All published articles of this journal are available on ScienceDirect.
Prevalence of Smoking and its Associated Factors among Adolescent Males in Bangladesh: A Community Survey
Abstract
Background:
Smoking is considered the symbol of adulthood and a “friend” during stress and loneliness to many adolescent people. It is well established that most adults start tobacco use in late childhood or adolescence. This study aimed to determine the smoking prevalence and its influencing factors among Adolescent males in a selected community in Bangladesh.
Methods:
A descriptive cross-sectional study was conducted from January to December 2019 among adolescent males in Savar Upazila, Dhaka, Bangladesh. A total of 472 adolescent males were recruited through the household survey using a proportional probability sampling (P.P.S.) procedure. The sociodemographic and smoking information was collected using an interviewer-administered semi-structured questionnaire. Various statistical analyses were performed.
Results:
The Prevalence of smoking was 25.0%. The bivariate analysis showed that age, religion, education, occupation, peer influence, and social stigma for the attraction were all associated (P<0.05) with smoking among adolescents. The multivariate analysis revealed that the smoking risk was six times higher (OR=6.46, 95% CI: 3.49-11.98) among the participants who see the smoking habit makes people more attractive and happier, about forty-two times (OR=41.9, 95% CI: 10.1-173.3) among those with a friend who smokes, about twenty times higher (OR=19.89, 95% CI: 9.2-42.8) among those who had a smoker in the family and more than two times higher (OR=2.721, 95% CI: 1.16-6.4) among respondents who had higher secondary & above level of education.
Conclusion:
In Bangladesh, particularly in rural regions, little is known regarding the incidence of adolescent smoking and associated risk factors. Peer pressure, stress, anxiety, weight loss, copying popular culture, celebrity influence, and tobacco product availability were critical factors in the study participants' decision to smoke. As a result, special regulations and actions should be implemented to curb current adolescent smoking patterns.
1. INTRODUCTION
Tobacco use is one of the leading risk factors for several non-communicable diseases. More than 5 million deaths world-wide can be attributed to direct tobacco use [1]. Bangladesh is one of the most populous countries in the 'world.' A large segment of Bangladesh's total population, about 35.3% (37.8 million adults), are tobacco users [2]. According to the Global Adult Tobacco Survey (GATS), the prevalence of smoking increased with decreasing socioeconomic status in Bangladesh [2]. Adolescent age is a transitional period from infancy to adulthood, in which a person experiences rapid physical, mental, and social growth and development [3]. During this period, the ability for abstract thinking, distinguished from concrete thought, increases gradually through solving problems or making decisions. Approximately 90% of the people who smoke for the first time are adolescents, and the rate of smoking among them is rising steadily [4]. The stressful life events during adolescence are associated with adopting unhealthy behaviors such as tobacco smoking; social circumstances and physical traits can moderate the relationship. Despite considerable success from decades of anti-smoking messages, increasing taxes on tobacco products, purchasing restrictions, and social norms that shame and stigmatize smokers, the problem persists [5].
Tobacco (smoking and smokeless) is now more easily accessible, available, and socially acceptable, that is why more adolescents access it and thus become addicted [6]. Tobacco smoking is associated with multiple health problems. It is considered one of the most preventable risk factors for six of the eight leading causes of morbidity and mortality at the global level [7]. In Bangladesh, the number of tobacco smokers is increasing daily because of the cheap availability of tobacco products, the lack of strong tobacco control regulations, and the weak enforcement of existing rules [7]. Bangladesh has a vast number of street children. Most of them maintain tenuous ties with their families, and some have no families, resulting in a highly stressful life. Tobacco smoking gives these kids excitement and relief from the all-pervasive gloom of street life and suppresses hunger, stress, and helplessness [8]. In 2007, a survey reported that about 5 million Bangladeshi died of tobacco-related illnesses. The aggressive marketing strategy of the national and multinational tobacco companies leads to a considerable burden of tobacco consumption and related consequences [9].
Most smokers start smoking at a younger age; about 80% initiate in their teens and become daily smokers as adolescents [10]. Smoking is associated with poor health and a variety of short-term adverse health effects in young people. Moreover, it may be a factor for underlying mental health problems like depression among adolescents. The smoking habit is seen mainly among the poor young generation because of the lack of awareness and poor practical education. The factors like peer pressure for smoking, attractive advertising for tobacco use, desire to look mature and availability are influencing factors for smoking [11].
In Bangladesh, the smoking prevalence is higher than the global prevalence among males. The prevalence of smoking among young males aged 13 to 15 is 13.2% [12]. Peer smoking is the most significant predictor of smoking among youths and young adults. Peer networks in which half or more members are smokers significantly increase the possibility of current tobacco smoking [13]. The direct and indirect loss due to the harmful effect of smoking is immeasurable. Smoking affects individual smoker, their family, and society. High costs are being used to treat smoking-related illnesses, besides reducing the strength of individuals' working capacity [14]. Smoking-related beliefs and perceived norms in individuals' social networks are essential in promoting tobacco cessation in our country. But it is challenging to prevent or intervene in smoking because of the high rates of smoking in this country and the high prevalence of smokers in individuals' social aspects [15]. Previous studies in Bangladesh have revealed the prevalence, burden, risk factors, and health effects of smoking in the workplace, public places, and homes among adults [1, 16-19]. However, little is known about adolescent smoking prevalence and its factors in Bangladesh, particularly in rural areas. This study aims to determine the prevalence of smoking and its related factors among Adolescent males in Bangladesh.
2. METHODS
2.1. Study Design, Period, Population, and Setting
A twelve-month descriptive cross-sectional study was carried out (January to December 2019). The study focused on the adolescent males of Savar's Bank colony. According to the 2011 Bangladesh census, the Savar is a Dhaka district Upazila with 1,387,426 people, including 207,401 persons aged 18 and older. Males accounted for 54.2 percent of the population. Savar is around 24 kilometers northwest of Dhaka, Bangladesh's capital.
2.2. Sample Size, Sampling Technique, and Selection Criteria
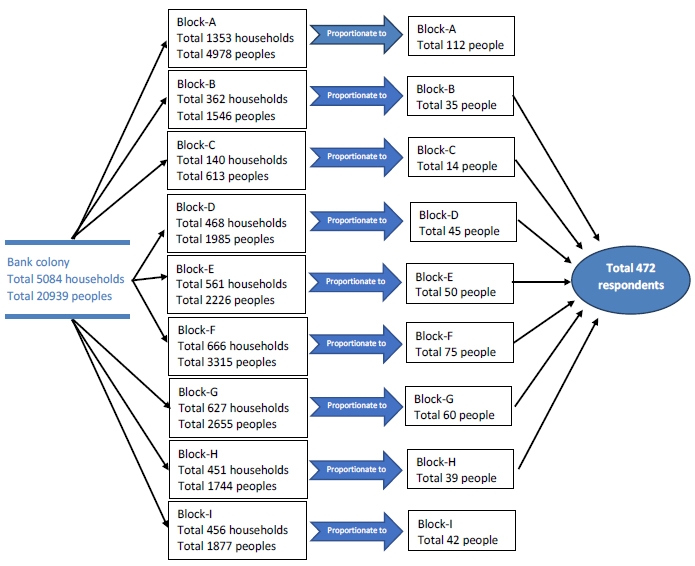
This study enlisted the participation of 472 adolescent males. A sampling frame was developed from the household survey. This study's target population was drawn out using probability proportional-to-size (PPS) sampling. The list of households in the Bank colony was combined with the total number of persons living in those houses, and 472 participants were proportionately selected (Fig. 1). The respondents were chosen based on the following criteria for inclusion: (1) adolescent males (between the ages of 10 and 18); (2) residents of Savar Upazila's Bank colony; (3) physically capable; and (4) willing to take part in the study.
2.3. Data Collection Procedure and Management
The survey instrument used in this study was created based on similar studies conducted in Bangladesh [7, 20]. The semi-structured interviewer-administered questionnaire utilized in this study was first developed and verified before data collection. The questionnaire incorporates both structured and unstructured interviewing techniques. In our survey, only a few predetermined questions were used. Instead, the descriptive response was elicited through open-ended questions. The questions were kept simple and easy to understand. Public health specialists and behavior scientists were asked to evaluate the instrument and provide feedback on the content's relevance and accuracy and the instrument's relevancy and simplicity. The English questionnaire was first created and then translated into Bangla, and the Bangla version of the questionnaire was utilized to collect data. Before the data was collected, the questionnaire was pretested on 30 people in the PalliBidyut residential area of Ashulia, Dhaka. The results of the pretesting were not included in the final analysis. Experts' advice was sought to reshape the questionnaire into a more manageable, simpler, and shorter instrument that could be completed in a short amount of time.
Smoking is the act of inhaling and exhaling the fumes of burning plant material. The information was gathered using a semi-structured questionnaire presented by an interviewer that included questions about socio-demographics, smoking status, patterns, and reason. The sociodemographic factors studied were age, religion, education, occupation, and income. Smoking habits, peer influence, reasons for smoking, duration, the existence of a smoker in the family, and plan to quit smoking were all components of the smoking-related variables. The purpose of the study was explained in detail to the respondents and their guardians before data collection. Before beginning the data collection, the respondents and their guardians gave informed consent. The data was acquired using a face-to-face interview when the principal investigator visited the respondents' homes.
2.4. Data Analysis
Before the data collection, the questionnaire was coded to simplify it into statistical software. Each questionnaire was double-checked for completeness following the data collection, and the entire data set was double-checked for consistency and accuracy. Then, data were entered, coded, cleaned, and finally analyzed using the Statistical Package for Social Sciences (SPSS 20 version). Multiple statistical analyses such as Chi-square (χ2) test, bivariate logistic regression, and multivariate logistic regression were used to correlate different variables.
3. RESULTS
3.1. Sociodemographic Characteristics of the Respondents
A total of 472 respondents participated in this survey. The mean age (±SD) of the adolescents was 16.3 (±1.29) years, and 404(85.6%) of the respondents were Muslims. Most of the adolescents' fathers, 308(65.3%), were jobholders, whereas most mothers, 314(66.5%), were homemakers. Most families had a monthly income of 50,000 BDT, and the majority of adolescents, 394(83.5%), had ≤4 family members. Of 472 adolescents, 404(85.6%) had up to secondary education, 348(73.7%) of the respondents' fathers had a Bachelor's degree or above, and 284(60.2%) of the respondents' mothers had less than a Bachelor's degree. The prevalence of smoking was substantially (P<0.05) linked with age, both parents' employment, the family's monthly income, and educational qualifications (respondents, fathers, and mothers) in this study. However, there was no significant association (P>0.05) between religion, family size, and smoking prevalence (Table 1). Out of 472 adolescents, 118(25.0%) were smokers, and 354(75.0%) were non-smokers. Moreover, the calculated probability and OR of smoked respondents were 0.25 and 0.33, respectively. Thus, the prevalence of smoking tobacco products among adolescents is 25%. It represents one-fourth of all adolescent household members who smoke for various reasons, including peer pressure, stress and anxiety management, weight loss, copying popular culture, celebrity impact, and various other issues (Table 1).
3.2. Risk Factors of Smoking among Adolescent Male
Other factors were shown to be considerably greater in contributing to the teenage smoking habit after controlling for relevant confounders. According to the bivariate study, age, religion, education, father's work, peer influence, and societal stigma for the attraction were all linked to using tobacco (smoking) among adolescent males. The risk of smoking was more than two times higher (OR=2.721, 95% CI: 1.16-6.4) among respondents who had higher secondary & above levels of education. Compared to non-smokers, the opinion of smokers as highly attractive and cheerful (OR=6.46, 95% CI: 3.49-11.98) was six times higher among adolescent smokers. Furthermore, smoking risk was about forty-two times higher (OR=41.9, 95% CI: 10.1-173.3) among those with a friend who smokes. The smoking risk was about twenty times higher (OR=19.89, 95% CI: 9.2-42.8) among those who had a smoker in the family. Religion, opinions about smoking and comfort, and plans to quit smoking shortly, on the other hand, were determined to be insignificant in the multivariate analysis (P>0.05) (Table 2).
| Demographic Characteristics | Prevalence of Smoking | χ2 | p-value | |
|---|---|---|---|---|
| Yes, n (%) | No n (%) | |||
| Age (years) | ||||
| ≥14 to ≤16 | 12 (4.7) | 240 (95.3) | 38.9 | 0.000 |
| ≥17 to ≤18 | 106 (48.2) | 114 (51.8) | ||
| Mean ± SD | 16.33 ±1.29 | |||
| Religion | ||||
| Muslim | 104 (25.7) | 300 (74.3) | 4.1 | 0.25 |
| Non-Muslim | 14 (20.6) | 54 (79.4) | ||
| Father's Occupation | ||||
| Service holder | 60 (19.5) | 248 (80.5) | 22.9 | 0.000 |
| Business & Others | 58 (35.3) | 106 (64.7) | ||
| Mother's Occupation | ||||
| Housewife | 64 (20.4) | 250 (79.6) | 11.2 | 0.004 |
| Job & Others | 54 (34.1) | 104 (65.9) | ||
| Family Monthly Income (BDT) | ||||
| ≥1500 to<50,000 | 92 (22.7) | 314 (77.3) | 10.3 | 0.000 |
| ≥50,000 to 200000 | 26 (39.4) | 40 (60.6) | ||
| Family Size | ||||
| ≤4 members | 92 (23.4) | 302 (76.6) | 9.3 | 0.053 |
| ≥5 members | 26 (33.4) | 52 (66.6) | ||
| Educational Qualification | ||||
| Up to Secondary | 88 (21.8) | 316 (78.2) | 15.5 | 0.000 |
| Higher Secondary & Above | 30 (44.1) | 38 (55.9) | ||
| Father's Educational Level | ||||
| Below Graduation | 50 (40.3) | 74 (59.6) | 45.8 | 0.000 |
| Graduation & Above | 68 (19.5) | 280 (80.5) | ||
| Mother's Educational Level | ||||
| Below Graduation | 56 (19.8) | 228 (80.2) | 17.5 | 0.004 |
| Graduation & Above | 62 (33) | 126 (67) | ||
| Total | 118(25.0) | 354(75.0) | ||
| Characteristics/Risk Factors |
Bivariate Analysis OR (95% C.I.) |
P-value |
Multivariate Analysis OR (95% C.I.) |
P-value | |
|---|---|---|---|---|---|
| Age (years) | 14≥ to 16 ≤ | 1 | 1 | ||
| 17≥ to 18≤ | 0.239 (0.18 -0.32) | 0.000 | 0.25(0.18-.35) | 0.000 | |
| Religion | Muslim | 1 | 1 | ||
| Non-Muslim | 2.174 (1.24-3.8) | 0.006 | 1.39(0.78-2.48) | 0.257 | |
| Father's occupation | Service holder | 1 | 1 | ||
| Business &Others | 1.628 (1.10-2.4) | 0.013 | 1.77(1.06-2.95) | 0.031 | |
| Mother's occupation | Housewife | 1 | 1 | ||
| Business &Others | 0.803(0.55-1.18) | 0.263 | 0.31 (0.19-0.50) | 0.000 | |
| Respondents Educational Qualification | Up to Secondary | 1 | 1 | ||
| Higher Secondary & Above | 0.427(0.23-0.80) | 0.008 | 2.721(1.16-6.4) | 0.021 | |
| Smoking habit makes people more attractive and happier | No | 1 | 1 | ||
| Yes | 5.92(3.88-9.04) | 0.000 | 6.46 (3.49-11.98) | 0.000 | |
| Close friends smoked tobacco | No | 1 | 1 | ||
| Yes | 15.89(7.53-33.54) | 0.000 | 41.9 (10.1-173.3) | 0.000 | |
| Opinion regarding weight reduction | No | 1 | 1 | ||
| Yes | 0.279(0.65-1.2) | 0.086 | 0.16 (0.03-0.84) | 0.031 | |
| Opinions about smoking and comfort | No | 1 | 1 | ||
| Yes | 0.63(0.35-1.15) | 0.130 | 0.47 (0.14-1.52) | 0.206 | |
| Duration of smoking | No | 1 | 1 | ||
| Yes | 3.004(0.631-4.30) | 0.167 | 2.03 (1.32-3.11) | 0.001 | |
| Presence of smokers in the family | No | 1 | 1 | ||
| Yes | 0.82(0.43-1.6) | 0.565 | 19.89 (9.2-42.8) | 0.000 | |
| Plan to quit smoking shortly | No | 1 | |||
| Yes | 1.49(0.57-3.89) | 0.421 | 1.9(0.85-6.46) | 0.278 | |
4. DISCUSSION
Adolescent smoking is a severe problem that has received particular attention in current health policy. In developing countries, smoking is now acknowledged as a significant public health issue. Bangladesh is one of the most populous countries in the developing world. The Union's projects in Bangladesh focus on strengthening civil society for long-term tobacco control sustainability, developing and enforcing sub-national smoke-free initiatives, and assisting the Bangladeshi government in improving and effectively implementing national tobacco control legislation and policy. A cross-sectional study was undertaken among 472 adolescent males to determine smoking prevalence. The respondent's mean age (±SD) was 16.3±1.3 years. Similar studies conducted in India, Zimbabwe, and China revealed 16.6±1.3, 15.9±1.8, and 15.35±1.84 years [21-23]. The prevalence of smoking among the 472 male adolescents was 25.0 percent, much lower than the national prevalence rate of 35.3% percent predicted by GATS in 2017 [2]. In a prior survey of adolescents in Brazil, the prevalence of smoking was reported to be 29.3 percent [24]. Another study conducted among high school students in Zimbabwe indicated that 37.8% of males had ever smoked [22].
According to the bivariate analysis, age, religion, education, father's occupation, the impact of peers, and societal stigma for the attraction were all linked to smoking among adolescent males. Peer influence [25] and a sense of inferiority were predictors of teenage smoking [26]. Smoking prevalence was more likely to double among adolescents with less than a high school education (OR=2.721, 95% CI: 1.16-6.4). A comparable study found that school-level among vocational high school students was positively linked with current adolescent smoking (OR=3.14, 95% CI: 2.49-3.98) [23].
The smoking risk was 42 times higher (OR=41.9, % CI: 10.1-173.3) among those with a smoking friend. In addition, having a smoking friend (OR=5.67, 95% CI: 2.06-7.09) and having cigarettes offered by friends (OR=4.21, 95% CI: 2.46-5.76) were found to be factors linked to smoking in a study [24]. Another study discovered that exposure to smokers increased one's likelihood of becoming a smoker (OR=8.7, 95% CI: 5.9-12.8) [22]. Parents should discourage their kids from making friends with smokers so that peer pressure will not influence them to start smoking.
Those who had a smoker in the family were about twenty times more likely to smoke (OR=19.89, % CI: 9.2 - 42.8). According to a study conducted in China, teenagers are likely to smoke when their parents smoke (OR=1.24, 95% CI: 1.09-1.40) [23]. According to another study, teenagers with smoker parents were likelier to be smokers (OR=1.7, 95% CI: 1.2-2.5) according to another study [22]. A family member should quit smoking to prevent adolescents from being enticed to smoke. Because the study was conducted in a specific location with a small sample size, it is essential to undertake a similar study with a larger sample size and in a different place to address this geographic and sampling limitation [27, 28]. The study was cross-sectional, and a semi-structured interview was used. The design of the present study may result in some biases. The respondents are primarily aware of the hazardous effects of tobacco. However, still, a considerable number of male adolescents smoke [29]. This shows the need for specific regulations and measures. Close associates should offer moral support to their children during stress and anxiety [30, 31]. There is much need for education and awareness regarding the harmful effects of smoking in society [32-34].
CONCLUSION
Adolescent smoking prevalence is more than the national average, which appears to be undesirable given the harmful health impacts of smoking. Peer pressure, coping with stress and anxiety, losing weight, copying popular culture, celebrity influence, and the availability of tobacco products are all common reasons for adolescent smoking. In addition, despite being fully aware of the hazardous effects of tobacco, a considerable number of male adolescents smoke. Therefore, specific regulations and measures should be implemented to lower the current trends of teenage smoking. In times of stress and anxiety, parents and family members should offer moral support to their children, who may be tempted to start smoking to relieve the tension. In addition, parents, teachers, and older members of society should educate adolescents about the adverse effects of smoking more comprehensively and intensively to increase their motivation to quit smoking. As a result, it's critical to undertake a more extensive study with a diverse population.
LIST OF ABBREVIATIONS
| BDT | = Bangladesh Taka |
| DIU | = Daffodil International University |
| ERC | = Ethical Review Committee |
| GATS | = Global Adult Tobacco Survey |
| OR | = Odds Ratio |
| PPS | = Proportional Probability Sampling |
| SD | = Standard Deviation |
ETHICS APPROVAL AND CONSENT TO PARTICIPATION
The study was approved by the Ethical Review Committee (ERC) of Dhaka Medical College.
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT TO PUBLICATION
Informed consent was obtained from all participants of this study.
STANDARDS OF REPORTING
STROBE guidelines were followed.
FUNDING
None.
AVAILABILITY OF DATA AND MATERIAL
The data and material are available on request from the corresponding author [F.M].
CONFLICT OF INTERESTS
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors are thankful to all respondents of this study and those who helped or contributed in one way or another while conducting this study.


