All published articles of this journal are available on ScienceDirect.
Comparable Public Health Responses to COVID-19 Pandemic
Abstract
Coronavirus-2 (SARS-CoV-2) is a serious respiratory disorder and has challenged public health organizations everywhere. To effectively target government interventions, the most vulnerable persons to coronavirus disease-19 (COVID-19), the development of serious health indications and mortality must be identified. We conducted a thorough literature review to provide the existing position of technical information in these domains, stressing the necessity for a united worldwide approach, touching forward and learning for upcoming diseases. Medline, Embase and Global Health, and the Web of Science, were searched by the end of August 2021. The search criteria were SARS-CoV-2 and COVID-19-specific. A broad array of descriptions has been recycled regarding the harshness of the condition. Furthermore, multiple countries took various public health steps to control the transmission of COVID-19. In this review, we are enlisting the countries and their short- andlong-term public health responses to combat this pandemic. We also described four key sections of public health responses, i-e, monitoring, public education, crowd control and establishment of health care facilities followed by various countries to prevent the pandemic.
1. INTRODUCTION
At the end of December 2019, first case of coronavirus-infected pneumonia was detected in Wuhan, China [1]. Infected patients with an unclear cause exhibited dyspnea, temperature, chronic cough, and mutual lung infiltrate on radiology. The disease is known as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), and the condition is known as Coronavirus Disease 2019 (COVID-19) according to the World Health Organization (WHO). In late January 2020, the WHO classified the COVID-19 occurrence as a Public Health Emergency of International Significance, and warned that nations with ageing healthcare infrastructuremight be particularly vulnerable. Early detection, social isolation, prompt rehabilitation, and other preventative measures may impede disease propagation. This illness has posed significant threats to global health systems and country economies. Because there was no specific cure for the condition, therefore there is a demanding need to identify other methods to control its spread. SARSCoV-2 is currently producing a worldwide outbreak of coronavirus sickness (COVID-19) [1]. The virus's overall mortality risks are highly alienated, with these kinds of marginalized communities bearing a higher risk of depression-related health outcomes.
The global public health approach to the emergence of COVID-19 has been diverse and evolving. South Korea conducted intensive screening and considerable attempts to separate afflicted persons and track/isolation relations, but Sweden stayed closed to health treatments aimed primarily at vulnerable groups. The United Kingdom (UK) measured several possibilities earlier when choosing solitude, isolation, and social exclusion restrictions, which improved in mid-July 2020. Confinement is currently existing and re-implemented in phase 2. Unlike Canada's early attempts to “soften the slope,” American states a number of approaches, with various states currently relaxing their policies to varying degrees. China took a tough stance, quarantining and isolating afflicted people in the affected Hubei province. India was placed under a tight time and the 40-day lockdown was imposed, and it was later extended until May 31, 2021 [2].
Huge numbers of people remain exposed to public health programs in some form or the other from around the planet, begging the issue of how stringent regulatory reactions should be in superbugs and how long can or should such last restrictions be maintained. The COVID-19 outbreak has convinced the public health officials in many countries to pass legislation and use various techniques to stop the spread of infection, including pushing patients to self-isolation. This brief overview aims to outline these approaches and reactions in a few nations, then analyze how these approaches might aid in viral transmissions prevention and evaluate the efficacy of their programs divided by the total number of instances for each country listed. The findings may be useful for policymakers, regulators, and academia.
1.1. Why Public Health Responses are Important?
The capacity to identify the demographic groups with high vulnerability to the virus has numerous public health implications. Stratified vaccination plans for governmental delivery, such as those for influenza, can be created using such data [3]. It may also be able to prioritizeze more standard precautions of populations at higher risk of deteriorating patients and make healthcare services more accessible by identifying people who are most likely to be exposed to common infections and require critical care. Vulnerable populations can receive official advice informing them that they are more susceptible to the SARS-CoV-2 virus and encouraging them to change their lifestyle behaviors [4]. To approach such populations, more organized “segment and shield” procedures can be used, such as decreasing communication with extra collections and crowding while eliminating limitations for the general population, and it is conceivable to establish which collections need further defense [5]. On the other hand, potential human health projects have been critiqued for their lack of inclusion, particularly because of unintended detrimental consequences for already marginalized groups [6]. Early 30th March 2020, vulnerable people in the UK were urged to be very rigorous with communal separating actions, while those inside the same group who were at higher risk were referred to as “shielded” persons and given additional counseling [7]. Similarly, it was also found that the influenza vaccine clusters were embattled by the National Health Service, while the latter was built on medical judgment. These layers were designed to be as flexible as possible to protect as many customers as possible. As additional evidence emerges, such as whether the emergence of lesions in the brain is related to patients with or without before the cardiovascular disorders and the respiratory system contributes significantly to illness etiology [8].
During infectious disease outbreaks of novel infective syndromes, it's dangerous to promptly and precisely detect the groups. We performed a thorough analysis and excellent observation of the recent worldwide studies in the case of COVID-19, concentrating on three key outcomes: COVID-19 indicators, its effects, and illness or death. Any possible risk factors, populations, or research methods were all considered. As a consequence of our results, we emphasize significant information gaps in earlier work and the need for uniform worldwide methodologies in the future, particularly in the event of influenza.
2. METHODOLOGY
Between November 1st, 2019 and March 26th, 2020, we examined Medline, Embase, and Global Health, as well as Web of Science, for published materials. Only phrases unique to the virus and disease, along with the word “or,” were used to duck absent papers on danger issues: “covid-19”, “coronavirus”, “severe acute respiratory syndrome coronavirus 2”, “SARS-CoV-2”, “2019-nCoV-2”, “acute respiratory syndrome”. The search was conducted without any restrictions or filters. Across all databases, the same search phrases were utilized. Relevant studies, research papers, and the greyish literary works of global health findings, were found from 26 countries with the most disclosed COVID-19 people. For other countries, it was presumed that statistics would be lacking to generate relevant information. The search terms were subjected to specific criteria, such as individuals with positive SARS-CoV-2 viruses verified by amplification (PCR) were acceptable. There were significant differences in clinical diagnosis among research, although portal veins were the gold standardized method for current infection at the jump of the epidemic [9], and other methodologies such as Loop-Mediated Adiabatic Synthesis or antibody assays were not involved.
2.1. Quality Assessment
Two referees self-sufficiently judged the excellence of the research that was included. Two more researchers evaluated the quality of research published in English and other languages, with a third editorial team memberoffering additional quality assurance. The evaluations were conducted with the review's goals that were not frequently the same as the goals of the supporting investigations. The integrity included in instructions was measured using a questionnaire established by Downs and Black [10]. When analyzing the supremacy of experiments, the response rate [11] investigated to identify a corresponding elevated risk of 10% from a statistical significant cautious benchmark of 50% between unprotected was measured at various authorities consuming the Kelsey technique within Epi Info, features developed by the US Midpoint for Syndrome Control [12]. The 10% figure was obtained from government debates in the United Kingdom when the learning was steered. A 5% alpha was chosen as the benchmark. We went with a simple two-layer model with 1:1 lighting among them. Altered brinks were recycled for case-control, cohorts, and bridge studies. These qualities were rated on a scale of 0 (low power) to 5 (high power). If the data were corrected for age, sex, civilization, and any amount of comorbidities, we deemed them sufficiently confounded adjusted. The requirement for ethnic adjustment was overlooked in ethnically homogeneous populations. When two analyses with different quality scores were reported in a single manuscript, the more conservative score was kept [13]. The quality assessment did not prevent studies from being included. Synthesize and analyze the outcomes studied (illness, severity of disease, mortality) were grouped first, followed by the risk variables studied. The findings were categorized based on whether they provided evidence that, given the numberf people who were engaged, the vulnerability under consideration constituted a health risk [14]. We retrieved all data on possible dangers in research that focused on a particular health threat of concern with influencing adjustment (although acknowledging that certain independently corrected values for variables may remain muddled even though those for the characteristics of the project do not) [15]. Even though there was significant heterogeneity in qualitative research, methodology, and lifestyle factors evaluated, we provided a thorough descriptive evaluation and equilibrium was a condition for our results instead of a conceptual [16].
3. RESULTS
In certain locations, consultation or surveillance were also used throughout the outbreak period [17-20]. Public health plans and response methods are classified into four key sections [6, 20]: a) Monitoring: Countries with regard through telemonitoring techniques or extensive research at airports or on regional borders, the whole or part of the community. Some nations, notably Singapore, also used approaches such as the use of the Global System of Positioning/credit card data or the establishment of self-monitoring or psychology consulting websites [21]; b) Public education: Many governments have sought to provide clear information about the virus to enable community education. In addition, information was sent to individuals through various types of media or message services on preventive measures or appropriate procedures in the college; c) Crowd control: Governments used certain strategies to reduce collections. The measures included social separation, quarantining, road traffic management, closure of schools and universities, postponement of activities and shutdowns [22]; d) Preparation of health care facilities: Established and/or developed in some nations to ensure adequate care facilities, including large hospitals with the greatest level of care [23]. In both treatment and recovery phases, hospitals or shelters have been established or designated to care for suspected or confirmed patients. The death rate in those countries might then be reduced by such facilities (Fig. 1).
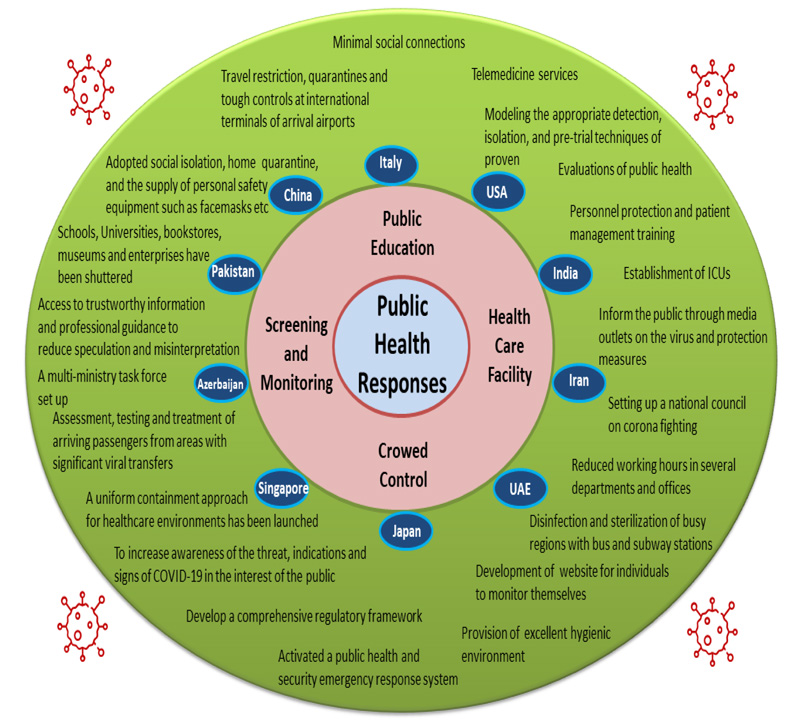
The countries have initiated public health responses at various levels to combat COVID-19. These public health responses were divided into four sections i-e, Public education, Screening and monitoring, Crowed control and health care facilities. Further, each country designed responses per their pandemic situation and fatality rate.
The proposed public health controls might lead to successful approaches in certain countries to cope with the current pandemic. However, some nations require harsher laws or practices. Some nations could manage the virus via the World meters website, and their overall rate of infections stayed consistent following a certain date. Some other nations have decreased their death rate with increasing total cases, even though their cases continue to rise to a larger extent [24].
4. DISCUSSION
Since 2002, the world has had three outbreaks, followed by the SARS CoV epidemic, the MERS CoV in 2012 and the COVID-19 pandemic in 2019. Global distresses were caused by the immediate spread and the high transmission rate among people.
Some methods for the screening and treatment of COVID-19 cases have been introduced. Singapore has helped to avoid the transmission of infection and to confine it into certain medical centers with early and quick response to the outbreak and implementing preventive methods. The propagation of the virus across the country has been stopped using suitable techniques, including the entry of COVID-19 patients [25]. By using these approaches, the general public would have access to accurate information on the place and time of the exposure and other information. Since connections between breach and privacy of the patient safeguard the health status [26]. Although China was the most affected initially, the outbreak attained stabilization following tight surveillance and widespread quarantine. Since early March 2020, according to the “Worldometer” figures, the rate has gradually increased. Italy employed a sophisticated monitoring operation to detect and reinforce numerous incidents at the personal level [27]. To prevent the virus from spreading to everyday life without any serious problems, China succeeded in the early identification of cases via surveillance and rigorous contact tracing between confirmed cases and implementation of border control procedures [28]. Singapore also has the experience of the 2003 SARS outbreak and was successful because of its preparation. In addition, ICUs were fully developed and responded to the viral epidemic quickly.
Although the number of verified cases in China is increasing, this country still has a very low fatality rate. This may be a result of the government's quick response to the emerging problem by means of control measures like social distance, public education and technical progress [29]. Similarly, Australia and Singapore suffered relatively low fatality rates because of early reactions and control programmes. Iran has developed a residential psychotherapy system and established an independent monitoring website for suspected COVID-19 cases. This country tried to battle the pandemic in many ways, but today it seems that more coherent, quicker and more effective actions are required to stop the spread of the virus, particularly among its most vulnerable people. Furthermore, appropriate and stable economic resources and their effective use are needed. The Japanese Government utilized social distance and travel restrictions to tackle the problem recently. This country has managed the viral epidemic with a comparably low death rate. The experience with the SARS outbreak may favorably impact the reaction of Canada to the COVID-19 pandemic, particularly in relation to facility preparedness, according to epidemic monitoring specialists from Canada. However, due to the increasing number of new patients, the increasing load in hospitals and care centers may remain a significant problem [30]. The increased illness propagation and the necessity to provide urgent care to more patients is a major threat to the healthcare system brought about by the current COVID-19 epidemic in Italy [31]. While Italy has a well-equipped health system and the Government has responded swiftly to the outbreak, this country has not been prepared to address the COVID-19 epidemic and the number of patients is still increasing. This scenario has justified a number of health care issues across the country. More suitable team efforts, proactive planning and training methods appear to give greater management support [31]. The exact frequency and accurate death rate were unknown at the moment. In this scenario, more obvious and complete statistics are necessary to contribute to decision-making and to raise public awareness. Everyone in these nations has to emphasize greater real-time screening of transmission and death, while certain countries, like Spain and France, have developed proper control methods involving large lockdowns in order to battle the pandemic. The government's late response to the epidemic in Spain was the primary cause of its inability to manage the illness. Moreover, the hospitals were in a harsh state due to the financial crisis in this country. The reasons for this might be different in France. French citizens were less determined than other nations to obey the national lockdown rules [32].
China dominated the viral transmission rate at the start of the pandemic with the quickest spread, and other nations took over China in the next few weeks. As noted before, the number of confirmed cases and deaths has increased significantly in Italy and Spain. As of the 19th of March 2020, Italy has overtaken China with over 3400 deaths due to the virus, while the United States, compared to other nations, have the greatest overall number of cases [33]. A great example of a quick reaction in the US would be a comparison between New York and California. In contrast to New York, California succeeded in curbing the spread of the virus. Experts in disease prevention think that the most important difference between these two regions does not concern the population or geography, but the time individuals started to stay at home and the differences in their response to social separation. Overall, New York has had 9 times as many cases, 7 times more hospital patients, and 14 times as many deaths as California [34]. While China was originally the first country infected with the greatest incidence of confirmed cases and fatality, it can now be recognized as a successful country due to reinforced policies and public health response. The community was also adequately educated about the need for COVID19 to meet national approaches to mask wear, hand washing, social separation and temperature monitoring of the population. China also seeks to restore regular social and economic activity by maintaining a tough containment policy [35]. In the early days of the outbreak, the administration did not recognize the pandemic and downplayed its significance [36].
Management and research techniques in many nations are still remarkably unknown. This would be advantageous for international cooperation in controlling the pandemic, and greater information about the new virus would be obtained through a deep screening process. Among the most widely recognized control and illness prevention strategies are identifying suspected cases, preventing viral transmission by means of isolation, personal protection, and managing infections [35]. Some models also anticipate the favourable influence of these strategies on monitoring infection transmission [36]. Furthermore, a validated emergency supply chain in health care is required for rapid assessment, response and monitoring during such pandemic based on enablers driving and dependence power, including the autonomous, dependent, linkage and independent groups [37]. In order to successfully manage infection transmission, it is essential, in all nations, for more effective clinical treatment of infected patients, readiness for public health responses, and quick and precise epidemic screening. Likewise, the policy framework for the legal, environmental and political issues should be the immediate concern of the governments and health officials on a global level [38].
CONCLUSION
According to the management decisions of various countries about quarantine, lockdown, social isolation and flight suspension, the successful tactics for confronting the current epidemic are largely guaranteed by its intensity and anonymity. Besides these efforts, several nations have concentrated on adopting rigorous case detection and screening methods. In summary, governments should adopt laws and implement stringent and prompt steps to stop the spread of the disease and reduce its unintentional mortal impacts.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus Disease 2019 |
| WHO | = World Health Organization |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
Dr. Falak Zeb is the Executive Guest Editor of the journal.
ACKNOWLEDGEMENTS
Declared none.


