All published articles of this journal are available on ScienceDirect.
Socio-Demographic and Clinical Correlates of Depressive Symptoms Prevalence and Severity Among People Living with Human Immunodeficiency Virus in Ethiopia: A Cross-Sectional Study
Abstract
Background:
Mental illness is the leading cause of disability all over the world greatly impacting several vulnerable groups particularly people living with the Human Immunodeficiency Virus (HIV). Depression is the most common mental illness especially in people with human immunodeficiency virus and its prevalence is increasing rapidly in the world at an alarming rate among this group population.
Objectives:
The main aim of this study was to investigate the prevalence and severity of depressive symptoms and related factors among patients living with the Human Immunodeficiency Virus
Methods:
An institutional-based cross-sectional study design was conducted among 398 Human Immunodeficiency Virus patients. Patient Health Questionnaire (PHQ-9) and Logistic regression analysis were used to determine predictors of depressive symptoms.
Results:
A total of 398 patients with the diagnosis of HIV were enrolled in the present study, whereby the majority were females (275, 69.9%). Prevalence of depressive symptoms among HIV-positive patients was 43.5% (95% CI: 38.2, 48.7). In multivariate analysis, poor sleep quality (AOR: 5.72, 95% CI: 3.52,9.27), Poor social support (AOR: 1.95, 95% CI: 1.15,3.29), lack of education status (AOR: 4.10, 95% CI: 1.92,8.76) elementary school (AOR: 2.46,95% CI: 1.26,4.79) and high school educational status (AOR: 2.11,95% CI: 1.01,4.42) were positively associated with depressive symptoms in people living with the Human Immunodeficiency Virus.
Conclusion:
The prevalence of depression symptoms was found to be significantly high in patients living with HIV. Patient’s poor sleep quality, poor social support and lower educational status were found to be dependent predictors of depressive symptoms. Hence, it is important to conduct more interventions to assess the depressive symptoms among HIV patients.
1. INTRODUCTION
Depression is a common mental disorder that is presented with depressed mood, loss of interest (pleasure), decreased energy, feeling of guilt, low self-worth, disturbed sleep or appetite or poor concentration. Depression is different from usual mood fluctuations and short-lived emotional responses to changes in everyday life. It can cause the affected person to suffer greatly and function poorly at work, school, and in the family. At its worst, depression can lead to suicide. Depression is the most common and disabling mental illness globally [1].
Depression is the fourth leading cause of disability worldwide as assessed by the World Health Organization and will be the first by 2030. The world mental health survey conducted in 17 countries found that on average, about 1 in 20 people reported having an episode of depression in the previous year [2, 3]. Furthermore, depression and HIV / AIDS are expected to be the only two causes of illness worldwide by the year 2030 [4].
Depression is one of the foremost disabling factors in chronic illnesses. Additionally, it is a common psychiatric co-morbidity worldwide, affecting HIV-infected patients, with estimates of lifetime prevalence rates - ranging from 4% to 45% [5]. This causes more impairment and more wellbeing losses than most other chronic diseases [6]. Depression has a negative impact on clinical outcomes in HIV-infected patients by decreasing adherence to medication, quality of life, the outcome of care, worsening disease progression and thus increasing morbidity and mortality [7].
The prevalence of depression in HIV-infected patients in southern Brazil accounts for 53.5% [8], in china 40.9% [9] and in India 67% [5].Other studies conducted in different countries on the prevalence of depression among HIV patients showed to be in Cameron 26.7% [10], in Malawi18.9% [11].
In Ethiopia, the prevalence of depression among people living with HIV varies from 14.6%-43 [6, 3, 12-15]. Previous studies have shown that factors such as unemployment, age, CD4 count, sex, educational status, drug side effects, family/social support, stigma, stage of HIV, living companion, marital status, monthly income and opportunistic infection are predisposing factors leading HIV/AIDS patients to depression [12].
Although the prevalence of depression among HIV / AIDS patients is high, few studies have been carried out in Ethiopia with no research carried out at the Jimma University Medical Center. This study was carried out to fill this research gap that could provide evidence for the successful prevention and treatment of depression in people living with HIV / AIDS in the future. Hence; this research was intended to investigate socio-demographic and clinical correlates of depressive symptoms prevalence and severity among people living with human immunodeficiency virus in West Ethiopia. In addition, this research highlighted the prominent role of sleep quality in the impact of depressive symptoms on people living with HIV when compared with previous literature.
2. MATERIALS AND METHODS
2.1. Study Design and Sample Size Determination
Cross-sectional institutional-based study was performed at the antiretroviral therapy follow-up clinic of Jimma University Medical Center (JUMC among People Living With Human Immunodeficiency Virus (PLWHIV) from June to October 2018. Patients who participated in this study were aged 18 years or older and receiving ART. Nevertheless, those who were seriously ill and were unable to speak during the data collection time because of their illness were excluded.
Patients who met the criteria were told about the study by their physicians and their consent to participate was obtained. Trained investigators performed the survey using consecutive convenience sampling to achieve the target sample size. All participants have been told of the voluntary and confidential existence of the research. Interviews were conducted after the participants had given written informed consent. In this study, the database used contain identification numbers to protect participants' privacy. The study was approved by the Jimma University medical center's ethical review board.
The sample size was determined using a single population proportion formula. Taking 43.9% prevalence of depression from previous study [14], 95% confidence interval (Z = 1.96) and 5% margin of error (d = 0.05), the initial sample size was 379. By considering a 5% non-response rate, the final sample size was determined to be 398. A total of 398 questionnaires were distributed and all questionnaires were returned, indicating a response rate of 100%.
2.2. Instruments
Data were collected using interviewer-administered structured questionnaire. The socio-demographic questions included information on age, sex, educational status, marital status, employment status, religion, ethnic group, and Socio-Economic Status (SES) as monthly income for individuals based on Ethiopian currency.
Depressive symptoms were assessed using the PHQ-9 questionnaire: For each of the 9 questions in the questionnaire, there were four possible options and the patients were required to choose 1 for each question. The scores awarded for each of the four options were as follows: ‘not at all’-0; ‘several days’-1; ‘more than half of the days’- 2; ‘nearly every day’ -3. The scores from all nine answers were added or computed a variable to obtain a final total which was graded or recoded into different variables to determine absence or presence of depressive symptoms and the severity as follows: 0-4 =minimal or none; 5-9=mild; 10-14=moderate; 15- 19=moderately to severe; 20-27=severe. Overall, participants with total scores of 0 – 4 were considered not to have depression while participants with scores of ≥ 5 – 27 were considered to have depressive symptoms having 9 items specificity (67%) and sensitivity (86%), which was validated in Ethiopia with Amharic and Afan Oromo version with cronbachs alpha of 0.85 [16].In the present study, the reliability alpha was 0.771.
Sleep quality reporting was assessed using Pittsburg Sleep Quality Index (PSQI). This scale measures subjective aspects of sleep quality. It is a 19-item self-report combined from seven component scores, each of which has a range of 0-3points. In all cases, a score “0” indicates difficulty, while a score of “3” indicates severe difficulty. The seven component scores are then added to yield one “global” score. Global scores greater than five are indicative of clinical levels of poor sleep quality.
The Pittsburgh Sleep Quality Index (PSQI) has been validated in the Ethiopian adult population for the measurement of quality and pattern of sleep in adults. PSQI has 82% sensitivity and 56.2% specificity. Each component receives a score from zero to three, with the final score on the instrument ranging between 0 and 21. The higher the score, the worse the quality of sleep, and scores > 5 indicate poor sleep quality [17].To assess the level of social support for the patient, Oslo Social Support Scale was used which has three items [18].
For clinical factors, patients’ chart review was used that includes the WHO stage of HIV status classification, CD4 count (the most recent), viral load (the most recent), current medication regimen, duration of HIV/AIDS diagnosed and duration of anti-retroviral therapy medication.
2.3. Operational Definition
Depressive symptoms: measured by using PHQ-9. Participants who scored a sum total of 5 and above on the PHQ-9 scale were considered having depressive symptoms.
Severity of depressive symptoms: a score of 1 to 4 referred to ‘no depression’, 5 to 9 ‘mild depression’, 10 to 14 ‘moderate depression’, 15 to 19 ‘moderately severe depression’, and 20 to 27 indicated ‘severe depression’.
2.4. Statistical Analysis
Data was checked on completion; data was edited, cleaned and coded then entered into Epidata 3.1softwer and exported to Statistical package for social science (SPSS) version 20 for analysis. Bivariate analysis was used to identify factors associated with depressive symptoms among people living with HIV/AIDS. Variables with p-value <0.25 in bivariate analysis were considered as candidates for multiple logistic regressions. Multiple logistic regressions were performed using backward Logistic Regression method to identify factors independently associated with dependent variables. P-value <0.05 was considered statistically significant. Predictors of depressive symptoms among people living with HIV/AIDS were found to be at 95% confidence intervals.
3. RESULTS
3.1. Participants’ Characteristics
Participants’ general characteristics are shown in (Table 1). Of the total sample (N = 398), 69.9% were females. In terms of educational status, the majority of participants 76(19.1%) lacked education status. In addition, the result showed that more than half were 206 (51.8%) married. More than half of the participants had taken 1e (Tenofovir+Lamivudine+ Efavirenz); highly active antiretroviral therapy (HAART) component. The result showed that the duration of diagnosis ranged from 1 to 3 years with a mean of 1.90 (SD=0.758) and the duration of taken medication ranged from 1 to 3 years with a mean of 1.90 (SD=0.789).
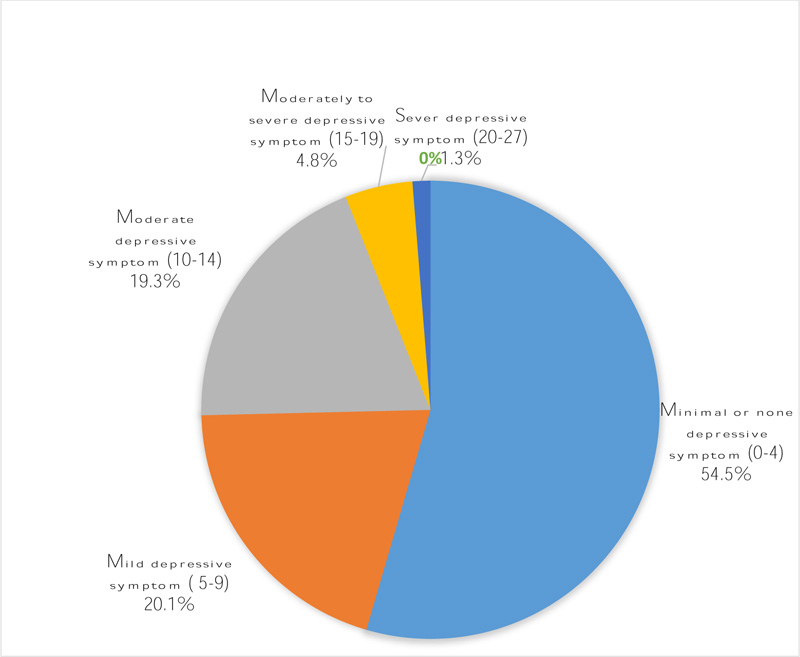
Table 1.
| Variables | Total N =398(%) |
Depressive symptoms | COR | p-value | ||
| Yes n=173(43.5%) |
No n=225(56.5%) |
|||||
| Gender | Male | 123(30.1%) | 28.3% | 32.9% | Reference | - |
| - | Female | 275(69.9%) | 71.7% | 67.1% | 1.24(0.81,1.91) | 0.329 |
| Respondents’ age | <=30 | 128(32.2%) | 32.9% | 31.6% | 1.31(0.74,2.33) | 0.354 |
| - | 30-35 | 75(18.8%) | 17.3% | 20.0% | 1.09(0.57,2.08) | 797 |
| - | 35-45 | 116(29.1%) | 32.4% | 26.7% | 1.52(.85,2.73) | 0.56 |
| - | >45 | 79(19.8%) | 17.3% | 21.8% | Reference | - |
| Educational status | lack of education | 76(19.1%) | 26.0% | 13.8% | 4.89(2.46,9.72)* | .000 |
| Elementary | 146(36.7%) | 38.7% | 35.1% | 2.86(1.56,5.24)* | 0.001 | |
| High school | 93(23.4) | 24.3% | 22.7% | 2.77(1.44,5.34)* | 0.002 | |
| Diploma and above | 83(20.9%) | 11.0% | 28.4% | Reference | - | |
| Marital status | Single | 48(12.1%) | 9.8% | 13.8% | Reference | - |
| Married | 206(51.8) | 50.9% | 52.4% | 1.36(0.71,2.61) | .356 | |
| Divorced | 79(19.8%) | 23.1% | 17.3% | 1.87(0.89,3.91) | 0.96 | |
| Widowed | 65(16.3%) | 16.2% | 16.4% | 1.38(0.64,2.98) | 0.412 | |
| Occupational status | Governmental employee | 67(16.8%) | 10.4% | 21.8% | Reference | - |
| Private employee | 84(21.1%) | 20.8% | 21.3% | 2.04(1.02,4.08)* | 0.043 | |
| Merchant | 47(11.8%) | 12.7% | 11.1% | 2.31(1.09,5.27)* | 0.003 | |
| Farmer | 7(1.8%) | 2.3%1. | 3% | 3.63(0.74,17.82) | .112 | |
| House wife | 60(15.1%) | 13.9% | 16.0% | 1.82(0.86,3.83) | .118 | |
| Daily laborers | 33(8.3%) | 9.8% | 7.1% | 2.89(1.21,6.91)* | 0.017 | |
| No job(Unemployed) | 67(8.3%) | 21.4% | 13.3% | 3.36(1.63,6.92)* | 0.001 | |
| Other | 33(8.3%) | 8.7% | 8.0% | 2.27(0.95,5.43) | 0.066 | |
| Highly active antiretroviral therapy (HAART) regimen | 1c(Zidovudine+Lamivudine+Nevirapene) | 88(22.1%) | 27.7% | 17.8% | Reference | - |
| 1d(Zidovudine+Lamivudine+Efavirenz) | 41(10.3%) | 9.2% | 11.1% | 0.53(.25,1.14) | 0.103 | |
| 1e(Tenofovir+Lamivudine+Efavirenz) | 221(55.5%) | 54.9% | 56.0% | 0.63(0.38,1.03) | 0.067 | |
| 1f(Tenofovir+Lamivudine+Nevirapene) | 37(9.3%) | 5.8% | 12.0% | 0.31(0.13,.71)* | 0.006 | |
| other | 11(2.8%) | 2.3% | 3.1% | 0.48(0.13,1.74) | 0.263 | |
| Monthly income | <200 | 134(33.7%) | 40.5% | 28.4% | 1.86(1.13,3.08)* | 0.015 |
| 200-1000 | 145(36.4%) | 34.1% | 38.2% | 1.17(0.71,1.93) | 0.538 | |
| >1000 | 119(29.9%) | 25.4% | 33.3% | Reference | - | |
| Time since HIV diagnosis | <6 | 136(34.2%) | 39.3% | 30.2% | Reference | - |
| 6-10 | 166(41.7%) | 40.5% | 42.7% | 0.73(.46,1.15) | 0.175 | |
| >10 | 96(24.1%) | 20.2% | 27.1% | 0.574(0.34,.98)* | 0.042 | |
| Duration of ART medication | <5 | 145(36.4%) | 34.7% | 37.8% | Reference | - |
| 5-9 | 147(36.9%) | 42.2% | 32.9% | 1.31(0.88,2.22) | .156 | |
| >9 | 106(26.6%) | 23.1% | 29.3% | 0.86(0.51,1.43) | .560 | |
| Current (most recent) CD4+ cell count, cells/mm3 | <200 | 101(25.4%) | 30.1% | 21.8% | 1.49(0.89,2.41) | .131 |
| - | 200-350 | 84(21.1%) | 19.7% | 22.2% | 0.95(0.55,1.66) | .868 |
| - | 351-500 | 76(19.1%) | 17.3% | 20.4% | 0.92(0.52,1.62) | .762 |
| - | >500 | 137(34.4%) | 32.9% | 35.6% | Reference | - |
| social support | poor social support | 142(35.7%) | 45.1% | 28.4% | 2.23(1.41,3.59)* | 0.001 |
| - | moderate social support | 89(22.4%) | 20.8% | 23.6% | 1.24(0.73,2.11) | .420 |
| - | strong social support | 167(42%) | 34.1% | 48.0% | Reference | - |
| Current (most recent) Viral load | <50copies(Undetectable) | 257(64.6%) | 60.6% | 72.7% | Reference | - |
| - | >50copies (detected) | 124(31.2%) | 39.4% | 27.3% | 1.73(1.12,2.67)* | 0.013 |
| Sleep quality | Good sleep quality | 168(42.2%) | 20.2% | 59.1% | Reference | - |
| - | Poor sleep quality | 230(57.8%) | 79.8% | 40.9% | 5.70(3.61,8.91)* | .000 |
3.2. Depressive Symptoms and Clinical Related Characteristics
From the total study participants, 173(43.5%) had depression symptoms (95% CI: 38.2, 48.7) with females (71.1%) being more prevalent than males (28.3%). And also the symptoms were more prevalent (54.9%) among respondents taking 1e medication regimen and in participants who had a poor sleep quality (79.8%). The prevalence of depressive symptoms in poor social support was 45.1%. Through the univariate analysis, we found that depressive symptoms were correlated with education level, occupational status, HHART variable, monthly income, disease length, social support, viral load and sleep quality (p < 0.25) (Table 1).
3.3. Description of Depressive Symptoms Among HIV/AIDS Patients
In this study, the prevalence of depressive symptoms was found to be (43.5%) with (95% CI: 38.2, 48.7). Fifty-four percent (54.5%) of patients had no depressive symptoms. Based on severity scale, 20.1% had mild depressive symptoms, 19.3% had moderate depressive symptoms and 4.8% had moderately severe depressive symptoms (Fig. 1).
3.4. Depressive symptoms and sleep problems
We found that the majority 55.5% of those with depressive symptoms reported fairly good subjective sleep quality, (49.7%) were unable to fall asleep within 60 minutes and (40.5%) had very poor habitual sleep performance (Table 2).
| Variables | Depressive symptoms | P –value | |
| Yes n=173(43.5%) |
No n=225(56.5%) |
||
| Subjective sleep quality (Component 1) | - | - | .0001 |
| Very good | 41(23.7%) | 129(57.3%) | - |
| fairly good | 96(55.5%) | 86(38.2%) | - |
| fairly bad | 19(11.0%) | 8(3.6%) | - |
| very bad | 17(9.8%) | 2(0.9%) | - |
| Sleep latency (Component 2) | - | - | .0001 |
| 0(<15 minutes) | 33(19.1%) | 120(53.3%) | - |
| 1(16-30minutes) | 9(5.2%) | 21(9.3%) | - |
| 2(31-60 minutes) | 45(26.0%) | 43(19.1%) | - |
| 3(>60minuntes) | 86(49.7%) | 41(18.2%) | - |
| sleep duration (Component 3) | - | - | .0001 |
| >7 hours | 38(22.0%) | 72(32.0%) | - |
| 6-7hours | 25(14.5%) | 69(30.7%) | - |
| 5-6 hours | 61(35.3%) | 61(27.1%) | - |
| <5 hours | 49(28.3%) | 23(10.2%) | - |
| Habitual sleep efficiency (Component 4) | - | - | 0.0001 |
| >85% (very good) | 43(24.9%) | 97(43.1%) | - |
| 75%-84% (fairly good ) | 31(17.9%) | 57(25.3%) | - |
| 65%-74% (fairly bad) | 29(16.8%) | 40(17.8%) | - |
| <65 % (very bad) | 70(40.5%) | 31(13.8%) | - |
| Sleep disturbances (Component 5) | - | - | 0.0001 |
| 0 (very good) | 36(20.8%) | 132(58.7%) | - |
| 1-9( fairly good) | 67(38.7%) | 46(20.4%) | - |
| 10-18 (fairly bad) | 51(29.5%) | 29(12.9%) | - |
| 19-27( very bad) | 19(11.0%) | 18(8.0%) | - |
| use of sleep medicine (Component 6) | - | - | .459 |
| not at all | 157(90.8%) | 211(93.8%) | - |
| less than once a week | 6(3.5%) | 4(1.8%) | - |
| once or twice a week | 10(5.8%) | 10(4.4%) | - |
| Daytime dysfunction (Component 7) | - | - | .0001 |
| 0(Very good) | 122(70.5%) | 198(88.0%) | - |
| 1(Fairly good) | 28(16.2%) | 14(6.2%) | - |
| 2(Fairly bad) | 22(12.7%) | 13(5.8%) | - |
| 3(Very bad) | 1(0.6%) | 0(0.0%) | - |
| Variable | β | Standard error | Wald | p-value | AOR (95%) confidence interval |
| Poor sleep quality | 1.743 | .247 | 49.895 | .000 | 5.72(3.52,9.27)** |
| Good sleep quality | - | - | - | - | Reference |
| Poor social support | .666 | .268 | 6.206 | .013 | 1.95(1.15,3.29)** |
| moderate social support | .260 | .309 | .708 | .400 | 1.297(0.71,2.37) |
| strong social support | - | - | - | - | Reference |
| Illiterate | 1.411 | .387 | 13.303 | .000 | 4.10(1.92,8.76)** |
| Elementary | .898 | .342 | 6.912 | .009 | 2.46(1.26,4.71)** |
| High school | .746 | .377 | 3.904 | .048 | 2.11(1.01,4.42)** |
| Diploma and above | - | - | - | - | Reference |
| Variables | Minor/no depression (PHQ-9)(0-4) |
Mild depression (PHQ-9= 5-9) | Moderate depression (PHQ-9 = 10-14) |
Moderate-severe depression (PHQ-9 = 15-19) |
Severe depression (PHQ-9 = 20-27) |
p-value |
| good sleep quality | 132(60.8%) | 23(28.8%) | 12(15.6%) | 1(5.3%) | 0(0.0%) | 0.0001 |
| Poor sleep quality | 85(39.2%) | 57(71.3%) | 65(84.4%) | 18(94.7%) | 5(100.0%) | |
| Poor social support | 58(26.7%) | 41(51.3%) | 30(39.0%) | 8(42.1%) | 5(100.0%) | 0.0001 |
| moderate social support | 52(24.0%) | 20(25.0%) | 11(14.3%) | 6(31.6%) | 0(0.0%) | |
| strong social support | 107(49.3%) | 19(23.8%) | 36(46.8%) | 5(26.3%) | 0(0.0%) | |
| Illiterate | 31(14.3%) | 20(25.0%) | 22(28.6%) | 3(15.8%) | 0(0.0%) | 0.004 |
| Elementary | 75(34.6%) | 32(40.0%) | 27(35.1%) | 8(42.1%) | 4(80.0%) | |
| High school | 48(22.1%) | 20(25.0%) | 20(26.0%) | 4(21.1%) | 1(20.0%) | |
| Diploma and above | 63(29.0%) | 8(10.0%) | 8(10.4%) | 4(21.1%) | 0(0.0%) |
3.5. Factors Associated with Depressive Symptoms
In multivariate logistic regression analysis, sleep quality was found as the most important influencing factor of depressive symptoms among HIV-patients. Respondents with poor sleep quality were 5.72 times more likely to suffer from depressive symptoms (AOR=5.72, 95% CI = 3.52, 9.27). Patients with poor social support were 1.95 times more likely to suffer from depressive symptoms (AOR=1.95, 95% CI = (1.15, 3.29). Educational status was found to be significantly associated with depression; being no education 4.10 times (AOR=4.10,95% CI=1.92, 8.76), having Elementary educational status 2.46 times (AOR=2.46, 95% CI=1.26, 4.71) and having High school level of education 2.11 times (AOR=2.11,95% CI=1.01,4.42) more likely to develop depressive symptoms than participants who had a diploma and above (Table 3).
3.6. Effect of Predictor Variables on Prevalence and Severity of Depression Symptoms
Prevalence of participants with a PHQ-9 score indicative of major depressive symptoms was significantly higher among participants who reported poor sleep quality, poor social support and illiterate educational status compared with participants who had good sleep quality, strong social support and high level of educational status as shown in (Table 4).
4. DISCUSSION
The depressive symptoms reported in our study found a high prevalence of 43.5% as an overall finding which is consistent with findings from previous studies conducted in Ethiopia [6, 12, 14] and elsewhere [9]. Our prevalence estimates are however lower than estimates reported from Southern Brazil (53.5%) among 249 participants living with HIV [8] and India (67%) among 104 participants living with HIV [5]. The reported prevalence in our study is nearly two times higher than the estimates reported within [13, 15] and outside Ethiopia [10, 11]. The reason for this discrepancy in findings may be attributed to several factors, including the population being studied, the study periods, the differences in measures, cut point of tools and the sample size used. For instance, we used the PHQ-9 scale with a cut point greater than or equal to five whereas in southern Brazil, the Beck Depression Inventory (BDI) was used; in Tigray Ethiopia, Hamilton Depression Rating Scale (HAM-D) with a cut point greater than 17 was used and in India, the General Health Questionnaire (GHQ) and Montgomery-Asberg Depression Rating Scale (MADRS) were used.
In our sample, 79.8% of participants with depressive symptoms reported poor quality of sleep, and 40.9% of participants with non-depressive symptoms reported poor quality of sleep. Multivariate logistic regression has shown that sleep quality was the strongest risk factor associated with depressive symptoms among HIV-patients. This finding was in line with other studies [9].
The risk of depressive symptoms was nearly 2-folds among participants reporting poor social support relative to those reporting strong social support. People living with HIV who do not have a close family to report their problem cannot get treatment and may have increased depressive symptoms [12, 19]. This may also be attributed to reduced social support in the sense of HIV; due to various factors such as educational failure, food insecurity, loneliness and weakening, AIDS is associated with increased depressive symptoms.
In our study, respondents who had no education or who had finished primary school alone had increased chances of depressive symptoms relative to respondents with more AOR=(4.10, 95% CI:(1.92,8.76). This study is in line with the Malawi study [11]. The possible explanation for this could be the fact that individuals with low socioeconomic and educational status have given less value to their self-esteem and led a stressful life as compared to more educated people.
In our study, there was no association of depressive symptoms with respondents’ age, gender, marital status, income, HAART regimen, duration of illness from HIV/AIDS, viral load and the CD4 count. This aspect of the study is in line with the study conducted in India [5].
CONCLUSION
This study provided information regarding the magnitude of depressive symptoms which were found to be high in people living with Human Immunodeficiency Virus and poor sleep quality, poor social support and lower educational status might be the factors contributing to the depression symptoms among people living with HIV/AIDS.
We recommend active steps to increase awareness about depression among clinicians and patients, with the help of psychiatrists or psychologists as counselors, to identify early and help depressed patients. Active, early intervention can help prevent the worsening of depression and its impact on life.
LIST OF ABBREVIATIONS
| 3TC | = Lamivudine; |
| ABC | = Abacavir; |
| AIDS | = Acquired Immunodeficiency Syndrome; |
| OR | = Adjusted Odds Ratio; |
| ART | = Antiretroviral Therapy; |
| AZT | = Zidovudine; |
| CD4 | = Cluster of Differentiation (cells) ; |
| CNS | = Central Nervous System; |
| EFV | = Efavirenz; |
| HIV | = Human Immunodeficiency Virus; |
| JUMC | = Jimma University Medical Center; |
| LPV/r | = Lopinavir with ritonavir booster; |
| NVP | = Nevirapene; |
| PHQ9 | = Patient Health Questionnaire ; |
| PLWHIV | = Persons living with Human Immunodeficiency Virus ; |
| PSQI | = Pittsburgh Sleep Quality Index ; |
| REC | = Research Ethics Committee ; |
| SPSS | = Statistical Package for Social Sciences; |
| TDF | = Tenofovir |
AUTHORS’ CONTRIBUTIONS
WM designed the study, collected and analyzed the data, and reviewed the manuscript. DZ and MT; designed the study, supervised data collection, analyzed the data, drafted the manuscript and critically reviewed the manuscript. All authors read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research was approved by the Institutional Review Board at Jimma University, Ethiopia (Ref. No.: JHRTGD /334/2018), before data collection.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Interviews were conducted after the participants had given written informed consent.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and analyzed during the current study are available from the corresponding author,[W. M. M], on reasonable request.
FUNDING
Financial funding was provided by the Jimma University with grant number 6223.
CONFLICTS OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We would like to thank Jimma University Medical Center, ART Clinic officials for facilitating the data collection process and Nurses working in ART clinics for their co-operation during data collection.


