All published articles of this journal are available on ScienceDirect.
A Validation and Feasibility of a Questionnaire to Assess Literacy, Fear, Hesitancy, and Acceptance of COVID-19 Vaccine in Thailand
Abstract
Introduction:
Few studies have developed tools to evaluate COVID-19 vaccine literacy (VL), especially in Asia. In this study, an online tool was utilized to assess COVID-19 VL, vaccine fear (VF), vaccine hesitancy (VH), and vaccine acceptance (VA) among village health volunteers (VHVs) in Thailand.
Methods:
A cross-sectional online questionnaire was distributed to 210 VHVs between 10th to 14th September, 2021 to assess their VL, VF, VH, and VA levels. Item objective congruence (IOC) and Cronbach’s alpha were used to estimate the validity and reliability of the questionnaire. The two-independent sample t-test, Wilcoxon rank-sum test, ANOVA, and the Kruskal-Wallis test were employed to compare differences between the scores. Pearson correlation and Spearman’s rank correlation were used to estimate the correlation of the scores.
Results:
The online questionnaire showed high validity, with IOC values over 0.70 and reliability over 0.87 for all items. Median scores of VL, VF, and VH for the 210 participants were high (VL 2.92 and VF 2.5 out of a maximum of 4, and VH 2.43 out of a maximum of 5). The mean VA score was low (0.21 out of a maximum of 1) and significantly different between demographic variables. A significant correlation was found between VL and VH and VF and VA.
Conclusion:
The online questionnaire showed high values of validity and reliability. This tool proved to be beneficial for evaluating VL, VF, VH, and VA in Thailand. Further studies using a larger population are required to verify these results.
1. INTRODUCTION
Coronavirus disease 2019 (COVID-19) has caused panic, impacted mental health, and disrupted healthcare systems worldwide [1-3]. The new COVID-19 variant (Delta) spreads rapidly with greater transmissibility [4]. By October, 2021, the Department of Medical Science confirmed that 76 out of 77 provinces in Thailand had recorded cases of COVID-19 with the Delta variant [5]. Over 10,000 new COVID-19 cases have been reported in Thailand since July, 2021, with an average of 100 deaths per day [6].
Many countries have promoted COVID-19 vaccination campaigns to contain the virus and attain the concept of herd immunity. Globally, 34% of the population has been fully vaccinated. In Thailand, however, this proportion is only 23% [7]. There is an urgent need to improve the public ability to detect fake news and promote health literacy of vaccine benefits against SARS-CoV-2 [8].
Health literacy reflects the capacity to gain access to, understand, and use health information in ways that promote and maintain good health [9]. However, gaining information regarding vaccines requires certain literacy skills. Previous studies developed and applied the concept of health literacy to create tools for vaccine literacy (VL) comprising functional, interactive, and critical elements. The validity and feasibility of a vaccine literacy tool were demonstrated by studies conducted in Italy and Croatia [10, 11].
Improved health literacy may increase vaccination acceptance (VA) [8]. However, the COVID-19 vaccines are developing at a very fast pace; therefore, some safety concerns still remain, resulting in vaccine hesitancy (VH) among the public [12]. Inevitably, another consequence of the COVID-19 pandemic is vaccine fear (VF).
Fear is a condition commonly associated with infectious diseases. Pappas et al. demonstrated a direct association between the speed and invisibility of disease transmission and its morbidity and mortality [13], while a study in Austria demonstrated that people also dread the consequences of vaccination [14]. Moreover, high levels of fear and anxiety may affect thinking processes and how to react to COVID-19 [13]. Several studies applied tools to assess the fear of COVID-19, while Ahorsu et al. developed a Fear of COVID-19 Scale [15-17].
In Thailand, village health volunteers (VHVs) are responsible for public COVID-19 control. These VHVs are hailed as “unsung heroes” by the World Health Organization (WHO) [18]. In 2021, when the first vaccines arrived in Thailand, the Thai prime minister encouraged village health volunteers to increase public trust in the COVID-19 vaccination program. Hence, there is a need to obtain and communicate vaccine information, especially by VHVs [19].
As aforementioned, it is necessary to estimate COVID-19 VL, VF, VH, and VA among VHVs at different times using separate tools. Such a study has never been performed in Thailand, especially regarding vaccine literacy.
This study developed and validated a comprehensive questionnaire as a tool to evaluate COVID-19 VL, VF, VH, and VA among 210 VHVs in Thailand.
2. MATERIALS AND METHODS
2.1. Study Design and Settings
A cross-sectional study was conducted between 10th to 14th September, 2021 among VHVs in Thailand. Social media, namely Line and Facebook, were used for data gathering. The 40-item questionnaire was prepared using Google Forms (in the Thai language), available at https://1th.me/wMgHw.
2.2. Study Sample and Data Collection
Eligible study participants were VHVs over 18 years old who had registered for the mobile application SMART VHV. This study was conducted in provinces representing regions of Thailand as Chiang Mai for North, Ubon Ratchathani and Udon Thani for Northeast, Chonburi for East, Songkhla for South, and Bangkok for Central. The total number of eligible study participants in 2021 was 11,690. The sample size was calculated based on estimating a finite population means [20]. Given a population of 11,690, a standard deviation of 0.71, determined error of 0.1 and alpha of 0.05, the required sample size was determined as 191. An additional 10% was added to compensate for loss, giving a final sample size of 210.
2.3. Instruments and Measurements
The self-rated questionnaire asked about demographic characteristics, COVID-19, vaccine literacy (VL), fear (VF), hesitancy (VH), and acceptance (VA). Questionnaires, including a research information sheet and informed consent form, were made available to study subjects online using Google Form. Details of the instruments, tools, and measurements are presented below.
2.4. Demographic Data
Demographic data were categorized to identify sex, age, educational level, marital status, religion, occupation, medical condition, family income, and work experience.
2.5. Vaccine Literacy (VL)
The VL score was originally based on “health literacy” (HL), a self-rated questionnaire specific to village health volunteers (VHVs), including three health literacy scales [9, 10]. The questions were specifically adapted to the vaccination domain and cultural characteristics of the Thai population. Vaccine literacy comprised 12 items (questions) divided into three scales, functional VL (items l1 to l5), interactive, also called communicative VL (items l6 to l10), and critical VL (items 11 to 12). Functional VL questions concerned language capabilities involving the semantic system, while other questions addressed interactive/critical VL, such as problem-solving and decision-making. Answers were given by the interviewee according to a Likert scale with four possible choices as 4-never, 3-rarely, 2-sometimes, and 1-often.
2.6. Vaccine Fear (VF)
The fear of COVID-19 scale (FCoV-19S) with 5 items was applied to evaluate the VF score [15-17]. Participants rated their perception of susceptibility to COVID-19 infectability on a 4-point Likert scale ranging as 4-never, 3-rarely, 2-sometimes, and 1-often. The total score was calculated by adding each item score (ranging from 5 to 20). A higher score represented a higher level of COVID-19 VF.
2.7. Vaccine Hesitancy (VH)
The VH score was modified from the Vaccine Hesitancy Scale (VHS) developed by Akel, Kb et al. [21]. Vaccine hesitancy consisted of 7-items assessed on a 5-point Likert scale with answer choices ranging from 1 to 5 as 5-strongly disagree, 4- disagree, 3-neutral, 2-agree and 1-strongly agree. The total score was calculated by adding each item score (ranging from 7 to 35). The higher the score, the greater the COVID-19 VH.
2.8. Vaccine Acceptance (VA)
The VA score was developed based on the literature review. The final version of the questionnaire had 6 items that collected information regarding COVID-19 VA. The questionnaire comprised a 3-point Likert scale ranging from 1 to 3 as 1-yes, -1-no and 0-not sure for 1-6 items.
All the questionnaires were developed in the Thai language, and the items were evaluated for content validity. Three experts, including one doctor, one nurse, and one researcher with extensive experience in health literacy, were invited to review the questionnaire for content validity. Content validity refers to whether or not the content of the scale is capable of measuring what it is intended to measure as the defined objective. The quantitative content validity of the questionnaire as the index of item objective congruence (IOC) was more than 0.7 for all items. The reliability of the VL, VF, VH, and VA questionnaires was tested on 30 participants and evaluated using Cronbach’s alpha, with results of 0.85, 0.86, 0.85, and 0.86, respectively.
The online questionnaire was distributed via the social media platforms Line and Facebook. These two social media are the most popular in Thailand and are used by VHVs to communicate and coordinate with each other. The research purpose was explained to the area VHV leaders, who then distributed the questionnaire to their Line or Facebook groups and asked their VHVs to complete the questionnaire. The study subjects were initially screened for inclusion criteria, including age and registration for the mobile application SMART VHV. If they were eligible to participate, they signed the informed consent form by clicking on it, and the structured questionnaire then appeared on their device screens. In this study, all questionnaires were completed by participants. As we have specified in the google form, respondents would not be able to submit if they did not answer all of the questions. Completed questionnaires were submitted via the online platform Google Form. The survey took about 10 minutes to complete. All completed questionnaires were stored via Google Form.
2.9. Statistical Analysis
Descriptive statistics were used to report data as numbers and percentages, while continuous data were summarized as means with standard deviations or medians with interquartile range (Q1, Q3).
The validity and reliability of the questionnaire were assessed by IOC and Cronbach’s alpha. Principle component analysis (PCA) was performed to identify items that showed the highest data variability.
Differences in mean demographic variable scores of VL, VF, VH, and VA were first tested for normal distribution using the Kolmogorov-Smirnov test and variance equality test. Then, the two-independent sample t-test or Wilcoxon ranked-sum test were applied for variables with normal distribution and non-normal distribution, respectively. For multiple group comparisons of variables with normal distribution, ANOVA was used, while the Kruskal-Wallis test was used for variables with a non-normal distribution. Correlations between VL, VF, VH, and VA scores and age were examined using the Pearson correlation and Spearman’s rank correlation where appropriate. Statistical significance was set at p<0.05. All analyses were conducted using Stata version 15.
3. RESULTS
3.1. Demographic Characteristics, VL, VF, VH, and VA Scores among VHVs
In total, 210 VHVs completed the online survey via Google Form. Most were female (87.14%) with an average age of 53 years. The average length of VHV service and income was 11.87 years and 16,654.22 Thai baht, respectively. Higher proportions of education lower than bachelor's degree (85.24%), no comorbidity (61.26%), couples (64.42%), business owners (84.82%), and Buddhism (91.90%) were found in categories of education, comorbidity, marital status, occupation, and religion.
Vaccine literacy, fear, hesitancy, and acceptance scores averaged 2.85 (SD: 0.59), 2.68 (SD: 0.95), 2.51 (SD: 0.86), and 0.21 (SD: 0.46), respectively, while sub-domains of literacy score as functional, interactive, and critical averaged 2.98 (SD: 0.65), 2.65 (SD: 0.64) and 3.05 (SD: 0.82), respectively (Table 1).
| Variable | N (%) | Mean SD | Median (Q3-Q1) |
|---|---|---|---|
| Age (years) | - | 53.02 (11.70) | 53 (15) |
| Income (baht/month) | - | 16,654.22 (58,920.51) | 10,000 (10,500) |
| VHV service (years) | - | 11.87 (9.20) | 10 (12) |
| Sex | |||
| Female | 183 (87.14) | - | - |
| Male | 27 (12.86) | - | - |
| Education | |||
| < bachelor | 179 (85.24) | - | - |
| >= bachelor | 31 (14.76) | - | - |
| Comorbidity | |||
| No | 117 (61.26) | - | - |
| Yes | 74 (38.74) | - | - |
| Marital status | |||
| Single, alone or widowed |
74 (35.58) | - | - |
| Couple | 134 (64.42) | - | - |
| Occupation | |||
| Business owner | 162 (84.82) | - | - |
| Employee | 29 (15.18) | - | - |
| Religion | |||
| Buddhism | 193 (91.90) | - | - |
| Other | 17 (5.71) | - | - |
| Literacy score | - | 2.85 (0.59) | 2.92 (2.5, 3.25) |
| Functional literacy | - | 2.98 (0.65) | 3 (2.6,3.4) |
| Interactive literacy | - | 2.65 (0.64) | 2.6 (2.2, 3) |
| Critical literacy | - | 3.05 (0.82) | 3 (2.5,4) |
| Fear score | - | 2.68 (0.95) | 2.5 (1.8, 3.56) |
| Hesitancy score | - | 2.51 (0.86) | 2.43 (2, 3.14) |
| Acceptance score | - | 0.21 (0.46) | 0.2 (-0.2, 0.6) |
3.2. Reliability between Evaluators and VHVs
The questionnaire was tested using 30 evaluators before implementation with 210 VHVs. Table 2 shows high consistency of Cronbachʼs alpha values between both groups for literacy (0.85, 0.86), fear (0.85, 0.86), hesitancy (0.86, 0.86) and acceptance (0.85, 0.87).
Cronbachʼs alpha values of VHAs (n=210) were higher than for the evaluators (n=30) as 0.860 for VL, 0.858 for VF, 0.863 for VH, and 0.869 for VA. Cronbach’s alpha values of functional, interactive, and critical literacy were 0.850, 0.853, and 0.846, respectively.
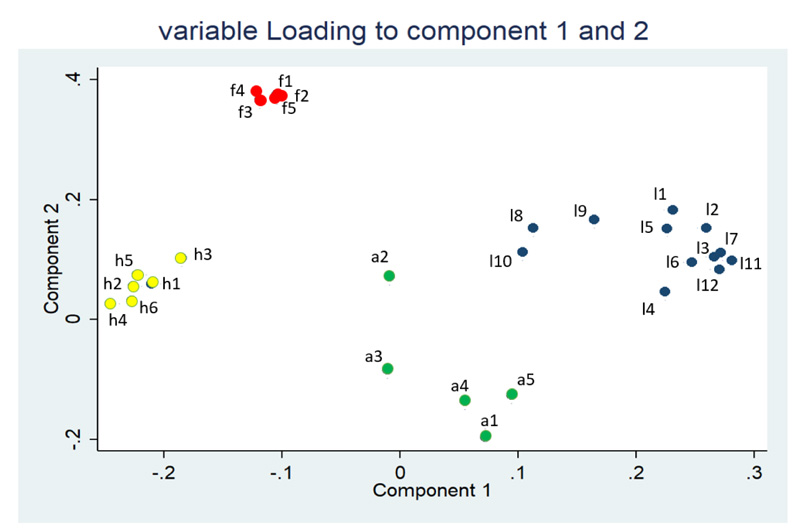
PCA was performed to identify items that showed the highest data variability. Most item domains were classified between two main components (Fig. 1).
| Item | Cronbach’s alpha | |
|---|---|---|
| n=30 | n=210 | |
| Literacy | 0.85 | 0.86 |
| Functional | 0.85 | 0.85 |
| Interactive | 0.85 | 0.85 |
| Critical | 0.85 | 0.85 |
| Fear | 0.85 | 0.86 |
| Hesitancy | 0.86 | 0.86 |
| Acceptance | 0.85 | 0.87 |
| Total | 0.85 | 0.87 |
3.3. Different Scores of Vaccine Literacy, Fear, Hesitancy, and Acceptance Variables
Significantly different VL, VF, and VA scores were found among age groups, while the VA score also showed significance for marital status, occupation, and religion variables. Single, alone or widowed had a higher VA score than a couple (mean difference 0.14; 95% CI: 0.01 to 0.27). VHVs who were employees had higher scores than business owners (mean difference 0.24; 95%CI: -0.42 to -0.05), while Buddhism also had a higher VA score than other religions (mean difference 0.36; 95%CI: -0.58 to -0.13). Most (92%) of the VHVs were Buddhists. Vaccine fear had a significantly different median score only in the occupation category, suggesting that business owners had higher VF than their employees (median difference: 0.56; 95%CI: 0.16 to 0.72). No score differences were recorded for VH. Results are shown in Table 3.
| Literacy | Fear | Hesitancy | Acceptance | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | N | Median (95%CI) | 95%CI diff | p-value | Median (95%CI) | 95%CI diff | p-value | Median (95%CI) | 95%CI diff | p-value | Mean (95%CI) | 95%CI diff | p-value |
| Age | |||||||||||||
| <40 | 30 | 2.67 (2.43-2.90) |
NA | <0.001 | 2.82 (2.4, 3.43) |
NA | 0.018 | 2.36 (2, 2.86) |
NA | 0.690 | -.04 (-0.20, 0.13) |
NA | 0.007* |
| 40-49 | 57 | 2.75 (2.5-2.91) |
NA | 0.0003(l1) | 2.6 (2.10, 3.17) |
NA | 0.0067(f1) | 2.43 (2.08, 3.06) |
NA | 0.21 (0.08, 0.34) |
NA | 0.0194(a1) | |
| 50-59 | 61 | 3.08 (3-3.25) |
NA | 0.0267(l2) | 2.8 (2.28, 3.25) |
NA | 0.0263(f2) | 2.28 (2, 2.57) |
NA | 0.23 (0.11, 0.34) |
NA | 0.0103(a2) | |
| >60 | 62 | 2.96 (2.75, 3.08) |
NA | 0.0394(23) | 2.18 (1.87, 2.37) |
NA | 0.0138(f3) | 2.43 (2.14, 3) |
NA | 0.32 (0.22, 0.43) |
NA | 0.0002(a3) | |
| Working years | |||||||||||||
| <10 | 103 | 2.83 (2.75, 3) |
NA | 0.843 | 2.6 (2.4, 2.92) |
NA | 0.098 | 2.43 (2.28, 2.85) |
NA | 0.525 | 0.20 (0.11, 0.29) |
NA | 0.872 |
| 10-20 | 66 | 3 (2.75, 3.08) |
NA | 2.6 (2.18, 3.10) |
NA | 2.21 (2, 2.93) |
NA | 0.23 (0.12, 0.35) |
NA | ||||
| >=20 | 41 | 2.92 (2.75, 3.11) |
NA | 2.16 (1.71, 2.81) |
NA | 2.14 (2, 2.80) |
NA | 0.22 (0.08, 0.36) |
NA | ||||
| Sex | |||||||||||||
| Female | 183 | 3 (2.58, 3.17) |
-0.25, 0.25 | 0.73 | 2.56 (2.07, 3.68) |
-0.20, 0.56 | 0.324 | 2.28 (2, 3) |
-0.28, 0.43 | 0.540 | 0.21 (0.15, 0.28) |
-0.19, 0.18 | 0.952 |
| Male | 27 | 2.92 (2.83, 3) |
2.48 (2.26,2.80) | 2.43 (2.14, 2.57) |
0.21 (0.03, 0.38) | ||||||||
| Education | |||||||||||||
| Below bachelor’s degree | 179 | 2.92 (2.82, 3) |
-0.33, 0.083 | 0.25 | 2.52 (2.20, 2.80) | -0.40, 0.28 | 0.673 | 2.43 (2.14, 2.59) |
-0.28, 0.28 | 0.984 | 0.22 (0.15, 0.21) |
-0.15, 0.21 | 0.740 |
| Bachelor’s degree or above | 31 | 2.83 (2.75, 3.25) |
2.44 (1.98,3.24) | 2.43 (2, 3) | 0.19 (0.06, 0.27) |
||||||||
| Comorbidity | |||||||||||||
| No | 117 | 2.83 (2.75,3) |
-0.25, 0.083 | 0.261 | 2.4 (2.08,2.65) | -0.44, 0.08 | 0.213 | 2.43 (2.14, 2.80) |
-0.14, 0.28 | 0.486 | 0.21 (0.12, 0.30) |
-0.15, 0.13 | 0.901 |
| Yes | 74 | 3 (2.83, 3.17) |
2.8 (2.2, 3.27) | 2.29 (2.14, 2.71) |
0.22 (0.13, 0.31) |
||||||||
| Marital status | |||||||||||||
| Single, alone or widowed | 74 | 3 (2.75,3.17) |
0, 0.25 | 0.134 | 2.3 (2, 2.67) |
-0.48, 0 | 0.064 | 2.43 (2.15, 2.71) |
-0.14, 0.28 | 0.538 | 0.31 (0.20, 0.41) |
0.01, 0.27 | 0.037** |
| Couple | 134 | 2.87 (2.75,3) |
2.64 (2.4, 3.03) |
2.28 (2.14, 2.57) |
0.17 (0.09, 0.25) |
||||||||
| Occupation | |||||||||||||
| Business owner | 162 | 2.92 (2.83, 3) |
-0.16, 0.25 | 0.759 | 2.56 (2.28, 2.92) |
0.16, 0.72 | 0.01 | 2.43 (2.14, 2.57) |
-0.57, 0.14 | 0.151 | 0.19 (0.12, 0.27) |
0.05, 0.42 | 0.01** |
| Employee | 29 | 2.83 (2.56, 3.17) |
2 (1.65, 2.57) |
3 (2.86, 3.14) |
0.43 (0.26, 0.6) |
||||||||
| Income | |||||||||||||
| <10,000 baht | 104 | 2.96 (2.75, 3) |
-0.17, 0.17 | 0.99 | 2.76 (2.34, 3.28) |
-0.04, 0.44 | 0.130 | 2.43 (2.14, 2.86) |
-0.14, 0.28 | 0.455 | 0.16 (0.07, 0.25) |
-0.22, 0.23 | 0.111 |
| >10,000 baht | 106 | 2.87 (2.75, 3) |
2.4 (2.12, 2.65) |
2.43 (2.14, 2.57) |
0.26 (0.18, 0.35) |
||||||||
| Religion | |||||||||||||
| Buddhism | 193 | 2.97 (2.93, 3) |
-0.5, 0.83 | 0.191 | 2.44 (2.2, 2.72) |
-0.24, 0.68 | 0.316 | 2.28 (2, 3.28) |
-0.28, 0.57 | 0.650 | 0.24 (0.18, 0.30) |
0.13, 0.58 |
0.002** |
| Other | 17 | 2.67 (2.42, 3) |
2.84 (2/16, 3.40) |
2.43 (2.18, 2.57) |
-0.12 (-0.36, 0.13) |
||||||||
3.4. Correlation of Vaccine Literacy, Fear, Hesitancy, Acceptance, and Age
The correlation between VL, VF, VH, VA and age was also investigated using simple correlation analysis (Table 4). A positive correlation was shown between Age and VL (r=0.1910). VL and VH, VA and VF, Age and VF, and Age and VA had a negative correlation with rho values - 0.389, - 0.2669, -0.1919 and 0.2654, respectively.
| Literacy | Fear | Hesitancy | Acceptance | Age | ||
|---|---|---|---|---|---|---|
| Literacy | rho (95%CI) | 1 | ||||
| p-value | ||||||
| n | 210 | |||||
| Fear | rho (95%CI) | 0.0809 (-0.055 to 0.214) |
1 | |||
| p-value | 0.2428 | |||||
| n | 210 | 210 | ||||
| Hesitancy | rho (95%CI) | - 0.389 * (-0.498 to -0.268) |
0.1170 (-0.019 to 0.248) |
1 | ||
| p-value | 0.001 | 0.0909 | ||||
| n | 210 | 210 | 210 | |||
| Acceptance | rho (95%CI) | 0.1041 (-0.032 to 0.236) |
- 0.2669* (-0.388 to -0.136) |
-0.0365 (-0.171 to 0.099) |
1 | |
| p-value | 0.1328 | 0.0001 | 0.5984 | |||
| n | 210 | 210 | 210 | 210 | ||
| Age | rho (95%CI) | 0.1910* (0.057 to 0.318) |
-0.1919* (-0.319 to -0.058) |
-0.0377 (-0.172 to 0.098) |
0.2654* (0.135 to 0.387) |
1 |
| p-value | 0.0055 | 0.0053 | 0.5873 | 0.0001 | ||
| n | 210 | 210 | 210 | 210 | 210 |
4. DISCUSSION
Several studies have assessed fear, hesitancy, and acceptance of COVID-19 [12, 14-17], but none of the studies have evaluated vaccine literacy among VHVs, especially in Thailand. VHVs are important intermediate communicators between healthcare professionals and people that deliver health information directly to villages. During the COVID-19 pandemic, VHVs played an important role in screening, quarantine, and basic care, resulting in early detection and greater public knowledge by encouraging COVID-19 vaccination in Thai communities [22, 23]. Here, a questionnaire was developed to cover COVID-19 vaccine literacy, fear, hesitancy, and acceptance. To the best of our knowledge, this is the first study to evaluate COVID-19 vaccine literacy among VHVs in Thailand. The developed tool showed high validity and reliability for all items, with an overall Cronbach’s alpha value of 0.87. The study found high average scores for vaccine literacy, fear, and hesitancy but low acceptance scores.
The structured questionnaire also gave high validity and reliability at above 0.87 for all dimensions (literacy, fear, hesitancy, and acceptance), concurring with the findings of Biasio et al. and Gusar et al. [10, 11]. Biasio et al. developed a novel tool that examined VL, referred to as the Health Literacy Vaccinale degli adulti in Italiano (HLVA-it). They reported Cronbach’s alpha values for functional, interactive, and critical vaccine literacy as 0.8814, 0.9021, and 0.9369, respectively. Here, questions in the vaccine literacy section were based on the tool of Biasio et al., giving Cronbach’s alpha values of functional, interactive, and critical literacy as 0.860, 0.863, and 0.8570, respectively. This implied that the questionnaire was feasible for application in the Thai community. However, item loading of vaccine literacy favored by PCA gave a different result from Biasio et al. and Gusar et al.
The Italian study by Biasio et al. showed that interactive and critical vaccine literacy both had high loading on component 1, while functional vaccine literacy had higher loading on component 2 [10]. Similarly, the Croatian study by Gusar et al. showed that interactive and critical vaccine literacy were dominant in component 1, while functional vaccine literacy had high loading on component 2 [11]. In our study, functional and critical vaccine literacy had a higher contribution to component 1, while interactive vaccine literacy showed high loading on component 2 (Supplementary data Table S1). These different major loadings of items among the population suggested that vaccine literacy varied by population and country. Hence, vaccine literacy evaluation among a specific population was required.
The average literacy score among VHVs was over 2.5, similar to previous studies [10, 11, 24, 25]. The high literacy score possibly resulted from the examination of mostly healthy people with non-severe diseases. VHVs are not official healthcare professionals. Their duties include updating the public with the latest COVID-19 information during the vaccination campaign launched in late February, 2021 [(19)]. The prime minister of Thailand tasked the VHVs to boost acceptance of the COVID-19 vaccine in local Thai communities [26]. Our interactive VL scores were lower than the functional and critical scores. Cherif et al. used a cut-off value of 2.5 to classify high and low VL and found low VL in cancer patients in Tunisia [27]. Interactive VL scores in our study were higher than 2.5. Health literacy is a vital ability for accurately analyzing health information; higher levels of health literacy were linked to improved health status [16]. Health literacy and vaccine literacy both require individuals to assimilate the applicable information and make an informed vaccination decision [28]. The concept of vaccine literacy is similar to health literacy and is defined as “not simply knowledge about vaccines but also about developing a system with decreased complexity to communicate and offer vaccines as a sine qua of a functioning health system” [29, 30]. Furthermore, VL is also relevant to health promotion and can be defined as the process of empowering individuals to take care of their health [30, 31]. Therefore, vaccine literacy among VHVs focused on interactive skills that reflected the ability to interact with healthcare providers and interpret the information delivered to the public [31].
Different scores of VL, VF, VH, and VA were also examined by characteristic variables. Higher age had significantly better average VL scores. This finding was inconsistent with previous studies [11, 24]. Baker et al. concluded that functional vaccine health literacy declined with increasing age [31]. A possible explanation for our results was the study population of VHVs who had registered for the mobile applications “SMART Village Health Volunteer” and “Aor Sor Mor Online” that served many functions, including getting news, updating the COVID-19 pandemic situation, and supporting knowledge regarding COVID-19 prevention and vaccination. Users can also share advantageous information in the form of texts, images, audio, and video. VHVs work closely with community leaders, networks, and officers [32]. Therefore, all participants were able to access information. Our study recruited VHVs with a median age of 53 years (Q1: 46; Q3: 61). A previous study with a large sample size revealed that adults less than 69 years old showed a non-significant increased risk of health literacy decline compared to those aged 52 years old [33], concurring with our result of higher literacy among older age groups.
Fear of adverse effects from the COVID-19 vaccine is one of the major problems that obstruct vaccine uptake [34]. The average VF score was 2.68 out of a maximum of 4. A higher score means higher fear of the COVID-19 vaccine. Our VF score concurred with a study in Vietnam at 60% of the maximum score; however, the Vietnamese study focused on fear of SARS-CoV-2 rather than the vaccine [17]. This finding was similar to a study in Bangladesh by Hossain et al., who reported moderate to high fear levels, with a mean fear score of 18.53 out of 35 (S.D.=5.013) [35]. Fitzpatrick et al. examined the relationship between COVID-19 fear and social vulnerabilities as well as mental health repercussions in people in the United States. They found that respondents were fearful, with an average score of nearly 7 on a scale of 10 [36]. Several studies concluded that fear and stress caused insomnia and mental disorders [35-37]. Our fear scores significantly differed among age groups. People less than 40 years old were more fearful than those over 60, while some studies revealed that older adults had higher levels of fear than younger adults [35, 38, 39], and many indicated a decline in fear in older adults and argued that aging was a protective factor [40-43].
Vaccines available in Thailand (as of October, 2021) include the inactivated virus Sinovac (CoronaVac) (SV) and the adenoviral vector AstraZeneca (ChAdOx1nCoV-19), (AZ) [44]. Reports indicated that young people might suffer more from side effects than the elderly [45], concurring with our results of increased fear among younger people. Different fear scores were also found between employees and business owners. Employees were less fearful than business owners because most had welfare payments provided by their companies. The possibility of injection injury also resulted in fear and contributed to vaccine hesitancy [46].
The average VH in our study was 2.51 out of 5, with no significant differences in hesitancy scores among demographic variables. Vaccine hesitancy resulted from fear. A recent study determined three common reasons for vaccine hesitancy among Thai citizens, as stated by participants: “The vaccine can have dangerous side effects,” “I may be allergic to the vaccine,” and “The vaccine may not work” [47]. In our study, the three highest average scores of hesitancy were observed for “not sure about the efficacy of the Coronavac (Sinovac) vaccine,” “vaccination is the best way of preventing COVID-19,” and “do not trust the information provided by the government.” Therefore, to reduce the hesitancy of Thais, transparency in educating people about vaccine efficacy is needed. Concentrating efforts on implementing the abovementioned procedures will greatly assist in reducing COVID-19 vaccine hesitancy among VHVs in Thailand. This will considerably help to control the spread of the COVID-19 pandemic. Increased participation of local authorities, such as healthcare authorities, media, and regular authorities, including relevant research authorities, will aid COVID-19 control efforts of VHVs in Thailand.
Unsurprisingly, acceptance scores of the COVID-19 vaccine were low among VHVs. Studies in several countries revealed negative acceptance of COVID-19 vaccines [48] at greater than 30% of the overall population [49-51]. Vaccine acceptance varied depending on geographical location, with low acceptance in Kuwait (23.6%) and Jordan (28.4%) and moderate acceptance in Italy (53.7%), Poland (56.3%), and Russia (54.9%). In addition, the proportion of the participants accepting the use of a safe and effective COVID-19 vaccine was the highest in China at 88.6% [49]. One of the main reasons for these attitudes was doubts that the vaccines were safe [48-52]. Significantly different scores were recorded among age groups, marital status, and occupation. Older age groups had higher acceptance scores. This result concurred with a study in Thailand that demonstrated higher mean scores of acceptance in older adults (≥65 years) [47]. Higher COVID-19 vaccine acceptance among older adults was also found in several studies [53-56]. In Thailand, the two major vaccines are SV and AZ. The efficacy of SV has been questioned compared to mRNA vaccines [57], while younger people reported more side effects after taking a shot of AZ [46]. These reports contributed to higher acceptance scores among the elderly (>60 years). Cocktail vaccines were introduced nationwide in Thailand in July, 2021 [58]. However, the WHO warned that mixing vaccines from different manufacturers lacked conclusive evidence of strong immunity [59].
The association between COVID-19 vaccine literacy, fear, hesitancy, and acceptance was also investigated. Significantly negative associations were found between hesitancy and literacy, acceptance and fear, and age and fear. This implied that increasing VL reduced VH. Turhan et al. reported that people with low health literacy or difficulty accessing accurate information regarding COVID-19 vaccines had higher levels of vaccine hesitancy. Conversely, participants with less vaccine reluctance showed reduced vaccine hesitancy if they were able to access information concerning the decision-making on the merits of vaccination [60]. Minimizing fear increased vaccine acceptance. Many studies documented that intensifying COVID-19 immunization mobilization and delivering positive messages about vaccine efficacy reduced fear and boosted vaccine acceptability [54, 61]. There was a significant positive association between age and acceptance, similar to comparing the median difference of acceptance scores by age, as mentioned earlier. Therefore, the Thai government should pay attention to the young age group to boost vaccination uptake.
This study had limitations as follows. First, the sample population was not large enough to display significant results, but this was not the primary purpose. Results demonstrated the feasibility of an online survey using popular social platforms, such as Line and Facebook. Future studies should conduct surveys using a larger population via an online questionnaire. Second, this research was conducted during the fourth wave of COVID-19, and the vaccination campaign had already been launched in Thailand. Thus, the scores may not reflect vaccine literacy, fear, hesitancy, and acceptance at the start of the pandemic. Third, this research was performed on VHVs. This group of people operates as intermediate communicators between healthcare professionals and people in the community. Findings were, therefore, generalized to a particular segment of society.
CONCLUSION
The online structured questionnaire showed high validity, reliability, and feasibility among VHVs in Thailand. Based on the study, high average scores of literacy, fear, and hesitancy but low acceptance scores were found, with different scores of literacy, fear, and acceptance of COVID-19 recorded for age, marital status, and occupation. Some correlations were identified between the four dimensions of COVID-19. Further studies with larger sample sizes are needed to clarify the results of this assessment tool among VHVs in Thailand.
AUTHORS’ CONTRIBUTORS
JW, PSi, and PSa contributed to conceptualization and methodology. SN and JL contributed to data curation and investigation. PSi and JW performed the statistical analyses and wrote the original draft. This study was supervised by PSa and JW. PSi, JW, SN, and JL participated in editing the manuscript. All authors have read and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| VL | = Vaccine Literacy of COVID-19 |
| VF | = Vaccine Fear of COVID-19 |
| VH | = Vaccine Hesitancy of COVID-19 |
| VA | = Vaccine Acceptance of COVID-19 |
| VHV | = Village Health volunteer |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was reviewed and approved by the Institutional Ethical Review Board of the Faculty of Public Health, Chiang Mai University (IRB No.ET033/2021).
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all study participants.
STANDARDS of REPORTING
The study observed the STROBE guidelines.
AVAILABILITY OF DATA AND MATERIALS
Datasets used and /or analyzed are available from the corresponding author on reasonable request [J.W].
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the village health volunteer network in Thailand for distributing the online survey.
SUPPLEMENTARY MATERIAL
Supplementary material is available on the publisher's website along with the published article.


