All published articles of this journal are available on ScienceDirect.
Effect of M-Health Application: “Chicken LOF” (Low Fat in 90 Days) on Lipid Profile and Body Composition Among Dyslipidemia Healthcare Workers: A Randomized Controlled Trial
Abstract
Background:
Non-communicable disease has become a public health concern and is associated with an unhealthy lifestyle and aging.
Objective:
This study aimed to explore the effect of M-Health Application: “CHICKEN LOF” on lipid profile and body composition in healthcare workers with dyslipidemia.
Methods:
This study was a randomized controlled trial conducted on 80 full-time healthcare workers having dyslipidemia from Phuket City Hospital. Participants were randomly assigned by a computer generator into an intervention group and control group. The intervention group received “CHICKEN LOF”: M-Health Application and usual care, and the control group received only usual care. Outcomes were measured on days 30, 60, 90 and compared to baseline.
Results:
The mean age was 33.9 years in the intervention group and 33.2 years in the control group. The baseline characteristics were not statistically or significantly different. However, significant changes were observed in intervention group regarding total knowledge (p<0.001), total attitude (p=0.001), total practice (p<0.001), HDL-C (p=0.002), weight (p<0.001), BMI (p=0.001), body fat percentage (p=0.029), bone mass (p=0.030), BMR (p=0.032) and total body water (p=0.027). In pairwise comparison, a significant increase in knowledge, attitude and practice was found from the baseline to day 30, 60 and 90, respectively.
Conclusion:
In the present study, CHICKEN-LOF mobile application was found to be effective in terms of knowledge, attitude and practice, and contributed to improving lipid and body composition. This study suggests a longer term implementation to evaluate sustainability not only in the healthcare setting but also in the community.
1. INTRODUCTION
Nowadays, more non-communicable diseases (NCDs) prevail than communicable diseases (CDs). Altering patterns of consumption, living standards and aging population are linked with an increased prominence of diseases such as cancers, heart disease, stroke, mental illness, diabetes and other conditions linked to obesity [1]. There is a growing prevalence of NCDs in emerging economies associated with unhealthy modern lifestyles (unhealthy diet, physical inactivity, smoking and the consumption of alcohol) affecting the socio-economic development [2].
In 2015, 17 million premature deaths (under the age of 70) were caused by NCDs, of which 82% were in low- and middle-income countries, and 37% were caused by Cardiovascular Diseases (CVD) [3]. Similarly, in South East Asia, many types of CVDs reported a quarter of all deaths annually. NCDs in Thailand are estimated to account for 74% of all deaths. Proportional mortality of CVDs is around 23% in 399,100 people [4].
Dyslipidemia is the main sign associated with CVDs which is one of the major NCDs. Body composition is also one of the key health status criteria relevant to individuals. The most significant change in body composition is associated with the metabolism system, and in this context, it is linked with dyslipidemia. According to the Thailand health report in 2013, Thai people partook in exercise less frequently, consumed more sweet, oily, and salty food and ate fewer vegetables and fruits, whilst smoking and drinking more alcoholic beverages. This lifestyle being conducive to CVDs/ Diabetes Miletus (DM) [5]].The prevalence of Thai dyslipidemia was found to be 40.2% in women and 30.1% in men, respectively, while a hospital in Thailand reported the prevalence of dyslipidemia in hospital staff during the year 2008-2011 to be 66.5%, 60.3%, 63.4%, 61.5%, respectively [6]. The improvement in dyslipidemia management among healthcare workers will not only benefit themselves but also patients.
Recent advances in information technology (IT) have in turn led to advances in the management of patients, and especially elderly patients with chronic illnesses [7]. There were some studies which have shown the effectiveness of these technologies especially mobile health (m-health) interventions such as smartphone, mobile phone, short message service (SMS) and mobile application on health-related behaviour promoting healthy lifestyle [8]. Therefore, M-Health applications are a means of communicating, collecting patient information and monitoring self-care. This study aims to explore the effect of “CHICKEN LOF”: M-health application on lipid profile and body composition among healthcare workers with dyslipidemia as a communication channel to improve their knowledge, attitude and practice (KAP) of lipid profile and body composition.
2. MATERIALS AND METHODS
2.1. Study Participants and Area
This study was conducted among fulltime healthcare workers having dyslipidemia from Phuket City Hospital, Thailand. It is the first administrative organization hospital and run by the Phuket administrative organization. According to data collected by the hospital, there were a total of 328 full-time staff (physicians not included) with 129 out of 220 staff being monitored showing an abnormal lipid profile during their health check-ups in 2018. The inclusion criteria of the study participants were as follows: 1) Full-time healthcare worker (age 20-55 years old) who had at least one-year working experience at the study hospital, 2) Had taken a lipid profile test in 2018 and had at least one abnormal lipid profile in their result, 3) No clinical symptoms and significant change in body weight in last 12 months, and 4) Having smartphone and internet access. The abnormal lipid profile in this study accounted for total Cholesterol more than 200 mg/dL and/or LDL Cholesterol more than 100 mg/dL and/or HDL Cholesterol Level less than 60 mg/dL and/or Triglyceride Level more than 150 mg/dL. Participants with pregnancy or planned pregnancy within 3 months of this trial were excluded from this study and participants who received new medicines for lipid profile lowering after starting the program were excluded from this study.
2.2. Study Design and Sample Size
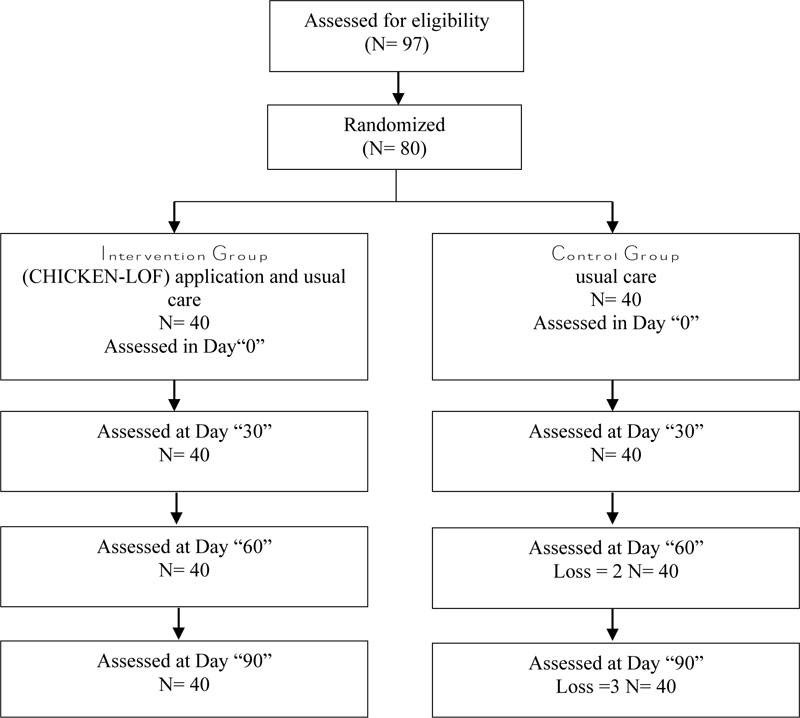
This study was a randomized controlled trial. The sample size was calculated by G*power 3.1.5 program. After adding a 10% drop-out and consideration for type II error, the final size for each group was 40, and the total sample size for this study was 80 full-time healthcare workers with dyslipidemia. Then, participants were randomly assigned by a computer generator into 2 groups (intervention and control). The participants were blinded when given treatment. The intervention group received “CHICKEN LOF”: M-Health Application and usual care. The control group received only usual care. Both groups were homogeneity tested to confirm the similarity between the 2 groups. The methodology “Intention to Treat Analysis” was used; the following flow chart is shown in Fig. (1).
A total of 4 serial measurements were done at day 0 (baseline), 30, 60 and 90. A self-administered questionnaire was used and there were 3 parts of the instruments as follows;
- Characteristics and lifestyle effects on health including general characteristics of the participants (age, gender, night shift (hours/ week), smoking and alcohol consumption) and lifestyle-related activities (dietary habits, exercise, hours of sleep, vitamin D intake, water consumption and job stress).
- Knowledge Attitude and Practice. In the Knowledge part of the assessment, a total of 19 statements were included and scored “1” point for “True”, and “0” point for “False”, “Do not know” and “Incorrect” answers. The total score varied from 0 to 19. A total of 16 statements were included and Likert scale was used: “5” points for “Strongly Disagree (SD)”, “4” points for “Disagree (D)”, “3” points for “Neutral (N)”, “2” points for “Agree (A)” and “1” point for “Strongly Agree (SA)” for all “Negative” statements while reverse scoring of 1 point to 5 points was for all “Positive” statements. The total score varied from 16 to 80. In the Practice part, there were a total of 20 statements and scored “1” point for “Always”, “2” points for “Sometimes” and “3” points for “Never” for all “Negative” statements and reverse scoring for all “Positive” statements. The total score varied from 20 to 60. The knowledge score was divided into 1 point, attitude score was divided into 5 points and the practice score was divided into 4 points.
- Record list of Lipid Profile and Body Composition. Lipid Profile was completed by the hospital blood department and it included TC (mg/dL), HDL-C (mg/dL), TG (mg/dL), and LDL-C (mg/dL). Results were required to be reported to the researcher and assistants within 7days after the test. The “TANITA model BC-731: Body Composition Monitor” from the hospital was used as a tool of assessment for body composition and it measured Waist(cm), Hip (cm), BMI (kg/m2), Body fat mass (kg), Body fat percentage (%), Fat free mass (kg), Skeletal muscle mass (kg), Visceral fat level, Waist-Hip ratio, and Basal metabolic rate (kcal). All blood samples were destroyed according to proper hospital procedures after results were attained.
2.4. Outcomes
The primary outcome of this present study was to compare the change of KAP of lipid profile and body composition modifying within and between groups at day 30, 60, 90 and baseline. The secondary outcomes were to compare the change of lipid profile and body composition within and between groups at day 30, 60, 90 and baseline.
2.5. Intervention and Setting
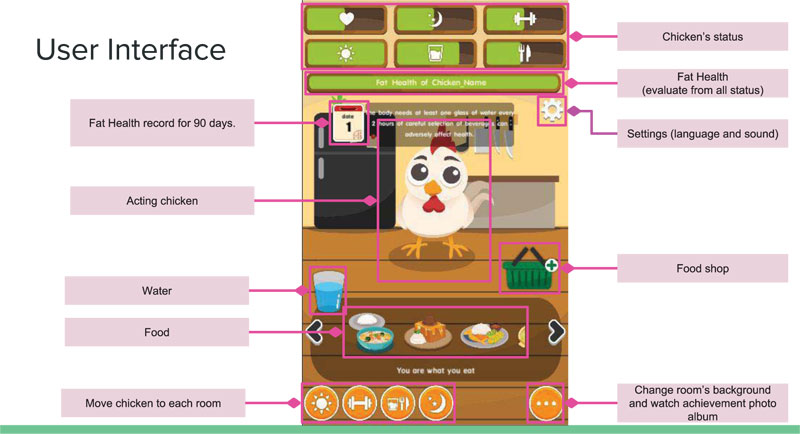
The “CHICKEN LOF” application was developed from a board game for this study with the players (users) being representative of themselves. This application has both English and Thai versions. There are 6 modes in the application. They are as follows; a walk in the sun, be happy, calm and sleep, drink more water, exercise daily, and food control. This application was installed directly into each of the personal mobile phones of participants as it cannot be downloaded online. The user interface of the Chicken LOF mobile application is shown in Fig. (2).
The participants from the control group did not receive this application. Both the control group and intervention group received usual care which included general consultation by the physician in the hospital regarding diet and exercise after blood testing.
2.6. Statistical Analysis
The present study used SPSS version 22 for data analysis and homogeneity of baseline characteristics was analysed by using Independent t-test for nominal data and Chi-square test for categorical data. For inferential statistics, One-Way ANOVA Repeated Measurement was used for comparison of all time points within groups for both the intervention group and the control group. The pairwise comparison of One-Way ANOVA Repeated Measurement was done for the intervention group at different times of measurement. The Independent t-test was used to compare the change between the intervention group and the control group for all time points. The level of significance was set at p < 0.05 for all statistical analyses.
3. RESULTS
The mean age of the intervention group was 33.9 years and that of the control group was 33.2 years. Most of the participants were females (29 participants in the intervention group and 33 participants in the control group). Both groups had a night shift of approximately 10 hours/week. About half of the participants from each group had job stress and more than half of the participants slept less than 7 hours. In both groups, no daily cholesterol/ calories control (32 participants in the intervention and 29 participants in control) and no daily exercise (38 participants in the intervention and 35 participants in control) were found. All of the baseline characteristics showed no statistically significant difference between the intervention group and the control group.
The statistically significant differences between the intervention group and the control group were found in terms of total knowledge (p=0.002 on day 60 and p=0.003 at day 90), total attitude (p=0.009 on day 60 and p=0.001 at day 90), HDL-C (p=0.049 at day 90) and LDL-C (p=0.048 at day 90).
Table 1 shows the modifiying total knowledge, attitude and practice regarding lipid and body composition within groups at baseline, day 30, 60 and 90. All of the participants in the intervention group showed statistically significant differences in the mean score of total knowledge, attitude and practice (P< 0.001, p= 0.001 and p< 0.001 respectively).
The change of lipid profile within groups at baseline, day 30, 60 and 90 is shown in Table 2. Only TG (mg/dl) showed statistically significant changes in mean score within the intervention group (p= 0.002).
Table 3 shows the change in body composition within groups at baseline, day30, 60 and 90. Among all variables of body composition, the following variables showed statistically significant changes in the intervention group: weight (Kg), BMI (kg/m2), Body fat percentage (%), bone mass, BMR, Total Body Water (%) (p< 0.001, p= 0.001, p= 0.029, p= 0.030, p= 0.032 and p= 0.027, respectively.
Pairwise comparison of knowledge, attitude, practice, lipid profile and body composition within the intervention group at baseline, day 30, 60 and 90 is shown in Table 4 and Table 5. In KAP, there were statistically significant mean differences between baseline and at day 30, 60 and 90. In the lipid profile of HDL-C (mg/dl), statistically significant mean differences were found between baseline and day 60, and between day 30 and 90. In BMI (kg/m2), all time points showed statistically significant mean differences except between day 30 and 60, and between day 60 and 90.
Within-group comparison by using one-way anova repeated measure
| KAP | Group | Source |
Sum of Squares |
df |
Mean Squares |
F | P value |
| Knowledge Total | Intervention | Time (Baseline, Day30, 60, 90) | .377 | 3 | .126 | 7.573 | <.001* |
| Error (Time) | 1.942 | 117 | .017 | ||||
| Control | Time (Baseline, Day30, 60, 90) | .015 | 3 | .005 | .221 | .882 | |
| Error (Time) | 2.406 | 108 | .022 | ||||
| Attitude Total | Intervention | Time (Baseline, Day30, 60, 90) | 2.459 | 3 | .820 | 6.306 | .001* |
| Error (Time) | 15.206 | 117 | .130 | ||||
| Control | Time (Baseline, Day30, 60, 90) | .113 | 3 | .038 | .242 | .867 | |
| Error (Time) | 16.827 | 108 | .156 | ||||
| Practice Total | Intervention | Time (Baseline, Day30, 60, 90) | .610 | 3 | .203 | 7.339 | <.001* |
| Error (Time) | 3.244 | 117 | .028 | ||||
| Control | Time (Baseline, Day30, 60, 90) | .040 | 3 | .013 | .410 | .746 | |
| Error (Time) | 3.543 | 108 | .033 |
| Lipid profile | Group | Source | Sum of Squares |
df | Mean Squares |
F | P-value |
| TC (mg/dL) | Intervention | Time (Baseline, Day30, 60, 90) | 2363.619 | 3 | 787.873 | 1.650 | .182 |
| Error (Time) | 55871.131 | 117 | 477.531 | ||||
| Control | Time (Baseline, Day30, 60, 90) | 657.378 | 3 | 219.126 | .560 | .643 | |
| Error (Time) | 42297.122 | 108 | 391.640 | ||||
| TG (mg/dL) | Intervention | Time (Baseline, Day30, 60, 90) | 1729.350 | 3 | 576.450 | .380 | .768 |
| Error (Time) | 177443.150 | 117 | 1516.608 | ||||
| Control | Time (Baseline, Day30, 60, 90) | 1589.750 | 3 | 529.917 | .120 | .948 | |
| Error (Time) | 478205.500 | 108 | 4427.829 | ||||
| HDL-C (mg/dL) | Intervention | Time (Baseline, Day30, 60, 90) | 498.669 | 3 | 166.223 | 5.201 | .002* |
| Error (Time) | 3739.581 | 117 | 31.962 | ||||
| Control | Time (Baseline, Day30, 60, 90) | 194.831 | 3 | 64.944 | 2.258 | .086 | |
| Error (Time) | 3105.919 | 108 | 28.759 | ||||
| LDL-C (mg/dL) | Intervention | Time (Baseline, Day30, 60, 90) | 374.075 | 3 | 124.692 | .143 | .934 |
| Error (Time) | 102368.925 | 117 | 874.948 | ||||
| Control | Time (Baseline, Day30, 60, 90) | 5519.101 | 3 | 1839.700 | .870 | .459 | |
| Error (Time) | 228315.149 | 108 | 2114.029 |
| Body composition | Group | Source | Sum of Squares |
df | Mean Squares |
F | P-value |
| Weight (Kg.) | Intervention | Time (Baseline, Day30, 60, 90) | 54.321 | 3 | 18.107 | 8.007 | <.001* |
| Error (Time) | 264.599 | 117 | 2.262 | ||||
| Control | Time (Baseline, Day30, 60, 90) | 3.753 | 3 | 1.251 | .524 | .666 | |
| Error (Time) | 257.620 | 108 | 2.385 | ||||
| BMI (kg/m2) | Intervention | Time (Baseline, Day30, 60, 90) | 16.090 | 3 | 5.363 | 5.713 | .001* |
| Error (Time) | 109.847 | 117 | .939 | ||||
| Control | Time (Baseline, Day30, 60, 90) | 3.417 | 3 | 1.139 | .783 | .506 | |
| Error (Time) | 157.168 | 108 | 1.455 | ||||
| Body fat percentage (%) | Intervention | Time (Baseline, Day30, 60, 90) | 208.221 | 3 | 69.407 | 3.123 | .029* |
| Error (Time) | 2600.246 | 117 | 22.224 | ||||
| Control | Time (Baseline, Day30, 60, 90) | 21.290 | 3 | 7.097 | 1.051 | .373 | |
| Error (Time) | 729.298 | 108 | 6.753 | ||||
| Visceral Fat Level | Intervention | Time (Baseline, Day30, 60, 90) | .389 | 3 | .130 | .331 | .803 |
| Error (Time) | 45.856 | 117 | .392 | ||||
| Control | Time (Baseline, Day30, 60, 90) | .056 | 3 | .019 | .025 | .995 | |
| Error (Time) | 80.487 | 108 | .745 | ||||
| Muscle Mass (kg) | Intervention | Time (Baseline, Day30, 60, 90) | 8.926 | 3 | 2.975 | 1.799 | .151 |
| Error (Time) | 193.457 | 117 | 1.653 | ||||
| Control | Time (Baseline, Day30, 60, 90) | 10.925 | 3 | 3.642 | .885 | .451 | |
| Error (Time) | 444.172 | 108 | 4.113 | ||||
| Physique Rating | Intervention | Time (Baseline, Day30, 60, 90) | 1.092 | 3 | .364 | 1.030 | .382 |
| Error (Time) | 41.345 | 117 | .353 | ||||
| Control | Time (Baseline, Day30, 60, 90) | .541 | 3 | .180 | .314 | .815 | |
| Error (Time) | 61.959 | 108 | .574 | ||||
| Bone Mass | Intervention | Time (Baseline, Day30, 60, 90) | .217 | 3 | .072 | 3.089 | .030* |
| Error (Time) | 2.743 | 117 | .023 | ||||
| Control | Time (Baseline, Day30, 60, 90) | .029 | 3 | .010 | 1.050 | .374 | |
| Error (Time) | 1.008 | 108 | .009 | ||||
| BMR | Intervention | Time (Baseline, Day30, 60, 90) | 22141.925 | 3 | 7380.642 | 3.037 | .032* |
| Error (Time) | 284355.075 | 117 | 2430.385 | ||||
| Control | Time (Baseline, Day30, 60, 90) | 11687.486 | 3 | 3895.829 | 1.364 | .258 | |
| Error (Time) | 308572.514 | 108 | 2857.153 | ||||
| Metabolic Age | Intervention | Time (Baseline, Day30, 60, 90) | 29.300 | 3 | 9.767 | 1.215 | .307 |
| Error (Time) | 940.200 | 117 | 8.036 | ||||
| Control | Time (Baseline, Day30, 60, 90) | 141.243 | 3 | 47.081 | 1.445 | .234 | |
| Error (Time) | 3518.257 | 108 | 32.576 | ||||
| Total Body Water (%) | Intervention | Time (Baseline, Day30, 60, 90) | 15.109 | 3 | 5.036 | 3.172 | .027* |
| Error (Time) | 185.756 | 117 | 1.588 | ||||
| Control | Time (Baseline, Day30, 60, 90) | .052 | 3 | .017 | .007 | .999 | |
| Error (Time) | 256.580 | 108 | 2.376 | ||||
| Waist-Hip Ratio | Intervention | Time (Baseline, Day30, 60, 90) | .014 | 3 | .005 | 1.834 | .145 |
| Error (Time) | .295 | 117 | .003 | ||||
| Control | Time (Baseline, Day30, 60, 90) | .004 | 3 | .001 | .832 | .479 | |
| Error (Time) | .179 | 108 | .002 |
| Variable | Group | Time | Mean difference | Std.Error | P-value | 95%CI for difference | |
| Lower bound | Upper bound | ||||||
| Knowledge Total |
Intervention | Baseline-Day30 | -0.069 | .022 | .003* | -0.113 | -0.025 |
| Baseline-Day60 | -0.102 | .031 | .002* | -0.164 | -0.040 | ||
| Baseline-Day90 | -0.130 | .040 | .002* | -0.210 | -0.050 | ||
| Day30-Day60 | -0.033 | .023 | .167 | -0.080 | .014 | ||
| Day30-Day90 | -0.061 | .029 | .041* | -0.120 | -0.003 | ||
| Day60-Day90 | .028 | .024 | .251 | -0.078 | .021 | ||
| Attitude Total |
Intervention | Baseline-Day30 | -0.185 | .086 | .039* | -0.359 | -0.10 |
| Baseline-Day60 | -0.231 | .100 | .026* | -0.433 | -0.030 | ||
| Baseline-Day90 | -0.344 | .097 | .001* | -0.541 | -0.147 | ||
| Day30-Day60 | -0.047 | .060 | .442 | -0.168 | .075 | ||
| Day30-Day90 | -0.159 | .063 | .016* | -0.286 | -0.032 | ||
| Day60-Day90 | -0.112 | .068 | .104 | -0.249 | .024 | ||
| Practice Total |
Intervention | Baseline-Day30 | -0.084 | .035 | .020* | -0.154 | -0.014 |
| Baseline-Day60 | -0.160 | .041 | <0.001* | -0.242 | -0.078 | ||
| Baseline-Day90 | -0.139 | .036 | <0.001* | -0.212 | -0.066 | ||
| Day30-Day60 | -0.076 | .040 | .068 | -0.157 | .006 | ||
| Day30-Day90 | -0.055 | .034 | .116 | -0.124 | .014 | ||
| Day60-Day90 | .021 | .037 | .579 | -0.054 | .096 | ||
| Variables | Group | Time | Mean difference | Std.Error | P-value | 95%CI for difference | |
| Lower bound | Upper bound | ||||||
| Lipid profile | |||||||
| HDL-C | Intervention | Baseline-Day30 | -2.000 | 1.210 | .106 | -4.447 | .447 |
| (mg/dL) | Baseline-Day60 | 3.250 | 1.591 | .048* | -6.468 | -0.032 | |
| Baseline-Day90 | -4.825 | 1.189 | <0.001* | -7.229 | -2.421 | ||
| Day30-Day60 | -1.250 | 1.028 | .231 | -3.330 | .830 | ||
| Day30-Day90 | -2.825 | 1.251 | .030* | -5.356 | -0.294 | ||
| Day60-Day90 | -1.575 | 1.248 | .214 | -4.099 | .949 | ||
| Body composition | |||||||
| Weight | Intervention | Baseline-Day30 | .448 | .233 | .063 | -0.025 | .920 |
| (Kg.) | Baseline-Day60 | .960 | .396 | .020* | .159 | 1.761 | |
| Baseline-Day90 | 1.563 | .398 | .000* | .758 | 2.367 | ||
| Day30-Day60 | .512 | .288 | .083 | -0.070 | 1.095 | ||
| Day30-Day90 | 1.115 | .371 | .005* | .364 | 1.866 | ||
| Day60-Day90 | .602 | .297 | .049* | .002 | 1.203 | ||
| BMI | Intervention | Baseline-Day30 | .265 | .129 | .047* | .004 | .526 |
| (kg/m2) | Baseline-Day60 | .653 | .269 | .020* | .109 | 1.196 | |
| Baseline-Day90 | .805 | .262 | .004* | .276 | 1.334 | ||
| Day30-Day60 | .387 | .231 | .102 | -0.080 | .855 | ||
| Day30-Day90 | .540 | .242 | .031* | .051 | 1.029 | ||
| Day60-Day90 | .152 | .112 | .181 | -0.074 | .379 | ||
| Body fat | Intervention | Baseline-Day30 | .195 | 1.406 | .890 | -2.650 | 3.040 |
| percentage | Baseline-Day60 | 1.208 | .698 | .092 | -0.205 | 2.620 | |
| (%) | Baseline-Day90 | 2.880 | .880 | .002* | 1.101 | 4.659 | |
| Day30-Day60 | 1.012 | 1.249 | .422 | -1.513 | 3.538 | ||
| Day30-Day90 | 2.685 | 1.264 | .040* | .128 | 5.242 | ||
| Day60-Day90 | 1.672 | .520 | .003* | .622 | 2.723 | ||
| Bone Mass | Intervention | Baseline-Day30 | .055 | .036 | .131 | -0.017 | .127 |
| Baseline-Day60 | .088 | .043 | .051 | .000 | .175 | ||
| Baseline-Day90 | .093 | .042 | .035* | .007 | .178 | ||
| Day30-Day60 | .032 | .030 | .286 | -0.028 | .093 | ||
| Day30-Day90 | .037 | .031 | .227 | -0.024 | .099 | ||
| Day60-Day90 | .005 | .016 | .750 | -0.027 | .037 | ||
| BMR | Intervention | Baseline-Day30 | 11.475 | 4.356 | .012* | 2.664 | 20.286 |
| Baseline-Day60 | 25.625 | 13.039 | .057 | -0.749 | 51.999 | ||
| Baseline-Day90 | 29.650 | 13.017 | .028* | 3.320 | 55.980 | ||
| Day30-Day60 | 14.150 | 12.729 | .273 | -11.596 | 39.896 | ||
| Day30-Day90 | 18.175 | 13.160 | .175 | -8.443 | 44.793 | ||
| Day60-Day90 | 4.025 | 5.955 | .503 | -8.021 | 16.071 | ||
| Total Body Water (%) | Intervention | Baseline-Day30 | -0.107 | .168 | .527 | -0.448 | .233 |
| Baseline-Day60 | -0.387 | .294 | .195 | -0.981 | .206 | ||
| Baseline-Day90 | -0.795 | .368 | .037* | -1.539 | -0.051 | ||
| Day30-Day60 | -0.280 | .225 | .221 | -0.735 | .175 | ||
| Day30-Day90 | -0.688 | .315 | .035* | -1.325 | -0.050 | ||
| Day60-Day90 | -0.408 | .277 | .149 | -0.967 | .152 | ||
4. DISCUSSION
In this study, it was found that the CHICKEN LOF (M-Health application) had positive effects on total knowledge, attitude and practice of lipid and body composition, lipid profile (HDL-C) and body composition (Weight, BMI, Body Fat percentage, Bone Mass, BMR and Total Body Water percentage) among healthcare workers in Phuket City hospital. In a systematic review study on mobile phone interventions to increase physical activity and reduce weight, it was pointed out that all technology interventions including mobile phone applications with health education components are effective for physical activity and weight reduction [9]. This current CHICKEN LOF application supports users (participants) in their accountability or self-monitoring for healthy lifestyle [10]. This is supported by a systematic review study on mobile phone intervention for facilitating self-management of long term illness in which m-Health proved to be useful for self-monitoring and self-management [11].
The intervention group had shown that there was statistically significant mean difference in knowledge, attitude and practice in the intervention group compared to the control group. Increased means of total knowledge, attitude and practice of lipid profile and body composition at day 30, 60 and 90 compared to baseline were found. It can be stated that this study using m-Health intervention was useful in improving health knowledge and attitude and practice for self-management of metabolic disorders such as obesity and diabetes. The findings accord with another study on translating exercise intentions into behaviour [12].
Although it is important to reduce LDL-C in the lipid profile to treat dyslipidemia, there was no significant change in the reduction of LDL-C within the intervention group in this study [13]. This result is in contrast with the study on the efficacy of combined strategy for hypercholesterolemia patients that there was a reduction in LDL-C [14]. It can be related to those participants who had night shift load, that the cumulative and annual incidence of metabolic syndrome is higher among night-shift healthcare workers than day-shift healthcare workers (2.9% versus 0.5%) [15]. Among lipid profiles, HDL-C (mg/dl) in the intervention group showed a significant mean difference between baseline and day 90, and between day 30 and 90 with a positive effect.
The participants in the intervention group presented a significant change in body composition (Weight, BMI, Body Fat percentage, Bone Mass, BMR, Total Body Water) compared to the control group. The weight and BMI of participants in the intervention group increased from baseline to day 30, 60 and 90 and this result is in contrast with the study on the effect of lifestyle modification using the smartphone application which might be due to different participants of studies (healthcare workers versus patients) [16]. This result is also in contrast with the study on the efficacy of smartphone-based weight loss intervention [17]. It might be due to a short-term lifestyle modification by using a mobile phone application; however, this did not have a significant impact but it is feasible and more effective than other interventions and low and middle-income countries can easily apply this intervention. In another study on the effectiveness of smartphone application for weight loss, there was no increased weight loss compared to the control group and it might be related to lack of motivation of the participants to lose weight and/or lack of self-monitoring regarding their diet and physical activity. Therefore, it is required to question participants regarding their intention, interest, motivation and whether they have a goal in mind to lose weight in the screening process of the study [18].
There are some limitations in the present study. The study was conducted for only 90 days whilst there can be more reduction and changes in both the lipid profile and body composition in long term implementation. The participants of this present study were healthcare workers and had medical/ health knowledge, so there may be generalization of outcomes.
CONCLUSION
This present study has shown a positive effect of M-Health application: CHICKEN LOF on lipid and body composition among healthcare workers with dyslipidaemia. It is also feasible to apply for self-monitoring of healthy lifestyles in the community especially in low and middle-income countries. Further studies with longer implementation periods are recommended for the sustainable effect of M-health interventions. Policymakers should include this Chicken LOF mobile application in the policies once a longer duration research had shown effectiveness, and it should be applied in primary care settings.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The ethical approval of this study was taken from the Research Ethics Review Committee for Research Involving Human Research Participants, Health Sciences Group, Chulalongkorn University, Thailand (COA no. 249/2019).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
This study took informed and written consent from all participants. Participants were informed regarding the purpose of the study including usage and publication of data, anonymity, confidentiality and freedom to participate and withdraw.
AVAILABILITY OF DATA MATERIALS
The data supporting the findings of the article is available in the SuwadeePuntpanich at suwadeepuntpanich@gmail.com with the reference “COA 249/2019”.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors thank the management team, all supporting staff and the participants (healthcare workers) of the Phuket City Hospital.


