All published articles of this journal are available on ScienceDirect.
Change in Orthopedic Trauma Practice under Strict Lockdown due to COVID-19 Pandemic
Abstract
Introduction:
The COVID-19 pandemic has led to remarkable changes in several aspects of medical practice. Elective surgeries, including orthopedic surgery, were deferred worldwide, allowing hospitals to accommodate higher numbers of COVID-19 patients and reduce the possible risk of infection among healthcare workers. However, healthcare systems aimed to continue providing emergency services at similar standards. In this study, we aim to highlight the impact of lockdowns secondary to the pandemic on orthopedic trauma practice in a country that was described to have one of the strictest lockdowns worldwide. We aim to examine the trends of change in number and type of orthopedic trauma cases and the changes to decision making and patient care among orthopedic surgeons.
Methods:
This cross-sectional study is based on a survey that was designed and delivered to orthopedic surgeons from different health sectors i.e. governmental, military, private and university hospitals. The questionnaire was distributed through the official Jordan orthopedic association WhatsApp group by the end of the 4th week of strict lockdown. A total of 256 orthopedic surgeons were invited to participate and responses were limited to one per participant. 147 replies were received with a response rate of 57.4%. Data were analyzed using the Statistical Package for the Social Sciences Version 23 (SPSS Inc., Chicago, IL) statistical software.
Results:
A total of 147 surgeons participated in the study with a response rate of 57.4%. The mean age of the participants was 39.8 years, with the majority being between 30 and 40 years (n=70; 48%). There was a significant decline in the number of trauma cases admitted to the Emergency Departments (ER), especially cases with polytrauma. During this period, the most common reported fractures were proximal femur fractures (47.6%) followed by distal radius fracture (17%). 30% of participants used to perform more than 10 trauma operations per week. This percentage dropped to 7.5% during the pandemic lockdown. 25% did not operate at all during the lockdown period. Outpatients practice was significantly affected with almost 40% of orthopedic surgeons not managing any single patient. Regarding the use of Personal Protective Equipment (PPE), 85% of the surgeons used face masks and gloves only during their patient's encounter. Inside the operating room, only 9.5% of surgeons used fully protective PPEs. Regarding the changes in practice, 62% of surgeons reported an increased tendency toward non-operative management with a significant delay in follow up of patients. The use of telemedicine was effective in the management of less than 50% of patient encounters, according to our participants. Private practice respondents reported more than 50% drop in their income during the lockdown.
Conclusion:
Strict lockdown in Jordan led to significant changes to orthopedic trauma practice in terms of the number and type of cases. Emergency and outpatient services were similarly affected. Orthopedic surgeons developed a tendency towards more conservative management and less surgical treatment. There is a need for stricter implementation of guidelines regarding the use of PPE especially in the operating theatre. Telemedicine use in management and follow up of trauma patients needs further assessment in terms of its efficacy and efficiency to patients and to healthcare professionalswith regards to its medico-legal aspects.
1. INTRODUCTION
Trauma is a major cause of morbidity and mortality worldwide and has a very significant impact on the health systems and the economies of developing countries [1, 2]. Road Traffic Accidents (RTAs) for example, are one of the leading causes of fatality each year. Orthopedic trauma, in particular, has a significant burden in terms of capacity and finances on these already exhausted healthcare systems [3]. In Jordan- a country of 10 million populations and with a GDP of almost 4000 USD per capita-4% of fatalities results from RTAs according to CDC report [4]; this is considered as one of the highest worldwide.
Jordan reported its first novel coronavirus (COVID 19) case on March 2nd 2020, [4]. Since then, the Jordanian Government started an early response with aggressive measures and legislations to force social distancing. Schools and universities were shut as early as March 14th, 2020 heading to a total lockdown and curfew on March 21st, 2020. This is considered as one of the strictest measures worldwide at this early stage of the pandemic [5]. This led to a cessation of all non-emergency health services, including outpatient clinics and elective surgeries. This strict lockdown lasted until the end of April when non-emergency medical services started to re-open gradually.
Orthopedic trauma surgery in Jordan is considered a well-established surgical specialty. Because of momentous changes that have been observed in response to this pandemic related lockdown, we tried to evaluate the effects of this strict lockdown on orthopedic trauma practice in terms of changes in number and type of cases, changes in the behavior of the care givers in aspects of self-protection, patient confrontation and decision making. We finally tried to identify possible consequences on the standards of orthopedic patients' care.
2. MATERIALS AND METHODS
This cross-sectional study is based on a survey that was designed and delivered to orthopedic surgeons from different health sectors i.e. governmental, military, and private and university hospitals. The questionnaire was distributed through the official Jordan orthopedic association WhatsApp group by the end of the 4th week of strict lockdown. A total of 256 orthopedic surgeons were invited to participate. The responses were limited to one per participant. A total of 147 surgeons have participated in the study, with a response rate of 57.4%.
A self-administered online questionnaire of 32 questions was sent to the group and was composed of three sections; 1) general information about the practitioner, 2) orthopedic trauma practice and personal protection behavior and 3) patients’ follow up and care (Appendix A).
Objectives and goals were explained at the beginning of the questionnaire to all participants. This study aimed to examine trends of change in the number and type of orthopedic trauma cases and alterations to decision making and patient care among orthopedic surgeons. Retired surgeons and practitioners working outside Jordan at the time of lockdown were excluded.
Data were analyzed using the Statistical Package for the Social Sciences Version 23 (SPSS Inc., Chicago, IL) statistical software. The analyses included descriptive statistics and Chi-square test. A significance level of 5% (P ≤ 0.05) was considered statistically significant.
3. RESULTS
A total of 147 orthopedic surgeons participated in this study, with a mean age of 39.8 years +/- 9.6 years. Majority of participants (n=70; 48%) were in the age group (30-40 years) followed by the age group (41 – 50) (n=42; 28%). Participants were distributed between different sectors i.e. public 33%, private 30%, military 24%, and 13% in both private and public sectors. Other demographic variables and characteristics of participants are summarized in Table 1.
| Category | Variable | Number (%) |
|---|---|---|
| Age | ||
| < 30 years | 12 (8%) | |
| 30 - 40 | 70 (48%) | |
| 41 - 50 | 42 (28%) | |
| 51 - 60 | 13 (9%) | |
| 61 - 70 | 10 (7%) | |
| Marital status | ||
| Single | 18 (12%) | |
| Married | 129 (88%) | |
| Type of practice | ||
| Public sector alone | 49 (33%) | |
| Private sector alone | 44 (30%) | |
| Military sector | 35 (24%) | |
| Private and public sectors | 19 (13%) | |
| Academic position | ||
| Resident | 38 (26%) | |
| Fellow | 2 (1%) | |
| Specialist (1-10 years' experience) | 62 (42%) | |
| Consultant (>10 years' experience) | 45 (31%) | |
| Clinical experience | ||
| 1-5 years | 71 (48%) | |
| 6-10 years | 30 (20%) | |
| 11-15 years | 20 (14%) | |
| >15 years | 26 (18%) | |
| Medical co-morbidities | ||
| None | 117 (80%) | |
| One co-morbid condition | 22 (15%) | |
| 2 co-morbid conditions | 6 (4%) | |
| 3 or more comorbidities | 2 (1%) | |
| Smoking | ||
| No | 69 (47%) | |
| Yes | 78 (53%) |
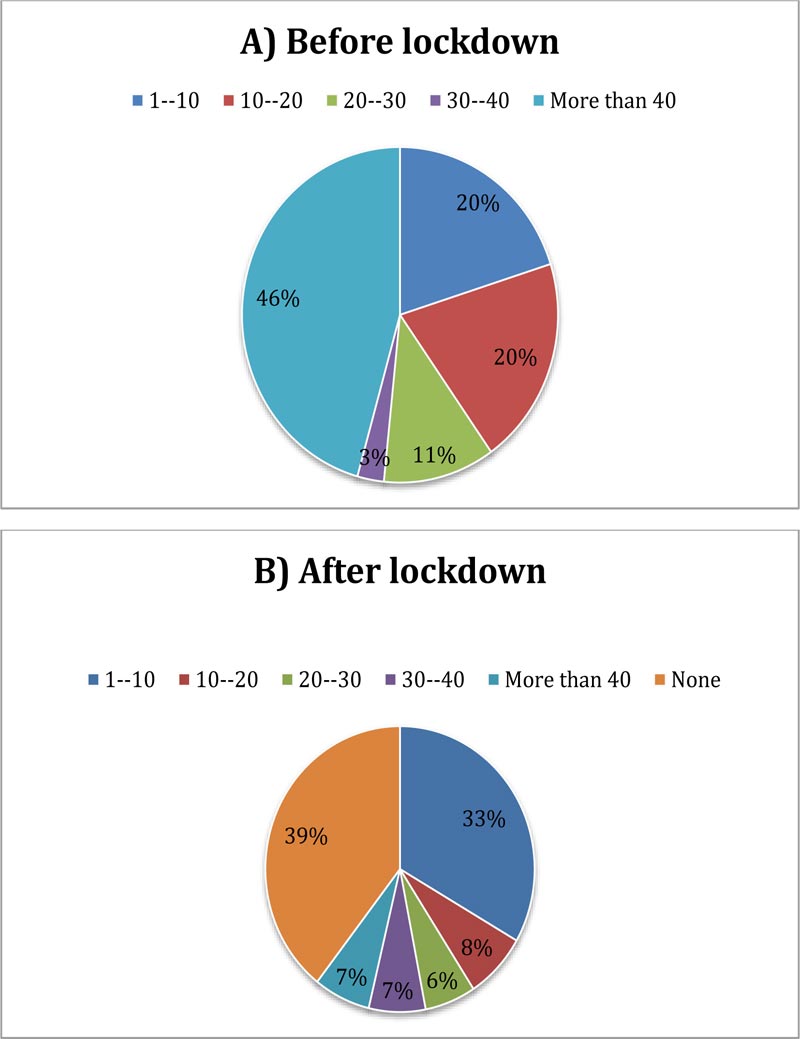
Regarding changes in orthopedic trauma burden, 67 of the entrants (45.6%) used to treat more than 20 trauma cases in ER per week in the era before the lockdown, but this figure dropped to 20 (13.6%) after the lockdown. 17.7% of participants did not treat a single patient in ER during the same period (Fig. 1).
The percentage of complex injuries and poly trauma markedly decreased during the lockdown. Before the lock down, complex trauma constituted a significant proportion (>10%) of practice for three quarters of our participants. However, only 20% of surgeons reported the same proportion after the lockdown. 30% of participants used to perform more than 10 trauma surgeries per week and this ratio dropped to 7.5% during the lockdown. 25% of surgeons did not operate at all during this period.
The most common fracture reported was proximal femur fractures (47.6%), followed by distal radius (17%). In general, practitioners reflected that most ER cases were not true emergencies. There was a significant decline in the number of outpatient cases. Before lockdown, 46% of practitioners used to treat more than 40 patients per week compared to only 7% of participants seeing the same number during the lockdown. Almost 40% did not manage any patients during the same period (Fig. 2).

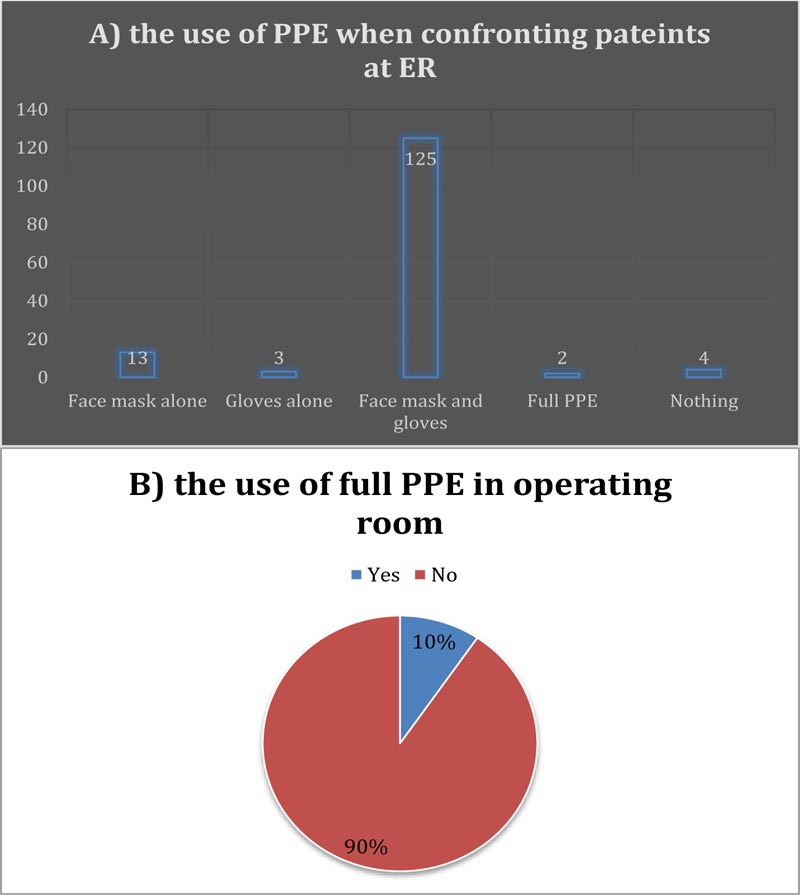
Regarding the personal attitude toward the use of PPEs, 125 participants (85%) used both face mask and gloves during their ER encounters, while 2.7% used no PPEs at all. Surprisingly, only 9.5% of participants used full PPEs, including face shields or goggles, while performing surgeries inside the operating room (Fig. 3).
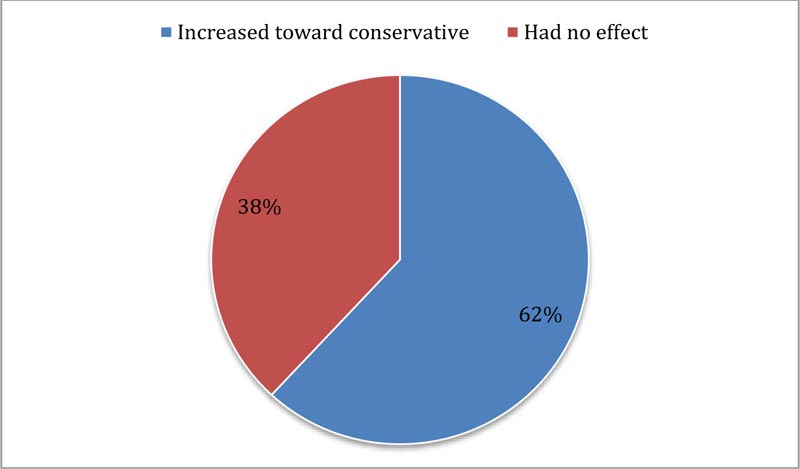
Patient care and follow up were also affected by the lockdown, as reported by the participants. 62% of surgeons reported that the pandemic increased their tendency in decision making toward non-operative management (Fig. 4). This was studied in correlation to their age, seniority level, sector of practice, medical comorbidities and marital status. Age and Seniority level only were found to be significantly correlated with the change in decision making (P= 0.01 and 0.03respectively); consultants showed more tendency toward non-operative management compared to residents and junior specialists (Table 2) 40.8% of participants reported a delay in following up their patients due to the lockdown restrictions and 15.6% reported that followup appointments were missed. Most of the care providers responded that the use of telemedicine helped in solving patients’ problems but that it was helpful in less than 50% of cases.
| Group Statistics | ||||||
|---|---|---|---|---|---|---|
| Decision-making | N | Mean | Std. Deviation | Std. Error Mean | Sig. (2-tailed) P value | |
| Position | toward conservative | 91 | 2.62 | 1.190 | .125 | .030 |
| No change | 56 | 3.04 | 1.026 | .137 | ||
| Age | toward conservative | 91 | 38.46 | 9.363 | .982 | .033 |
| No change | 56 | 41.93 | 9.733 | 1.301 | ||
| Post-board experience | toward conservative | 91 | 1.90 | 1.126 | .118 | .134 |
| No change | 56 | 2.20 | 1.197 | .160 | ||
| Morbidities | toward conservative | 91 | 1.23 | .559 | .059 | .291 |
| No change | 56 | 1.34 | .668 | .089 | ||
| Smoker | toward conservative | 91 | 1.51 | .503 | .053 | .440 |
| No change | 56 | 1.57 | .499 | .067 | ||
| Marital | toward conservative | 91 | 1.11 | .314 | .033 | .530 |
| No change | 55 | 1.15 | .356 | .048 | ||
| Type | toward conservative | 91 | 2.10 | 1.055 | .111 | .065 |
| No change | 56 | 2.43 | 1.024 | .137 | ||
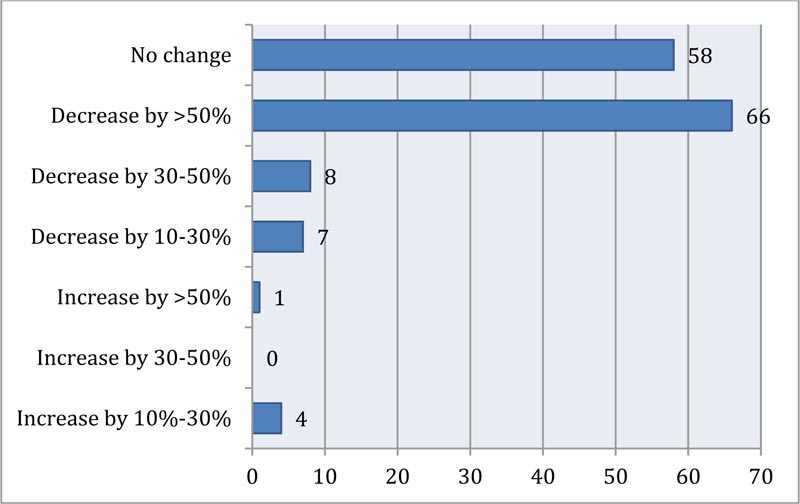
Finally, a question about changes to surgeons' income outlined that self-employed private practice participants were hit hard by the pandemic with a reduction of more than 50% in their income (P= 0.01) compared to public practice participants who were not affected at all as they were on fixed payroll by their institutions (Fig. 5).
4. DISCUSSION
The COVID-19 pandemic-which was declared by WHO on March 11th 2020, led to conspicuous global reaction to the novel viral disease. This reaction was inconstant and incon- sistent between different countries; varying from mild closure of economic activities and public services with recomm- endations for social distancing to strict lockdowns with comp- lete curfews hindering people mobility and ceasing most of economic activities. These ‘non-essential activities’ included non-emergency medical services in many countries [6-9]. Elective surgeries were deferred worldwide, allowing hospitals to accommodate higher numbers of COVID-19 patients and to reduce the risk of cross infection among healthcare workers [8, 9].
Orthopedic trauma, a never stopping problem, has been affected in many ways during this rampant viral disease. Globally, it has been estimated that the cancellation rate for orthopedic surgery was 82% [10]. A study from Wuhan (China), the epicenter of the pandemic, investigated the effects of the disease on orthopedic practitioners. A total of 26 orthopedic surgeons from 8 hospitals in Wuhan were identified as having COVID-19; they studied the different variables associated with the risk of contracting the infection and discussed protection policies and practices. Participation in real-time training on prevention measures was found to have a protective effect against COVID-19. Not wearing an N95 respirator was found to be a risk factor [6].
In another interesting paper discussing how orthopedic surgeons in China were coping with the pandemic, the author divided the response into three phases: 1) the initial phase was when the information about the pandemic was scarce. During this phase, the operation of medical and surgical services was unaltered and ran as usual. 2) The second phase started with the implementation of a strict lockdown after the severity and danger of the COVID 19 became clear. In this phase, protocols for emergency admissions were instituted with aggressive measures of patient testing. All orthopedic surgeons were placed on ‘back-up’ for any possible need to treat COVID 19 patients. Elective surgeries were all canceled. 3) The third phase started with the reopening the country’s facilities with a full alert to possible relapse. Specific and stratified protocols were set for both emergency and outpatient admissions depending on patient evaluation; this included history of fever, PCR test and lung CT scans. These protocols were extended to include how surgeons should deal with patients in the operating room with different level of restrictions from routine to restricted levels [7].
A paper from Italy; Europe’s hardest hit country in the first three months of the pandemic, described the practice during that period. Non-emergency orthopedic surgeries were all cancelled in Lombardy in the first three months. Patients with traumatic injuries in need of surgery and who were suspected of having the COVID19 infection were instructed to wait in emergency rooms until definitive results of coronavirus tests were done and ready [8].
In another orthopedic department in Padova Italy, significant restrictions were implemented, leading to an overall reduction of all surgical activities by 30% compared to 2019. They also had a reduction in outpatient clinic activities and admissions to the orthopedic emergency unit. In their study, they stated that ‘extensive swab testing’ has proven successful; out of 160 people tested in their department, only three COVID-19 positives were found. And out of 200 patients undergoing surgical procedures, only two positive patients were found, they concluded that Extensive swab test of all people (even if asymptomatic) and proactive tracing and quarantining of potential COVID-19 positive patients may diminish the virus spread [9].
The Jordanian Government reacted aggressively to the pandemic after reporting the first case early in March. This reaction escalated quickly to a complete lockdown by the third week of March. This was described as one of the strictest worldwide [5]. The curfew had its effects on all branches of medical practice as all outpatient services and elective procedures were canceled, limiting practice to emergency cases only. The idea was to shift the focus and efforts to handling the rapidly sweeping pandemic to avoid overwhelming the healthcare system in this small country with limited resources.
In this study, we examined the changes in orthopedic trauma practice in terms of quantity and type of cases, and the practitioner’s behavior toward self and patient protection, decision making and follow up of patients (Appendix A). We gathered information regarding changes to orthopedic practice from the people who actually provide the service. The information-at times- had to be gathered as trends rather than absolute numbers due to difficulty in obtaining accurate data and statistics from hospitals and medical practices during these extraordinary circumstances.
Medical practice in Jordan is divided into three major sectors: public, military and private practice. A small percentage of practitioners work in both public and private practices. We received a good variety of replies from all different sectors and from different levels of seniority ranging from residents to consultants. The analysis showed that the orthopedic surgery body in Jordan is relatively young with a mean age of 39.8 years. The majority had no chronic medical conditions with a high prevalence of smokers among the group, reflecting- as expected- the high percentage of smokers among the Jordanian population in general [11].
As it could be speculated from a very strict lockdown, the results showed a significant reduction in orthopedic trauma cases seen in Emergency departments. The percentage of practitioners who were treating more than 20 patients per week dropped to less than a third. 17.7% of participants did not treat any patient during the lockdown. The number of trauma surgeries also showed a notable reduction with one quarter of surgeons not performing any operation during one month of lockdown. The most common injury reported was proximal femur fracture (47.6%), which is the most common fracture in people aged above 65 [12]. But in a country with only 3% of its population above 65 years of age, this represents a change in trauma incidence and type secondary to the lockdown. The same can be concluded from the decrease in reporting of distal radius fractures (17%), rated second most common fracture in our study, while many studies put distal radius fracture on the top of incidence rate in Jordan [12, 13].
In a similar study, evaluating the impact of COVID 19 on orthopedic practice in a hot spot in India, results show more than 75% decline in outpatient cases reported by about half of the participants. There was also a significant decline in the number of elective surgeries performed, especially arthroplasty and spinal surgeries. Participants in the study reported strict adherence to PPE use and no one of the participants contracted COVID 19 during the study period. Telemedicine was used by the participants in this study; patients were found to prefer video calls over other social media applications like WhatsApp [14].
A paper from turkey elaborated on changes in the management of pediatric orthopedic cases. A survey completed by pediatric orthopedic surgeons showed significant effects on their practices. There was a significant reduction in outpatient referrals (75%). None of the participants did any elective surgeries during the early pandemic period of March and April [15].
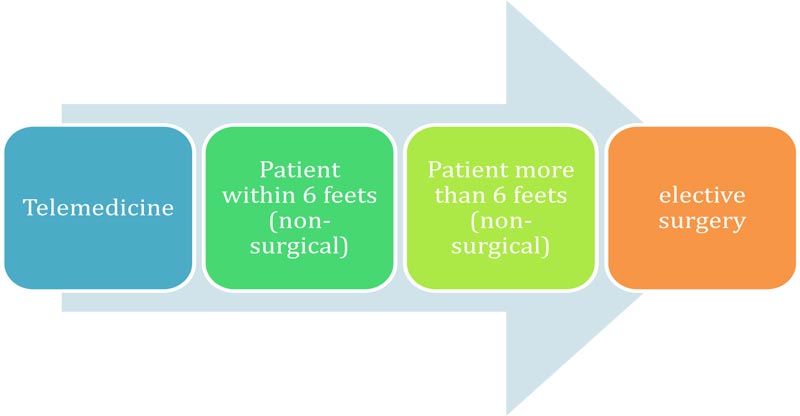
The matter of PPE is pivotal in the defense against this crippling pandemic. Health workers on the frontlines are at the highest risk of acquiring the disease. Guidelines by many orthopedic organizations and societies came to light in order to help surgeons deal safely with their patients in outpatient, inpatient and emergency room settings as well as in the operating room [16-18]. For example, The American Acad- emy of Orthopedic surgery, in its clinical considerations during COVID-19 recommended delaying elective surgeries; it has set the first priority to be the safety of patients and the second priority is the safety of health care personnel and staff during patient confrontation. It classified the risk for transmission of the disease between care providers and patients into four categories depending on the method of the encounter; 1) telemedicine: No risk, 2) personal communication more than 6 feet away from the patient: lower risk, 3) personal communication within 6 feet from the patient: greater risk and 4) Elective surgery: Greatest risk [19, 20] (Fig. 6). Farrell et al. suggested some recommendations to increase safety inside the Operating Room (OR) including avoiding laminar flow, minimizing number of personnel in OR, the use of N95 masks and goggles, especially when power tools are used, stopping using pulse lavage, the use of absorbable sutures to reduce the number of visits post-operatively and the use of clear dressing material to allow wound inspection via telecommunication [21].
Deficiency of PPE in many countries led to a change in guidelines and decision-making regarding dealing with both trauma and elective cases [6]. In our survey, most practitioners showed good practice in wearing face mask and gloves while dealing with ER patients. Unfortunately, this was not the case while performing surgeries as 90.5% of staff did not use full PPEs, including face shields or goggles. We compared this to another practice in the same region reported by a study from turkey; in their study, only 12% of participants didn’t use any added PPE like goggles when performing surgeries [15]. Emerging guidelines urged all staff in OR to adhere to the use of full PPE. This is especially important in orthopedic procedures which are considered the highest in aerosol generation [16, 17, 19-20].
Resuming outpatient orthopedic service after lockdown must be planned carefully ensuring the safety of patients and care providers. Lal et al. suggested introducing new measures and tools for application in outpatient departments, including staff screening and testing, patient pre-visit questionnaires and screening, online registration and appointment scheduling, effective and short encounter, and the use of digital methods for documentation and payment. They also suggested a full algorithm for appointment management and reception of patients starting from the main entrance of the facility till leaving it. They also provided recommendations regarding spatial organization and timeline control of the outpatient clinic atmosphere [22].
Many factors play a role in deciding between conservative and operative management. The new viral pandemic could have had a role in changing the surgeon’s mind regarding the best treatment option under the circumstances. The results of this study showed a change toward non-operative treatment by 61.9% of the respondents. We investigated the change in decision making in correlation to surgeon's age, seniority level, sector of practice, medical co-morbidities and marital status. Results showed that factors affecting the change in decision making were age and participant’s seniority level; as consultants showed a preference toward non-operative management compared to residents and junior specialists.
Follow up of orthopedic patients is crucial in optimizing the outcome. In Jordan, as in many other countries, outpatient visits were significantly reduced to minimize contact [14, 15, 18, 21]. This had led to an increase in the use of telemedicine during the current crisis [23-25]. Telemedicine can help deal- ing with many cases without the need to bring the patient to the hospital or clinic. The patient can be given an advice or an over the counter prescription. History, for example, can be taken over the phone, and wounds can be inspected via a video call. This practice will significantly reduce the burden on orthopedic clinics and resources taking into consideration the global battle with providing enough PPE to health practitioners. Daily ward rounds can be done this way which reduces number of the surgeon’s visits to ward.
Our participants’ experience with the use of telemedicine to follow up their patients were variable; most of the respondents stated that they could solve patients’ problems in less than 50% of cases while 15.6% could not do any follow up of their patients during the lockdown. This loss of patient follow up could have had tremendous effects on the wellbeing of patients and a significant delay in dealing with potential complications that could arise, this should be explored more in further studies.
In addition, the impact of the lockdown affected the income of our participants. Even though this was the only question that was not obligatory, all participants responded. The results had two major and almost equal trends. While public sector practitioners showed minimal or no change to their income, private sector doctors stated that they lost more than 50% of their income.
Until the beginning of October 2020, at the time of preparing this paper, the number of patients diagnosed with COVID-19 infection were just more than 22 thousand cases with 166 fatalities. There have been many causalities between healthcare workers dealing with COVID-19 patients. Despite this sudden rise of cases, complete lockdown was not implied again because of its massive negative impact on economy and health care system.
CONCLUSION
The novel coronavirus (COVID-19) pandemic led to strict lockdowns in many countries. Jordan, as an example of a country with a very strict lockdown, experienced many changes to orthopedic trauma practice during the curfew. The number and type of cases showed significant changes with an overall decrease in the number of trauma cases reported, particularly complex and multiple trauma patients.The number of trauma surgeries showed a significant reduction, and the surgeons’ attitude toward patient encounters changed with new habits of wearing PPEs although the compliance inside the operating room was poor. There was a slight increase in the tendency towards non operative management especially among senior doctors. This study showed the need for stricter implementation of guidelines to protect patients and staff. Follow up of patients was found to be difficult during the lockdown and telemedicine stood out as an important part of practice under these unusual conditions. However, the medico-legal consequences of telemedicine need further assessment. The effect of lockdown on the follow up and wellbeing of our orthopedic trauma patients is an important concern that needs further research in the near future.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Institutional approval was obtained from the Institutional Review Board of the Hashemite University, Jordan (Approval No. 2020 /2019 /6/2).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from each participant prior to the study.
AVAILABILITY OF DATA AND MATERIALS
All data and supplementary material are available from the corresponding author [A.A.R.A] upon request.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest regarding this project and they approved it for publication
ACKNOWLEDGEMENTS
We would like to extend our thanks and gratitude to Dr. Deema Faisal Masarweh from the University of Jordan for helping the research team in performing the statistical analysis using SPSS software.
SUPPLEMENTARY MATERIAL
Supplementary material is available on the publisher's website along with the published article.


