All published articles of this journal are available on ScienceDirect.
The Connection between Health Promotion, Prevention, and Psychosocial Health: An Innovative Action Model
Abstract
The promotion of psychosocial health among individuals, groups, and society is becoming an increasingly important task and research topic in the field of public health. Psychosocial health is a complex interaction between the psyche of an individual and the social environment in which that individual lives. Promoting psychosocial health is often challenging and complex for health care professionals. Therefore, an important question of public health significance is: how can we address and improve the psychosocial health of individuals, groups, as well as society in general?
An interdisciplinary team of specialists at the Department of Health Professions at the Bern University of Applied Sciences, Switzerland, focused on the connection between health promotion, prevention, and psychosocial health. This team newly defined these topics in relation to how they could be synergistically combined to promote psychosocial health. Additionally, they presented an action model to graphically depict their connection.
The proposed action model is based upon already well-established concepts, models, frameworks in health promotion, and prevention practice. In a further step, they have depicted them in a way that clearly integrates and combines their core concepts for their practical application in promoting psychosocial health. As these topics are overlapping, their clear illustration is important in promoting their systematic and planned usage.
This new and innovative approach encourages the systematic usage of health promotion and prevention for the promotion of psychosocial health. The next step would be the implementation and evaluation of this action model, especially the measurement of the outcome (psychosocial health). The integrative and intentional use of health promotion and prevention is an innovative approach for the promotion of psychosocial health in public health practice.
1. INTRODUCTION
The promotion of psychosocial health among individuals, groups, and society, is becoming an increasingly important task and research topic in the field of public health. Issues potentially affecting one’s psychosocial health include, for example, workload and competition at work, demanding family life, rising health care costs, along with social inequality and insecurity [1]. Psychosocial health is a complex interaction between the psyche of an individual and the social environment in which a person lives [2, 3]. See video (Definition of psychosocial health) in the Supportive/Supplementary Material section of this article. A number of factors that have a major impact on the health of individuals/groups are social in nature. For instance, the neighborhood in which one lives, a change in occupation, or having to migrate to a new country could all have an impact on one’s health. These factors are often out of an individuals’ direct control; however, they can either positively or negatively affect one's health. Promoting psychosocial health is often challenging and complex [4]. Therefore, an important question of public health significance is: how can we address and improve the psychosocial health of individuals, groups, as well as society in general? Healthcare professionals and public health authorities can positively influence the psychosocial health of individuals, groups, and communities who they are supporting.
2. MAIN TEXT
An interdisciplinary team of specialists at the Department of Health Professions at the Bern University of Applied Sciences, Switzerland, focused on the connection between health promotion, prevention, and psychosocial health. This team newly defined these topics in relation to how they could be synergistically combined to promote psychosocial health. A practical E-learning program was developed to promote their integration at this university. In this article, these newly established definitions, as well as an action model, will be introduced.
2.1. Definitions
The proposed definitions (Table 1) delineate that health promotion and prevention can be distinguished conceptually, as their approaches to health and illness differ from one another. While health promotion aims at improving/promoting health and resources (salutogenesis), prevention focuses on avoiding disease and its associated risk factors. In practice, however, health promotion and prevention often have the same goal, which is to improve or maintain the health and health competencies of the population. Consequently, they have been combined in the targeting of psychosocial health. Health promotion focuses on strengthening the personal resources of individuals and groups as well as improving the resources present in the social environment. Primary prevention targets detecting and reducing the risk of an illness from occurring (e.g. from unhealthy behavior or detrimental environments). Secondary and tertiary prevention focus their interventions on reducing the negative consequences of symptoms or diseases. The aim of quaternary prevention is the identification of patients’ risk for over-medicalization. Primordial prevention focuses on the avoidance of the development of risk factors, which have not yet occurred (e.g. early childhood health programs to avoid disease later in life). The combined support of health promotion and prevention positively impacts the psychosocial health of individuals, groups, and societies.
| Definition of Psychosocial Health for Health Professions (Condensed Version) |
|
The psychosocial health of an individual varies over time. It can be thought of as being on a continuum between psychosocially healthy and ill. It encompasses an individual’s experience, perception, psychological/mental processes, behaviour, as well as lifestyle.
It has a reciprocally associated relationship to one’s social context and relationships (family, friends, co-workers, etc). Additionally, it is influenced by social structures (society, etc.). The body along with consciousness, are regarded as prerequisites for being able to interact with the social environment. They are necessary to exist in a social context and to express oneself through behaviour. Psychosocial health varies over time (e.g. different phases of life / life events) and can be strengthened through resources and support (emotional support, own relational abilities). It can also be weakened by risks and stressors (e.g. work-related stress). The locus of psychosocial health is clearly placed upon the individual. |
| *This definition of psychosocial health is based upon a concept analysis, which is being submitted to a scientific, peer-reviewed journal in 2021. Also, see video based upon this concept analysis: Definition of psychosocial health (in the Supportive/Supplementary Material section of this article). |
| Definition of Health Promotion for Health Professions |
|
Health promotion supports the process that enables and increases peoples’ self-determination and control over their health. Health promotion improves the personal and social conditions necessary for health.
Based upon the Salutogenic Model from Antonovsky (1979), health and illness move along a continuum. They are also influenced by one’s social, personal and physical resources. This is a paradigm shift in contrast to the biomedical model (pathogenesis), which instead focuses on disease. Salutogenesis thus investigates what keeps people healthy, rather than what makes them ill. Cooperation between various political policies and healthcare sectors is a prerequisite for the promotion of the health throughout society (WHO, 1998). These sectors are required to advocate for health and equal opportunities, and to enable and support the various health interests of society through mediation and advocacy (WHO, 1986). |
| Definition of Prevention for Health Professions |
|
The goals of disease prevention are to avoid of the development of risk factors, which have not yet occurred (primordial prevention), and to reduce the risk factors, occurrence and spread of disease (primary prevention). Additionally, early detection is intended to reduce the incidence of diseases (secondary prevention). Chronic diseases should be targeted as early as possible, to prevent subsequent damage or relapses (tertiary prevention). Identification of patients’ risk for over-medicalization (quaternary prevention) is important for both the patient and the healthcare system. Preventive interventions can focus on individuals, groups, as well as the societal level (Green & Tones, 2010). Along with the focus of prevention at the societal level, a person-centered approach is also of importance. An essential component is this approach is patient education. It is vital that preventive interventions be planned and implemented with patients, along with their families. |
| The relationship between Health Promotion and Prevention |
|
Health promotion and prevention can be distinguished conceptually, as their approaches to health and illness differ from one another.
Health promotion emphasizes a positive and holistic view of health (Tengland, 2009). In addition to focusing on a generally healthy population, its strategies also target vulnerable or at-risk groups. This denotes planning and implementing interventions that focus on the social and economic determinants of health (Tengland, 2009). In contrast, preventative measures focus mainly on specific diseases. They aim to either prevent them from occurring, to reduce their risk, to detect them at an early stage, or to reduce their consequences (Tengland, 2009). Health promotion strategies generally have a broader scope and target group. They tend to have a bottom-up or participatory approach, while prevention strategies often have a top-down approach (Tengland, 2009). In practice, however, Health promotion and prevention often have the same goal, which is to improve or maintain the health and health competencies of the population. Therefore, both measures are necessary to achieve this goal. |
| The relationship between Psychosocial Health, Health Promotion and Prevention |
|
Health promotion aims to strengthen the personal resources of individuals and to support them. It also aims to reinforce the resources and opportunities present in the social environment. Health promotion can reinforce the relationship between individuals and their social environment (social formations and structures). This is crucial for psychosocial health.
Health promotion focuses its interventions at the group, organizational, community and societal levels. It mainly aims to improve the social determinants of health. This indirectly positively impacts the psychosocial health of individuals. The social environment (work environment) can also be targeted, thus supporting psychosocial health. Primary prevention activities support the psychosocial health of individuals, by focusing on reducing the risk of illness associated with unhealthy behavior/lifestyles and health hazards. Secondary and tertiary prevention measures support the psychosocial health of individuals via treating/improving the disease/symptoms, or through supporting individuals with chronic diseases. Quaternary prevention supports the psychosocial health of individuals by identifying their risk for over-medicalization. |
| © Bern University of Applied Sciences, Switzerland, 2020 |
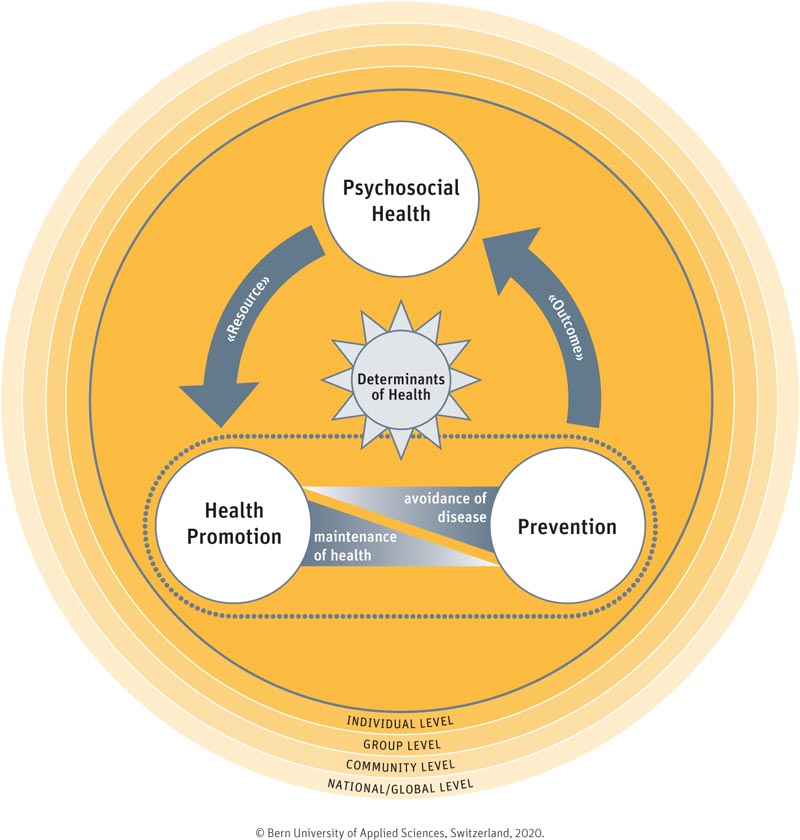
2.2. Action Model
In order to depict how health promotion and prevention could be systematically utilized to promote the psychosocial health of individuals, groups, and society, a novel action model was developed (Fig. 1). This action model is designed to guide health professionals and authorities in promoting psychosocial health amongst their target groups. In this graphic, health promotion and prevention are encircled together with a dotted line, which depicts that they are meant to be utilized jointly. Situated between health promotion and prevention are two grey triangles. They represent the interdependence that salutogenesis has with health promotion and prevention. The triangle connected to health promotion illustrates that it focuses on what makes people healthy; whereas, the triangle connected to prevention symbolizes that it focuses on avoiding what makes them ill.
The sun-like symbol in the middle of the graphic depicts the significance and interconnectedness that the Determinants of Health have in relation to health promotion, prevention, and psychosocial health. The Determinants of Health are often social in nature, and therefore, impact the health of all individuals living in the surrounding environment [5]. Examples of the social Determinants of Health include the physical environment, social network, education and health literacy, employment opportunities, and the healthcare system [6]. Thus, improvement in these social determinants of health are a key focus of health promotion and prevention strategies. The circles surrounding the graphic portray how this action model can be utilized at all population health levels (individual, group, community, global).
The arrow with “outcome” written inside is the “action” part of the model. It depicts how health promotion and prevention actions, strategies, models, etc., can be used to promote psychosocial health. Thus, the improved psychosocial health of individuals, groups, etc., is seen as an outcome. The arrow with “resource” written inside represents that if an individual has adequate resources (through her/himself and her/his environment) and sufficient psychosocial health, it is likely that she/he will be more motivated and able to maintain health and to avoid illness. Importantly, a lack of resources may make it more difficult to undertake health-promoting or preventive measures.
The proposed action model is based upon already well-established concepts, models and frameworks in health promotion and prevention practice. In a further step, we have depicted them in a way that clearly integrates and combines their core concepts for their practical application in promoting psychosocial health. As there is a lot of overlap present among these topics, this clear illustration is important to promote their systematic and planned usage. It will now be highlighted in more detail how this action model is intended to be applied (Fig. 2).
2.3. Core Concepts Essential to Health Promotion
Ottawa Charter: A key component in health promotion practice is the advocating, enabling, and mediating action strategies delineated in the Ottawa Charter: developing personal skills, strengthening community action, creating supportive environments, reorienting health services, and building healthy public policy [7]. Additionally, there are specific principles that guide health promotion practice. The principles of participation, empowerment, and a holistic and positive conceptualization of health, are the basis for the relationship which will be formed between the health professional and the individual/group [8,9]. Other health promotion principles, such as advocacy and social justice and equity in health [10], reflect that the health professional is focused upon reducing inequities in health. The remaining principles, such as intersectoral collaboration, building upon existing strategies, and usage of multiple strategies, guide health professionals in the broadening and systematic usage of their targeted interventions/projects [11]. The use of a settings approach, which denotes taking action in the settings in which everyday life takes place (e.g. workplace, schools, hospitals, cities, etc.), is also core to health promotion strategies [12]. There is a specific focus on the organizational structures and systems within the settings approach, as these affect the health of all involved individuals. The settings approach is also connected with an ecological model of health promotion, as it acknowledges that health is “determined by a complex interplay of environmental, organizational and personal factors” (Dooris, 2006, p. 55).
2.4. Core Concepts Essential to Prevention
Differentiated usage of the five main types of prevention (primordial, primary, secondary, tertiary, quaternary (see previous description) are important in the development of strategies/interventions /projects, as they target different persons/groups at varying stages of health/disease [13]. Prevention strategies can either focus directly on the behavior of individuals/groups/society (e.g., with information & education), or they can target the structure which indirectly affects behavior. Structural (environmental) prevention measures enable health-promoting behaviors and deter potentially hazardous behaviors, by making them more difficult to engage in. Examples of such structures are the built environment (sidewalks, green space, bike paths) or legislation /policies (food composition and labeling, advertisement, seatbelt legislation) [14, 15].
2.5. Usage of Health Promotion and Prevention to Impact Psychosocial Health (As An Outcome)
There are numerous, more specific models and frameworks which guide health professionals in planning and implementing interventions/projects/ programs. Family-centered Care [16], Theory of Planned Behavior [17, 18], Transtheoretical Model of Behavioral Change [19, 20] and Self-efficacy [21-24], are examples of more focused models, which, in addition to the broader, core concepts of health promotion and prevention, offer more specific guidance to health professionals. Models, such as the Integrated Model of Population Health Promotion Model [25], the Public Health Action Cycle [26], and the Precede-Proceed Model [27, 28], are tools that can be utilized during project/program planning to ensure more systematic usage of health promotion and prevention.
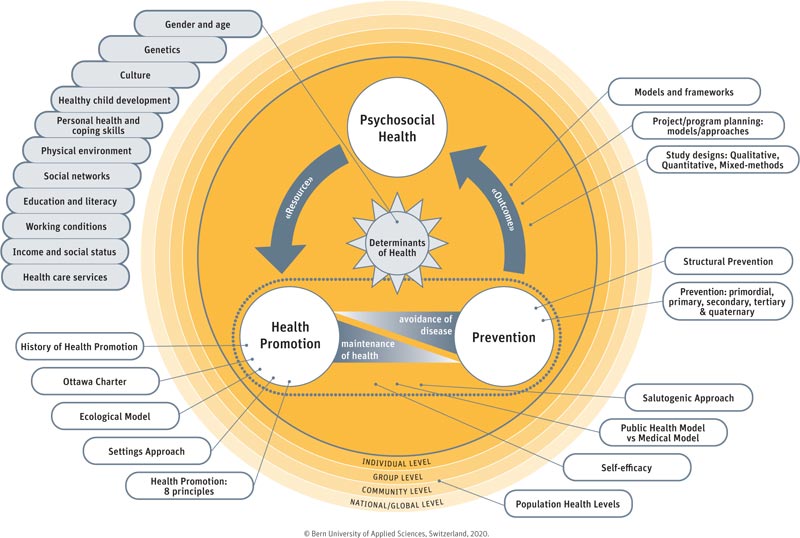
It is also important to integrate more general, public health-related concepts when introducing change among various population health levels. Integration of constructs, such as epidemiology, ethics in public health, healthcare systems, and policies, along with study design (quantitative, qualitative or mixed methods), is also important when planning interventions/projects/programs in health promotion and prevention.
2.6. Conceptualization of the Action Model
The definitions and action model are based upon core aspects from health promotion and prevention practice, along with expert knowledge from an interdisciplinary team of specialists. To the authors’ knowledge, such an action model does not exist in the international literature. This new and innovative approach encourages the systematic usage of health promotion and prevention in the promotion of psychosocial health. The next step would be the implementation and evaluation of this action model, especially the measurement of the outcome (psychosocial health).
CONCLUSION
The integrative and intentional use of health promotion and prevention is an innovative approach for the promotion of psychosocial health in public health practice. The proposed action model guides health professionals in utilizing health promotion and prevention to promote psychosocial health among their target groups. Internationally, such a model does not exist. Therefore, it offers a new and systematic approach to promote psychosocial health among various population health levels.
SUPPORTIVE/SUPPLEMENTARY INFORMATION
Video: Definition of Psychosocial Health
Peter, K.A., Golz, C., Hahn, S. & Richter, D. (2018). Definition of Psychosocial Health. Bern University of Applied Sciences, Department of Health Professions: Bern, Switzerland. Video. https://www.youtube.com/watch? v=0_0olJf-1H0&feature=youtu.be
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
This work was financially supported (non-grant) by Bern University of Applied Sciences (through the SALUTE Project), Bern, Switzerland.
CONFLICTS OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


