is a national, diversified health care organization serving members through its businesses in health insurance, dental insurance, vision care, and reinsurance. Our mission is to make high-quality health care readily available, easily understandable and truly affordable in the communities we serve [4].
2. OBJECTIVE
As a public health crisis, it is important to consider a broad and comprehensive framework for intervening to mitigate harm and further spread of opioid addiction. Unlike other types of epidemics, this one was iatrogenic, due to a combination of social factors, pharmaceutical company marketing and some medical association support, leading to overprescribing of opioids in the late 1990's for acute and chronic pain [1,22]. With 11% of the U.S. population having some form of chronic pain, it is important to realize how this overprescribing created a large population of Americans conditioned to be or become addicted with escalating risk beyond just the addiction itself [23]. Generally, someone with chronic back pain would not seek street drugs for the relief of that pain. However, the prevailing medical practice of the late 1990's and early 2000's was to prescribe opioids more liberally for acute and chronic pain. This practice not only created persons with addiction, but also created a population of people who were conditioned now to seek opioids for pain relief that they would not otherwise had considered. If the legal source is cut off or insufficient, it is now a plausible alternative for this person to consider the cheaper and more potent street drugs. And that is exactly what we have seen. During the "second wave" of the opioid crisis, four in five (80%) of new heroin users started out misusing prescription painkillers [24]. This switch to street injectable drugs brings all of the additional issues of medical complications due to non-sterile injections, infectious diseases, criminal activity and unregulated drug compounds. The introduction of more deadly forms such as fentanyl has increased the stakes and the importance of interrupting this pathway as well as aggressive identification and rehabilitation for those with OUD.
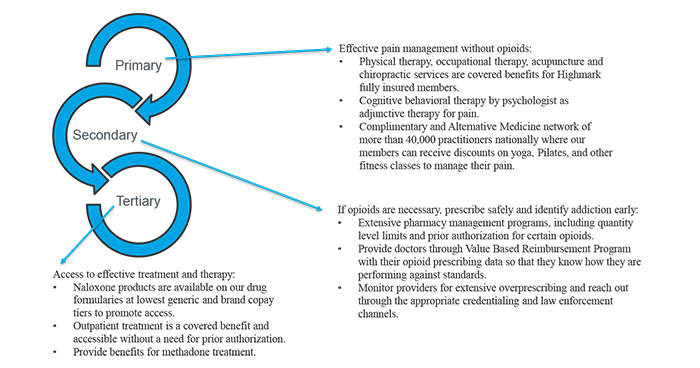
As with other epidemics, a public health prevention framework seems particularly useful to address root causes and effects [5]. The recognition of "Deaths of Despair", in predominately middle-aged white males of which opioid addiction and overdoses are one of the manifestations which point to the underlying structural and social determinant factors that must be addressed over time to turn the tide on the crisis [7-35]. Reducing opioid prescriptions in the context of a comprehensive strategy would more likely result in sustainable improvement and reduction in the cost, disruption, morbidity and mortality of opioid addiction. With this approach in mind, Highmark developed, implemented and evaluated quality management-focused opioid interventions utilizing such a strategy (Fig. 1). The strategy focused on three preventive leverage points:
- Primary Prevention: focused on the more appropriate management of pain to reduce the need to use opioids. This includes the application of evidence-based traditional and alternative treatments for pain.
- Secondary Prevention: for those circumstances where opioids were indicated, the aim was to reduce overprescribing of opioids by putting in place tools and controls to encourage safe prescribing of opioids consistent with the CDC guidelines [8,9]. This also included de-escalating protocols for those on high doses.
- Tertiary Prevention: for those with OUD the goal was to reduce morbidity, mortality and family/community disruption while proactively offering interventions to support a lasting recovery.
These were provider, member, and community-focused interventions in DE, PA, and WV, and executed over the time period. We examined medical and pharmacy claims for data (2013-2017) by age (18-65 years of age), product (commercial, diagnosis with OUD), total Opioid RX fills (per 1,000 members), opioid use by dose (dosage level by MME), opioid use by duration (number days of opioid use), rate per 1,000 members diagnosed with OUD, and region (DE, PA, and WV). We also discuss the integrated and coordinated strategies needed for the deployment of an integrated public health approach used to address the current opioid epidemic.
3. STUDY DATA AND METHODS
This opioid work was completed by Highmark Inc. for quality assurance, and now these collected data were used to conduct a retrospective review for research purposes. This retrospective review was approved by the Allegheny Singer Research Institute - WPAHS Institutional Review Board.
3.1. Outcomes and Data
We examined the medical and pharmacy claims of Highmark commercially insured members per calendar year from 2013 to 2017. Highmark members with a diagnosis of cancer, HIV and/or who had received services for palliative or hospice care were excluded. All other eligible adult Highmark commercial members under age 65 were included in this analysis. Our final total sample size consisted of, on average, 9,700 OUD diagnosed commercial members per year. Data were examined by regions defined as our service area of DE, PA, and WV.
Prescription claims data were used to estimate raw opioid prescription counts and opioid prescription dosage and duration. Member-level dose and duration were calculated based on taking the average MME dosage and total prescription days for all prescriptions a member received within a calendar year. Medical claims were used to measure the number of Highmark members with an ICD code-based diagnosis of OUD (ICD 9 and ICD 10 Z79.891). Rates were computed on a per 1,000 member basis or percentage basis, where noted. These outcome measures are used by others in these kinds of opioid use evaluations [1,8,11,14,25].
Statistical Analysis System (SAS 9.5 version, NC) was used for these analyses. Operational data and opioid dashboards used provided tracking and monitoring data in real time over the observation periods.
3.1.1. Deployment of an Integrated Public Health Approach Used to Address the Current Opioid Epidemic
3.1.1.1. Highmark's Three-Pronged Strategy
During both the pre-opioid epidemic and during its declared national state of emergency period, traditional utilization management approaches appeared to be ineffective in slowing the spread of the epidemic. We believed more could be done. We also recognized that no single entity could do this alone [1]. We began working with many partners outside of Highmark as well as coordinating teams internally, including our medical policy,pharmacy, and fraud teams, among others. Over the years, our Financial Investigations and Provider Review (FIPR) department worked with the U.S. Attorney's Office for the Western District of Pennsylvania in its ongoing fight against opioids [26]. This work with the U.S. Attorney's Opioid Fraud Task Force marks the latest milestone in the department's continued mission to combat health care fraud. This work resulted in millions of dollars saved [26]. Dollars recovered from medical claim reimbursements made to providers as a result of fraud, waste and abuse (FWA), savings in form of policy changes that have helped close risk areas for FWA, as well as prevented losses such as medical claims, that have been identified as being improper FWA and have been stopped [26].
Leveraging claims data, in 2016, we also partnered with axial Healthcare® to equip providers in WV with evidence-based decision support tools on pain management and opioid therapy [26]. Driven by analytics and supplemented by consultation with axial Healthcare®'s licensed pharmacists, these tools gave providers insight into their own opioid prescribing patterns and guidance on clinical best practices for opioid prescribing [26]. Results were impactful, as more than 250 providers received extensive, targeted clinical consultation on pain management. Patients receiving opioids from multiple prescribers dropped by more than 28%, and patients receiving opioids alongside certain sedatives - a significant risk factor for opioid overdose - fell by more than 25% [26]. In 2017, we began the process to scale up this program, and expanded it to PA in 2018 (data in progress).
3.1.1.2. Prong 1: Primary Prevention
Prong 1 was focused on effective pain management. This meant facilitating our member's access to the full spectrum of evidence-based pain management options, including acupuncture, massage, physical therapy and more.We offered discounts on other services through a Complementary and Alternative Medicine network of more than 40,000 practitioners nationally, where our members can receive access to yoga, Pilates, and other fitness classes to manage their pain. We also worked closely with our Allegheny Health Network (AHN) partners who established an innovative pain management clinic housed in the AHN Center of Excellence [27]. A principal goal was to treat the whole person by integrating behavioral health and primary care. To start, patients were screened for OUD at a number of AHN's primary care practices. Screenings began at Forbes Family Medicine where the physicians utilized the 'Screening, Brief Intervention, and Referral to Treatment' (SBIRT) protocol - an evidence based practice used to identify, reduce, and prevent problematic use, abuse, and dependence on alcohol and illicit drugs.
3.1.1.3. Prong 2: Secondary Prevention
Prong 2 was focused on safe prescribing. In this category, we wanted to ensure if opioids were necessary, that they were prescribed safely; and we identified addiction risk and issues early. We promoted the CDC's opioid prescriber guidelines' "go slow and low" approach [1,25]. This meant that authorized health care providers should advance to opioids for their patients as a last option and start with the lowest dose for the shortest duration. Extensive pharmacy management programs, including quantity level limits and prior authorization for certain opioid prescribing patterns, and pharmacy "lock-in" to prevent "doctor shopping" when abusive use patterns were identified and coordination with our FIPR unit were deployed. Our Provider Services strategy included measurement and education for physicians through our True Performance Program regarding their opioid prescribing patterns. It also monitored providers for extensive overprescribing and resources reach out through the appropriate credentialing and law enforcement channels.
3.1.1.4. Prong 3: Tertiary Prevention
Prong 3 was focused on effective treatment and therapy for those that have OUD to reduce morbidity and mortality and the negative impact on families and communities. Highmark made Naloxone® products available on our drug formularies at the lowest generic and brand co-pay tiers to promote access. Outpatient treatment for detox and maintenance Medication Assisted Treatment (MAT) was also a covered benefit and accessible without a need for prior authorization. Because maintenance of OUD on methadone reduces the incidence of fatal and non-fatal heroin overdoses [16, 22] we also provided benefits for methadone treatment for WV (2017) and PA (2018) to ensure our members can start on the road to recovery.
3.1.2. Health System's Integrated and Coordinated Infrastructures to Make an Impact on the Opioid Crisis
3.1.2.1. Organizational Design and Culture
Changing a culture of an organization to address the opioid crisis is not an easy task; it is a large-scale undertaking and requires state-specific tools that need to be put in place [1, 29-32]. Our OUD-related departments were redesigned to reflect co-ordinated, multidisciplinary and collaborative efforts to improve our efficiency, accuracy, and response time for serving our members, and with added emphasis in year 2017-2018. First, we further enabled our health system to work together [26,30-32] to prepare for, prevent, respond to, recover from, and mitigate the effects of the opioid crisis in DE, PA, and WV. This involved operational and system-level changes, including aligning our data-driven interventions with our mission and vision, increasing funds for the opioid work in the Highmark budget, redesigning units and increasing human resource capacity to better address the persistent wide variations in OUD and opioid overdoses by state.
3.1.2.2. Committee Oversight and Quality Opioid Data Collection, Surveillance, and Trends Data
Since 2017, as standard practice in the opioid space, our ongoing opioid-focused initiatives were informed by published research, regulation, direct input (internal and external providers and content experts), operational data reporting, and department leadership. In 2017, we began addressing the need to establish a Health Plan Opioid Operating Committee (HPOOC). HPOOC, under the auspice (an enterprise wide OOC umbrella), and with oversight of Highmark, AHN, and Gateway, fully implemented in 2018, met monthly to review data, report on initiatives happening across the Health Plan and discuss potential strategic initiatives to move forward. In 2017, we further addressed the need to have operational data reporting in real time. We then established our Health Plan Opioid Data Dashboard that measures our progress in real time, and against BCBS Association's (BCBSA®) national opioid health outcomes data [6] Optum® benchmarks [12], and CDC's [1,25] opioid guidelines.
3.1.2.3. Redesigned Units
We further improved opioid-focused content expertise across the health system by increasing resources in related departments, including medical teams; policy teams; clinical pharmacy teams; clinical services teams; behavioral health services teams; abuse, misuse, fraud prevention teams; and education and communication teams, among others. We also deployed cross-trained, people-shared staff and resources.
3.1.2.4. Multi-Sector Partnerships and CBPR Frameworks
We enacted significant programs and policy changes designed to help members as they battle opioid abuse and addiction in our community focused and partner-driven war on opioids. These were provider, member, and community-focused interventions. Because no single entity can do this alone [1, 30-32], we collaborated with local, state, and federal agencies; local school districts; businesses; law and drug enforcement; and community-and faith-based organizations. Our community-based interventions utilized evidence-based strategies and community-based participatory (CBPR) frameworks [31]. All related strands of our community participated in this discussion, and with equal decision-making helped inform all aspects of the opioid work at the local level [31]. This helped to ensure that our interventions were formed "with" the community rather than "about" the community to combine knowledge with actions that improve community health1 [31-32]. It also helped us build on the strengths and resources of the community, and identify processes needed to maintain our partnerships over time [1,30].
3.1.2.5. Highmark Coordinates with Highmark Foundation, Highmark Caring Place, and Allegheny Health Network
We also collaborated with our Highmark Foundation®, Highmark Caring Place®, and the Allegheny Health Network®(AHN). Highmark contributed $600,000 in multi-year support for programs in DE, PA, and WV to address local needs [26]. In 2017, to help further improve opioid-focused efforts by first responders in our community [26], our Highmark Foundation®, a philanthropic arm of Highmark, contributed another $120,000, including funding for police departments to carry Naloxone®. These efforts resulted in making NaloxoneA(®) available to non-medical first responders. The Highmark Caring Place®, our center for grieving children, adolescents and their families, worked with families after the overdose death of a parent or child [35]. In 2017, Highmark Caring Place served 144 children due to an opioid death, an increase from five children served in 2014 [26]. Thus, further providing support for grieving children due to opioid death. In 2016-2017, state-specific Drug Takeback/Disposal events were also deployed to provide opportunities in the community for disposal of any unused and expired prescription drugs. Because members of our community were deeply affected by the opioid epidemic, AHN utilized an innovative approach to meet the multi-faceted needs of those with opioid use disorder 44. AHN's Addiction Medicine Program aimed to help patients overcome their addiction and begin a journey to healthier living. Maternal Health and Perinatal Hope programs were deployed, and Emergency Room Warm Hand-off pilot programs with direct case management referrals were also launched at AHN(published elsewhere) [27].
4. STUDY RESULTS
Total Opioid RX fills per 1,000 Members.
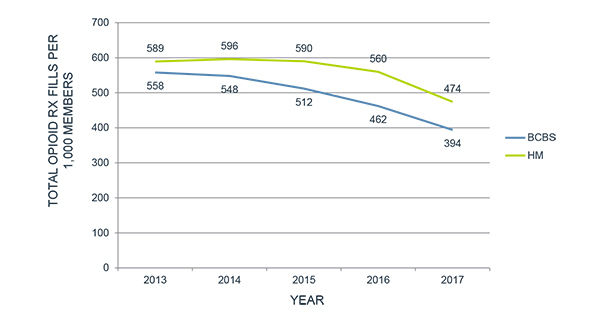
As shown in Fig. (2), between 2013 and 2017, there was a 19 percent decrease (starting point 589, ending point of 474) across the eligible Highmark membership of total opioid prescription fills normalized per 1,000 members. A 15% decrease was observed between 2016 and 2017, and this was a sharper decrease than observed in previous years between 2013 and 2016. In terms of RX fills by geography, the results varied by state between 2016 and 2017, with the biggest decreases in WV and PA at 16% each and 10% in DE. This trend was similar to the BCBSA® national averages for commercial members. To also compare our averages with non-BCBSA® national averages, we ran a secondary analysis and measured our results to Optum® benchmarks, which included both commercial and Medicare Advantage members. A similar trend was also observed.
Opioid Use by Duration and Opioid Prescription average Dosage Level by MME.
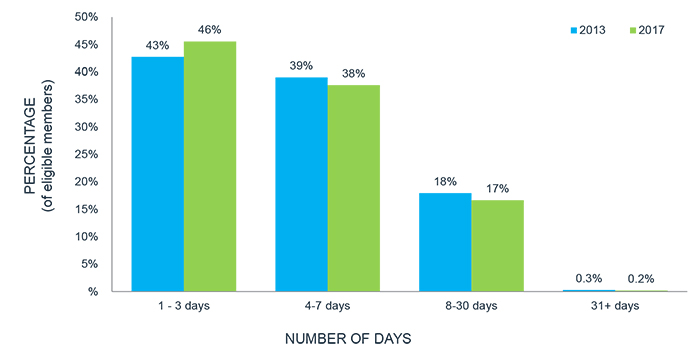
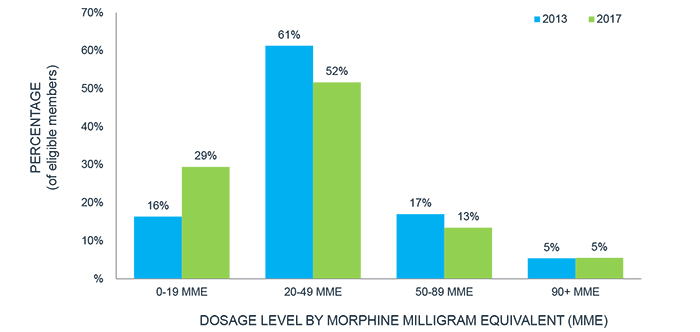
As shown in Fig. (3), over the course of four years, significant positive changes were seen across the eligible Highmark member population. There was a shift in the duration of opioid prescriptions from being 4 or more days to being 3 days or fewer. The same trend was seen across BCBSA® national trends for opioid use by duration. As shown in Fig. (4), when looking at average opioid prescription dosage in MME, Highmark exhibited significant shifts in decreasing the potency of the prescriptions to lower-dose and lower MME prescriptions. For those members who previously would have been prescribed higher doses, in particular in the 20-89 MME range, there was a significant shift to lower dose prescriptions, notably 0-19 MME. While trends were similar to BCBSA® national averages and Optum® benchmarks (data not shown), Highmark exhibited superior results in lowering the average strength of opioid prescriptions compared to the BCBSA®.
4.1. Rate Per 1000 Members Diagnosed with OUD
In 2017, the Highmark rate was 7.72 per 1,000 members, up from 4.12 per 1,000 members in 2013. Results also showed that in 2017, there were less commercial members (n=9,811) with diagnosed OUD than the previous year, showing a decrease from n=10,397 in 2016.
5. DISCUSSION
Our results showed decreases in the total number of opioid RX fills; opioid use by duration; and opioid dosage in MME for our commercial members in DE, PA, and WV. Over these years, three major shifts in behavior resulted, which align with the CDC and NIDA prescribing guidelines [1, 10-23]. First, between 2013 and 2017, there was a decrease of 19% of total opioid prescription fills. A 15% decrease was observed in 2017, up from 5% in 2016, and with wide variation by state. Our 2017 initiatives included additional pharmacy policy changes like quantity limits for safe prescribing and to prevent abuse, misuse and diversions. We do not know whether individuals shifted from prescribed drugs to illicit injectable drugs because it was outside the scope of this study. However, our three-pronged strategy did include provider, member, and community focused education. As expected, additional studies examining OUD treatment and health policy options for the prevention of any unintended public health consequences which may result from illicit drug use are needed.Second, between 2013 and 2017, there was a shift for opioid prescription patterns to shorter durations, from being 4 or more days to being 3 days or fewer. The majority of these members switched to 7 days or less of opioid use. In 2017, 84% of the members took 7 days or less, which compared to 57% at that level in BCBSA® data. Third, there was a shift for taking opioids at a much lower dosage. Results showed a reduction by 13 percentage points of the number of members on higher strength 20+ MMEs opioids.
Determining the pain management strategies used by members taking opioids at much lower levels and / or for a much shorter period of time was outside the scope of this study. However, our approach did include modifications of our opioid medical policies to reflect that alternative treatments are covered benefits for Highmark fully-insured members. Cognitive behavioral therapy through psychologists as adjunctive therapy for pain as well as a Complementary and Alternative Medicine network were also provided. Additional studies examining non-opioid prescribed therapy options and utilization of clinical and behavioral health services by age, sex, and regions are needed. In terms of OUD diagnosis, results showed that our members are getting diagnosed. However, additional studies are needed to determine whether these diagnosed patients received and / or completed treatment. Our findings did not rule out the possibility that other factors [1,33-35] like the increased prevalence of depression, environmental factors, epigenetics, and phenomena like "Death of Despair" [34-35], may also impact our results. If true, then we may yield more effective outcomes by refining our three-pronged strategy for particular populations.
6. LIMITATIONS
Our retrospective study had several limitations. First, our opioid results included only adult Highmark commercial members < 65 years of age in DE, PA, and WV and are not generalizable to all segments in society. Second, our data were reported by state-level only. Although we did follow the standard practice of state-level reporting used by others in the opioid space [1-3], other related reporting (e.g. by zip code or by race/ethnicity) was outside the scope of this study. Third, we did not examine the cause of pain or type of pain management therapy for which the member was issued the prescribed opioid. Thus, we cannot comment as to whether the member's pain could have been effectively managed without opioids and /or if the member received any complementary and alternative medicine options.
7. IMPLICATIONS FOR POLICY & PRACTICE
We enacted significant programs and policy changes designed to help members as they battle opioid abuse and addiction in our community-focused and partner-driven war on opioids. These were provider, member, and community focused interventions. Because no single entity can do this alone [1], we collaborated with local, state, and federal agencies; local school districts; businesses; law and drug enforcement; and community-and faith-based organizations.
Although our results showed improvements over a five-year period, it is unknown whether these results can be sustained in 2018 and beyond. Since our results were sustained in three of the top six states with the highest rates of opioid-related overdose death, we predict that these results could be sustained over time to some degree. Opioid prescribing is declining; diagnosis has increased, providing opportunity for evidence-based treatment. However, nationally, the opioid death rate has yet to peak [36-41]. We believe that continued comprehensive efforts, expansion of treatment access to MAT [42-43], risk reduction through availability of rescue medication [44-55], strategies around non-fatal overdose protocols and leveraging technologies such as telemedicine [46-47] will bend this curve.
CONCLUSION
The burden of opioid addiction and mortality in America is substantial and increasing, including in DE, PA, and WV. Utilizing a three-pronged strategy, coordinated approaches and CBPR frameworks, our study demonstrated improvements in total Opioid RX fills, opioid use by dose (MME), opioid use by duration, and number of members diagnosed with OUD. This innovative approach could also help alleviate the opioid epidemic by changing industry practices and building public awareness. No one organization alone can reverse this opioid epidemic. Other health systems, insurance plans, and policy makers in the opioid space should consider using these approaches when setting priorities, allocating their limited resources, designing programs to prevent OUD, improving access and options for proper management, and getting individuals into treatment.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This retrospective study was approved by the Allegheny Singer Research Institute – WPAHS Institutional Review Board, USA with Approval Number: ASRI WPAHS IRB # 000015120.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the Data Analytics Repository Dashboard at Highmark Inc.
FUNDING
This work was supported by Highmark Inc.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the support of the countless Highmark Health employees who provide day-to-day support for the deployment of the efforts to eradicate opioid overuse described in this article.


