All published articles of this journal are available on ScienceDirect.
Spatial Association Between Sociodemographic, Environmental Factors and Prevalence of Stroke Among Diabetes and Hypertension Patients in Thailand
Abstract
Background:
Stroke is one of the top leading causes of death and disability among adults and the elderly worldwide. Hypertension (HT) and Diabetes Mellitus (DM) are the most common contributory risk factors of stroke, accounting for up to 75% of all cases. This study aimed to investigate the spatial association between sociodemographic and environmental factors and the prevalence of stroke among DM and HT patients in Thailand.
Methods:
This spatial study applied global Moran’s I, the local indicators of spatial association (LISA) and spatial regression to examine the localised associations of sociodemographic and environmental factors and the prevalence of stroke among DM and HT patients in Thailand.
Results:
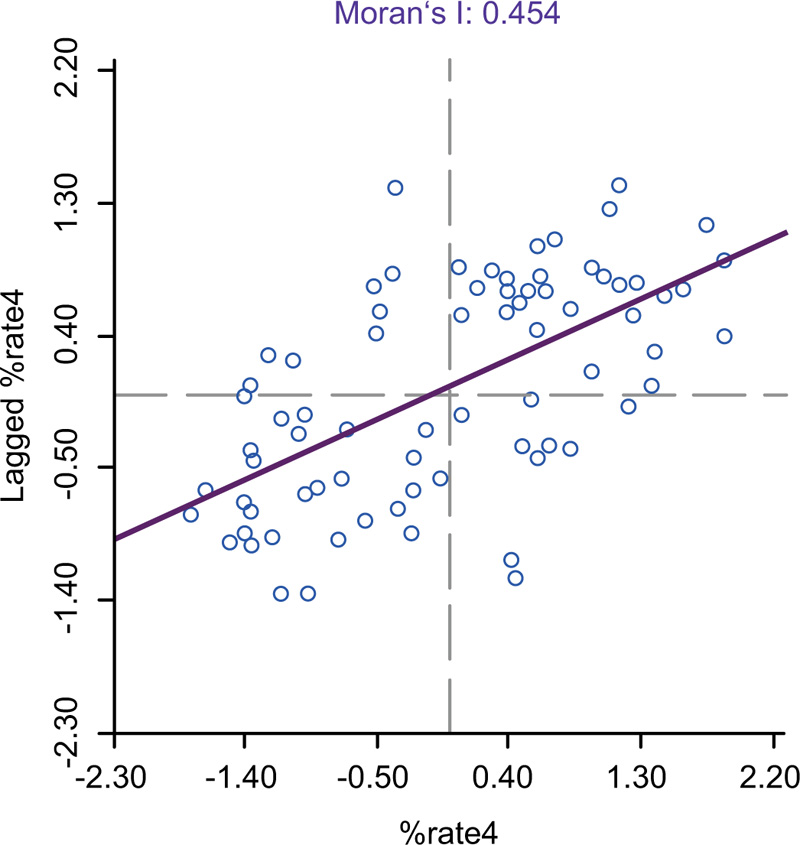
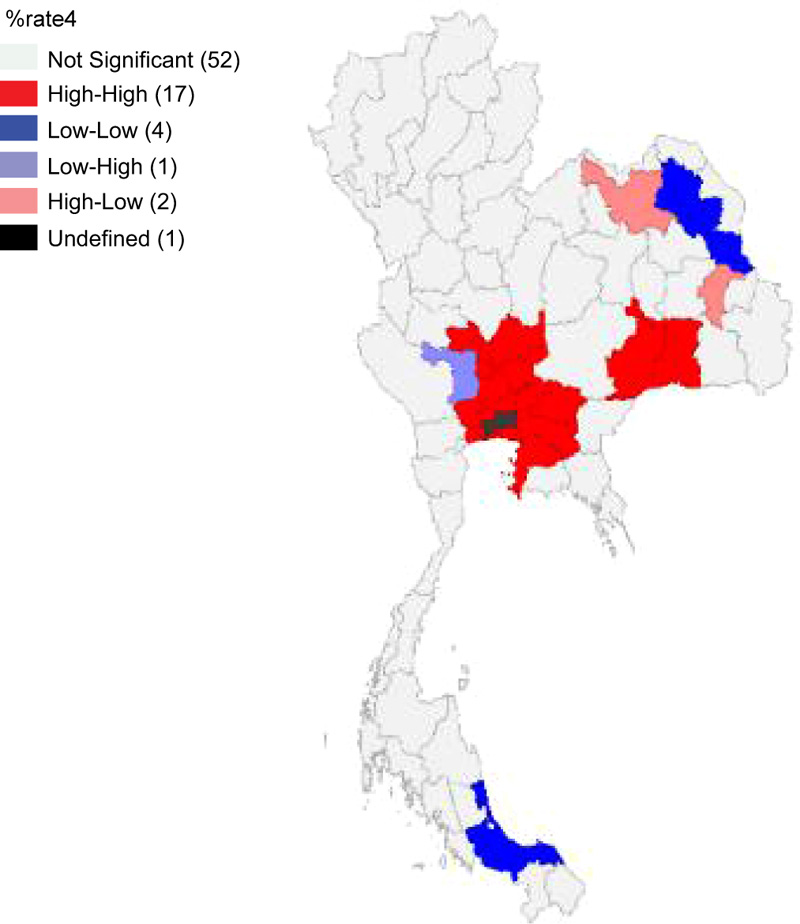
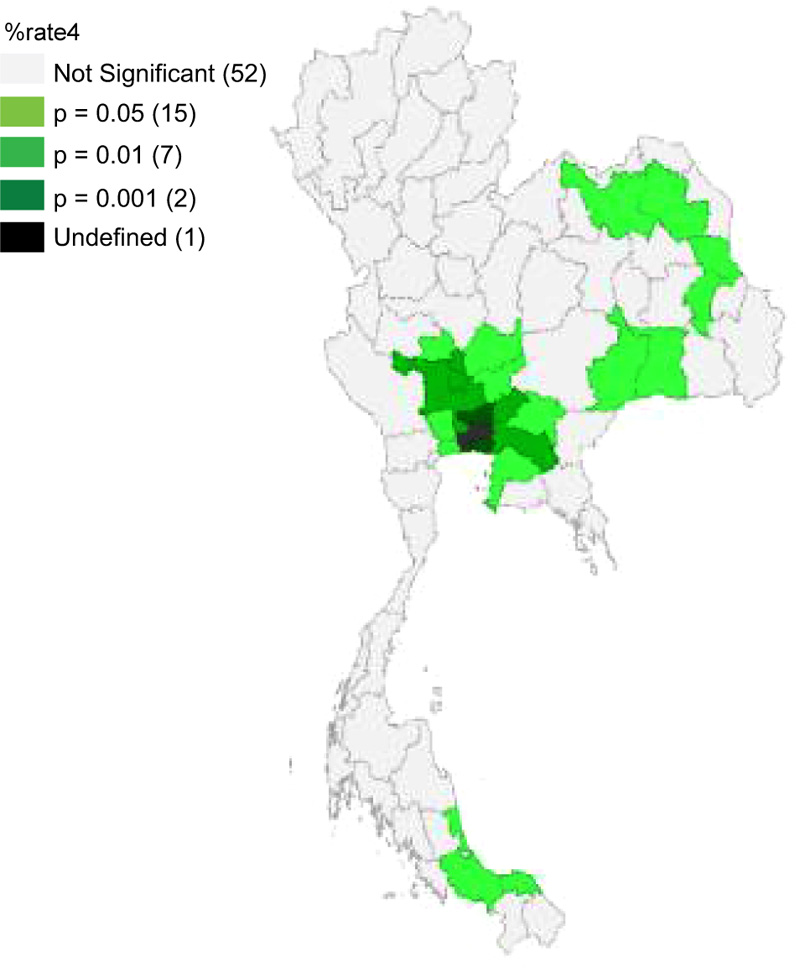
The univariate Moran’s I scatter plot of the annual prevalence of stroke in Thailand’s provinces observed significant positive spatial autocorrelation with the Moran’s I value of 0.454 (p < 0.05). The High-High clusters of strokes were mostly located in the center. The Bivariate Moran’s I indicated a spatial association between various factors and the prevalence of stroke in which the LISA analysis indicated; 16 Hot-spots or High-High clusters (HH) and 4 Cold-spot or low-low clusters (LL) with alcohol store density, 17 HH and 4 LL clusters with tobacco store density, 9 HH and 9 LL clusters with elderly population density, 5 HH and 3 LL clusters of primary care per population ratio, 16 HH and 3 LL clusters with LST, and 10 HH and 5 LL clusters with NTL. The Spatial Error Model (SEM) of spatial regression analysis has been observed to be the best model that could predict the variation in the prevalence of stroke by 50.80% (R2=0.508). SEM indicated tobacco store density (coefficient=0.065, P<0.05), elderly population density (coefficient=0.013, P<0.001, LST (day) (coefficient=1.417, P<0.05), and NTL (coefficient=0.021, P<0.05) were statistically significant associated with the prevalence of stroke among DM and HT patients in Thailand.
Conclusion:
Our study observed that the distribution of alcohol stores, density of tobacco stores, concentration of older adults, increasing day temperature and density of NTL were likely to be associated with enhancing the prevalence of stroke in the cluster and neighboring provinces of Thailand. The findings of this study will benefit public sectors or related organizations to develop efficient measures to control stroke.
1. INTRODUCTION
Stroke is the commonest cause of death and adult disability worldwide [1]. According to the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2017 data, stroke ranks third among all causes of death and disability (as measured by disability-adjusted life-years (DALYs) [2]. In addition, it was the second most common cause of death worldwide in 2017 [2]. Between 1990 and 2017, the prevalence of stroke increased by 11% in upper-middle-income countries (from 1.40 to 1.55%), while it decreased by 3% (from 1.03 to 1.00%) and 8% (from 1.26 to 1.16%) in low- and high-income countries, respectively [1-3]. However, the prevalence of stroke remained unchanged in lower-middle-income countries (1.08%) [2]. In 2018, it was estimated that 13.7 million people would die due to stroke, two-thirds of which occur in high-middle-income countries [3]. Thailand is one of the upper-middle-income countries located in the Southeast Asia Region, where the stroke is the first cause of death among females and the second cause of death among males of all ages [4].
Stroke is a serious health issue, the interference of focal or global neurological related to the distraction of cerebral blood circulation. This process lasts more than twenty-four hours resulting in death without knowing the cause of death other than a vascular origin. The brain cells begin to die quickly if no oxygen is supplied from the blood to eliminate the waste [5]. Stroke survivors may have difficulties that necessitate temporary or long-term assistance. The economic costs of post-stroke care are enormous; its complications impose a financial burden not only on the personal level but also on the global level. At present, the total global healthcare expenditure is approximately 34% on stroke [5]. The average per-person healthcare expenses of stroke, including inpatient care, rehabilitation, and follow-up care, tend to increase continuously in the future [6, 7].
The distribution of stroke risk factors is changing worldwide. Over the past few decades, Thai society has gradually transformed from a country of agriculture to an industrial nation. Urbanization, swift transition in the economy and health effects have changed Thai people's lifestyles, eventually increasing the prevalence of metabolic syndrome and cardiovascular diseases. Stroke is strongly related to being overweight, obesity, physical inactivity, smoking, drinking alcohol and congenital disease. Even though stroke is multifactorial, contributory risk factors such as uncontrolled Hypertension (HT) and Diabetes Mellitus (DM) with uncontrolled blood glucose levels play a crucial role. HT is the leading cause of stroke, accounting for up to 75% of all occurrences. Furthermore, DM is linked to a 30% increase in the risk of stroke [8, 9]. The study of the global prevalence of stroke in patients with diabetes and hypertension revealed that the prevalence rate was 5.8% - 32.3% [10, 11]. A study in Thailand observed that ischemic stroke, intracranial stroke and transient ischemic stroke were 22.9%, 12.0%, and 20.4%, respectively, among diabetes and hypertension patients [12].
Many environmental factors are attributed to the proximate environment. The impact of socioeconomic and environmental factors such as urbanization, density, and economic growth was likely to be associated with the development of stroke. Land surface temperature, changing weather conditions, and access to tobacco and alcohol stores correlated with the prevalence of stroke. Geospatial analysis showed that non-communicable diseases (NCDs) are prevalent in the adult and elderly population, particularly those living in urban areas. The prevalence of NCDs is believed to be influenced by increased per capita alcohol and tobacco intake, including stroke and cardiovascular disease [13-18].
Previous studies found that environmental risk factors are important causes of disease burden and their impacts on NCDs, specifically unhealthy diet and lifestyles; other environmental factors such as tobacco stores, urban or built-up lands, the concentration of the elderly population and land surface temperature is also related to various health problems. Geographic information systems (GIS) and spatial analysis are increasingly used to investigate spatial disease patterns. In particular, local indicators of spatial association (LISA) have demonstrated their usefulness in epidemiological studies, including stroke. Epidemiological research using GIS and spatial analysis methodologies has revealed that stroke has spread over numerous places with varying spatial patterns [19, 20]. Additionally, the SLM and SEM have also been applied to the situation of stroke for multivariate association verification and predictive analysis [21]. To our knowledge, very limited studies have been carried out to identify the factors of sociodemographic and environmental related to stroke in DM and HT patients in Thailand. Therefore, to fill this research gap, we have hypothesized whether sociodemographic and environmental factors could play a role in influencing stroke. Hence, this study aimed to investigate the spatial association between sociodemographic and environmental factors and the prevalence of stroke among DM and HT patients. The findings of this study will be used by the Ministry of Public Health (MOPH), academics, researchers, decision-makers and public health staff to build regional health strategies for stroke prevention and control. Furthermore, the findings of this study are critical for guiding evidence-based stroke care planning, prevention and resource allocation by analyzing the risk of stroke in various geographical regions and an innovative plan to reduce the burden of stroke among DM and HT patients.
2. METHODS
2.1. Ethical Consideration
The Khon Kaen University Ethics Committee approved the present study for Human Research (Reference No. HE642237).
2.2. Study Area
All 77 provinces of Thailand were selected for this study. Thailand is an upper-middle-income country in Southeast Asia with a population of around 66 million and a land area of 514,000 km2. The country has a land area of 511,770 km2 and a water area of 2,230 km2. There are 77 provinces, 878 districts, 7,225 sub-districts and 74,965 villages in the spatially administrative hierarchy.
2.3. Data Sources
These data were collected by the Health Data Center (HDC) of Thailand's MOPH between 2016-2021were used. The outcome is defined as having a stroke diagnosed previously by a physician. This study comprised 276,855 participants aged 35 years and above who matched the HDC inclusion criteria and were diagnosed with DM and/or HT. In addition, study participants were currently having insulin therapy or oral medications to control blood glucose levels and blood pressure, along with the participants being treated on a long-term basis.
The independent variables include provincial densities of alcohol stores available in the Center of Alcohol Studies (http://cas.or.th/cas/), provincial densities of tobacco stores available in the Center of Tobacco Studies (https://cts.rutgers.edu/) were collected. Similarly, the provincial concentration of elderly population data was acquired from the National Statistical Office of Thailand. In addition, the provincial concentration of Primary Care data was acquired from GIS Health, Ministry of Public Health (http://gishealth.moph.go.th/). The Land Surface Temperature (LST) data were detected by MODIS sensors, which use band frequencies of 20–23 and 30–31. LST is available from Google Earth Engine (https://developers.google.com/earth-engine/ datasets/catalog/MODIS _006_MOD11A1). The night time light (NTL) data for Thailand were extracted from Suomi National Polar-orbiting Partnership (SNPP) Visible Infrared Imaging Radiometer Suite (VIIRS) satellite available from Google Earth Engine (https://earthengine.google.com).
2.4. Data Analysis
The GeoDa program was used in analyzing spatial autocorrelation and determining the spatial regression of geographical factors, economy, society, and prevalence of stroke among DM and HT patients in Thailand. The distance was used as a criterion for the weight matrix, and spatial correlation was analyzed. One of the most common approaches for calculating the degree of geographical correlation is to use the spatial autocorrelation statistic (Moran's I) [24]. Moran's I was the slope of the linear fit to the scatter plot. The product-moment correlation coefficient's interpretation was identical to that of the product-moment correlation coefficient. A value of +1 shows strong positive spatial autocorrelation (i.e., clustering of similar values), a value of 0 suggests random spatial ordering, and a value of -1 indicates strong negative spatial autocorrelation. The mathematical specification of the Equation quantifies the strength of a relationship between xi and its neighbor xj. The spatial weight matrix wij defines the geographical relationship between xi and xj. In particular, xi-x and xj-x represent the deviation of xi and xj from the average of x, respectively. (i.e., clustering of dissimilar values) (i.e., a checkerboard pattern). The formula for calculating Moran’s I statistic is as follows [19, 25].
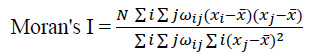 |
(1) |
Moran’s I have a flaw in determining the correlation's position. As a result, the mathematical core of Moran's I was extended to create local Moran I or LISA. In each location, it calculates spatial association. The generated maps (LISA significance maps) show sites with significant local Moran statistics and categories them by association type (LISA cluster maps). LISA's cluster maps feature four cluster categories: High-High, Low-Low, Low-High, and High-Low, and one pattern representing unpredictability. While Low-High and High-Low are not outliers, the statistically significant spatial correlation areas either imply a positive bivariate relationship with high incidence (High-High) or a positive bivariate link with low incidence (Low-Low) [22, 23].
2.5. Regression Analysis
The relation between sociodemographic factors and stroke rate in 77 provinces was examined with the regression models (i.e., SLM and SEM) using GeoDa version 1.6.6 to identify the presence of statistically significant stroke spatial clusters and multivariate associations [22].
Spatial regression models were used in analyzing the associations among socioeconomic factors, environment and prevalence of stroke among diabetes and hypertension patients in Thailand. The three main specifications of spatial regression models are (1) traditional OLS regression, (2) spatial lag model (SLM), and (3) spatial error model (SEM). SLM is mathematically defined, as shown in the following equation.
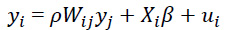 |
(2) |
Alternatively, the spillover effect can be integrated into regression using the SEM specification. This framework, in particular, permits the spatial influence of a location j to affect the area ivia the disturbance of cross-boundary relation. SEM is mathematically defined, as shown in the equation.
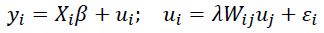 |
(3) |
The conventional form of the regression equation defines the combination of an independent variable Xi and disturbance ui jointly determining the dependent variable yi. Specifies a spillover influence originating from uj and affecting ui through the spillover coefficient λ and the spatial weight matrix Wij. The statistical significance of λ verifies the existence of spatial influence identified in SEM form by using statistical inference. The error term is Ɛi, which is independent and identically distributed [21].
The OLS regression has significant limitations in that it frequently assumes that the relationship between dependent and explanatory variables is uniform in space and does not account for spatial autocorrelation, which is frequently regarded as an outright violation of the classical regression model's principle of observation independence. Given that an OLS regression fails to detect the spillover effect, the usual specification is adjusted to include the impacts of neighboring areas, resulting in the SLM and SEM formulations. SLM presupposes a direct spatial influence between a specific location and its surroundings and is based on a spatially lagged dependent variable. Meanwhile, by allowing the influence of neighboring areas to pass through the disturbance term, SEM integrates indirect spatial dependency into the regression model [26]. The Akaike Information Criterion (AIC) value was also utilized to compare the model to the spatial regression model as a model selection decision indicator. It denotes a model with a high degree of goodness of fit. Models with small AIC values indicate a good fit.
3. RESULTS
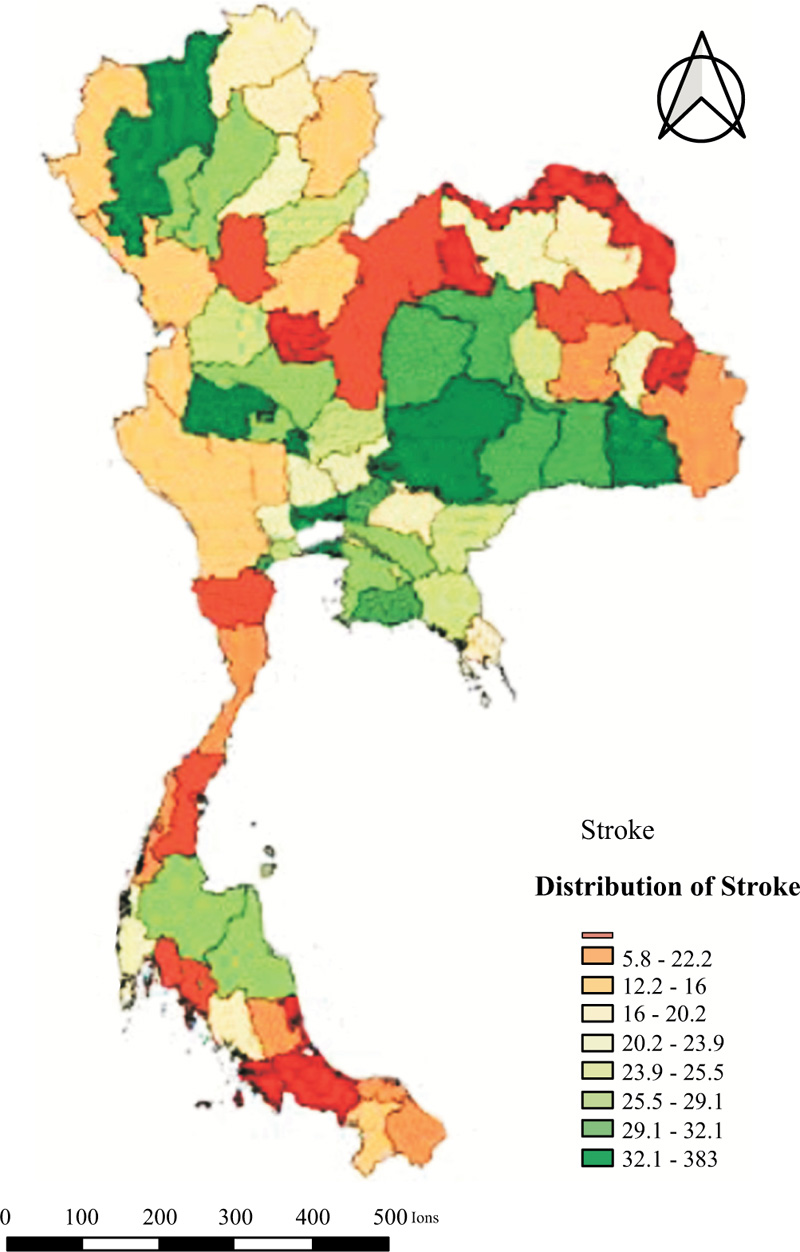
The overall stroke prevalence was 19.45 per 1,000 population. The highest prevalence was found in Uthai Thani (38.28/1,000 population), whereas the lowest was found in Nong Khai with 1.82/1,000 population. The quantile map indicated the highest deciles (32.1-38.3 per 1,000 population in eight provinces (Uthai Thani, Samut Prakan, Nakhon Ratchasima, Pathum Thani, Nonthaburi, Chiang Mai, Si Sa Ket, and Sing Buri;) (Fig. 1).
3.1. Local Spatial Patterns
The univariate Moran’s I scatter of the annual prevalence of stroke in Thailand’s provinces showed positive spatial autocorrelation. The Moran’s I value was 0.454, with a statistical level of significance (p < 0.05) with permutations (999). The clusters HH of stroke were mostly observed in the central region of Thailand, which included Chai Nat, Sing Buri, Ang Thong, Lop Buri, Ayutthaya, Saraburi, Nakhon Pathom, Nonthaburi, Pathum Thani, Nakhon Nayok, Samut Sakhon, Samut Prakan, Prachin Buri, Chachoengsao, Chon Buri, Buri Ram, and Surin however cold spot (low-low) clusters were located in Sakon Nakhon, Mukdahan, Songkhla, and Pattani mentioned in Table 1 (Figs. 2-4).
| Moran’s I | LISA | P-value | |||||
|---|---|---|---|---|---|---|---|
|
HH (17 Provinces) |
HL (2 Province) |
LL (4 Provinces) |
LH (1 Province) |
||||
| 0.454 | Chai Nat* Sing Buri** Ang Thong** Lop Buri* Ayutthaya** Saraburi* |
Nakhon Pathom* Nonthaburi** Pathum Thani*** Nakhon Nayok** Samut Sakhon* Samut Prakan*** |
Prachin Buri* Chachoengsao** Chon Buri* Buri Ram* Surin* |
Udon Thani* Yasothon* |
Sakon Nakhon* Mukdahan* Songkhla* Pattani* |
Suphan Buri** | 0.05* 0.01** 0.001*** |
3.2. Factors Associated with Stroke
Moran's I indicated significant statistical association patterns of an independent factor and stroke (p-value < 0.05). There was a spatial correlation between the distribution pattern of alcohol store density in the same direction as the stroke pattern. The outcomes of the bivariate LISA revealed a statistically significant positive correlation between alcohol store density and stroke (Moran's I= 0.184). LISA indicated areas with a concentration of alcohol stored and high prevalence of stroke with high values in the surrounding 3 provinces (Hot-spot or High-High cluster) in Chai Nat, Suphan Buri, Ang Thong, Ayutthaya, Saraburi, Nakhon Pathom, Nonthaburi, Pathum Thani, Nakhon Nayok, Samut Sakhon, Samut Prakan, Prachin Buri, Chachoengsao, Chon Buri, Buri Ram, and Surin. In contrast, LISA analysis showed clusters of a province with a low alcohol store density and stroke with low values of the surrounding 3 provinces (Cold-spot or low-low clusters). There were 4 low-low clusters in Sakon Nakhon, Mukdahan, Songkhla, and Pattani provinces, as shown in Table 2 (Fig. 5).
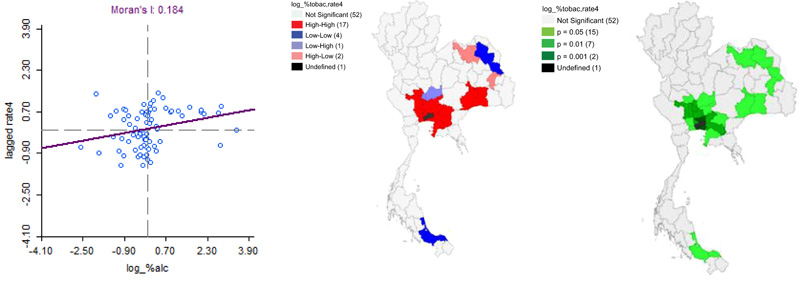
| Moran’s I | LISA | P-value | |||||
|---|---|---|---|---|---|---|---|
|
HH (16 Provinces) |
HL (2 Province) |
LL (4 Provinces) |
LH (2 Provinces) |
||||
| 0.184 | Chai Nat* Suphan Buri** Ang Thong** Ayutthaya** Saraburi* |
Nakhon Pathom* Pathum Thani*** Nakhon Nayok** Samut Sakhon* Samut Prakan*** Chachoengsao** |
Nonthaburi** Prachin Buri* Chon Buri* Buri Ram* Surin* |
Udon Thani* Yasothon* |
Sakon Nakhon* Mukdahan* Songkhla* Pattani* |
Sing Buri** Lop Buri** |
0.05* 0.01** 0.001*** |
There was a spatial autocorrelation of tobacco store density and a distribution pattern in the same direction with stroke (Moran's I of 0.165). The LISA analysis indicated 17 Hot-spots or High-High clusters of the high concentration of tobacco store and stroke with high values in the surrounding 3 provinces in Suphan Buri, Chai Nat, Lop Buri, Ang Thong, Ayutthaya, Saraburi, Nakhon Nayok, Prachin Buri, Chachoengsao, Chon Buri, Nonthaburi, Pathum Thani, Samut Prakan, Samut Sakhon, Nakhon Pathom, Buri Ram, and Surin. LISA analysis showed clusters of a province with a low concentration of tobacco stores and stroke with the low values of the surrounding 3 provinces (Cold spot). 4 low-low clusters in Sakon Nakhon, Mukdahan, Songkhla, and Pattani provinces are demonstrated in Table 3 (Fig. 6).
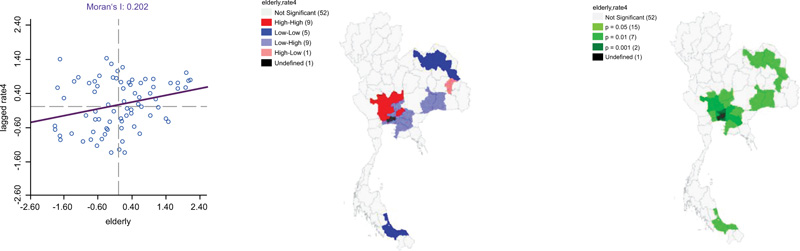
It has been revealed that the provinces have a high number of elderly populations high prevalence of stroke with a Moran's I of 0.202. The LISA analysis indicated 17 Hot-spots or High-High clusters of the high concentration of elderly population and patients with stroke with high values in the surrounding 3 provinces in Suphan Buri, Chai Nat, Sing Buri, Ang Thong, Lop Buri, Ayutthaya, Nakhon Pathom, Nonthaburi and Nakhon Nayok. In contrast, LISA analysis showed clusters of a province with a concentration of elderly population and prevalence of stroke was low values of surrounding 3 provinces (Cold-spot or low-low clusters). There were 9 low-low clusters found in Saraburi, Pathum Thani, Samut Sakhon, Samut Prakan, Chachoengsao, Prachin Buri, Chon Buri, Buri Ram, and Surin provinces illustrated in Table 4 (Fig. 7).
| Moran’s I | LISA | P-value | |||||
|---|---|---|---|---|---|---|---|
|
HH (17 Provinces) |
HL (2 Province) |
LL (4 Provinces) |
LH (2 Provinces) |
||||
| 0.165 | Suphan Buri** Chai Nat* Lop Buri* Ang Thong** Ayutthaya** Saraburi* |
Nakhon Nayok** Chachoengsao** Pathum Thani*** Samut Prakan*** Nakhon Pathom* Samut Sakhon* |
Prachin Buri* Chon Buri* Nonthaburi** Buri Ram* Surin* |
Udon Thani* Yasothon* |
Sakon Nakhon* Mukdahan* Songkhla* Pattani* |
Sing Buri** | 0.05* 0.01** 0.001*** |
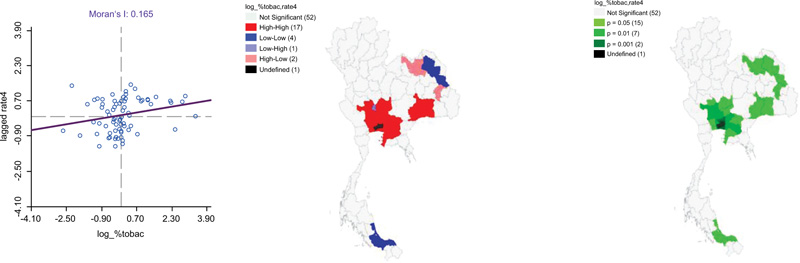
Table 4.
| Moran’s I | LISA | P-value | |||||
|---|---|---|---|---|---|---|---|
|
HH (9 Provinces) |
HL (1 Province) |
LL (9 Provinces) |
LH (5 Provinces) |
||||
| 0.202 | Suphan Buri** Chai Nat* Sing Buri** Ang Thong** Lop Buri* |
Ayutthaya** Nakhon Pathom* Nonthaburi* Nakhon Nayok** |
Yasothon* | Saraburi* Pathum Thani*** Samut Sakhon* Samut Prakan*** Chachoengsao** |
Prachin Buri* Chon Buri* Buri Ram* Surin* |
Udon Thani* Sakon Nakhon* Mukdahan* Songkhla* Pattani* |
0.05* 0.01** 0.001*** |
In addition, the bivariate LISA revealed a statistically significant negative correlation between primary care per population density and the prevalence of stroke (Moran's I= -0.109). LISA indicated areas with a concentration of primary care and a high prevalence of stroke with high values in the surrounding 3 provinces (Hot-spot or High-High cluster) in Chai Nat, Sing Buri, Ayutthaya, Ang Thong, and Saraburi. In contrast, LISA analysis showed clusters of a province with a low primary care per population density and stroke patients with low values in the surrounding 3 provinces (Cold-spot or low-low clusters). There were 3 low-low clusters found in Udon Thani, Sakon Nakhon, and Songkhla provinces. (Table 5) (Fig. 8)
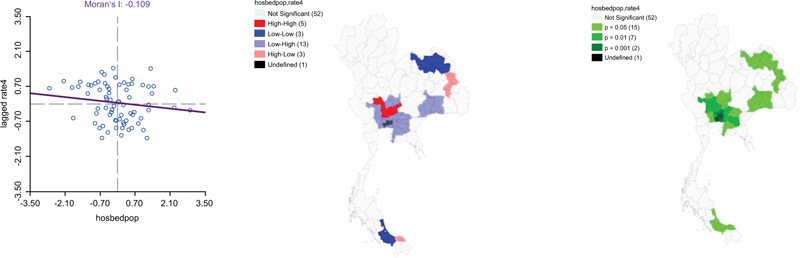
Table 5.
| Moran’s I | LISA | P-value | |||||
|---|---|---|---|---|---|---|---|
|
HH (5 Provinces) |
HL (3 Province) |
LL (3 Provinces) |
LH (13 Provinces) |
||||
| -0.109 | Chai Nat* Sing Buri** Ayutthaya** Ang Thong** Saraburi* |
Mukdahan* Yasothon* Pattani* |
Udon Thani* Sakon Nakhon* Songkhla* |
Nakhon Pathom* Samut Sakhon* Samut Prakan*** Pathum Thani*** |
Suphan Buri** Nonthaburi** Nakhon Nayok** Chachoengsao** |
Lop Buri* Prachin Buri* Chon Buri* Buri Ram* Surin* |
0.05* 0.01** 0.001*** |
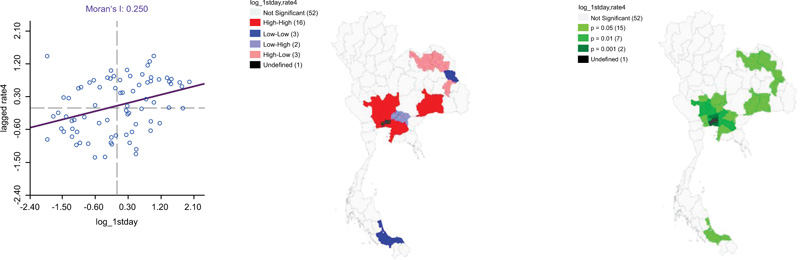
The temperature of LST (day) mean per square kilometer has a spatial autocorrelation of concentration of LST (day) and a distribution pattern prevalence of stroke in the same direction with a Moran's I of 0.250. The LISA analysis indicated 16 Hot-spots or High-High clusters of the high temperature of LST (day) and patients having a stroke with high values in the surrounding 3 provinces in Suphan Buri, Chai Nat, Sing Buri, Ang Thong, Ayutthaya, Lop Buri, Saraburi, Nakhon Pathom, Nonthaburi, Pathum Thani, Samut Sakhon, Samut Prakan, Chachoengsao, Chon Buri, Buri Ram, and Surin. LISA analysis showed clusters of a province with a concentration of LST (day) and stroke with low values of surrounding 3 provinces (Cold-spot or low-low clusters). There were 3 low-low clusters found in Mukdahan, Songkhla, and Pattani provinces, as can be seen in Table 6 (Fig. 9)
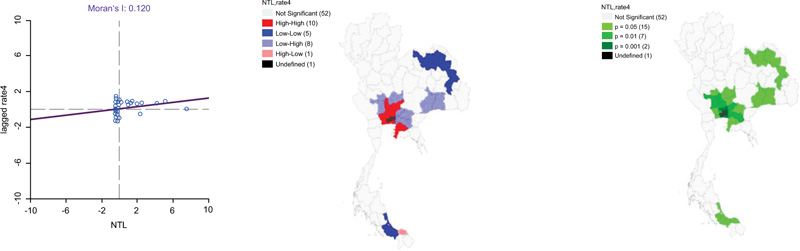
Moreover, there was spatial autocorrelation of concentration of NTL and a distribution pattern in the same direction with stroke with a Moran's I of 0.120. The LISA analysis indicated 10 Hot-spots or High-High clusters of the high NTL index and stroke with high values in the surrounding 3 provinces in Sing Buri, Ang Thong, Ayutthaya, Saraburi, Nakhon Pathom, Nonthaburi, Pathum Thani, Samut Sakhon, Samut Prakan, and Chon Buri. In contrast, LISA analysis showed clusters of a province with a concentration of NTL and stroke with low values of the surrounding 3 provinces (Cold-spot or low-low clusters). There were 5 low-low clusters found in Udon Thani, Sakon Nakhon, Mukdahan, Yasothon, and Songkhla provinces, respectively summarized in Table 7 (Fig. 10).
| Moran’s I | LISA | P-value | |||||
|---|---|---|---|---|---|---|---|
|
HH (16 Provinces) |
HL (3 Province) |
LL (3 Provinces) |
LH (2 Provinces) |
||||
| 0.250 | Suphan Buri** Chai Nat* Sing Buri** Ang Thong** Lop Buri* Ayutthaya** |
Nakhon Pathom* Pathum Thani*** Samut Sakhon* Samut Prakan*** Chachoengsao** |
Saraburi* Nonthaburi** Chon Buri* Buri Ram* Surin* |
Udon Thani* Yasothon* Sakon Nakhon* |
Mukdahan* Songkhla* Pattani* |
Nakhon Nayok** Prachin Buri* |
0.05* 0.01** 0.001*** |
| Moran’s I | LISA | P-value | |||||
|---|---|---|---|---|---|---|---|
|
HH (10 Provinces) |
HL (1 Province) |
LL (5 Provinces) |
LH (8 Provinces) |
||||
| 0.120 | Sing Buri** Ang Thong** Ayutthaya** Saraburi* Chon Buri* |
Nakhon Pathom* Nonthaburi* Pathum Thani*** Samut Sakhon* Samut Prakan*** |
Pattani* | Udon Thani* Sakon Nakhon* Yasothon* Mukdahan* Songkhla* |
Suphan Buri** Chai Nat* Lop Buri* Buri Ram* Surin* |
Nakhon Nayok** Prachin Buri* Chachoengsao** |
0.05* 0.01** 0.001*** |
3.3. Spatial Regression Analysis
The spatial modelling results are summarized in Table 8. The results of the OLS regression and SLM model estimated concentration of the elderly population was likely to be associated with having a stroke. The OLS and SLM models explained approximately 30.40% and 46.20% of stroke prevalence (R2 = 0.304) and (R2=0.462), respectively. In addition, the last SEM showed that 4 factors (tobacco store density, the concentration of the elderly population, land surface temperature (day), and nighttime light) were significant predictors and explained approximately 50.80% of stroke prevalence (R2 = 0.508).
| Factors | OLS | Spatial Regression Analysis Model | |
|---|---|---|---|
| SLM | SEM | ||
| Alcohol store density | 0.009 | 0.005 | 0.010 |
| (0.011) | (0.009) | (0.009) | |
| Tobacco store density | 0.068 | 0.059 | 0.065* |
| (0.054) | (0.046) | (0.049) | |
| The concentration of the elderly population | 0.012** | 0.009** | 0.013*** |
| (0.003) | (0.003) | (0.004) | |
| Primary care density | -0.017 | -0.014 | -0.019 |
| (0.025) | (0.021) | (0.020) | |
| Land Surface Temperature (day) | 0.889 | 0.855 | 1.417* |
| (0.772) | (0.652) | (0.726) | |
| Nighttime light | 0.019 | 0.012 | 0.021* |
| (0.011) | (0.009) | (0.010) | |
| Constant | 1.180 | - | - |
| (1.023)* | |||
| P | - | 1.105 | - |
| (0.863)*** | |||
| λ | - | - | 1.878 |
| (0.960)** | |||
| F-stat | 5.028 | - | - |
| R-Squared | 0.304 | 0.462 | 0.508 |
| Log Likelihood | 81.582 | 88.962 | 90.863 |
| AIC | 194.16 | 161.92 | 157.71 |
| BIC | 232.85 | 223.28 | 215.41 |
Note: **Correlation is significant at the 0.01 level.
Note: ***Correlation is significant at the 0.001 level.
Therefore, SEM was the best regression model. The parameter estimation shows that the tobacco store density, concentration of the elderly population, land surface temperature (day)and nighttime light density were positively autocorrelated with the prevalence of stroke. The R2 value indicated that SEM accounted for 50.80% of the variation in stroke. In the AIC test, SEM slightly outperformed the SLM with AIC157.71 versus 161.92, respectively. Therefore, SEM showed better performance in explaining the geographical distribution of the prevalence of stroke among diabetes and hypertension patients in Thailand.
4. DISCUSSION
In this present study, we have initiated to identify a spatial association between sociodemographics, environmental factors and the prevalence of stroke among diabetes and hypertension patients in Thailand. A wide variation in stroke prevalence was found among diabetes and hypertension patients in Thailand. Stroke clusters were found in almost every region of the country because stroke prevalence varies. Our findings suggested that sociodemographic and environmental factors are significantly positively correlated to the prevalence of stroke, including the density of tobacco stores, concentration of the elderly population, land surface temperature (day) and night-time light density.
One of the important findings of our study was the significant positive spatial correlation between the density of tobacco stores and the prevalence of stroke. The previous study found that the number of shops selling tobacco present a conducive environment for smokers. Similarly, people who smoke have more risk of stroke than people who do not smoke by approximately 1.5 - 6 times [3, 5]. The present fast and convenient telecommunication and business in the form of aggressive marketing by continuously advertising various forms such as sales promotion from public sectors will help for the distribution of tobacco's selling point comprehensively as well as supporting showcase is a passive tobacco advertising at the selling point, producing equipment for sale promotion, and organizing promotional activities. Therefore, tobacco selling points near the community will increase the chance of easy accessibility and further increase the smoking number and new smokers, which is significantly responsible for raising the chances of ischemic stroke or hemorrhagic stroke causing paralysis [16, 27-29].
Moreover, our study also revealed that the concentration of the elderly population correlated with the prevalence of stroke. Age is one of the most critical risk factors for developing stroke. The prevalence of stroke has been rising continuously in the past years [30, 31]. According to the ageing mechanism of the human body, it leads to the change of cross-substance such as collagen and elastin and the transformation of the internal substance of the tissue cells, which makes it harden, dry and lack an elastic, especially the organ that is frequently found deterioration are skin and vascular. Therefore, vascular deterioration by age affects having a stroke in the elderly more than that of other aged people [11, 12, 31, 32].
Our results indicated the association between the density of LST (day) and the prevalence of stroke. The findings of this present study corresponded with many previous studies, which found that heat waves' effect on surface temperature affects mortality from cardiovascular disease and stroke [18]. The rising surface temperature and infrared heat waves make a phenomenon of heat dome- which leads to the surface transformation and temperature that directly affect human blood circulation and lead to mortality causing cardiovascular diseases and stroke. In particular, the area that the risk group was living in is dense and precarious to expose surface temperature to the elderly, the poor and children. [33].
In our setting, NTL also predicts a significant positive correlation with the prevalence of stroke. As conventionally acknowledged, NTL is a good proxy of economic activity. Therefore, NTL density was useful in quantitatively characterizing the intensities of socioeconomic activities, urbanizations, and lifestyle. Our result was consistent with the findings of WHO, which revealed that urbanization correlates with increased incidence of chronic diseases in large urban areas because of differences in lifestyle [34]. Similarly, a previous study found that the mortality rate due to stroke was in the upper rank of the big cities in many countries, i.e., nearly 70%. [35]. This might be due to the urban area dweller having to face the risk factor affecting the living conditions because a health problem in an urban area is related to the transformation of environmental, social conditions, economic conditions, and culture [13, 15]. Similarly, the study also suggested that the incidence and prevalence of stroke will be higher in people who lived or moved to areas with more prosperity or urban areas. [36]
This study has drawn the roadmap of spatial association between sociodemographic and environmental factors and the prevalence of stroke among diabetes and hypertension patients in Thailand. This study has been a stepping stone to enhance the spatial factors and their contributions to stroke and related death. Thus, efforts should be devoted to strengthening health promotion on stroke prevention, such as controlling risk factors, especially health behavior and physiology factors. People can be health promoters for themselves by having health literacy and the skills to prevent health risks of themselves and creating participation with family, health team, and community to support the controlling of risk factors to reduce the risk of having a stroke.
Furthermore, the public sector should promote the determination of working plans and guidelines to prevent stroke using an integration working procedure and supporting the participation of the community and all sectors to create a health-literate society through policymaking mechanisms or tools to prevent population risk. Furthermore, the government should promote a healthy environment, especially in urban areas. Besides, the public sector should have a role in developing a comprehensive and strictly applied law, which includes increasing tobacco tax; banning tobacco advertising, promotion, and sponsorship. Moreover, applications of spatial analysis using open data and open-source software packages in public health planning should also be promoted and extended to other diseases.
CONCLUSION
Worldwide prevalence of stroke has been increasing in trend as of Thailand. Spatial autocorrections on the prevalence of stroke had been significantly clustered in several provinces of Thailand. Distribution of alcohol stores, the density of tobacco stores, the concentration of older adults, increasing day temperature, and the density of NTL were significantly likely to be associated with enhancing the prevalence of stroke in the cluster and neighboring provinces of Thailand.
Therefore, the main findings of this study will be helpful for policymakers, medical practitioners, researchers, and developers to develop effective strategies for reducing the stroke burden in a country. Specifically, the obtained analytical results would help the government in prioritizing present programs aimed at curtailing the prevalence of NCDs in specific geographic regions, particularly in the central region where the prevalence of stroke is extremely high
LIST OF ABBREVIATIONS
| GBD | = Global Burden of Diseases |
| NCDs | = Non-communicable Diseases |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethics approval was received from the Khon Kaen University Ethics Committee for Human Research (Reference No. HE642237).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were per the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analysed during this study are available on request from the corresponding author [W.L.].
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors thank the Ministry of Public Health for sharing health data.


