All published articles of this journal are available on ScienceDirect.
Dental Patient Management in the Context of the COVID-19 Pandemic: Current Literature Mini-Review
Abstract
Background:
Considering dental data gain associated with COVID-19 in the last few months of 2020, it is highly important to provide an assertive critical literature review with the categorization and systematization of available findings.
Objective:
The purpose of this article is to shed light on the concerns of dentists who provide treatment of children and adults during the pandemic of COVID-19.
Methods:
The search for relevant publications related to the objective topic was done via the Google Scholar engine with the use of next keywords: “dentistry”, “coronavirus”, “COVID-19”, “dental treatment”. All collected articles were processed using content-analysis principles with further systematization and categorization of obtained data in Microsoft Excel 2019 software (Microsoft Office, 2019).
Results:
Overview of trans-national guidelines considering COVID-19 prevention within dental care conditions could be categorized into the next few aspects: elective pattern of dental care, postpone dental treatment, screening algorithms through telecommunication and use of specialized PPE. Under the emergency mode of dental care, there are three basic P’s that should be considered during every dental procedure: patient’s self-care, prophylaxis and prioritization of pathology elimination approaches.
Conclusion:
Dentists should be fully informed and supported with CDC and WHO guidelines and recommendations, but also with national and regional legislation act related to control of dental care provision during COVID-19 epidemy. Changes in the general dental practice during the post-COVID era are inevitable, but those represent normal development and recovery of the dental field after pandemic mode.
1. INTRODUCTION
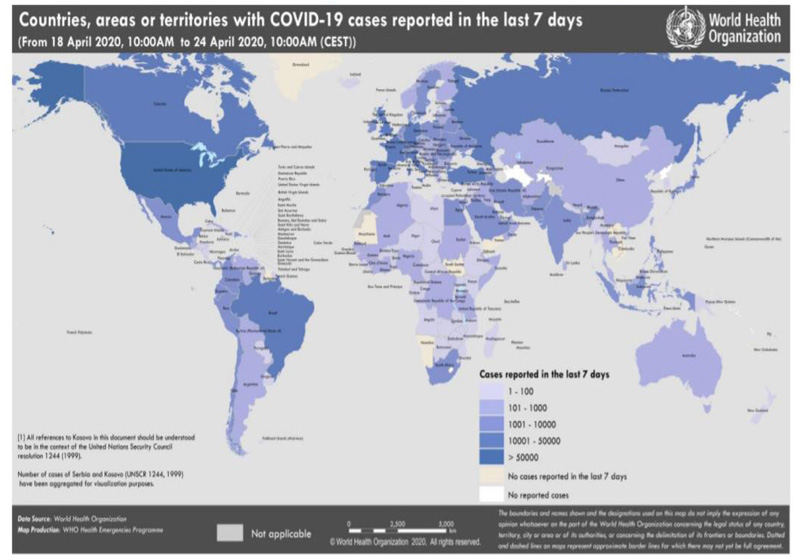
The novel coronavirus has been named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), whereas the disease associated with it is referred to as COVID-19. It has become one of the most important problems for the healthcare profession. According to the WHO situation report (April 24, 2020) update on COVID-19, there have been 2,626,321 confirmed cases and 181 938 deaths worldwide [1] (Fig. 1). In Ukraine, total confirmed cases 7647 and 193 deaths.
The dental practice is the focus of nosocomial infection, and care must be taken to minimize the risk of infection between dentists and patients. Due to the New York Times article considering the occupations that are at the greatest risk of coronavirus infection, dentists were represented as a category of health professionals with one the highest risk level [2]. COVID-19 risk score for the dental hygienists was equal to 997 for the dental assistants to 925 for the general dentists to 92,1 for the oral and maxillofacial surgeons to 923 [3].
The clinical characteristics of COVID-19 have not yet been fully established. The signs and symptoms include various stages, such as asymptomatic, mild, moderate, severe and critical [4, 5]. Most patients show symptoms, including dry cough, which is usually accompanied by fever, respiratory distress, rapid fatigue and other less common symptoms like the reduced sense of smell (hyposmia) and abnormal taste sensation (dysgeusia) [5, 6]. Pediatric patients with COVID-19 mostly owe to family cluster or with close contact history. Infected children have relatively milder clinical symptoms than infected adults [7]. As children may be asymptomatic or have mild, nonspecific symptoms, all patients and parents of children should be considered potential carriers of COVID-19 unless otherwise stated [8]. SARS-CoV-2 is highly transmissible; the incubation period can range from 0 to 24 days, therefore transmission can occur before any symptoms are apparent [1-5].
It is interesting to note that with the coronavirus pandemic situation, a quantity of articles related to the topic of dental care under the risk of specific viral infection influence has grown increasingly, even though the evidence grade of some of these publications remains discussible. Nevertheless, considering such dental data gain associated with COVID-19 in the last few months of 2020, it is highly important to provide an assertive critical literature review with the categorization and systematization of available findings.
2. OBJECTIVE
The purpose of this article is to shed light on the concerns of dentists who provide treatment of children and adults during the pandemic of COVID-19.
3. MATERIALS AND METHODS
The search of relevant publications related to the objective topic was done via Google Scholar engine with the use of next keywords: “dentistry”, “coronavirus”, “COVID-19”, “dental treatment” [9]. All collected articles were processed using content-analysis principles with further systematization and categorization of obtained data in Microsoft Excel 2019 software (Microsoft Office, 2019). Categories of content-analysis have formed analogically to the chosen keywords. Such analysis was held next way:
1. xls-spreadsheet was divided into five rows consisted of such categories as, “Bibliographical information about the article”, “Database, in which article was indexed”, “Relevant issue of COVID-19 pandemic dental aspects described in the article”, “Information about the same issue described in other articles (with bibliographical information of such)”, “Significant/unique information considering COVID-19 impact on dentistry stated in the analyzed article”;
2. Every filled cell in the row of “Information about the same issue described in other articles (with bibliographical information of such)” was marked by the color and grouped with other similar findings;
3. Units of analysis were formed from clusters of unique and repeated information considering dental aspects of COVID-19 pandemic;
4. Categorization of all the findings due to their unique or repeated features was held due to the text-mining and intellectual filter principles, which helped to systematize all the data provided in the sample of the analyzed article;
5. Interpretation of findings was held through their comparison with further contextual conclusions forming.
4. RESULTS AND DISCUSSIONS
Dentists should be familiar with how coronavirus is spread, how to identify patients with this infection, and what additional protective measures should be taken during practice to prevent transmission.
Even though the overall amount of patients attending dental offices was progressively decreased during the COVID-19 period, but among emergency patients, there was a trend of a higher quantity of oral infections during dental visits (raised from 51% during pre-COVID era up to 71,9% during COVID epidemy) [10]. Under the condition of a cross-sectional study, it was noted that despite the dentists’ awareness of transmission modes and symptoms of coronavirus infection, they were not fully informationally supported with perspectives of extra-precautions measures regarding dental clinical personnel and patients, respectively [11]. On the other hand, in the multinational study, authors had noted that dentists characterized with the “good knowledge and practice scores” considering all the aspects of COVID-19, but for further infection control, they are also advised to follow CDC and WHO recommendations and guidelines [12].
Dental procedures are mostly aerosol-generating procedures that are associated with the transmission of viral infections [10]. Previously it was described that COVID-19 disease can be transmitted through respiratory drops and sprays of saliva and blood through contact with mucous membranes and infected fumits [13]. Notably, a report of one case of 2019-nCoV infection in Germany indicates that transmission of the virus may also occur through contact with asymptomatic patients [14]. Moreover, there is new information coming considering salivary glands as potential accumulation depo of viruses [15].
Basically, there are four main routes of coronavirus infection spread within dental office conditions: 1) personal (direct) contact with different kind of respiratory secretions; 2) indirect contact with already exposed (contaminated) surfaces or instruments; 3) breath-in of viruses localized in airborne particles; 4) contact with aerosol enriched by virus via open mucosal surfaces of the body [16].
Dental units have a significant number of potentially contaminated surfaces, such as dental chairs, their handles, dental instruments after treatment, which is possible through transmission [10-12, 17, 18]. In the light of the COVID-19 pandemic situation, every surface in the dental office should be considered as potentially contaminated. Dental clinics should regularly observe universal precautions. They are crucial to avoid the transmission of the CoV-2 virus as well as transmission from infected patients to healthcare providers. Administrative measures, infection prevention training, dental clinic staff safety, hand hygiene, personal protective equipment, respiratory hygiene (cough etiquette), sterilization and disinfection of patient items and devices should be used [10, 11, 16-18]. Moreover, some literature sources reflect the need to provide disinfectants and masks for patients in the waiting room, while others prohibited the presence of more than one patient in the waiting room for a period of minimum 30 minutes after the last patient had left the office. The establishment of pre-check triages facilities is also considered as a preventive measure before patients visits to the dental clinic [10, 12, 16].
WHO has identified a pandemic as having six different phases [19]. Countries will be in different phases at different times, so universal guidance cannot be given for all at one time. Countries have taken various measures to provide dental care during a pandemic. For example, in the UK, all dental cases are handled by telephone and only receive basic treatment at designated centers. In Brazil, the National Health Agency recommended only emergency dental care, and all private clinics should stop treatment. In Brazil, the Ministry of Health has also introduced provisions for telehealth services to reduce the transmission of disease [20-24]. Telehealth systems have been implemented in the USА. Even if most countries limit dental care to emergency situations only, the recommendations differ between countries. Around the world, many primary and secondary dental services are suspended, and in many countries, telephone triadic identification systems are available for patients requiring immediate intervention [20-24].
Treatment should be provided only when local, regional and national guidelines are adhered to and, in the opinion of the dentist, safe for children, the patients who accompany them and the dentists. In this COVID-19 pandemic, universal infection control procedures are extremely important.
There are three levels of dental personnel protection during COVID-19 period: 1) primary or standard protection (for the staff within dental clinic condition); 2) secondary (advanced) protection (for dental professionals); 3) tertiary protection (highly advanced for the contact with suspected or already confirmed coronavirus infection) [25]. In February 2020, European Centre for Disease Prevention and Control had published universal guidelines for wearing and removing PPE (personal protective equipment) in the healthcare conditions while providing medical care or any other kind of medical services, including dental, for patients suspected of confirmed COVID-19 diagnosis [26].
International Federation of Endodontic Associations (IFEA) provided the following preparation checklist that needs to be reviewed before endodontic dental treatment during the COVID-19 pandemic: 1) is there is a practical need for providing dental treatment instead of trying to help the patient with some pharmacological approach?; 2) can the patient be managed while minimizing the need of aerosol-forming procedure or by some other options with excluding such risks; 3) does your dental care facility provided with all necessary PPE?; 4) can you guarantee consistency with all relevant established disinfection and sterilization protocols?; 5) do you know the algorithm for the COVID-19 case report?; 6) can you exclude all your previous personal experience that potential could be related with possible coronavirus infection [27]?
The most important thing is that all members of the dental team are responsible for their professional activities. In addition, dental teams should be familiar with treatment options that minimize or eliminate aerosol-generating procedures, many of which are based on modern karyology, well-established in the scientific literature, and minimally invasive in nature. It should also be borne in mind that pandemic experience and staging will vary geographically. The importance of brushing your teeth with fluoride toothpaste to prevent dental caries should continue to be emphasized when contacting patients [22]. Dentists should video consult with parents to promote positive behavior in the oral cavity.
Among different roentgenological techniques, the use of extraoral ones (orthopantomography or cone beamed computed tomography) is preferable during COVID-19, since those are not associated with the risk of possible cough or gag reflex development [28]. The use of rubber-dams, anti-retraction handpiece and high-volume saliva ejectors are also highly recommended, among other dental equipment [28].
The use of Ibuprofen not only in the pharmacological dental treatment algorithm but overall among somatically compromised patients should be avoided due to the possible side effect in the form of a negative immune system reaction [29]. Instead of Ibuprofen, WHO recommended the use of acetaminophen as alternative analgetics [28]. Brazilian research group recommended to restrict the use of inhalation sedation with nitrous oxide and pharmacological sedation with the aim of resolving some patients’ dental problems during coronavirus pandemic situation [30].
Peng X. et al. gave the recommendation: about working clothes extra disposable protective clothing outside, disposable doctor cap, protective goggles, face shield, disposable surgical mask, disposable latex gloves, and impermeable shoe cover should be worn [25]. A patient’s preprocedural mouth rinse with 1% hydrogen peroxide or 0.2% povidone, rubber dam, anti-retraction high-speed dental handpiece is strongly recommended also as an extra preventive measure for cross-infection [25].
Overview of trans-national guidelines considering COVID-19 prevention within dental care conditions could be categorized into the next few aspects: elective pattern of dental care, postpone dental treatment, screening algorithms through telecommunication, and use of specialized PPE [31] (Table 1).
Berlin-Broner Y. highlighted that in today’s epidemic conditions, dentistry is going through the changes in the hierarchy of needs. As he had stated under the emergency mode of dental care, there are three basic P’s that should be considered during every dental procedure: patient’s self-care, prophylaxis, and prioritization of pathology elimination approaches [32]. Marwaha et al. had systematized all the safety and preventive measures considering dental care in the COVID era into the next 5 principles: identification, infection control, self-protection, postpone elective dental manipulations, pharmacological management [28].
| Risk of exposure to COVID-19 infection during dental diagnostics and treatment | Countermeasures |
| Avoiding dental visits except those that need emergence care provisions; postponed dental treatment | |
| Providing consultation and diagnostics through a teledentistry/telephone (remote) approach | |
| Scheduled patients’ visits with only one patient present in the waiting room and forming 30 minutes gap between patients to provide all the disinfection measures | |
| Disinfectants and mask for patients in the waiting room | |
| Decontamination of all dental instruments and dental units with sufficient exposure time after each patient | |
| Full PPE-set use by dental professionals | |
| Relevant disinfection and sterilization protocols within the dental office | |
| Preprocedural mouth rinse for patients | |
| Rubber dam, anti-retraction high-speed dental handpiece use |
Logically that such critical changes in the dental field will influence the financial and economical pattern of the sector. Due to the information provided by the Health Policy Institute (American Dental Association), there are at least 4 different scenarios of dental sector recovery after COVID-19 epidemy. Nevertheless, it should be mentioned that in the USA, the amount of dental care spending could be reduced up to 66% in 2020 and up to 32% in 2021 [33]. Nearly 38% of lesser patients had attended dental office during the COVID-19 period comparing to the period of one month before epidemy started [10]. From the one side, the episodical use of additional protective equipment is associated with the greater cost of provided dental services, while retention and support of such «non-contagious» dental office conditions demand continuous perspective changes in the whole dental care economy sector. Contrarily dentistry as any other economical fiend is in need of financial support right now for its further normal functioning and development. Retrospectively it seems consistent that crossing of such pandemic burden associated with further redistribution of financial, economical and material values.
CONCLUSION
High importance should be considered to the early recognition, diagnosis, and treatment of children and adults infected by COVID-19, but the primary task of the dentist relies on the disruption of coronavirus spread routes within dental office conditions. Dentists should be fully informed and supported with CDC and WHO guidelines and recommendations, but also with national and regional legislation act related to control of dental care provision during COVID-19 epidemy. Changes in the general dental practice during the post-COVID era are inevitable, but those represent normal development and recovery of the dental field after pandemic mode.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
The study was not funded by any research grant or other sources of financial support.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


