All published articles of this journal are available on ScienceDirect.
Effectiveness of Deep Breathing and Body Scan Meditation Combined with Music to Improve Sleep Quality and Quality of Life in Older Adults
Abstract
Background:
In older adults, physiological changes affect sleep and may cause impaired daily function and Reduced Quality of Life (QOL). This study aimed to investigate the effectiveness of deep breathing exercises and body scan meditation combined with music to improve sleep quality and QOL.
Methods:
A randomized controlled trial with allocation concealment method was conducted. Fifty-nine older adults with poor sleep quality were recruited using block randomization to intervention and control groups. The intervention group was instructed to do deep breathing and body scan meditation while listening to music through Bluetooth speakers once a day for thirty minutes before sleeping, a daily practice to last for eight weeks. The Pittsburgh Sleep Quality Index (PSQI) and Pictorial Thai Quality of Life (PTQL) were administered to both groups prior to the intervention and 8-week post-baseline of the intervention.
Results:
The global PSQI in the intervention group significantly decreased following the intervention, whereas the control group showed no difference. There was a decrease in individual PSQI components as well for the intervention group, namely, sleep efficiency, perceived sleep quality, and daily disturbance. The intervention group did not differ from the control group in sleep efficiency or perceived sleep quality, but there was a significant difference in the daily disturbance. Additionally, the total PTQL in the intervention group significantly increased between the two time periods, whereas there was no difference in the controls. The intervention group scored higher in each domain of PTQL, except for the economic domain.
Conclusion:
A daily practice of deep breathing and body scan meditation combined with music has a positive effect on improving sleep quality and QOL among older adults. Hence, this intervention should be implemented to improve sleep quality and promote QOL in older adults.
1. INTRODUCTION
A United Nations report indicates that in 2019, there were 703 million persons aged 65 years or over globally. The number of older persons is projected to double to 1.5 billion in 2050 [1]. One study showed that age-related changes lead to light sleep and a decrease in sleep efficiency [2]. Most of the sleep problems in the elderly include difficulty falling asleep, waking up during the night, waking too early, and daytime drowsiness [3].
Data from epidemiological surveys show that the prevalence of poor sleep quality varies by country. In China, some studies reported a prevalence of 49%- 50% among older adults, while South Korea reported about 60% of older adults aged 65 years and above [4-6] suffered from poor sleep quality. In Thailand, the prevalence of poor sleep quality in older adults is 57.1% [7]. Sleep quality is an important component of good health and sleep disorders adversely affect the physical and mental constructs of older adults [8]. Sleep disorders decrease performance while increasing cognitive and memory dysfunction [9]. Long-term effects may cause diseases such as obesity, diabetes, and heart disease [10]. Additionally, sleep quality has a direct impact on many other health outcomes and the Quality of Life (QOL) in older adults [11].
The National Institutes of Health (NIH) and the National Institute of Mental Health advised that the treatment of sleep disorders should start with non-pharmacological management [12]. As a result, there has been increased interest in Complementary and Alternative Medicine (CAM), given its potential to control the body's systems. Mind-body medicine, a sub-group of CAM, has various techniques for strengthening the mind and the body, such as meditation and relaxation techniques [13-15]. These techniques are amongst the most cost-effective, safe and easy to perform and have been shown to enhance psychological well-being as well as improve sleep quality, depressive symptoms, and quality of life [16-18]. To our knowledge, few studies have evaluated the effects of deep breathing exercise, body scan meditation and music relaxation on sleep quality in older adults who are more vulnerable to poor sleep. This study aimed to evaluate the effectiveness of deep breathing exercises and body scan meditation combined with music (DBM) on the quality of sleep and QOL in older adults with poor sleep quality.
2. MATERIALS AND METHODS
2.1. Study Design
An 8-week randomized controlled trial with allocation concealment method was conducted with a parallel-group design. Neither the researcher who collected the data before and after the intervention nor the participants, had known of allocations into DBM and control groups. DBM and control groups were trained and collected data at different times and places. After the baseline examination, participants were randomized using block randomization to two groups, (a) the DBM group, receiving deep breathing exercise and body scan meditation combined with music (b) the control group only receiving routine care. The study was performed between November 2017 to January 2018. The trial was registered in the Thai Clinical Trials Registry (ID: TCTR 20170405001).
2.2. Participants
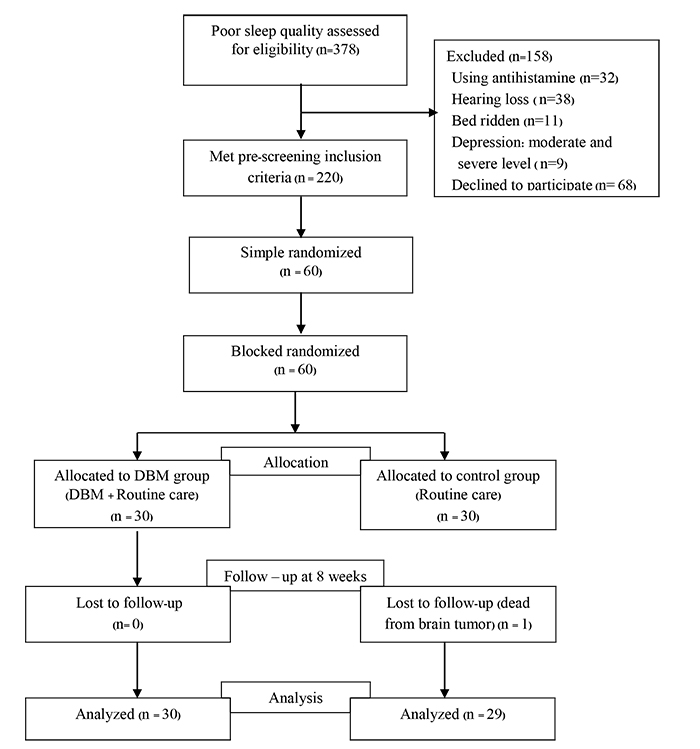
A total of 378 older adults from a primary healthcare center in Chiang Mai Province, Thailand, who were 60 years of age with poor sleep quality, were screened for the study using the Pittsburgh Sleep Quality Index (PSQI) sleep quality assessment. A total of 220 participants met the inclusion criteria and consented to participate in the present study (Fig. 1). The inclusion criteria were: the ability to walk independently, scoring 6 to 14 on the PSQI, and being willing to participate in the study. The exclusion criteria included severe head injuries, a history of mental health problems, depression, taking anti-depressive drugs and antihistamines with steroids, and have hearing loss.
Of this group, 60 participants were randomly selected and assigned to DBM (n=30) and control (n=30) groups using block randomization with 2 randomly selected block sizes and an allocation ratio of 1:1. The sample size was calculated based on a previous study [19] with a power of 80% and alpha of 5% using n4 Studies program for a randomized controlled trial with a continuous outcome [20]. The sample size was estimated to be 58 people at a coefficient interval of 95%. Dropouts were anticipated, so to ensure an adequate final sample size, 30 participants were selected per group. A total of 59 participants (mean age = 70.27±7.65; 14 men and 45 women) completed the study including 30 in the DBM group (mean age = 70.43±7.06; 8 men and 22 women) and 29 in the control group (mean age = 70.10±8.33; 6 men and 23 women) at week 8. One participant from the control group died from an undiagnosed brain tumor two weeks after the start of the intervention (Fig. 1).
2.3. Intervention
The DBM or intervention group learned how to do deep breathing exercises and body scan meditation while listening to music. The participants attended weekly 30-minute classes at a center-based facility for the first month to learn the deep breathing exercises and body scan meditation from an instructor. Each participant was given a Bluetooth speaker, which had a preprogrammed MP3 file with music and a guided body scan meditation. They were instructed to use the Bluetooth speaker to aid them in practicing body scan meditation combined with deep breathing for 30 minutes before sleep on a daily basis. This was done for a total duration of 8 weeks. They were also instructed to fill out “performance record forms” which were collected at the end of the intervention. The contact numbers of the researcher (first author) were given to the participants in the event that they had questions about their daily practice.
Specifically, participants were asked to: (1) Lie down in a comfortable position and close their eyes and (2) Listen to the guided body scan meditation and music while engaging in deep breathing. During guided meditation, they were instructed to relax all their muscles, beginning from the soles of their feet moving up to the top of their heads. As they were relaxing their muscles, they breathed through their noses, paying attention to the sound of their breathing, and saying the word “one” quietly to themselves as they exhaled; for example, breath in-out, ‘one’; in-out, ‘one... They were to continue this pattern for 30 minutes.
To assess their compliance, participants were asked to fill out a daily performance record immediately after waking. The trainer made follow-up visits every week for the first month and provided any needed assistance regarding the daily practice. During the second month, participants were visited every fortnight. After 8 weeks, their “performance recording forms” were collected.
The control group received routine care and did not receive any intervention. They attended a once a week training on sleep hygiene for 4 weeks. During the second month, they received guidelines for sleep hygiene and met twice to share their experiences.
2.4. Data Collection
Data were collected at baseline and after the 8th week of the intervention by a research assistant who was blinded to the group to which each participant had been assigned. Outcome measurements were taken at these times. The primary outcome of sleep quality was assessed using the PSQI, while the secondary outcome of QOL was assessed using the Pictorial Thai Quality of life (PTQL). Participants also completed a questionnaire on demographic information, which included age, gender, level of education, marital status, body mass index (BMI), medical history, smoking, and alcohol drinking habits.
2.4.1. Primary outcomes
Sleep quality was accessed using the PSQI [21], which measured the quality and patterns of sleep in older adults by self-report. The PSQI has seven components, including sleep latency, sleep duration, subjective sleep quality, sleep efficiency, sleep disturbance, daytime dysfunction, and use of medication for sleep. Scoring was based on a scale of 0 to 3, with 3 reflecting the most negative option. The total score was the sum of the seven components and ranged from 0 to 21. A total PSQI score of ≥5 indicated poor sleep quality, whereas <5 reflected good sleep quality.
Statistical analyses focused on three factors, sleep efficiency (using sleep duration and sleep efficiency variables), perceived sleep quality (using subjective sleep quality, sleep latency, and sleep medication variables), and daily disturbances (using sleep disturbances and daytime dysfunctions variables) [22, 23]. The Cronbach's alpha and test-retest reliability for the total PSQI score were 0.83 and 0.85, respectively. A sensitivity of 89.6% and a specificity of 86.5% have been denoted for the intervention versus control participants at a cutoff point of 5 on the PSQI [21].
2.4.2. Secondary outcome
The QOL was assessed using a version of the PTQL specific for Thai older adults and assessed six domains of quality of life: physical, cognitive, affective, social function, economic and self- esteem. Each item was scored on a scale of 0-3, with 0 indicating “no problem” and 3 indicating “have a severe problem”. The total score was calculated by summing the six domains and ranged from 0 to 72. A total PTQL score of 0 to 17 indicated poor QOL, 18 to 48 moderate QOL, whereas the good quality of life was reflected by a total PTQL score of 49 to 72. The reliability coefficients for the alpha coefficients of the PTQL total test was 0.88, and the value of six scales, Cronbach's alpha ranged from 0.81 to 0.93, respectively [24].
2.5. Statistical Analysis
All data were analyzed using parametric and non-parametric tests because the data had both normal and subnormal distributions. Chi-square tests and independent t-test were conducted to compare the homogeneity of the demographic characteristics and all baseline outcomes between the intervention and control groups. The Wilcoxon signed ranks test and Mann Whitney test were used to compare the mean differences or median percentile (25-75) within each group. p<0.05 indicated statistical significance.
3. RESULTS
3.1. Participant Characteristics
Demographic data and baseline characteristics of the participants are presented in Table 1. There was no statistically significant difference found between the two groups regarding age, sex, marital status, educational level, medical history, BMI, smoking, and alcohol usage.
3.2. Comparison of the PSQI between DBM and Control Groups
The DBM and control groups had similar problems regarding sleep at baseline. Both groups experienced waking up at night and an inability to go back to sleep, body pains, snoring and feeling suffocated. They noted that they suffered from sleep problems for close to a month or more. Participants tried to manage sleep problems with medicine, praying, and not napping during the day. About 10% of the older adults in the DBM group and 6.8% in the control group used sleeping pills to address sleep problems (data not shown).
The baseline global PSQI and PSQI component scores between the DBM and control groups were not significantly different. After the intervention, the global PSQI median scores in the DBM group significantly decreased (p = 0.001), whereas the scores in the control group did not change. The median scores for sleep efficiency, perceived sleep quality and daily disturbance after the intervention significantly decreased in the DBM group (p = 0.001, 0.001 and 0.003, respectively), whereas there was no difference in scores for sleep efficiency and perceived sleep quality in the control group, but the daily disturbance score did have a significant difference (p = 0.032) (Table 2). This study found that 18 older adults (60.0%) in the DBM group experienced an improvement in five or more points of the PSQI and 16 older adults (40%) experienced improvement but less than five-point of the PSQI (data not shown).
| Characteristics |
DBM Group (n=30) |
Control Group (n=29) | p-value |
| Age (years)aMean±SD | 70.43±7.06 | 70.10±8.33 | 0.870 |
| Sex, n (%)b | |||
| Male | 8 (26.7) | 6 (20.7) | 0.590 |
| Female | 22 (73.3) | 23 (79.3) | |
| Marital status, (n %)b | |||
| Single | 2 (6.7) | 0 (0.0) | 0.084 |
| Married | 11 (36.7) | 18 (62.1) | |
| Widowed | 17 (56.7) | 11 (37.9) | |
| Education level n (%)b | |||
| Illiterate | 1 (3.3) | 0 (0.0) | 0.422 |
| Primary school | 25 (83.3) | 27 (93.1) | |
| High school | 4 (13.3) | 2 (6.9) | |
| Chronic disease, n (%)b | |||
| No | 7 (23.3) | 6 (20.7) | 0.501 |
| Yes | 23 (76.7) | 23 (79.3) | |
| Hypertension, n (%)(n=23) | 12 (52.2) | 12 (52.2) | |
| Diabetes, n (%)(n=23) | 2 (8.7) | 5 (21.7) | |
| Hypertension and Diabetes, n (%)(n=23) | 6 (26.1) | 6 (26.1) | |
| Gout, n (%)(n=23) | 2 (8.7) | 0 (0.0) | |
| BMI (kg/m2)a, Mean±SD | 24.97±2.75 | 25.14±5.20 | 0.874 |
| Smoking, n (%)b | |||
| No | 28 (93.3) | 27 (93.1) | |
| Yes | 2 (6.7) | 2 (6.9) | |
| Alcohol drinking, n (%)b | |||
| No | 23 (76.7) | 27 (93.1) | 0.075 |
| Yes | 7 (23.3) | 2 (6.9) |
| Outcomes | Pre-test | Post-test | p-value within group‡ | ||||
| Mean ± SD | Median | P25th-75th | Mean ± SD | Median | P25th-75th | ||
| Global PSQI | |||||||
| DBM(n=30) | 9.60±2.62 | 8 | 7-13 | 4.00±2.31 | 3 | 2-5.25 | 0.001** |
| Control (n=29) | 8.45±2.26 | 8 | 6.5-10 | 10.38±4.85 | 11 | 7-14 | 0.05 |
|
p-value between groups† |
0.105 | 0.001** | |||||
| PSQI components: Sleep efficiency | |||||||
| DBM(n=30) | 3.43±1.38 | 3 | 2-4.25 | 1.23±1.33 | 1 | 0-2 | 0.001** |
| Control (n=29) | 3.34±1.67 | 3 | 2-5 | 3.93±2.05 | 5 | 2-6 | 0.186 |
|
p-value between groups† |
0.817 | 0.001** | |||||
| PSQI components: Perceived sleep quality | |||||||
| DBM (n=30) | 3.80±1.60 | 4 | 2-5 | 1.17±1.26 | 1 | 0-2 | 0.001** |
| Control (n=29) | 3.10±1.39 | 3 | 2-4 | 3.52±2.16 | 3 | 2-6 | 0.425 |
|
p-value between groups† |
0.113 | 0.001** | |||||
| PSQI components: Daily disturbance | |||||||
| DBM(n=30) | 2.37±0.92 | 3 | 1.75-3 | 1.60±0.81 | 2 | 1-2 | 0.003* |
| Control (n=29) | 2.00±1.10 | 2 | 1-3 | 2.93±1.38 | 3 | 2-4 | 0.032* |
|
p-value between groups† |
0.132 | 0.001** | |||||
| Outcomes | Pre-test | Post-test |
p-value within group‡ |
||||||||||||
| Mean±SD | Median | P25th- 75th | Mean±SD | Median | P25th-P75th | ||||||||||
| Total PTQL | |||||||||||||||
| DBM (n=30) | 51.40±10.56 | 55 | 42-60 | 59.20±6.61 | 62 | 53.7-63.5 | 0.001** | ||||||||
| Control (n=29) | 35.60±9.35 | 35 | 28-42.5 | 35.53±9.33 | 34 | 28-42.5 | 0.79 | ||||||||
|
p-value between groups† |
0.001** | 0.001** | |||||||||||||
| PTQL Physical Domain | |||||||||||||||
| DBM(n=30) | 9.00±2.44 | 9 | 7-10.2 | 11.30±2.23 | 11 | 9-13 | 0.001** | ||||||||
| Control (n=29) | 6.14±2.93 | 7 | 4-8 | 6.41±2.95 | 6 | 5-8 | 0.124 | ||||||||
|
p-value between group† |
0.004* | 0.001** | |||||||||||||
| PTQL Cognitive Domain | |||||||||||||||
| DBM(n=30) | 5.03±2.29 | 5 | 3-7 | 6.57±1.52 | 7 | 5-7 | 0.001** | ||||||||
| Control (n=29) | 3.28±1.68 | 3 | 2-3 | 3.31±1.77 | 3 | 2-3 | 0.317 | ||||||||
|
p-value between groups† |
0.001** | 0.001** | |||||||||||||
| PTQL AffectiveDomain | |||||||||||||||
| DBM(n=30) | 12.3±2.84 | 13 | 11-15 | 13.00±2.11 | 13 | 11-15 | 0.80 | ||||||||
| Control (n=29) | 6.52±2.32 | 6 | 5-7 | 6.52±2.32 | 7 | 5-7 | 1.00 | ||||||||
|
p-value between groups† |
0.001** | 0.001** | |||||||||||||
| PTQL Social functional Domain | |||||||||||||||
| DBM (n=30) | 9.53±2.33 | 10 | 8-12 | 10.87±1.50 | 12 | 9.75-12 | 0.003* | ||||||||
| Control (n=29) | 6.24±2.40 | 6 | 4-8 | 6.07±2.20 | 12 | 4-8 | 0.102 | ||||||||
|
p-value between groups† |
0.001** | 0.001** | |||||||||||||
| PTQL Economic Domain | |||||||||||||||
| DBM (n=30) | 4.73±1.63 | 6 | 4-6 | 4.53±1.67 | 5 | 3.5-5 | 0.317 | ||||||||
| Control (n=29) | 3.66±1.83 | 4 | 2-6 | 3.72±1.79 | 4 | 2-6 | 0.157 | ||||||||
|
p-value between groups† |
0.023* | 0.079 | |||||||||||||
| PTQL Self-esteem Domain | |||||||||||||||
| DBM (n=30) | 10.80±3.71 | 11 | 7-15 | 12.63±2.55 | 13 | 11-15 | 0.003* | ||||||||
| Control (n=29) | 9.59±3.01 | 9 | 7-12 | 9.83±3.17 | 11 | 7-13 | 0.083 | ||||||||
|
p-value between groups† |
0.173 | 0.001** | |||||||||||||
3.3. Comparison of QOL between DBM and Control Groups
Baseline scores of total PTQL for the DBM and control groups were significantly different (p = 0.001). After the intervention, the total PTQL median scores in the DBM group had significantly increased (p = 0.001), whereas the scores in the control group remained the same (p = 0.79). The median scores in most domains increased significantly in the DBM group: physical domain, cognitive domain, affective domain, social functional domain, and economic domain (p = 0.004, 0.001, 0.001, 0.001 and 0.023, respectively). However, there was no change in the self-esteem domain (p = 0.173). All of the PTQL domains in the control group were not significantly different (Table 3).
4. DISCUSSION
It has been observed that the deep breathing exercise and body scan meditation combined with music significantly improved the global PSQI and the PSQI components of sleep quality, particularly in sleep efficiency, perceived sleep quality, and daily disturbances. The median scores of sleep efficiency (including sleep duration and sleep efficiency) in the intervention group improved significantly after the intervention. Similar results were reported previously in the older adults in Iran who received an intervention using Benson's relaxation technique to improve the quality of sleep [25]. Likewise, Wang et al. and Feng et al. reported that the sleep efficiency of older adults in China improved after using a music intervention [26, 27]. Moreover, our study showed that the median score of perceived sleep quality (subjective sleep quality, sleep latency and sleep medication) in the intervention group increased significantly after eight weeks. This finding was consistent with previous studies that showed improvement in the scores of subjective sleep quality, sleep latency, and sleep medication [28, 29].
Likewise, sleep disturbances and daytime dysfunction median scores in the intervention group improved significantly after the intervention, which is in keeping with several previous studies that showed that relaxation techniques decreased sleep disturbances and daytime dysfunction in older adults [28, 30]. It seems possible that deep breathing exercises and body scan meditation combined with music improve sleep duration producing an adequate night’s sleep, which in turn increases the ability to perform daily activities. It is possible that music affects the stages of sleep. Sound waves from music are converted into electrical energy in the brain and different sounds may affect the body and mind. Low-frequency music (low intensity of sound) causes alpha brainwaves, which lead to relaxation, thus allowing older adults to fall asleep more easily. When music is played continuously, the parasympathetic nervous system is stimulated and endorphin hormone secretions produce feelings of happiness, calm, and can relieve pain. Collectively these feelings can increase the ease of falling asleep [31, 32].
In the current study, the deep breathing exercise and body scan meditation combined with music improved the total QOL in older adults suffering from poor sleep quality. This finding was consistent with previous studies that reported increased QOL in older adults using similar relaxation techniques - progressive muscular relaxation in Iran, in a nursing home in Spain, and relaxation combined with dance in Malaysia [16, 33, 34]. Other studies have showed that relaxation training improved QOL in patients with diabetes, chronic heart failure, chronic obstructive pulmonary disease, asthma, and patients after radical mastectomy [35-38].
Certain QOL domains such as physical, the cognitive, the social functional, the affective and the self-esteem significantly improved after the intervention, a finding that is consistent with previous studies [16, 18, 33]. Deep breathing and body scan meditation combined with music may stimulate endorphin secretion in the brain and lead to feelings of relaxation and happiness, which also contribute to improving QOL [21]. However, our study did not find any significant difference in the economic domain. It is possible that eight weeks is too short a period for economic assessment. Consequently, the next study should allow more time during the intervention to measure this outcome.
This study highlights the importance of deep breathing exercise and body scan meditation combined with music in improving the quality of sleep in older adults in home-based care. It is important to provide primary health care services in order to improve sleep quality among older adults. These techniques are easy to use at home for improving the time it takes to fall asleep, time asleep over time in the bed, and longer sleep duration in those who have poor sleep quality. The limitations of the study were the small sample size, short duration of treatment and follow-up, important baseline difference, and subjective outcome assessment. There is some suggestion that the combined therapy may improve subjective sleep quality and QOL in the short term. We recommend further exploring this intervention in a larger randomized controlled trial with a longer duration of treatment and follow-up with objective measurements such as biological markers and recording anxiety and stress levels to determine the actual relaxation achieved.
CONCLUSION
The results of this study showed that deep breathing exercise and body scan meditation combined with relaxation music improved sleep quality and QOL in older adults with poor sleep quality. We suggest that healthcare providers use body scan meditation combined with deep breathing training to improve sleep quality in older adults.
AUTHORS' CONTRIBUTIONS
All authors approved the final manuscript and agreed to submit to the Open Public Health Journal for publication.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Research Ethics Committee, Faculty of Medicine, Chiang Mai University, Thailand (No: 538/2015).
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
The legal protection of all participants was ensured and confirmed by written consent.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [P.S], upon reasonable request.
FUNDING
This study was supported by the Faculty of Medicine Research Fund, Chiang Mai University, Thailand (Grant number 050/2016).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to thank the participants. We are also grateful to Dr. Johan Van Rooyen of Webster University (Thailand) for editing this manuscript.


