All published articles of this journal are available on ScienceDirect.
The Training of Undergraduate Medical Students in General Medical Practice and Primary Health Care: A Scoping Review
Abstract
Background:
Undergraduate medical students are trained to acquire a general medical practice overview on qualifying. This training forms a foundation for primary health care service or further training towards a specialty of choice.
Objective:
The aim of the study was to determine the scope of published scientific literature on the training of undergraduate medical students in “general medical practice” and “primary health care,” exploring how these two concepts are understood, the pedagogical approaches employed by the trainers, the training platforms and the challenges encountered during the training.
Methods:
The review followed the five steps recommended by Arksey and O’Malley. Using the specified eligibility criteria, the research team systematically screened titles, abstracts, and full articles. Data were entered into Google Forms spreadsheets, which was followed by inductive data analysis of key themes.
Results:
130 articles were eligible for inclusion in the study. Thematic analysis yielded eight themes: definition of “general medical practice” and “PHC”, pedagogical approaches (conventional, PBL, teams and CBME), training platforms (tertiary and rural), medical students’ trainers (faculty, GPs and patients), training content, trainers’ and trainees’ perceptions, and challenges encountered.
Conclusion:
This scoping review has revealed that general medical practice and primary health care are approaches to holistic patient care taught at undergraduate medical training. Primary health care and general medical training are mainly undertaken in GP practices and rural settings. Competency-based medical education is emerging as an appropriate pedagogical method towards ‘fit-for-purpose’ training. The inclusion of patients as trainers in general medical practice and primary health care is yielding positive results.
1. BACKGROUND
Internationally, the training of undergraduate (UG) medical students takes various forms, guided by the health needs in a specific setting. In the USA, Canada, South America, Europe and Australia, the basic medical degree, i.e., Medical Doctor (MD), Bachelor of Medicine and Bachelor of Surgery (MBChB or MBBS), does not qualify the practitioner to practice as a general medical practitioner [1-7]. The undergraduate degree has to be followed by further training and obtaining a postgraduate degree for general medical practice [8-11]. In Asia, the basic medical degree is the MBBS, which is followed by a one-year internship, after which the candidate can choose to practice as a general medical practitioner (GP) or follow a particular specialty [12, 13]. A similar trend is followed in Africa [14, 15], where a GP is a ‘medical officer’ in private practice, who (unlike a ‘family physician’) does not have any further qualification following the UG medical training [16, 17]. It can, therefore, be argued that the various approaches in the training of a general medical practitioner are determined by the expectations of service delivery in the workplace, post-qualification, which in turn, informs the nature and emphasis of the training at the UG level. In most countries in Asia and Africa, general medical practice commences immediately after the internship year [15].
It is important to explore the definition of generalism or general medical practice in literature since the understanding of a concept informs its application [18]. General medical practice is commonly understood as the discipline that manages all medical conditions [19]. However, given the vast amount of ever-increasing knowledge in the medical field, it is clearly impossible for one individual to have it all [20]. Therefore, a more pragmatic definition of generalism in medical practice is required. In a similar manner, the definition of primary health care (PHC) needs exploration. In 1978, the World Health Organisation (WHO) adopted PHC as the most effective strategy to meet the health care needs of communities internationally [21]. However, the extent to which this definition has influenced UG medical training needs exploration.
Medical schools around the world adopt various pedagogical approaches in their UG training programs, some of which are lecture-based [22], problem-based [23], team-based [24] and competency-based [25]. The pros and cons of each approach need to be explored as well as its effectiveness and efficiency in student training in a given context. Furthermore, the stakeholders involved in the training of UG medical students need to be identified [26], including the skills they teach and the curriculum content [27, 28]. Understandably, the knowledge and skills training are governed by the community context where the training is undertaken [13]. Training platforms also play a significant role in providing the students with the required exposure, preparing them for the field of practice [29, 30].
The scoping study was conducted to map the literature on training in general medical practice and PHC for UG medical students, students’ trainers, pedagogical approaches applied, training platforms, stakeholder perceptions and challenges encountered in the process. The intention was to develop a database on the various dimensions of UG general medical practice training and PHC.
2. METHODS
The research team started to conduct this scoping review in 2018. It followed the framework outlined by Arksey and O’Malley, comprising five steps, (1) identification of a research question, (2) identification of relevant studies, (3) study selection criteria, (4) data charting, and (5) data collation, summarizing and reporting of results [31].
2.1. Stage 1: Identification of a Research Question
The guiding research question for the study was: ‘What is the scope of literature on the training of undergraduate medical students in general medical practice and primary health care?’ Specific questions emanating from the main question were:
● How is ‘general medical practice’ as well as ‘primary health care’ defined in the literature?
● What pedagogical approaches are employed in imparting knowledge and skills in the training of students in general medical practice and PHC?
● What are the training platforms used in general medical practice and PHC training?
● Who are the trainers of general medical practice and PHC?
● What are the perceptions of the trainers and medical students regarding training in general medical practice and PHC?
● What are the challenges facing undergraduate training in general medical practice and PHC?
2.2. Stage 2: Identification of Relevant Studies
Literature was searched using online databases and references of the articles obtained. The online database search was conducted using EBSCOHost, Pubmed, Sabinet, Science Direct, Scopus, and Web of Science. A few combinations of words and phrases obtained from the Medline MeSH (Medical Subject Heading) terms on undergraduate medical student training in general practice and PHC were tested (Table 1), and a comprehensive word string agreed to by the researchers was: ‘medical AND (student* OR undergraduate OR train*) AND general AND practice AND educat* OR phc’. An alert was set in the listed databases using the search string to receive additional articles during the preparation of the review manuscript and beyond.
| Population | Intervention | Outcome: General practice | Outcome: PHC |
|---|---|---|---|
| Undergraduate Medical Student Medical Student Student Doctor Trainee Doctor Learner Doctor Trainee Physician |
Training Education Learning Instruction Schooling Practice Coaching Guidance Tuition |
Doctor Medical Doctor General Practitioner Generalist Medicine Physician Medical Person MD Doc Medical officer Medical Intern Houseman Medical Graduate Medico Medical Expert |
Primary health care PHC Primary Care |
2.3. Stage 3: Study Selection Criteria
All articles, editorials, documentaries, and reviews in peer-reviewed journals, which reflected the keywords in the string mentioned above, written in English, conducted in humans, and published from 2008 to 2018, were included. We decided to confine ourselves to this period to get hold of the trend over the recent decade. Titles and abstracts were independently screened by LHM and GD. Full-text articles were independently screened by LHM and SJM, while GD removed the discrepancies. Further discrepancies were resolved through ongoing online discussions, as recommended by Levac et al. [32]. Google Forms [33] was used to screen the eligible journal articles. The template used comprised the following subheadings: is the article about undergraduate medical students? (population), is the article on general medical practice and/or PHC? (intervention), is the article about education/training/learning/mentoring/skills training of undergraduate medical students? (intervention), and does the article report on medical students qualifying as general medical practitioners? (outcome).
2.4. Stage 4: Data Charting
The research team developed a data charting form to capture information from the selected articles, according to the author/s, year of publication, population and sample, setting, aim and objectives, methods used, outcomes, conclusions and recommendations. Data were captured on Google Forms [33], which was followed by a quantitative and qualitative (thematic) data analysis.
2.5. Stage 5: Data Collation, Summarizing and Reporting of Results
A narrative description has been used to describe the scoping review findings, thereby providing insight into the themes that emerged.
| S.No. | Theme | Sub-Theme |
|---|---|---|
| 1. | Definitions | • General Medical Practice • Primary Health Care |
| 2. | Pedagogical Approaches | • Conventional lecture-based learning • Problem-based Learning • Learning in Teams • Competency-based Learning |
| 3. | Training Platforms | • Tertiary hospitals • GP Practices • Rural Facilities • Urban Facilities |
| 4. | Trainers of Medical Students | • Medical school academics (Faculty) • Hospital Staff • GPs • Patients |
| 5. | Content of General Medical Practice and PHC Training | • Technical skills • ‘Soft’ skills |
| 6. | Preparedness for Practice | |
| 7. | Perceptions on General Medical Practice and PHC Training | • Trainers • Patients • Students |
| 8. | Challenges in General Medical Practice and PHC Training |
3. RESULTS
3.1. Overview of Results
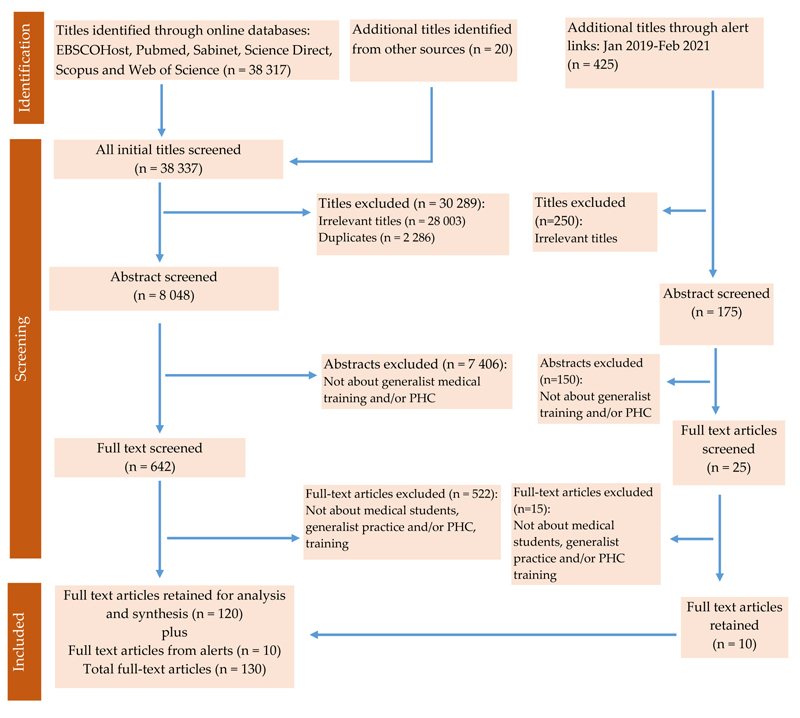
The EndNote (X9) referencing software was used to organize the information. Using the search string provided above, the comprehensive process yielded 38,317 titles. Titles added from other sources (including references of articles) were 20. At the time of the completion of the manuscript (28 February 2021), there were 425 titles that were added from the alerts, which were analysed through the inclusion criteria outlined above. Fig. (1) outlines the selection process (Table 2).
3.2. Definitions of General Medical Practice/Generalism
3.2.1. General Medical Practice/Generalism
There were various definitions linked to the key concepts of the review, particularly general medical practice and primary health care. The definitions were shaped by how they were utilized or perceived by end-users or based on what was regarded as the official key role of the position or level of care of the practitioner.
General medical practice has been defined as the discipline which “deals with health problems in their physical, psychological, social, cultural, and existential dimensions” [34]. It is characterized as the point of first patient contact with a healthcare provider, following a person-centered approach on the basis of health promotion, disease prevention and continuity of patient care [19, 34]. It has also been explained in terms of the key roles of a general medical practitioner, which are (1) holistic patient care which entails involvement in all aspects of the patient’s life, (2) management of undifferentiated patient problems, (3) coordination of care which involves other healthcare providers, (4) patient advocacy in consideration of the patient’s social determinants of health, (5) compassionate care which entails patient-centered communication, (6) reflective mindfulness, whereby the practitioner is self-aware of personal thoughts and emotions, and (7) life-long learning, which is a process of continuous personal and professional development [19, 35]. These roles and characteristics have been recommended for teaching at UG medical training [13]. One article indicated that general medical practitioners provide value to health care through the general medical approach they employ, rather than a comprehensive scope of medical practice, implying knowledge of all possible medical conditions (“a Jack of all trades and the master of none”), which is a misleading perception [19].
3.2.2. Primary Health Care
There were various definitions of PHC. Following the WHO definition of PHC in Alma-Ata in 1978 [21], a modern concept of PHC, aligning itself with Sustainable Development Goals (SDGs), has been elaborated as “a whole-of-society approach to health that aims equitably to maximize the level and distribution of health and well-being by focusing on people’s needs and preferences (both as individuals and communities) as early as possible along the continuum from health promotion and disease prevention to treatment, rehabilitation and palliative care, and as close as feasible to people’s everyday environment” [36]. A study demonstrated that there was no common understanding of PHC among the students’ clinical trainers [37]. There was an attempt to differentiate between primary care (PC) and primary health care (PHC). PC was explained as the ‘family doctor-type services’ provided to individuals and their families, while PHC was explained as a ‘system-level function’, with universal access to the use of resources through public participation [38, 39]. However, most literature used these terms interchangeably [40-42]. Whereas some authors referred to PHC as only the basic level of care [43, 44], offering mainly ambulatory care [45], there was a realization that it was actually an approach to the whole spectrum of healthcare delivery [46-48], essentially suited for inclusion at UG medical training [13].
3.3. Pedagogical Approaches in General Medical Practice Training and PHC
The literature search yielded mainly four pedagogical approaches which were employed in the general medical practice training of UG medical students: conventional lecture-based learning, problem-based learning (PBL), learning in teams, and competency-based medical education (CBME) [14, 22, 49-52]. Of particular note was that, internationally, countries tended to align their training curricula to their respective national healthcare systems so as to meet their healthcare needs [13, 43, 53, 54].
3.3.1. Conventional Lecture-based Learning
This was described as entailing teaching and learning in small groups or whole-class lectures to supplement other pedagogical approaches [23, 55, 56]. However, on its own, it was found to be less effective, because there is no evidence that lecture attendance translates “into listening, understanding and knowledge retention” [23]. This method does not inculcate critical thinking, problem-solving, independent and self-directed learning skills to the learners [55, 57].
3.3.2. Problem-based Learning (PBL)
A number of institutions have adopted and implemented PBL teaching and learning method to facilitate skills and knowledge acquisition [51, 53, 58-62]. In one study [63], it was found to be ineffective as a result of low faculty-to-student ratios [61]. Another challenge is that PBL needs to be applied in a number of independent students’ working groups per given class, wherein each group requires its own tutor and learning resource material. This tends to be costly compared to other methods, like the team-based learning discussed below [23].
3.3.3. Learning in Teams
This approach entails embedding medical students in the clinical training years into healthcare teams to learn from their senior colleagues and to add value to the healthcare system [64-67]. The discipline of Family Medicine is found to play an important role as the team coordinator [68]. These teams are interprofessional, involving participants from other health sectors and beyond the healthcare sector [36, 68-72]. The emphasis on ‘learning together to work together’ as professionals has also been highlighted [36]. Another variant of teamwork has been introduced through Team-Based Learning (TBL), which entails organizing students into permanent study groups in one classroom, and allocating them to an instructor who directs the learning activities. Clear core educational principles are outlined. Content mastery occurs over three phases: (1) pre-class preparation, (2) a readiness assurance test, and (3) knowledge application through group problem-solving assignments on real-life problems [23]. This approach has been recommended for low- and middle-income countries (LMICs), including African countries, as it can be employed at minimum cost [23]. African countries that have implemented it with significant success are Zimbabwe [24] and Tanzania [73]. However, no mention is made regarding interdisciplinary and interprofessional collaboration in this pedagogical approach.
3.3.4. Competency-based Medical Education
Competency-based medical education (CBME) recognizes that not all trainees master the required knowledge and skills at the same pace [25]. This calls for a learner-centric education system which will, in turn, translate into a patient-centric care system [74]. Its focus is, therefore, outcomes-based. It is essentially a paradigm shift from the ‘structure- and process-based system that defines the training experience by exposure to specific contents for specified periods of time’ (for example, six weeks’ exposure to the surgical discipline) to “ the competency-based system that defines the desired outcome of training”, which drives the educational process and its evaluation [75]. However, the implementation of CBME whereby individuals (trainers and trainees), institutions and regulatory bodies hold one another mutually accountable for achieving the outlined outcomes has remained a challenge [76]. In South Africa, the Health Professions Council of South Africa (HPCSA) requires medical school curricula to be aligned to ‘core’ graduate competencies, so that the graduates are skilled clinicians able to provide professional and ethical health care needed for the whole population [77, 78]. Further elaboration of CBME has led to the development of entrustable professional activities, whereby a trainer entrusts specific tasks or responsibilities to the unsupervised trainee once s/he has attained sufficient specific competence [79]. It is hoped that entrustable professional activities will address the question of qualifying medical practitioners’ preparedness for practice [3].
3.4. Training Platforms
The literature revealed that training in general medical practice and PHC occurred in PHC settings, among general medical practitioners’ (GPs’) practices, and in tertiary hospitals affiliated with medical schools.
3.4.1. Primary Health Care Settings
Students’ PHC exposure comprised rural and urban health facilities, as well as GPs’ practices [51, 80, 81]. Rural placement was the major training platform for student exposure to general medical practice training across all countries [43, 69, 82-86]. In the rural immersion, students were supervised by experienced clinical staff [83], with the aim of ensuring good quality teaching and learning in general practice [87]. The rural placements offered longitudinal integration learning opportunities to students, whereby they were involved in ‘patient continuity of care’ through follow-up [88, 89], and vertical integration, defined as “learning from professional colleagues at a different point of their career” [89], and collaborating with multiple disciplines. One study provided evidence that longitudinal clerkships in general practice increase the number of exposures to various conditions and diseases compared to the traditional hospital-based curriculum [29]. Most benefit was observed when the training was conducted in well-equipped training centres where students were provided with laptops and internet access [83]. However, the learning process was frustrating where there was a lack of these learning resources, particularly in the LMICs [81].
On the whole, the rural settings provided students the opportunity to practice procedures, as there was less competition for skills learning as compared to that encountered in the tertiary institutions [81], where there were various categories of learners (e.g., residents), competing for available cases. The rural settings were thus regarded as “an excellent learning environment for medical students to learn skills and knowledge from” [81]. Interestingly, when comparing the clinical skills experience of the rural placed students to that of their peers in tertiary hospital settings, it was found to be equivalent [83].
In addition to the rural and remote training platforms mentioned above, urban-based platforms located outside the tertiary hospitals were also utilized [30, 90, 91]. These comprised community-based public and private hospitals [92].
3.4.2. GP Practices
GPs constituted an excellent position to demonstrate a safe and effective patient consultation to medical students, matching symptoms with disease processes to emerge with the required understanding of the dynamic nature of illnesses [58, 93-99]. Many of the GPs have been found to be situated in urban areas [30, 93]. They play a key role in the longitudinal clinical placements program [58], where students gain hands-on experience on undifferentiated and unclassified patients, as well as common clinical conditions, rarely seen, especially in tertiary hospital settings [100]. One study has demonstrated that it is also feasible to teach large groups of students (e.g., ten students into one general medical practice), which was appreciated by students [101]. Evidence also indicates early student exposure to general medical practice is beneficial [102].
The training in PHC settings mentioned above has been identified as the trend towards the future in undergraduate medical students’ training [39, 103]. On evaluation, these placements have been found to improve the quality of undergraduate student training [104]. However, it has also been observed that the impact of community placements for general medical practice training is reduced if introduced late, at the verge of students’ course completion [105]. In cases where PHC platforms were unavailable, one institution created an innovative virtual alternative [106].
3.4.3. Tertiary Hospitals
Tertiary hospitals formed part of the training platforms for undergraduate student training [58, 83, 100, 107, 108]. These settings, which are usually affiliated with medical schools, expose students to tertiary-level diagnostic techniques, curative and palliative care, and management of chronic illnesses complications [109, 110]. However, these platforms have been reported unsuitable for general medical practice training to UG medical students as they are manned by specialist trainers [52].
3.5. Trainers of Medical Students
Various stakeholders were identified as trainers of undergraduate medical students, providing “an all stake-holder training approach” in general medical practice care [111]. GPs were the medical practitioners frequently available to train students in communities [30, 112]. Specialists (public and private) in tertiary institutions and those visiting distant learning platforms offered valuable input to students [30, 58, 101]. Nevertheless, specialists tended to be concentrated in tertiary hospitals [85, 111], with a dire shortage in rural settings [81].
Community hospital staff, including nurses and midwives, also featured as trainers [81, 83] as well as paramedics [69]. Patients also participated in student training [26, 38, 98]. For maximum contribution as trainers, patients were regarded as subjects with a voice rather than merely as objects of learning [98]. The value of involving standardised (simulated) and volunteering real patients as part of the overall student training and assessment has been recognized [113].
The training of medical students became effective when accompanied by constructive, timely, and acceptable feedback to the students [112].
3.6. Content of General Medical Practice and PHC Training
The World Organisation of Family Doctors (WONCA) recommended a well-structured undergraduate training program to be incorporated in the learning and teaching of general medical practice [114]. The literature displayed the broad concepts used by various institutions to integrate general practice in curricula [87, 115, 116]. Structuring involved dedicating specific number of hours to specific learning activities, e.g., lectures, seminars and practical classes [117].
Both ‘technical’ and ‘soft’ skills are taught to students. Technical skills are described as mainly procedural skills, including physical examination, side-room tests, special investigations, non-pharmacological and pharmacological management, as well as surgical procedures [118]. “Soft skills,” on the other hand, have been described as “interpersonal skills, professional attitudes, teamwork and ethics,” which are mainly imparted to students through role modeling by trainers [119].
3.6.1. Technical Skills
The importance of physical examination training in general medical practice [28, 120], including procedural skills [121] and acute (emergency) skills [122], has been highlighted. The training in the latter was found lacking among undergraduate medical students [123]. Other skills mentioned were palliative care [118], patient referrals to other disciplines and professionals [124], including accompanying patients from primary health care settings to hospitals [123].
3.6.2. ‘Soft’ Skills
‘Soft’ skills are also referred to as interpersonal skills [125]. The training of undergraduate students in interpersonal skills entails the mechanics of safe consultation skills [58, 94, 123]. Every consultation has to display patient-centredness, which is an approach that puts the patient rather than their disease into focus, with holistic care [126, 127]. This approach has been identified as one of the core required competencies [128, 129]. In demonstrating patient-centredness, the students were trained to follow the patient’s agenda, adopt a comprehensive (bio-psycho-social) approach and be empathetic to the patient. Additionally, s/he needs to reflect on what a patient says and be a mindful listener [130]. The training in patient-centredness has also been referred to as the Patient Partner Program (P3) [130]. Students were also taught advocacy for health defined as “action by a physician to promote social, economic, educational, and political changes that ameliorate threats to human health” [131], to build a generation of physician advocates [132], who will address health disparities in the various communities [55]. The introduction of the health disparities in the early years of the undergraduate program has been found to be effective in inculcating the culture of patient advocacy among students [133]. There was also training provided regarding ethics and professionalism [134], with a focus on social determinants of health, which becomes effective if student-driven [61, 135].
3.7. Preparedness for Practice
In a survey conducted in 2000/2001 in the UK, it was found that 42% of newly qualified medical practitioners felt that their medical school training had not adequately prepared them for the field of practice [3]. Although the situation showed a 28% improvement in a repeat study four years later (2005), it had not been eliminated [3]. In 2009, it was further observed that a significant increase in patient mortality occurred in the UK as a result of the influx of newly qualified doctors [136]. To this end, the General Medical Council (UK) [137] recommended that ‘all final-year undergraduates (should) initially undertake a structured shadowing period within the foundation posts that they would be commencing work in’ (general medical practice or specialty) [138]. This policy resulted in an increase in students’ confidence regarding their readiness for practice [139, 140]. The uncertainty in preparedness for practice at UG exit point was also reported in Africa [141], where factors significantly correlated with students’ preparedness for practice were identified as shadowing qualified medical practitioners’ (similar to the UK system) [117], training on real-life patients and students’ identification of role model trainers [142].
3.8. Perceptions on General Medical Practice and PHC Training
General practitioners tended to express satisfaction with the students’ clerkships in their practices [15, 95, 143]. They were motivated by the value they brought into the teaching system (altruism), the gratification they enjoyed in the process, as well as the enhancement of their self-esteem [95]. However, in some cases, they were dissatisfied with how the clerkships were organized [144]. Some medical students and faculty members expressed concerns that involving non-academic practitioners in students’ training could compromise teaching standards, and questioned their devotion to teaching while they also had to make money in their practices [15]. Indeed, it has been realised that GPs incur hidden costs in the training of students. To address this need, in other countries, e.g., the UK and Australia, the involved GPs are paid a reasonable allowance for their services and the improvement of the infrastructure to tailor-make it for learning [144].
Patients viewed their contribution to student training in a positive light [95, 144]. They regarded it as an opportunity to plough back into the care they had received from health care providers and to contribute towards the training of future doctors [114]. In the same vein, there were some patients who felt inconvenienced by the reduced attention given to them by their physicians as a result of students’ presence in the consulting room [95, 114], and the need for privacy and confidentiality [26], especially in private practices [15, 95].
While students recognised the value of the teaching and learning received from GPs, they did not think highly of GPs; their views were that a GP’s job was not as lucrative as other disciplines in terms of remuneration [145]. Furthermore, they thought GP service provision was “just basic,” uninteresting, subjected the practitioner to long working hours, and was only undertaken by those practitioners who could not pursue any specialty [145-147]. They lacked a clear understanding of the discipline [145]. It was found that those students who had a positive attitude towards general medical practice would also support changes towards the inclusion of more general medical practice sessions in the undergraduate curriculum [146]. In other settings, faculty and students did not perceive the GPs suitable for teaching medical students for fear of compromising training quality because they were viewed as lacking in continuous medical education and focused on money-making [15]. Nevertheless, students were appreciative of other aspects of PHC training like preventive programs [55].
3.9. Challenges in General Medical Practice and PHC Training
The literature revealed the challenges inherent in the training of medical students in general medical practice and PHC. These included the lack of integration of a general medical approach in the undergraduate curriculum, poor quality of supervision within primary care settings, and the assumption that knowledge and skills will be acquired through specialist-provided learning and teaching methods [53, 148], too little time dedicated to general medical practice training at the undergraduate level [124], inadequate trainers of primary health care [149], and the sometimes hostile environment which does not recognize the need for the incorporation of PHC at undergraduate level [150]. The scarcity of primary healthcare placement sites presented another challenge, hence suggesting the innovative use of ‘simulated’ general medical practice clinics using actors (simulated patients) [151] and the creation of virtual patient cases for PHC-based learning [106]. The results have been summarized in Table 3.
| Authors & Year | Origin | Type of Source | Purpose | Summary Points | Idea in Brief |
|---|---|---|---|---|---|
| 1. Definition of general medical practice | |||||
| Hashim MJ (2016) | UAE | Research | To describe principles of family medicine/general practice | Generalist approach and continuity of care | It is continuity of care |
| RCPSC (2013) | Canada | Report | To report on generalism and generalist education strategy in Canada | Generalists coordinate health care, have broad-based core abilities to manage diverse undifferentiated conditions. | It deals with coordination of health care |
| Mash R (2015) | South Africa | Research | To discuss the roles and training of primary care doctors | Medical graduates should be comprehensive generalists. | It is comprehensive |
| 2. Definition of primary health care | |||||
| Abbas SM (2012) | Pakistan | Research | To explore the views of teaching faculty on primary health care | Primary health care is comprehensive, including disease prevention, proper nutrition, safe water and sanitation | It is comprehensive health care |
| Chung C (2016) | Switzerland | Research | To determine the impact of the primary care curriculum on medical students’ perception of primary care | Longitudinal, well-structured primary care teaching programs are more effective in students following primary health care | It should be taught longitudinally |
| WHO (2018) | Kazakhstan | Report | Declaration of Astana on primary health care | PHC is prioritization, promotion and protection of populations and individuals through strong health systems | It prioritizes health promotion |
| 3. Pedagogical approaches | |||||
| Kershaw G (2017) | UAE | Research | To describe a health promotion project as a self-directed project-based learning task integrated within the curriculum | Students receive lectures to execute a given task in groups and present to the whole class after 12 weeks | Conventional lecture style |
| Garcia-Jardon M (2011) | Canada | Research | To determine MBChB-III students’ perceptions about some key aspects related to integrated PBL curriculum | Students generally presented favorable perceptions of the integrated PBL curriculum. There were concerns about the associated heavy workload and stress | Problem-based learning |
| Garcia-Huidobro D (2013) | Chile | Research | To develop an IPE course in primary care for medical, nursing, and psychology students and to assess their perceptions about learning | Learning Together to Work Together: Interprofessional Education for Students in a Primary Care setting | Learning in teams |
| Caverzagie KJ (2017) | USA | Research | To describe the challenges facing CBME | Stakeholders in teaching need to be aligned in defining outcomes, integrating the learning, and be mutually accountable | Competency-based learning |
| 4. Training platforms | |||||
| Huenges B (2014) | Germany | Position paper | To demonstrate the possible ways in which more aspects of primary care could be integrated into under-graduate medical training | During the teaching of different clinical subject areas (int med, surgery, gyne, ENT, dermatology, neurology) aspects of interfaces with PHC should be addressed | Tertiary platforms |
| Mahoney S (2012) | Australia | Research | To describe a new model for urban community based medical education | There is a wealth of clinical learning potentially in general and private community facilities |
Urban platforms |
| Bartlett M (2016) | UK | Research | To evaluate the rural teaching from the perspectives patients, general practice tutors, community hospital staff and students | Teaching undergraduate students in rural general practice in a new rural campus in England | Rural platforms |
| Mahoney S (2016) | Australia | Research | To compare urban and rural placed students in learning from GPs | The GPs who have provided the longitudinal clinical placements for this program have been key contributors to the program | GP platforms |
| Ramanayake RPJC (2015) | Sri Lanka | Research | To explore experiences of GPs on training medical students | Students learn different aspects of medicine at GP practices which they cannot acquire in other settings. | GP platforms |
| 5. Student trainers | |||||
| Sajjad M (2015) | Pakistan | Research | To outline how to Improve Workplace-Based Learning for Undergraduate Medical Students | The stakeholders involved in the workplace-based learning were the students, clinicians and the patients | Clinicians |
| Haffling A-C (2011) | Sweden | Research | To study medical students' learning experiences and the perspectives of GP supervisors and patients. | Student trainers were GPs and patients | GPs and patients |
| Prose N (2005) | South Africa | Research | Faculty took medical students to a community street facility for exposure | Students learnt in a community facility accompanied by a faculty trainer | Faculty |
| Strasser R (2016) | Canada & Australia | Literature review | To explore experiences in Australia and Canada of students learning medicine in the general practice setting | The teaching platforms have swung back to community settings from universities | GPs |
| 6. Skills training | |||||
| Wearne S (2011) | Australia | Research | To describe how procedural skills are learned and suggest a practical framework | The “see one, do one, teach one” as a model for skills teaching | Technical skills |
| Carpenter A (2014) | UK | Research | To train medical students on the fundamental principles of treating acutely unwell patients into the UG curriculum | Skills to manage emergency patients should be part of UG student training | Technical skill |
| Silverston P (2013) | UK | Research | To demonstrate a method of teaching consulting skills in primary care | Training in consultations skills | “Soft skills” in training medical students |
| Bombeke K (2010) | Belgium | Research | To explore the experiences of medical students and their teachers in relation to patient-centredness | when students are surrounded by non-patient-centred role models, they lose their patient-centred focus. | “Soft-skills” in training medical students |
| Barr J (2014) | Australia | Research | To train students on patient-centred medical education | Students need to be taught to be mindful listeners of patients | “Soft-skills” in training medical students |
| Rieffestahl AM (2021) | Denmark | Research | To explore learning of medical students from patients with chronic conditions in the context of communication skills training | Students expressed emotional responses on challenges in performing their role as practitioners | “Soft-skills” in training medical students |
| 7. Preparedness to practice | |||||
| Braniff C (2016) | UK | Research | To evaluate the impact of the assistantship on students' perception of their preparedness for starting work | The assistantship improves medical students' perception of their preparedness for starting work | Feeling of unpreparedness |
| Muthaura P (2015) | Kenya | Research | To explore the perceptions of the preparedness of medical graduates to take on internship responsibilities | Medical doctors expressed feeling poorly prepared for an internship in a low resource hospitals, especially in skills | Feeling of unpreparedness |
| 8. Perceptions on general medical practice and PHC training | |||||
| Matchaya M (2009) | Malawi | Research | To describe perceptions of medical students, recent medical graduates, faculty of the College of Medicine (Malawi) GPs towards an attachment of medical students to private practices | GPs held a positive attitude towards training students in their practices | GPs |
| Ramanayake RPJC (2015) | Sri Lanka | Research | To explore experiences of GPs on training medical students | Altruism, self-satisfaction and self-esteem are main reasons for GPs’ involvement in undergraduate training | GPs |
| Matchaya M (2009) | Malawi | Research | To describe perceptions of medical students, recent medical graduates, faculty of the College of Medicine (Malawi) GPs towards an attachment of medical students to private practices | Faculty, medical students and recent graduates of the did not perceive GPs as a resource to be tapped for the training of medical students | Faculty, students and recent graduates |
| Ramanayake RPJC (2015) | Sri Lanka | Research | To explore the training of medical students in general practice | Patients had positive attitudes towards students | Patients |
| Smith-Han K (2013) | New Zealand | Research | To investigate what future doctors are learning about the profession of general practice | General practice has been relegated to a low status (“bottom of the pile”) among students | Students |
| 9. Challenges in general medical practice and PHC training | |||||
| Wang HHX (2013) | China | Report | To report on General practice education and training in southern China. | There were challenges in resource restriction, rural and urban disparity, social attitude, and community involvement. | Resource constraints |
| Mash R (2015) | South Africa | Report | To propose how challenges in primary care education in South Africa can be overcome | Improving the leadership and supervisory skills of family physicians will make a significant contribution to a revitalized primary healthcare | Lack of leadership in PHC |
| Mariolis A (2008) | Greece | Editorial | To demonstrate that PHC attachment motivates students toward a generalist practice career. | A hostile environment which does not recognize the need for the incorporation of PHC at undergraduate level | Neglect of PHC in preference for specialization |
| Mahoney S (2012) | Australia | Case study | To describe a new model for urban community based medical education | Urban CBME would benefit from funding to provide infrastructure for teaching space and parallel consulting as has occurred in the rural CBME model | Scarcity of primary health care placement sites |
4. DISCUSSION
The review revealed various definitions and explanations of general medical practice and PHC, the pedagogical approaches employed in the training of undergraduate medical students on general medical practice and PHC, the training platforms used, the stake-holder trainers and the content of the training involved. Furthermore, the review also shed light on the perceptions of the trainers, students, and patients regarding the training program. Perceptions on the students’ preparedness for the practice field and the challenges facing the training program in general medical practice and PHC were also highlighted.
General medical practice was defined in various but similar terms as health care given at the patient’s first point of contact with a health care practitioner [19, 47], i.e., holistic care, as it takes into consideration the physical, subjective and contextual aspects of the patient in longitudinal (continuity of care) and integrated (interdisciplinary and interprofessional) parameters of health care [19]. This implies that a general practitioner approaches health care comprehensively, welcoming presenting patients, regardless of the nature of their health care needs [47]. In most cases, such patients have not yet been classified into disease entities (diagnoses) [47]. In the scoping study, the training of students in general practice was found to revolve around these terms. In the same vein, the terms defining PHC were “taking the whole society into consideration” [35, 37], “providing health and well-being” [35], “addressing the whole spectrum of ailments” [35] and “accessibility to communities” [35, 37, 38]. PHC was contrasted to primary care (PC); the latter was explained as the provision of health care to individuals and families, while the former was understood as operating at systems-level with public participation [37, 38]. Therefore, according to the literature, the difference between PC and PHC relates to the scope of practice [37, 38]. However, many authors used these terms interchangeably [38-41]. This implies that the reader of literature needs to understand the context within which PC and PHC are used so as to understand which of the two is being referred to.
A wide range of pedagogical approaches are used in the training of medical students in general medical practice and PHC [23, 25, 36, 51, 64, 69]. These are mainly employed in combination as determined by a particular training institution, the settings and availability of appropriate resources [57]. These approaches are better suited for LMICs, e.g., team-based learning which requires minimum training equipment and training personnel [23]. It seems that the current international trend is towards the learner-centric CBME, with the major focus on achievement of the desired outcomes in a specific competency, regardless of the time it takes to reach that point [74]. This has led to the development of entrustable professional activities, relating to the competency of the trainee to execute given tasks independently [79]. This approach, though still in development, seems to have identified the required ingredient in the training of professionals (including medical practitioners), as it brings into focus the application of acquired knowledge. Furthermore, if the competency outcomes of a professional are clearly outlined from the outset and achieved during training, the professional’s competency in the field of practice becomes predictable.
The training platforms used for student training in general medical practice were mainly those in PHC [80, 81, 83, 87], especially the rural settings [86, 88, 89] and GP practices [95, 96]. The latter were mainly concentrated in urban areas [30, 93]. This makes sense as training in these settings is mainly undertaken by general medical practitioners, away from specialised centres [96]. Students’ exposure in these settings tends to cover a wide range of conditions and increases the chances of hands-on experience, as competition from specializing students encountered in tertiary hospitals is minimal [81]. However, tertiary hospital training contributes to equipping students with knowledge on the management of patients with complex conditions which require specialised centres [109, 110]. Evidently, tertiary hospitals are not appropriate for general medical practice and PHC training.
The literature reveals that trainers of the medical students in general practice involve GPs [112], specialists [101], nursing fraternity [83], paramedics [68], real patients [98], and standardised (role-playing) patients [113]. This collaboration helps students in their interprofessional skills [69, 70]. Patients’ participation in students’ training highlighted the importance of treating patients as subjects (rather than objects) who can express opinions about students’ performance [98]. Hopefully, this helps inculcate the culture of patient respect among students to be carried over to the field of practice.
The content of student training entailed technical and ‘soft’ skills. Technical skills were explained as tangible and quantifiable because they deal with skills and procedures, which was not the case with ‘soft’ skills, which were attitude-based [125]. It is clear in the literature that the ‘soft’ skills have become the matrix for the technical skills, laying the foundation for the bio-psycho-social approach in health care delivery [136].
The preparedness for practice of qualifying practitioners is a concern in various countries, and measures have been put in place to meet the challenge [3, 115]. The measures included initially allowing students a shadowing period of training under a supervisor, which helped students adjust to the field of practice [115]. Indeed, it is common practice for newly qualified medical practitioners not to be independently entrusted with patient care on their arrival in the practice field [117]. Importantly, the mentoring on real-life patients conducted throughout the years of medical training (rather than leaving it for the practice field) has been found to better prepare medical students for practice [119].
There were various views and perceptions among the trainer stakeholders regarding the training in general practice, which became an important element to consider as it played a role in the training process [15, 95, 106, 128, 149]. GPs regarded the training of students in their practices as an opportunity for continuous self-learning and an enhancement of their self-esteem [95]. It was only when there was no proper organization of the program that GPs expressed dissatisfaction [149]. The trainers in the medical schools were concerned that the involvement of GPs in the training program could lower the teaching standards [15]. However, this was counterbalanced by the fact that the GPs involved tended to engage in continuous professional development, in order “to rise to the occasion” [95]. Patients were positive about their involvement in student learning [106, 128]. They were gratified by the contribution they were making in the training of future medical practitioners [114]. However, there were those who decried the process as compromising patient care by diverting the teaching doctor’s focus away from patients. While some students, on their part, were appreciative of the training by GPs and other non-specialist trainers [55], in some instances, they did not think highly of them [15]. They did not perceive general medical practice as a ‘lucrative’ and attractive field compared to specialties [149-151]. They displayed a lack of understanding of what the field entailed [149]. The authors of this scoping review are of the view that this situation presents a challenge for medical schools regarding general medical practice.
Training in general medical practice and PHC was not found to be without challenges. In some settings, there were inadequate trainers, too little time dedicated for UG training in general medical practice and PHC, and scarcity of training sites [53, 143, 144], leading to a low student-trainer ratio and poor results [61]. This calls for proper planning before implementation, by comprehensively assessing the learning environment as well as the availability of required resources. The system could then be developed gradually by phasing in the required components piecemeal.
5. LIMITATIONS
As stated above, the time period of the literature search of the scoping review was specified, which led to the exclusion of other relevant resources falling outside this period (2008 – 2018). To prevent loss of relevant literature which came while the review manuscript was being written, an alert was set in the listed databases using the search string, to receive additional articles dating from 2018 – February 2021. These were subjected to the same inclusion and exclusion criteria initially used. Although the grey literature search was performed, missing other references cannot be excluded. Furthermore, only English articles were included.
CONCLUSION
The aim of this scoping review was to map the literature on the training of medical students in general medical practice and primary health care. The understanding of general medical practice training centered around the biopsychosocial approach towards health care, while primary health care was understood as the basic level of care provided at primary health care facilities. Furthermore, the review also revealed that it should be understood as a system-based approach towards health care, focusing on the individual, families and communities, across the spectrum of disease. Student training on these broad concepts was implemented through various pedagogical approaches. Competency-based medical education, which ushered in entrustable professional activities, appeared to be a possible solution in training fit-for-purpose medical practitioners. Various student trainers based in the universities and distant training sites were identified. Although patients were identified as important stakeholders in the training team, there was a scarcity of the literature that reported on their inclusion. There is a need for further scoping reviews to map literature on patient inclusion in the training of medical students. Training platforms identified were primary health care settings, including rural sites. GP practices were found to be the most appropriate training sites for general medical practice and primary health care.
AUTHORS' CONTRIBUTIONS
LHM conceptualized the review. LHM and MM were involved in the review design. LHM was involved in data collection. All the authors were involved in data analysis and interpretation. All the authors were involved in the drafting of the manuscript and its critical revision for intellectually important content. All the authors have read and approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guidelines and methodologies were followed in this study.
FUNDING
This work is based on the research supported wholly by the National Research Foundation of South Africa (Grant Number 105229).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge Ms. Nomkhosi Charlene Mabuza for the secretarial work in the search of relevant literature.


