All published articles of this journal are available on ScienceDirect.
Factors Influencing Optimal Glucose Control among Type II Diabetes Patients: From the Health Behaviour Models’ Perspective
Abstract
Background:
Diabetes is a global health issue and one of the top ten causes of mortality, requiring focused research for understanding and implementing appropriate methods of diabetes management. Among the many approaches to managing optimal glucose control, embarking on the factors that influence engaging in health behaviours, such as managing glucose control, plays a pertinent role in addressing effective glucose control management.
Objective:
The present study has attempted to understand the influence of various factors (at the individual level and social level) on optimal glycemic control, which is considered one of the efficient parameters of diabetes management, utilizing the predominant health behaviour models- health belief model, theory of planned behaviour and socio-ecological model.
Methods:
This correlation study was conducted among 266 individuals from the Indian state of Karnataka. The purposive sampling technique was adopted to select participants over 18 years and those suffering from Type II diabetes.
Results:
The Pearson correlation analysis showed a significant positive relationship between perceived severity and HbA1c value and a inverse correlation with interpersonal relations and community domains. The multiple linear regression analysis results showed the statistically significant predictors of perceived severity, perceived benefits and interpersonal domains on glucose control.
Conclusion:
The study results put forward the influence of individual-level factors such as perceived severity, perceived benefits, and interpersonal factors in achieving optimal glucose control among type II diabetes patients. The study also highlights the importance of creating more awareness, especially in the Indian context with very low health literacy, which could help enhance the perceived benefits of diabetes specific health behaviours.
1. INTRODUCTION
Diabetes is a serious, chronic medical condition that impacts different aspects of an individual’s life. Globally, it is counted as a significant health issue that has the potential of reaching epidemic proportions [1]. At a global level, four million deaths were reported in 2017, ranking it among the top ten causes of death among the adult population. The incremental rise in the number of diabetes cases is estimated to cross 578 million by 2030 and reach 700 million by 2045, if the trend continues [2].
The number of diabetes cases in India rose from 26 million in 1990 to 65 million in 2016 [3]. As per the National Diabetes and Diabetic Retinopathy Survey report, 2019, the prevalence of diabetes among elderly over the age of 50 was reported to be 11.8% [4]. Demographic and Health Survey 2015-16 found a prevalence of 6.5% among adults under the age of 50 years [5].
Diabetes management is primarily concerned with maintaining normal blood glucose levels and, as a result, reducing the related long-term consequences. The nature of management includes self-management as well as pharmacological therapy [6]. The major goals and implementation of self-management are planned to incorporate the active participation of the patient and guidelines from the health care team [7].
The prime objective of diabetes management includes prevention of heart-related risk factors as diabetes is most frequently associated with major cardiovascular risk factors, such as hypertension and hypertriglyceridemia, which is the leading cause of death in individuals with these comorbid conditions [8]. Hence, the management plan incorporates measures to control glycemic levels and other treatments for the associated risk factors [9]. The application of stringent evidence-based management is required for appropriate diabetes treatment, which is a time-consuming and challenging task. The typical medical practice has limitations concerning finite appointment schedules, resources and increased demands. Thus, the diabetes management paradigm incorporates certain self–management practices to improve the quality of diabetes care [10].
Among the identified factors influencing better management of glycemic control, good adherence is associated with positive health outcomes and lower mortality among diabetic patients [11-14]. Adherence to medication and lifestyle modification is an important determinant of health outcomes among chronically ill patients. In those patients with diabetes, adherence to these factors is related to additional benefits, such as improved control over other associated risk factors and lower mortality rates [15].
Adherence to a lifestyle involving regular engagement in physical activities and dietary habits is a critical determinant of achieving glycemic control. These exercise and dietary guidelines, if followed properly, reduce or avoid the incidence of other comorbid medical conditions. The controlled consumption of carbohydrates is a major dietary regulation to be taken care of to maintain an optimal glucose level [16]. Further, interest in calorie restriction by stabilizing anti-ageing genes has been accelerating in recent years to delay and prevent programmed cell death associated with various chronic diseases. The nature-nurture interaction in the times of urbanization regarding access to food and its content leads to the induction of epigenetic alterations associated with glucose dyshomeostasis and increased risk for insulin resistance [17].
Advances in nutritional research have identified nutrient-sensing diets and have become an integral part of diabetes management and diabetes self-management education.
Advances in nutritional research have identified nutrient-sensing diets that regulate histone deacetylases which are involved in epigenetic control of gene expression that controls metabolic and tissue glucose and homeostasis. The anti-aging protein, Sirt 1, is closely associated with protection against DNA damage and therefore has genomic stability associated with diabetes. In calorie restriction, regulation of the sirtuin 1 gene, which is involved in longevity and ageing, has become an essential treatment for maintaining glucose and cholesterol levels, along with the reversal of chronic diseases such as obesity, diabetes and neurodegenerative diseases [17, 18].
Maintaining food quality, core body temperature and appetite control remains the three crucial factors in insulin therapy associated with diabetes management [18]. Dietary activators and genomic medicine are needed to maintain insulin therapy and prevent toxic immune reactions during diabetes management [19]. Therefore, dietary components that activate anti-aging genes improve insulin therapy. Care needs to be taken to include specific amounts and doses of Indian spices in the diet that do not interfere with insulin therapy and induce mitophagy in various diseases [19].
Self–monitoring of blood glucose levels is a recommended practice by physicians to help people achieve an optimal glucose level. It prevents, reduces the risk and delays the onset of diabetes-related complications that often occur due to unregulated and high blood glucose levels [47]. The goal is to record blood glucose levels at different points for maintaining a constant glucose level by more precise regimens. This measure of diabetes management facilitates the preparation of an individualized glycemic profile, thus helping formulate a customized treatment plan. It also helps patients and their family members plan appropriate choices in their daily treatment, such as in relation to diet, exercise, insulin intake or other potential agents. Regular physical activity is a protective factor in maintaining optimal glucose levels and other benefits of improving insulin action, weight loss and reduction of major cardiovascular risk factors [20].
Further, the individual develops awareness about their glycemic level, thereby impacting their decisions about lifestyle modification and adherence to management plans [21]. The efficiency of this management measure has been reported by much empirical evidence, such as through randomized control trials. Researchers had found a greater association between self-monitoring of glucose levels with better health outcomes among type 1 diabetes patients [22]. In the case of type 2 diabetes patients, an association was observed concerning better glucose level control [23].
Self-management of diabetes is influenced by multiple factors such as individual level, health care team and other social factors [24]. Identification of any inconsistencies concerning these aspects is vital in attaining better results because effective management depends on the congruence between them [25]. The lack of health-related information from the consulting physicians and lack of awareness about the target blood glucose level act as the major barriers to adhering to self-management [26]. The patient's knowledge level is thus identified as a major factor in adhering to diabetes management [27]. Adequate knowledge of diabetes management is related to improved adherence to medication, diet, glucose monitoring, and exercise [28].
Several individual and environmental factors influencing non-adherence to optimal glucose control act as barriers to self-management of diabetes [29]. The major individual-level factors identified include self-efficacy, motivation, health literacy and beliefs, locus of control, coping and problem solving skills, depression, forgetting, anxiety, excessive use of alcohol and presence of other comorbid health issues interfering with diabetes management. The factors identified in relation to the environment include social support, socio-economic factors, distance to the site of health care, availability of good quality health care, food and exercise opportunities [29]. Health belief model (HBM) is among the most popularized models in health promotion models, developed to explain an individual’s engagement in various health-promoting behaviours [30]. The initial stage focused on predicting an individual’s behavioral reactions to disease and the treatment modalities received [31]. From the perspective of HBM, the constructs facilitating an individual in engaging in health promoting behaviours are perceived benefits, susceptibility, seriousness, barriers, cues to action and self-efficacy. Accordingly, if an individual perceives high susceptibility and seriousness, then there are high chances that they would take necessary actions to prevent the disease. In addition, these preventive actions persist as long as the perceived health outcomes transcend the perceived barriers. Also, the extent to which self-efficacy factors make them believe in their capabilities to engage in health promoting behaviours plays an important role [31]. Aalto &Uutela (1997) found that in individuals with Type 1 diabetes, prediction of adherence to diet and glucose monitoring was related to the perceived benefits in relation to costs [32].
Though this model carries with it the advantage of explaining behaviour in terms of individual psychological constructs, the overemphasis on macro-structures of an individual’s thoughts is often considered a major limitation [33] Hence, other theories developed incorporating other factors facilitating engagement in health promoting behaviours. One such theory is the Theory of Planned Behaviour (TPB) [34]. The core factor facilitating an individual’s engagement in behaviour is behavioural intention, i.e., the more a person intends to carry out behaviour, the greater the chances that they actually perform the behavior [34]. The intentions are influenced by factors such as attitude towards the behaviour, subjective norms and perceived behavioural control. In line with the HBM, this theory also postulates that the main reason for engaging in any health-promoting behaviour is associated with certain beliefs [29].
Analysing each component of this theory, attitude encompasses an individual's evaluation of their own behaviours and its subsequent consequences. Regarding societal perceptions of the intended behaviour, subjective norms refer to how individuals experience the pressure to conform. Perceived control factors focus on the individual’s perception of their ability to engage in a particular behaviour [29]. Gatt & Sammut (2008) conducted research among Type 2 diabetes patients and found that attitudes, subjective norms and perceived behavioural control explained 49% of the variance in the intent to engage in self-care behaviour [35].
In contrast to the above models, socio-ecological theory (SET) of health promotion offers a more comprehensive account of factors influencing an individual's engagement in various behaviours [36]. The theory emphasizes the interactive nature of individuals and their environment as an important predictor of health outcomes [37].
Grounded in Urie Bronfenbrenner’s (1977) ecological framework, McLeroy et al. (1988) developed a multilevel ecological model specific to health behaviour. According to this model, there are five levels of influence on various health behaviour: individual, interpersonal, organizational, community and public policy [38-40]. Individual level focus on the ability of individuals to bring adaptive behavioral changes for achieving optimized health related to diabetes self-management and is influenced by factors such as attitudes, knowledge, skills, beliefs and self-confidence [41]. The interpersonal level incorporates those factors in association with individual's relationships with other people – family, friends, and so on. Previous research evidence has shown that relationships with friends, parents, colleagues and neighbours play an important role in individuals' health behaviours [39]. Further, empirical evidence also found that social support is associated with better metabolic control in an individual as well as enhanced diabetes self-management [42, 43].
Individuals are also associated with different organizations such as schools, workplaces, churches etc.; these organizational structures and processes were also found to significantly influence health and health behaviours. It has been found that these organizations facilitate behaviour change by providing a context for health promotion activities along with social support and acceptability [43]. Several factors, including the living circumstances in a particular geographic area, are considered while analysing the community-level influences on health behaviour. Literature evidence shows that the particular characteristics of communities, such as opportunities for education, community level awareness programmes, and recreation are linked with the health behaviours of individuals [44]. Through numerous regulatory channels, public policy impacts health behaviours at the local, state, and national levels. Because of the obstacles in reaching out to the broader population, this degree of impact often necessitates well-planned and persistent implementation [45-47].
Optimal glycemic control becomes the important outcome of treatment for diabetes. The complications can often lead to the death of the individual due to the primary cause of diabetes [48]. To reach that goal of optimal control along with the pharmacological therapy, the patient must follow a healthy self-care routine that involves diabetes specific diet, exercise regime, taking medication regularly, monitoring their glucose levels, and periodic consultation with the doctor. However, research has shown that implementing a healthy lifestyle that leads to optimal glycemic control is not easy and is influenced by many psycho-socio-cognitive factors [49]. The present study attempts to identify those factors from three major theoretical perspectives in Health Psychology- the Health Belief model (HBM), Theory of Planned Behaviour (TPB) and Socio-ecological theory (SET).
2. MATERIALS AND METHODS
2.1. Participants and Procedure
The study sample for the present study consisted of 266 participants above 18 years and were suffering from Type II diabetes. The study employed a correlational research design with a purposive sampling technique. The sample included a diverse group of participants- both educated and uneducated patients were included, from both rural and urban areas, engaged in various occupations. This makes the sample quite representative of the diabetic population in the Indian state of Karnataka. The socio-demographic details of the sample are furnished in Table 1. Data was collected from selected hospitals and clinics and directly through home visits. The participants were briefed about the study, and their voluntary consent was taken prior to data collection. Their socio-demographic details were collected, and the following questionnaires were administered sequentially. Simple and clear instructions were given to fill out the questionnaires. Descriptive and inferential statistics were used to analyze the gathered data.
2.2. Measures used for the Study
In the present study to measure the construct of HBM, items have been adapted from the scales developed by Robinson (2012), the perceived social support scale (Zimet et al.,1988) and the health value domain from the health belief model questionnaire (Norman & Fitter, 1989) [50-52]. To measure the constructs of TPB, the instrument used was a theory of planned behaviour questionnaire by Jennifer Amy Janzen Claude (2011) [53]. The dimensions of SET are measured using the socio-ecological model questionnaire by Glasgow (2000). The tool has good concurrent and criterion validity, and internal consistency was found to be 0.76 [54].
One of the best parameters for measuring glucose control is glycosylated hemoglobin (HbA1c), which provides an overview of individuals’ glucose control over the past four months. To obtain the HbA1c values, after collecting the data for other study variables, researchers reviewed and examined each participant's reports and recorded their respective HbA1c values. The participants' HbA1c values ranged from 5 to 12, with higher HbA1c values indicating lower glucose control.
2.3. Statistical Analysis
IBM SPSS Statistics 20 version was used to analyze the data. Descriptive statistics, Pearson correlation and multiple linear regression analysis were performed to describe the sample characteristics and to find the significant relationship and significant prediction of the variables, respectively. Multicollinearity was tested using the VIF values, and the constructs self-efficacy, cues to action, perceived barriers and community organizations were removed, and the constructs whose VIF values were found to be less than 10 were retained for regression analysis, satisfying the assumption that there is no multicollinearity between the predictors.
3. RESULTS
Table 1 shows the sample characteristics of the study participants. Most participants are in the group aged 46 - 60 years (48.12%) followed by 61 years and above (31.57%) category. 73.68% of the participants were male and 26.31% of them were female. Most of the participants (38.34%) received less than primary education and 66.54% were daily wage laborer. 74.43% of the participants were from urban backgrounds, while 25.56% were from rural backgrounds.
Table 2 shows a correlation analysis between the domains of the health belief model, theory of planned behaviour, socio ecological theory, and glucose control among the participants. The table shows a significant positive correlation between perceived severity and glucose control (HbA1c value) (p<0.01), which indicates that the higher the scores of perceived severity, the higher the HbA1c value and vice versa. Further, analysis shows a significant inverse correlation between interpersonal relations and glucose control (HbA1c value) (p<0.01), which indicates the higher the interpersonal relation scores, the lower the glucose control scores. And also, the higher the interpersonal relationship, the better the HbA1c value. Similarly, analysis shows a significant inverse correlation between community and glucose control (p<0.05).
| Variables | n% (266) |
|---|---|
| Age | |
| 18- 30 years | 5(1.87%) |
| 31-45 years | 48(18.04%) |
| 46-60 years | 128(48.12%) |
| 61 years < | 84(31.57%) |
| Gender | |
| Female | 70(26.31%) |
| Male | 196(73.68%) |
| Education | |
| Uneducated | 9(3.38%) |
| Less than Primary education | 102(38.34% |
| Up to primary school | 9(3.38%) |
| Upper primary | 33(12.4%) |
| High school | 50(18.79%) |
| Intermediate | 13(4.88%) |
| UG | 44(16.54%) |
| PG | 6(2.25%) |
| Occupation | |
| Farmer/ Daily wage labourer | 177(66.54%) |
| Private/ Government employee | 53(19.92%) |
| House wife | 2(0.75%) |
| Self Employed | 34(12.7%) |
| Residence | |
| Urban | 198(74.43%) |
| Rural | 68(25.56%) |
| Marital Status | |
| Married | 262(98.49%) |
| Unmarried | 4(1.5%) |
| Variables | Glucose Control |
|---|---|
| Perceived social support | -.029 |
| Health Value | .053 |
| Perceived Susceptibility | -.028 |
| Perceived Severity | .222** |
| Perceived Benefits | -.103 |
| Perceived Barriers | .048 |
| Cues to Action | -.008 |
| Self- Efficacy | .043 |
| Attitudes | -.050 |
| Subjective Norms | -.003 |
| Perceived Behavioural Control | -.117 |
| Doctor and Health Care Team | .051 |
| Family and Friends | .016 |
| Personal | -.067 |
| Interpersonal | -.199** |
| Community | -.122* |
| Media and Policy | -.001 |
| Community Organisations | -.107 |
Table 3 shows the stepwise linear regression of the domains of the health belief model, theory of planned behaviour and socio-ecological theory on glucose control. The statistically significant final model explained 9.1% (R2=.091), F (5,260) =8.708, p≤0.001. The significant predictors were identified as ‘perceived severity’(p<0.01), ‘perceived benefits’ (p<0.05) and ‘interpersonal relations’(p<0.05) levels among the domains of health belief model, theory of planned behaviour and socio-ecological theory.
| Variables |
Model 1 Std β |
t |
Model 2 Std β |
t |
Model 3 Std β |
t |
|---|---|---|---|---|---|---|
| Perceived Severity | .222 | 3.706*** | .190 | 3.148* | .195 | 3.236** |
| Interpersonal | -.162 | -2.669* | -.172 | -2.850* | ||
| Perceived Benefits | .128 | 2.156* | ||||
| R | .222 | .273 | .301 | |||
| R2 | .049 | .075 | .091 | |||
| F | 13.737*** | 10.591*** | 8.708*** | |||
| ΔR2 | .046 | .067 | .080 | |||
| ΔF | 13.737 | 7.126 | 4.648 | |||
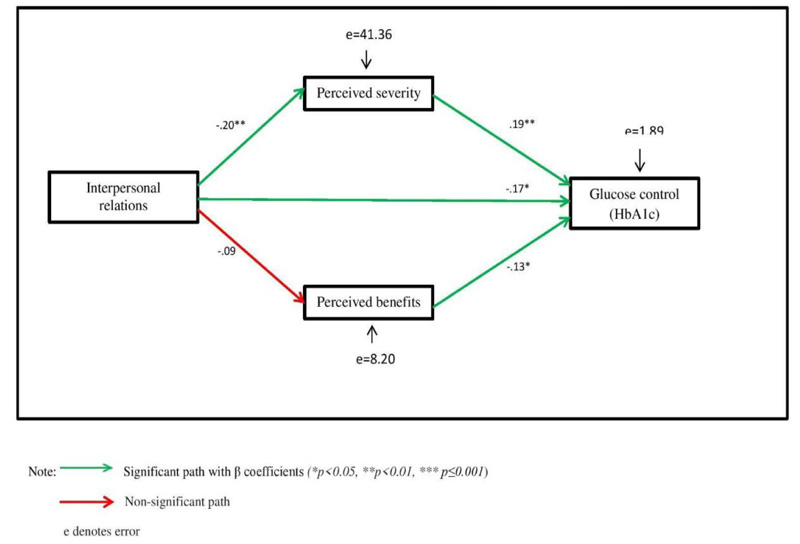
Path analysis was used to determine the pathways by which the constructs interpersonal relations, perceived severity, and perceived benefits interact to influence glucose control (HbA1c). Confirmatory factor analysis was computed, and the model fit measures were used to assess the model’s overall goodness of fit. The model yielded good fit for the data: CMIN/df= .261, GFI=1.00, CFI=1.00, TLI=1.138, RMSEA=.000 (Fig. 1).
4. DISCUSSION
The present study aimed to determine the various factors influencing optimal glycemic control among Type II diabetes patients from a perspective of the health belief model, the theory of planned behaviour, and the socio-ecological theory.
The study's results, which involved correlational and multiple regression analysis, showed that among all the theories' domains, only three significantly correlated with and predicted glycemic control- namely, perceived severity and perceived benefits of HBM, the interpersonal domain of SET. Perceived severity is an important subjective factor in determining the execution of health-promoting behaviours. Being conscious of the seriousness of the medical state motivates a person to engage in healthful activities on a regular basis [55]. Studies have shown that individuals with high perceived severity of diabetes and less perceived barrier to self-care were more likely to engage in diabetes management practices [56]. The results of the current study are in contrast to previous studies. Analysis of the results of the present study shows that the higher the perceived severity of a person, the higher the HbA1c level, indicating inadequate glucose control. Despite the fact that diabetes is a serious health problem and causes other health complications, patients have shown inadequate glucose control through analysis.
Patients with diabetes are expected to follow a complex set of behavioural actions to care of their diabetes on a daily basis. These actions involve engaging in positive lifestyle behaviours, including following a structured meal plan as well as engaging in appropriate physical activity; taking medications when indicated; monitoring blood glucose levels; responding to and self-treating diabetes-related symptoms; following foot-care guidelines; and seeking individually appropriate medical care for diabetes or other health-related problems (Goodall et al., 1991) [57]. In this context, patients are expected to form new health behaviour habit-formation. This habit formation is achieved easily for simple actions but not for elaborated routines (Gardner et al., 2012) [58].
On the other hand, factual information on diabetes does highlight the importance and benefits of maintaining glycemic control among diabetics. The higher the perceived benefits of optimal glycemic control, the greater will be the motivation of the patient to engage in diabetes self-care behaviour [59, 60]. Also, a patient with intrinsic motivation tends to identify the factors that he/she may alter in order to maintain better glycemic control [61]. They rely on themselves to act and bring about changes in their day-to-day life that leads to better management of diabetes.
Any individual and their goal directed behaviour are heavily influenced by his/her environment. The interpersonal factors influence the extent to which a diabetes patient strives toward achieving optimal glucose control [62]. Family, spouse, friends, and relatives form a network of support for the patient, educating them with the required information and encouraging them to engage in better self-care behaviors [63]. They provide tangible support in terms of helping patients plan and execute healthy behaviours that have a positive impact on glycemic levels. The results of the current study are in accordance with the findings of a South Indian study in which it was found that diabetes self-management behaviours can be substantially improved by improving family support [64]. It was also found that enhancing positive family relationships and increasing the involvement of families in the care and support of diabetes are likely to result in better self-management practices which in turn may improve glycemic control.
In addition, information about diabetes received from newspapers, television and magazines motivates the patient to execute self-care behaviours that directly impact glycemic control [65].
4.1. Limitations of the Study
In the present study, while collecting data, researchers failed to classify the patients according to their duration of the diagnosis. The current study has been conducted solely from the psychosocial perspective, collaborative research in the area, along with the biomedical aspect, would provide a more holistic understanding regarding glycemic control, considering the advanced research in the area of genetics, anti-aging and nutrition. The psychosocial support system of the patients is also less explored in the present study, which could also have provided an in-depth meaning about the quality of life of these patients.
CONCLUSION AND IMPLICATIONS
The present study successfully finds significant multi-level factors that might influence optimal glucose control among type II diabetes patients. The application of major health behaviour theoretical models has helped in concluding that all levels of influences need to be addressed while tailoring diabetes management interventions for patients. At an individual level, patients need to perceive the severity of their condition and should be intrinsically motivated to adhere to beneficial lifestyle modifications. The study results also highlight the importance of creating more awareness in the Indian context, where there is very low health literacy. Spreading awareness regarding the factual information about diabetes and ways to manage it is an essential step. This will enhance the perceived benefits of diabetes specific health behaviours. Awareness needs to be created through various virtual media platforms, like television advertisements, radio channels still used in rural India, and pamphlets in clinics. The information can be disseminated in three languages- regional, national and English- and in pictures to reach literate and non-literate patients. In addition, doctors and diabetologists should be made aware of the importance of the doctor-patient relationship. Clear and explicit communication between doctor and patient about the patient's condition, risk factors, and glycemic levels and its remedy helps the patient perceive the severity of their condition correctly. This will also enhance their health motivation. Along with these, the patient's family members need to be sensitized too, about their role in supporting the patient and keeping them motivated in executing diabetes specific behaviors.
LIST OF ABBREVIATIONS
| HBM | = Health Belief Model |
| TPB | = Theory of Planned Behaviour |
| SET | = Socio-Ecological theory |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Department of Psychology, School of Social and Behavioural Sciences, Central University of Karnataka, India (Ethical Clearance number: CUK/Psy/DERB-2018-09/10 Dated:08/11/2018).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All human procedures followed were in accordance with the guidelines of the Helsinki Declaration of 1975.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants of this study.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated during and/or analysed during the current study are available from the corresponding author [E.R] upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


