All published articles of this journal are available on ScienceDirect.
Incentives for Multimodal Treatment-first Step Towards Pay for Quality (P4Q) for Chronic Care: Health Services Research from Germany
Abstract
Background:
Pay for Quality (P4Q) is being discussed as an incentive to ensure high quality standards despite cost pressure in healthcare. However, P4Q can also have adverse effects, and the evidence for its effectiveness is limited, especially regarding chronic conditions and multimorbidity. For the treatment of the latter, specific evaluation criteria were defined. Whether these are feasible in the context of costs and remunerations is analyzed in this study using the German DRG system as an example. The aim is to show conditions under which P4Q can be effective.
Methods and Results:
Costs and remuneration for hospitals were compared for an exemplary geriatric indication, with and without complex treatment. Doing so, cost weights were shown to be more than triple for the latter. The results are applicable to health care systems with P4Q or similar approaches.
Conclusion:
Introducing complex treatments poses higher and costly demands regarding structure, processes, and interdisciplinary cooperation in organizations. Additional average costs can be calculated by comparison to regular treatment. Covering the extra costs creates the necessary conditions for P4Q and makes the implementation of complex treatments more likely. As high standards have to be guaranteed for complex treatments and patient satisfaction rises when these are introduced, quality improvements can be assumed. This study can inform Health policy (incentive models) medical societies, give impulses for quality management, and healthcare research (patient-oriented health, e.g. consumer-driven health care, shared decision-making). Future studies should report patient-related outcomes and investigate further diagnoses.
1. INTRODUCTION
The demand for health care services is rising due to demographic changes and an increase in patients with chronic conditions and multimorbidity. In combination with technological and scientific development, this makes the health system more costly. However, this does not automatically lead to quality improvements [1], often due to rigid remuneration systems without incentives for quality enhancement [2].
Pay for Quality (P4Q) is being discussed as one of the potential solutions. The number of scientific contributions on the topic has risen, but the evidence regarding effectiveness is limited. Moreover, P4Q programs targeting multimorbidity are rare [3], even though they may prove to be effective [4]. This is because they tend to focus on structural and procedural quality criteria, which are closely linked and thought to improve the outcome, without always providing proof.
Overall, research on P4Q has so far focused on (directly) influencing the quality of outcomes [5], while structural and process indicators have been less debated. However, in the case of complex treatments, these indicators are vital, especially concerning chronically ill or multimorbid patients for whom [1] outcome quality criteria are limited and [2] treatment needs to be given by a highly qualified, multidisciplinary team, over a longer period and high intensity of care. The latter aspect poses increased demands on the structure and process quality, which must be compensated for. Whether this is feasible and done is analyzed in this study using the German DRG system as an example. The aim is to show conditions under which P4Q can be effective.
2. BACKGROUND
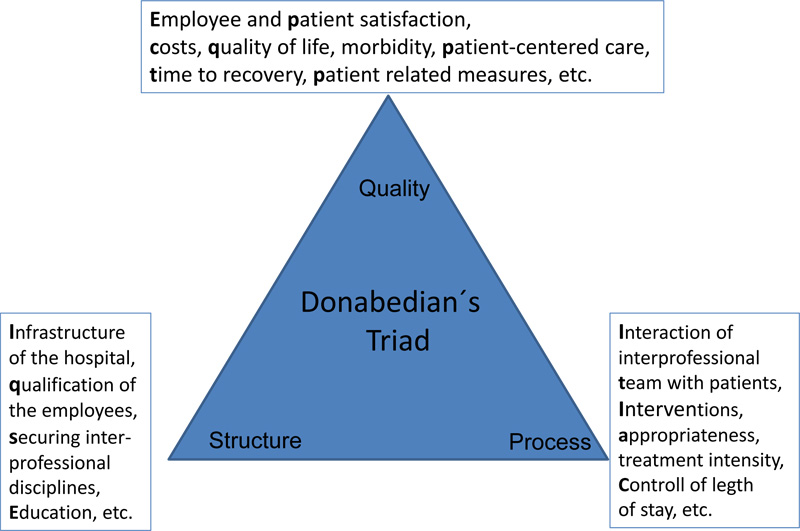
First impulses for developing innovative care systems that ensure quality and patient safety, as well as incentives for care providers, came from reports of the Institute of Medicine (IOM) in 1999 aus (IOM, 2001). In this context, various incentivization models (P4Q, P4P) are being discussed on a global level. Their aim is to promote treatment quality and remunerate care givers accordingly by defining mandatory quality requirements, which, in this study, are differentiated using Donabedian’s Triad.
So far, no reliable form of incentive structure has been found [5]. Some studies have reported that an undesirable effect of P4Q was to deny treatment to patients with multiple, serious comorbidities [6]. This issue can be addressed by specifying criteria for patients and, thus, remunerations to provide clarity for service providers and payers [7].
3. COMPLEX TREATMENT CODES
In Germany, this was done by introducing the possibility of complex treatment codes in the German procedure classification (OPS). OPS is an adaptation of the International Classification of Procedures in Medicine (ICPM) of the World Health Organisation (WHO). The purpose of including complex treatment codes was to make costly and specialized treatments billable in the German diagnosis-related groups (G-DRG) system.
3.1. Implementation
The cost weight of a DRG is used to determine its revenue. The average value of a cost weight is 1.0. The Institute for the Hospital Remuneration System (InEK) in Germany is responsible for calculating cost weights. It annually determines the values for each specific DRG based on the cost data reference hospitals submit. In 2017, cost weights were calculated using the following formula:
Cost weight = (personnel expenses: adjustment value) + (material costs: estimated federal base rate 2017 + InEK reference value 2017) x 0.5 + (infrastructure costs: adjustment value)
The adjustment value is a monetary value that introduces the material cost adjustment to calculate the cost weights of personnel and infrastructure. Thus, a patient case that has a higher cost weight than 1.0, according to its DRG classification, is more costly compared to the average and, thus, remunerated differently.
Applying the classification and remuneration code for complex treatments requires an in-patient stay of more than 14 days (some at least 21 days), and providing a comprehensive, interprofessional therapy aiming at the restoration of the functional ability. The number of treatment sessions during the in-patient stay is specified and has to be documented. The treatment aims, context, and plans are developed by an interdisciplinary team that has to meet certain standards regarding qualification and professional diversity. The plan is checked in frequent and documented meetings of the whole team and the treatment objectives are evaluated at least at discharge. Thus, structural, procedural and outcome quality indicators according to the Donabedian model are accounted for [8].
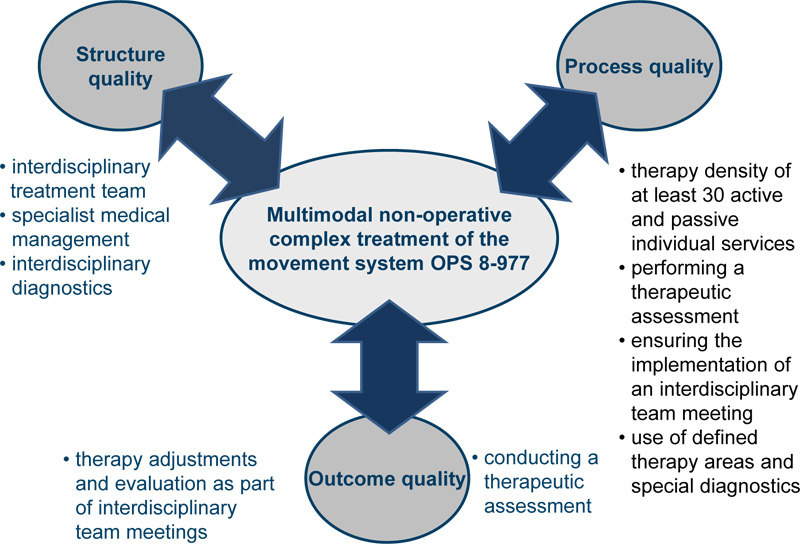
3.2. Multimodal Non-surgical Complex Treatment of the Musculoskeletal System (OPS 8-977)
OPS 8-977 was developed for the conservative treatment of complex musculoskeletal disorders. In this course of treatment, an interdisciplinary team aims to reduce the pain and improve physical abilities. It defines and meets to evaluate treatment goals and modify the treatment. It evaluates, under medical supervision, the standardized therapeutic assessment of different disciplines for the respective treatment procedures. OPS 8-977 requires in-patient hospitalization of at least 12 days, with interdisciplinary diagnostics and treatment under specialist medical supervision. Diagnostics and at least 5 diagnostic procedures belong to both structural and procedural features of a complex treatment. This specification should serve to analyze the significance of the causes of the disease and its influencing factors.
The OPS distinguishes between service area 1 (medical and psychological therapy) and service area 2 (procedures performed by therapists). Service area 1 must consist of a minimum of three procedures from the areas of pain treatment (infusions, modification of pharmacological treatment), reflex therapy (e.g. neural therapy, acupuncture, transcutaneous electrical nerve stimulation, etc.), manual medicine, infiltration therapy (e.g. therapeutic local anesthesia, anesthetic blockages, intraarticular or periarticular injections, spinal injections) and psychotherapy (e.g. cognitive behavioral therapy, person-centred psychotherapy).
OPS 8-977 requires a therapeutic application of at least three of the following procedures from service group 2: physiotherapy and manual therapy, physical therapy, relaxation techniques, medical therapeutic training. In total, 30 active and passive procedures from both service groups must be performed during the at least 12-day in-patient hospitalization.
4. METHODS
As example for multimodal in-patient care, we chose muscoskeletal diseases.
First, a procedure analysis was performed according to the specifications of Donabedian`s Triad for the multimodal non-surgical complex treatment of the musculoskeletal system (coded as OPS 8-977 in the German system).
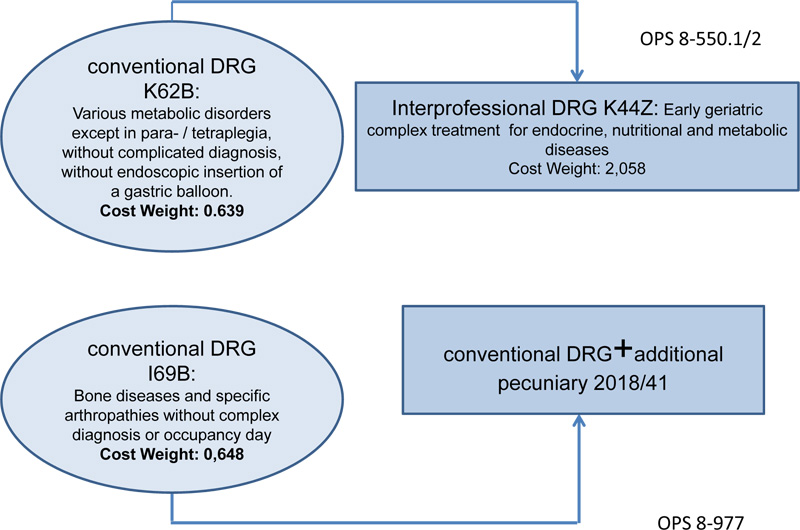
Second, the differences with and without complex treatment for (a) OPS 8-977 and (b) early geriatric rehabilitation therapy (OPS 8-550), were investigated. Specifically, the reimbursement implications for hospitals for an exemplary condition of OPS 8-977, namely bone diseases and specific arthropathies (OPS 8-977, I69A), and a particular condition of OPS 8-550: geriatric treatment for metabolic disorders (OPS 8-550, K62B), were all shown.
5. RESULTS
The results are presented below.
5.1. Procedure Analysis
OPS 8-977 was analyzed regarding structure, process, and outcome quality. Subsequently, the aspects covered in the regulations were related to the respective dimension of the triad and are listed in the table below:
The summary shows an assignment of Multimodal non-operative complex treatment to the quality dimensions, according to Doanbedian (Fig. 1).
| Dimension | Elements |
|---|---|
| Structure quality | interdisciplinary diagnostics, specialist treatment line, neuro-orthopedic structural diagnostics, manual medical function diagnostics, pain diagnosis, apparative diagnostics in functional pathological aspects (e.g., X-ray, MRI, CT, video-assisted motion analysis, posturography, computer-assisted motion or force measurement, EMG, optimization), psychodiagnostics, manual medicine, reflex therapy, infiltration therapy / interventional pain therapy, manual therapy and physiotherapy on a neurophysiological basis, medical training therapy, physical therapy, relaxation techniques |
| Process quality | at least 12 days of treatment, application of 5 diagnostic procedures, use of at least 3 of the following procedures: manual medicine, reflex therapy, infiltration therapy /interventional pain therapy, psychotherapy, use of at least 3 of the following procedures: manual therapy and physiotherapy based on neurophysiology, medical training therapy, physical therapy, relaxation procedures, achieving a therapy density of at least 30 active and passive individual services from the two performance groups, interdisciplinary team meeting |
| Outcome quality | conducting a therapeutic assessment |
5.2. Cost and Remuneration Analysis
In Fig. (2), the results (Institute for the Hospital Remuneration System, InEK) (Germany) referring to the multimodal complex treatment are shown on the right, those on the left refer to the standard treatment. As can be seen, the cost weights and, thus, the remuneration are very different. Complex treatment (OPS 8-550) leads to a cost weight more than three times higher than for standard treatment (3.22 for metabolic disorders).
The supplementary reimbursement, which is paid in addition to the DRG, is the result of negotiations of each individual hospital with its payers (OPS 8-977). In the case of a patient with polyarthritis (DRG I69B, cost weight 0.648), the hospital will receive approx. € 2.300 plus, for example, a supplementary reimbursement of € 1.500, which corresponds to a total of € 3.800 (Fig. 2).
6. DISCUSSION
Demographic change, a rising number of chronically ill and multimorbid patients not only affect individuals [9], but also leads to higher costs for the healthcare sector [10]. Health policy makers are looking for treatment options that are effective and targeted to individual patient needs [11]. The resultant continuing and intensive treatment necessary has to be implemented and compensated for [12]. Pay for Quality (P4Q) is being discussed as an option and the aim of the present study is to show conditions under which it can be effective.
Independent of the diagnosis, the implementation of P4Q is difficult [13]. Therefore, defining the basis, i.e., adequate interdisciplinary treatment models for various indications that also allow for personalization to cover individual needs, is called for first. This needs to be combined with a clear definition of quality criteria that are measurable. OPS 8-977 could serve as an example for chronic conditions of the musculoskeletal system, and this analysis based on Donabedian as a guideline for differentiating indicators. These could be linked to costs incurred, which, in the diagnoses presented here, is about triple the amount of regular treatment. Subsequently, remuneration should at least cover the costs for the treatment to make the implementation of complex treatment more likely. Developing a fair, standardized calculation base would be a vital step towards a unified incentivization system to be further refined by health policy, for example, by integrating patient-reported outcome measures.
CONCLUSION
The study showed how quality indicators could be analyzed for selected complex treatments, with a focus on the multimodal treatment of patients with chronic conditions Fig. (3). The interdisciplinary nature of complex treatments sets special requirements for the team structure and team processes [14]. For this, service providers need to be adequately remunerated. The incentive structure developed in Germany has an innovative character since it takes into account the expenditure pattern of reference hospitals. Cost weights for complex treatments are developed on this basis and remunerate patient care that is provided by an interdisciplinary team. Moreover, patient satisfaction rises when comparing data before and after the introduction of complex multimodal treatments [7]. Thus, the introduction of complex multimodal treatment codes in the G-DRG system has a high probability of improving the quality of care.
As only two complex treatments were analyzed, future studies should investigate further diagnoses. Moreover, the outcome indicators are not yet linked to incentive payments, therefore including patient reported outcome measures is recommended for the further development of P4Q approaches and their analysis.
LIST OF ABBREVIATIONS
| G-DRG | = German Diagnosis related Groups |
| ICPM | = International Classification of Procedures in Medicine |
| InEK | = Institute for the Hospital Remuneration System |
| OPS | = Operation and Procedure Code |
| P4Q | = Pay for Quality |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No human or animals were used in this research.
CONSENT FOR PUBLICATION
All patients participated on a voluntary basis and gave their informed consent.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors thank the reviewers for reviewing the manuscript.


