All published articles of this journal are available on ScienceDirect.
The Appraisal and Endorsement of Individual and Public Preventive Measures to Combat COVID-19 and the Associated Psychological Predictors among Chinese Living in Canada
Abstract
Aims:
The study examines the factors related to the appraisal and adherence of the individual and public health preventive measures.
Background:
The effectiveness of the measures battling the pandemic was largely determined by the voluntary compliance of the public.
Objectives:
This study aimed to identify psychological perception factors related to the appraisal of individual measures and endorsement of public health measures during the early stage of the COVID-19 pandemic among Chinese living in Canada.
Methods:
A convenience sample of 656 participants completed an online survey. Nonparametric Kruskal Wallis tests were used to compare COVID perception variables (e.g., perceived susceptibility, fear, perceived severity, and information confusion) among different sociodemographic subgroups. Bootstrapped regression models were used to assess the association of these variables with outcome measures.
Results:
Compared to their counterpart groups, lower perceived susceptibility was reported by adults 65 years and older (p = .002) or retired (p = .015); greater fear was reported by females (p = .044), those with lower education (p = .001), and Mainland Chinese (p = .033); greater perceived severity was reported by individuals with lower education and smaller household size (ps = .003). Perceived susceptibility was inversely associated with individual measure appraisal (p = .032). Perceived severity was positively associated with individual measure appraisal (p = .005) and public measure endorsement (p < .001).
Conclusion:
Individual behaviour measure appraisal was predicted by lower perceived susceptibility and higher perceived severity, whereas public health measure endorsement was related to higher perceived severity. These results inform the public and the policymakers about the critical factors that affect the preventive measure appraisal and endorsement.
1. INTRODUCTION
Since the World Health Organization (WHO) declared COVID-19 a pandemic on March 11, 2020, it has swept across the world. In order to combat the spread of the disease, worldwide lockdown and physical distancing measures have been implemented at both individual (e.g., wearing a face mask, handwashing, and disinfection) and societal levels (e.g., quarantine, social isolation and distancing, and lockdown). The Canadian federal government announced a 5-week lockdown on March 13, 2020 [1], and then Ontario declared a provincial state of emergency and began to order the closure of certain businesses and facilities on March 17, 2020 [2]. Individuals have been urged to comply with recommended preventive behavioural measures such as individual personal hygiene (e.g., handwashing, disinfection, wearing a face mask), along with the public health measures such as social distancing, school closure, and quarantine. The effectiveness of these measures largely depends on the voluntary compliance of the public. Given the lack of official regulations and monitoring, its optimal enforcement might be a challenge due to economic and civic rights concerns. Thus, it is important to identify the critical factors that affect the appraisal and endorsement of these measures and take these factors into consideration when developing new policies or measures. This is especially important for Chinese residents in Canada, considering their heightened vulnerability and the lower infection rate in East Asians compared to other ethnical groups [3]. Identifying the factors that contribute to the positive appraisal and active endorsement of the preventive health measures in this population will well inform the development of effective epidemiological regulation policies to battle the virus.
1.1. Chinese Residents in Canada during the Pandemic
According to the 2016 census, there were 1.77 million Chinese Canadians, making up 5.1% of the Canadian population [4]. Chinese communities in Canada exhibit unique experiences and challenges related to COVID-19. During the early stage of the pandemic, most COVID-19 cases in Canada were travel-related; thus, Chinese living in Canada were more vulnerable given their close ties with China, where the first COVID-19 cases occurred. Additionally, they may have experienced social isolation, exclusion, barriers, and stigmas related to using mental health services [5-7]. Thus, Chinese residents may represent a particularly vulnerable population in Canada for the psychological impacts of the pandemic. These challenges are likely to be exacerbated by the quarantine and social distancing practice during lockdowns. Past research reported a higher risk for COVID-19 infection and death in racialized minority groups (e.g., Asian and Black communities) compared to White individuals, likely due to exposure risk factors such as close contact, crowded households, shared spaces or facilities [8-11]. Despite their increased vulnerability, East Asians (particularly Chinese) had a lower infection rate relative to other ethnical groups in Toronto [3]. This urged researchers to identify psychological factors related to the preventive measure appraisal and endorsement in this specific population, which may inform culture-specific public health interventions.
1.2. COVID-19 Perception
Risk perception is the intuitive evaluation of hazardous events based on the event’s characteristics, severity, and management [12]. It is a significant predictor of preventive behaviour endorsement, and risk perception is predicted by socio-cultural and individual factors [12-15]. Research on risk perception and preventive measure endorsement during the early stages of the COVID-19 pandemic has revealed that personal experience with COVID-19, trust in expert and inexpert sources of information, personal and public efficacy of preventive measures, and social amplification of information through family and friends to be significant predictors across multiple countries [12-16]. Additionally, those with direct personal experience of the virus or hold more prosocial worldviews perceived higher risk [13].
A study with American citizens found that preventive measures were more strongly endorsed when people perceived a greater probability of global consequences (i.e., economic recession, reduced healthcare capacity) or were personally infected [14]. Studies with Mainland Chinese residents showed that increased endorsement of public and individual preventive measures was associated with proximity to Wuhan (risk-event), increased risk perception, perceived severity versus susceptibility of contracting the virus, and perceived efficacy of the preventive behaviours at managing the threat was associated with increased endorsement of public and individual preventive measures [16, 17]. Furthermore, trust in policymakers’ concern for the public’s safety and perceived understanding of COVID-19-related news and information attained through expert and inexpert sources were positively associated with endorsing preventive measures [15, 16]. Given their increased vulnerability and lower infection rate [3], Chinese residents in Canada may show different attitudes, risk perceptions, and psychological experiences of the pandemic, which might subsequently impact the appraisal and endorsement of preventive measures. The current study is one of the few highlighting this vulnerable minority population’s experiences during the COVID-19 pandemic.
1.3. Present Study
This study derives from a larger COVID-19 epidemiological research project surveying Chinese residents in Canada during the peak time of the first wave of the COVID-19 pandemic (April 25-June 10, 2020). It adopted a holistic, culturally sensitive, and community-based approach to fill the gap in the literature by examining the effects of psychological perception of COVID-19 (e.g., risk perception and attitudes towards COVID-19) on the appraisal of individual measures and endorsement of public health measures among Chinese living in Canada. The results will inform the identification of high-risk individuals and mitigate the psychological impacts of the pandemic on these individuals.
2. MATERIALS AND METHODS
2.1. Sample
Participants were primarily recruited through WeChat and occasionally through online platforms such as emails, the internet, and social media. For example, it was posted and promoted on the Canadian New Immigrants’ Well-being official website. WeChat was chosen as the major recruitment platform considering that it is the most widely used social media among Chinese worldwide. A total of 1078 respondents attempted to complete the online survey. They were screened with the following inclusion criteria: 1) At least 18 years old and migrated from China (including Mainland, Hong Kong, Taiwan); 2) Lived in Canada for more than four weeks (including citizens, short-term visitors, permanent residents, and international students); and 3) Can read and write Chinese. The respondents who did not meet the screening criteria, refused to consent, or those who did not provide any responses throughout the survey were excluded. As a result, the final sample included 656 eligible and valid respondents.
2.2. The Survey
This online survey aimed to assess the impact of COVID perception on the perceived effectiveness of individual preventive behaviours and endorsement of public preventive measures. It was built in QualitricsTM and delivered in Mandarin to Chinese residents in Canada between April 25th to June 10th in 2020. It collected information related to sociodemographic profiles, attitudes toward the COVID-19 virus, perceived effectiveness of individual preventive behaviours and endorsement of public measures, and the psychological impacts of the pandemic. Given the scope of the current report, the psychological impact results were not reported in this paper. The survey was designed and reviewed by the research team, including professors in epidemiology, public health, psychology, and sociology. The survey included both structured multiple-choice and open-ended text-entry questions.
2.3. Key Variables
2.3.1. Explanatory Variables
The explanatory variables of COVID-19 perception included perceived susceptibility (i.e., “How likely do you think it is that you will contract COVID-19?”), perceived severity (i.e., “Do you believe that the COVID-19 pandemic is a real threat?”), fear (i.e., “Are you personally afraid of contracting COVID-19?”), and confusion about COVID-19 information (i.e., “Do you feel confused or doubtful about the COVID-19 related information you received?”). The responses to these questions were based on a 5-point Likert scale ranging from “1” (most/agree/likely) to “5” (least/disagree/unlikely). These variables were reverse coded so that a higher value would indicate a greater intensity of the negative perception or attitude.
2.3.2. Dependent Variables
The two domains of dependent variables were appraisal (i.e., perceived effectiveness) of the individual preventive behaviours and endorsement of public preventive measures. Perceived effectiveness of individual preventive behaviours was assessed by rating the effectiveness of six behaviours: frequent handwashing, wearing a face mask, disinfection, going out less often, gargling with salt water, and taking vitamin C and/or other supplements, using a 5-point Likert scale from “1” (completely effective) to “5” (completely ineffective). Endorsement of public measures was assessed with five items: school closure/suspension, closure of public facilities and services, work from home, self-isolation at home for patients with mild symptoms, and 14-day quarantine after entering a new region/country. Each item was rated on a 5-point Likert scale from “1” (strongly agree) to “5” (strongly disagree). When appropriate, all responses were reverse coded, with a higher score indicating a more positive appraisal of individual preventive measures or a higher level of endorsement of public measures.
A confirmatory factor analysis was run on the two domains (appraisal and endorsement) of dependent variables. The model fit confirmed a 2-factor structure: Chi-square (n = 521, df = 39) = 59.95, p = .0385; RMSEA = 0.029; CFI = 0.993; SRMR = 0.032. Thus, the mean score for each domain was used as an outcome variable.
2.3.3. Covariates
Sociodemographic covariates were self-reported, including age groups (18-34, 35-44, 45-54, 55-64, ≥ 65), sex (male, female), education (high school/technical school, college, university, graduate school), employment (retired, student, employed, unemployed), income (low, average, high), birthplace (Mainland China, elsewhere), marital status (single/divorced/widowed, married/cohabited), and living arrangement (alone, 2 people, 3-4 people, 5 people or more).
2.4. Statistical Analysis
Since the explanatory variables of attitudes were not normally distributed, the median and interquartile range (IQR) and Wilcoxon mean score of each attitude variable were reported by sociodemographic covariates. The nonparametric Kruskal Wallis test was used to compare the attitudes across all categories of each sociodemographic variable. The two-tailed alpha was set to 0.05. In order to evaluate the prediction of COVID-19 perception on the appraisal of individual preventive behaviours and endorsement of public measures, a covariate-adjusted regression model was implemented with the bootstrap method (n = 10000) to correctly estimate the standard errors of the model. All analyses were done in SAS 9.4 and Mplus 8.2.
3. RESULTS
Most of the participants who completed the demographic questions were Ontario residents (88%), from Mainland China (97%), female (73%), married/cohabited (83%), with a university degree or higher (76%), living in a self-owned house (80%) and with at least 3 people in a household (74%). Approximately half of them have lived in Canada for at least 15 years (50%) and were Canadian citizens (58%). Table 1 presents the sample characteristics of those who completed the questions involved in the final analysis.
| Variables | Class | N | Susceptibility | Fear | Severity | Confusion | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
M (IQR) Mean Score |
p |
M (IQR) Mean Score |
p |
M (IQR) Mean Score |
p |
M (IQR) Mean Score |
p | |||
| Age | 18-34 | 44 | 3.00 (1.50) 211.59 |
0.0019 | 3.00 (1.50) 201.01 |
0.2530 | 4.00 (1.00) 227.24 |
0.6111 | 3.00 (1.00) 210.65 |
0.0968 |
| 35-44 | 76 | 3.00 (1.00) 241.51 |
4.00 (1.00) 238.26 |
4.00 (1.00) 222.89 |
3.00 (1.00) 226.01 |
|||||
| 45-54 | 206 | 3.00 (1.00) 244.25 |
4.00 (1.00) 237.05 |
4.00 (1.00) 225.27 |
3.00 (1.00) 248.48 |
|||||
| 55-64 | 83 | 3.00 (1.00) 235.46 |
4.00 (1.00) 240.35 |
4.00 (1.00) 246.37 |
3.00 (1.00) 212.80 |
|||||
| 65+ | 54 | 3.00 (1.00) 169.48 |
3.50 (2.00) 208.06 |
4.00 (1.00) 243.89 |
3.00 (0.00) 215.88 |
|||||
| Sex | Female | 335 | 3.00 (1.00) 231.43 |
0.4057 | 4.00 (1.00) 236.25 |
0.0441 | 4.00 (1.00) 226.91 |
0.5488 | 3.00 (2.00) 231.13 |
0.5460 |
| Male | 124 | 3.00 (2.00) 220.66 |
3.50 (1.50) 209.54 |
4.00 (1.00) 234.60 |
3.00 (2.00) 223.27 |
|||||
| Education | High School/ Technical School | 38 | 3.00 (1.00) 228.92 |
0.6840 | 4.00 (1.00) 284.87 |
0.0011 | 4.50 (1.00) 247.99 |
0.0025 | 3.00 (2.00) 228.37 |
0.6768 |
| College | 72 | 3.00 (2.00) 221.19 |
4.00 (1.00) 251.90 |
4.00 (1.00) 226.38 |
3.00 (1.00) 239.35 |
|||||
| University | 185 | 3.00 (1.00) 238.41 |
4.00 (1.00) 234.18 |
4.00 (1.00) 252.27 |
3.00 (2.00) 235.51 |
|||||
| Graduate School | 167 | 3.00 (1.00) 224.88 |
3.00 (2.00) 204.70 |
4.00 (1.00) 204.15 |
3.00 (1.00) 221.60 |
|||||
| Employment | Retired | 77 | 3.00 (1.50) 190.38 |
0.0148 | 4.00 (2.00) 213.16 |
0.0569 | 4.00 (1.00) 236.03 |
0.9462 | 3.00 (1.00) 207.65 |
0.1691 |
| Student | 16 | 3.00 (2.00) 202.34 |
3.00 (2.00) 168.53 |
4.00 (1.00) 223.03 |
3.00 (1.00) 192.16 |
|||||
| Employed | 303 | 3.00 (1.00) 239.42 |
4.00 (1.00) 232.46 |
4.00 (1.00) 228.05 |
3.00 (2.00) 235.46 |
|||||
| unemployed | 65 | 3.00 (1.00) 235.98 |
4.00 (1.00) 253.72 |
4.00 (1.00) 233.60 |
3.00 (2.00) 240.53 |
|||||
| Income | Low | 123 | 3.00 (1.00) 229.57 |
0.9163 | 4.00 (1.00) 233.02 |
0.6682 | 4.00 (1.00) 245.85 |
0.1923 | 3.00 (1.00) 216.50 |
0.3883 |
| Average | 202 | 3.00 (1.00) 226.51 |
4.00 (1.00) 232.82 |
4.00 (1.00) 226.41 |
3.00 (1.00) 235.38 |
|||||
| High | 135 | 3.00 (1.00) 232.21 |
4.00 (1.00) 221.21 |
4.00 (1.00) 219.07 |
3.00 (2.00) 232.59 |
|||||
| Birthplace | Mainland China | 446 | 3.00 (1.00) 230.12 |
0.5583 | 4.00 (1.00) 232.32 |
0.0328 | 4.00 (1.00) 230.42 |
0.6910 | 3.00 (2.00) 228.68 |
0.2146 |
| Elsewhere | 15 | 3.00 (2.00) 211.13 |
3.00 (2.00) 161.33 |
4.00 (2.00) 217.63 |
3.00 (1.00) 269.10 |
|||||
| Marital Status | Single/ divorced/widowed |
77 | 3.00 (1.00) 204.38 |
0.0547 | 3.00 (1.50) 214.27 |
0.2498 | 4.00 (1.00) 239.19 |
0.4493 | 3.00 (2.00) 231.28 |
0.8911 |
| Married/cohabited | 382 | 3.00 (1.00) 233.99 |
4.00 (1.00) 232.53 |
4.00 (1.00) 227.57 |
3.00 (2.00) 229.15 |
|||||
| Living Arrangement | Alone | 22 | 3.00 (1.00) 242.05 |
0.9271 | 4.00 (2.00) 237.22 |
0.9679 | 5.00 (1.00) 304.70 |
0.0033 | 3.00 (1.00) 219.77 |
0.1295 |
| 2 people | 98 | 3.00 (1.00) 222.63 |
4.00 (2.00) 224.01 |
4.00 (1.00) 245.08 |
3.00 (1.00) 217.65 |
|||||
| 3-4 people | 250 | 3.00 (1.00) 227.54 |
4.00 (1.00) 228.73 |
4.00 (1.00) 219.64 |
3.00 (1.00) 239.38 |
|||||
| 5 or more | 85 | 3.00 (1.00) 226.50 |
4.00 (1.00) 225.39 |
4.00 (1.00) 210.28 |
3.00 (1.00) 206.06 |
|||||
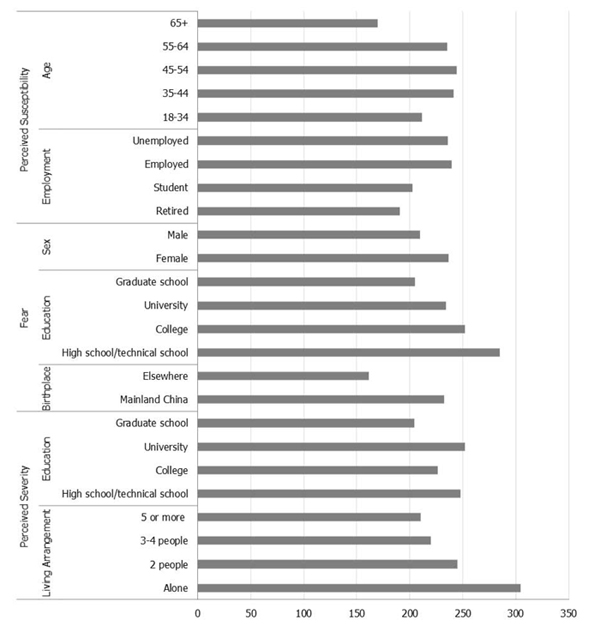
As shown in Table 1 and further illustrated in Fig. (1), the median, interquartile range (IQR), and Wilcoxon mean score of each attitude variable were reported by the sociodemographic variables. The Kruskal Wallis test for each pair of variables showed that compared to their counterpart groups, individuals in older age (65 years or older) or retired reported lower susceptibility (ps ≤ 0.02); females (p = 0.044), those with lower education (p = 0.001), or those born in Mainland China (p = 0.033) were more likely to report a higher level of fear; those in a larger household (p = 0.003) or those with the highest education (p = 0.003) perceived less severity of the pandemic. Confusion about COVID-19 information was not related to any sociodemographic variables. These significant results were also depicted in Fig. (1).
Table 2 shows the adjusted model to evaluate the impact of COVID perception on the health measure appraisal and compliance. After controlling for sociodemographic variables, individual measure appraisal was negatively associated with perceived susceptibility (B[SE]: -0.070 [0.033], p = 0.032) and positively associated with perceived severity (B[SE]: 0.116 [0.041], p = 0.005). Compared to males, females showed more positive appraisal of individual behaviours (B[SE]: 0.136 [0.062], p = 0.029). Those with a university or graduate degree showed a lower appraisal compared to high school graduates (B[SE]: -0.306 [0.113], p = 0.007; -0.350 [0.122], p = 0.004, respectively). Those born in Mainland China perceived the individual measures as more effective compared to those born elsewhere (B [SE]: 0.330 [0.107], p = 0.002).
After controlling for sociodemographic variables, public preventive measure endorsement was only positively associated with perceived severity (B[SE]: 0.148 [0.038], p < .001). Lower measure endorsement was found in mid-aged (i.e., 45-54 years of age) compared to older adults (i.e., 65 years and above), B[SE]: -0.281 (0.141), p = 0.047. Those who were employed showed a stronger measure endorsement relative to those who were retired, B[SE]: 0.240 [0.117], p = 0.040.
| Variables | Levels | Individual Measure Appraisal | Public Measure Endorsement | ||
|---|---|---|---|---|---|
| B (SE) | p | B (SE) | p | ||
| Susceptibility | -0.070 (0.033) | 0.032 | -0.023 (0.029) | 0.422 | |
| Severity | 0.116 (0.041) | 0.005 | 0.148 (0.038) | <.001 | |
| Fear | 0.054 (0.031) | 0.078 | 0.010 (0.027) | 0.699 | |
| Confusion | 0.016 (0.031) | 0.607 | -0.042 (0.029) | 0.141 | |
| Age | 18-34 | -0.126 (0.218) | 0.563 | -0.175 (0.158) | 0.268 |
| 35-44 | -0.191 (0.223) | 0.394 | -0.179 (0.154) | 0.245 | |
| 45-54 | -0.257 (0.220) | 0.243 | -0.281 (0.141) | 0.047 | |
| 55-64 | -0.146 (0.177) | 0.407 | -0.203 (0.123) | 0.099 | |
| 65+ (Ref) | 0 | 0 | |||
| Sex | Male (Ref) | 0 | 0 | ||
| Female | 0.136 (0.062) | 0.029 | 0.070 (0.063) | 0.265 | |
| Education | High school/Technical school (Ref) | 0 | 0 | ||
| College | -0.188 (0.124) | 0.128 | -0.028 (0.102) | 0.785 | |
| University | -0.306(0.113) | 0.007 | -0.090 (0.093) | 0.332 | |
| Graduate school | -0.350 (0.122) | 0.004 | -0.011 (0.100) | 0.912 | |
| Employment | Retired (Ref) | 0 | 0 | ||
| Student | -0.109 (0.224) | 0.626 | 0.151 (0.235) | 0.519 | |
| Employed | 0.208 (0.182) | 0.255 | 0.240 (0.117) | 0.040 | |
| Unemployed | 0.169 (0.203) | 0.405 | 0.193 (0.138) | 0.163 | |
| Income | Low (Ref) | 0 | 0 | ||
| Average | 0.026 (0.071) | 0.719 | -0.042 (0.060) | 0.482 | |
| High | 0.052 (0.081) | 0.520 | -0.003 (0.070) | 0.961 | |
| Birthplace | Mainland China | 0.330 (0.107) | 0.002 | 0.240 (0.138) | 0.082 |
| Elsewhere (Ref) | 0 | 0 | |||
| Marital Status | Married/cohabited (Ref) | 0 | 0 | ||
| Single/divorced/widowed | -0.074 (0.084) | 0.382 | -0.056 (0.086) | 0.515 | |
| Living Arrangement | Alone (Ref) | 0 | 0 | ||
| 2 people | 0.037 (0.174) | 0.830 | 0.047 (0.125) | 0.709 | |
| 3-4 people | 0.043 (0.164) | 0.792 | 0.057 (0.123) | 0.641 | |
| 5 or more | -0.049 (0.176) | 0.782 | 0.104 (0.135) | 0.441 | |
4. DISCUSSION
The present study aimed to understand the effect of risk perception and attitudes toward COVID-19 on preventive measure appraisal and endorsement among Chinese living in Canada. It was found that older adults or those retired reported less susceptibility to the virus. Females, those with higher education, or those with non-student employment status, and those born in Mainland China, reported a higher level of fear towards COVID-19 compared to their counterpart groups. Those living in households with larger sizes and with higher education levels perceived less severity of the pandemic. Overall, the individual measure appraisal was negatively associated with perceived susceptibility and positively associated with perceived severity of COVID-19, whereas public measure was positively associated with perceived severity. Females, those born in Mainland China, or those with lower education tend to show higher individual measures appraisal. Being 65 years of age and above (versus aged 45-54), presently being employed (versus retired) were associated with higher endorsement of public preventive measures.
A higher level of perceived susceptibility was related to lower individual measure appraisal but had no impact on the public measure endorsement, suggesting that high-risk perception might call for more strict and effective measures in place and thus make them devalue the effectiveness of the existing individual measures. Driven by their collective cultural value, the Chinese endorsed the public health measures equally well regardless of their personal infection risk perception. This speculation, however, needs to be further tested.
Increased perception of personal threat (severity) predicts both higher individual measure appraisal and higher public measure endorsement. This supports research on the Extended Parallel Process Model (EPPM) in that increased risk perception could act as a motivating factor when associated with increased efficacy of preventive measures [18, 19]. Increased severity perception can serve as a motivational factor to endorse preventive measures to prevent potential losses [16, 20, 21]. The higher severity was reported by those living alone and those with lower education relative to their corresponding counterpart groups. Presumably, individuals living in larger households might have more social or family support, which may mitigate their negative affective responses, such as feelings of loneliness and anxiety [22, 23], thus reducing their severity perception. Higher education may increase the overall sense of agency, which may reduce their perceived vulnerability to environmental threats [5, 6].
Participants from Mainland China reported a higher level of fear and rated the individual behaviour measures as more effective compared to those born elsewhere. This might be due to the social amplification of COVID-19 information from friends and family in the homeland, which may affect the attitudes of Chinese living in Canada [13]. Moreover, the heightened fear in Mainland Chinese echoes the previous finding of increased fear and risk perception with increased proximity to Wuhan, the original outbreak city [17]. Participants may experience a psychological closeness to the homeland, which may have elicited similar risk perceptions [17, 24, 25]. Another factor to consider is the social stigma that might affect preventive behaviour endorsement. Since the declaration of COVID-19 as a global pandemic, there has been an increase in racialized discrimination towards Chinese individuals in Canada and the United States [7, 26-28]. It could be that there is an increased level of fear resulting from the threat of racialized assaults that are compounded with the perceived threat of the COVID-19 virus.
It should be noted that this study also has some limitations. First, data were collected using a self-report method. Therefore the reliability of the responses needs to be considered when interpreting the results. Moreover, using an online survey may increase the likelihood of a sampling bias as some people may not have access to computers or a reliable internet connection. The study also did not assess a range of affective states. Instead, it primarily focused on fear as it related to preventive behaviour endorsement. Future studies may follow up to examine how other affective states, such as anxiety or worry, relate to risk perception and endorsement of preventive behaviours.
CONCLUSION
Individual behaviour measure appraisal was predicted by lower perceived susceptibility and higher perceived severity, whereas public health measure endorsement was related to higher perceived severity. These results inform the public and the policymakers about the critical factors that affect the preventive measure appraisal and endorsement.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by Ryerson University [REB 2020-132] and Memorial University of Newfoundland [20201772-ME].
HUMAN AND ANIMAL RIGHTS
No animals were used for the study that is the basis of this research. All the human procedures were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from each participant included in this study.
STANDARDS OF REPORTING
STROBE guidelines and methodologies were followed for this study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
This work was funded by the New Frontiers Research Fund through the Canadian Institute of Health Research (CIHR) and the Social Sciences and Humanities Research Council (SSHRC) [NFRF-2019-00012] awarded to Dr. Peizhong Peter Wang and Dr. Lixia Yang.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the support from the Centre for New Immigrants Well-being (CNIW, collaborator), Confederation of Chinese Alumni Associations (CCAA, knowledge user), and other supporting organizations. We would like to thank the project coordinator, Ying Cao, for her diligent support in participant recruitment and data collection. In addition, we would like to thank all our research participants for taking the time to complete the survey.


