RESEARCH ARTICLE
Analysis of a Typical COVID-19 Outbreak Spread by Tourist Groups
Ling Zheng1, #, Jinxi Yao2, #, Yunhui Yu1, Bo Wang1, Bin Luo1, *
Article Information
Identifiers and Pagination:
Year: 2022Volume: 15
E-location ID: e187494452212060
Publisher ID: e187494452212060
DOI: 10.2174/18749445-v15-e221206-2022-74
Article History:
Received Date: 16/5/2022Revision Received Date: 6/10/2022
Acceptance Date: 1/11/2022
Electronic publication date: 28/12/2022
Collection year: 2022

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Novel coronavirus disease (SARS-COV-2 infection or COVID-19) is a respiratory tract infection that has been linked to severe acute respiratory syndrome transmitted particularly through touching and respiration. The purpose of this study is to understand the epidemiological characteristics of COVID-19 cases in a typical tourist-related outbreak and explore the possible route for its transmission.
Methods:
All data and epidemiological survey reports of COVID-19 cases in the outbreak were reported by provincial and urban (county) Centers for Disease Control and Prevention and Health Commissions nationwide from October 16th to November 5th, 2021. The epidemiological survey reports included information on gender, age, source of infection (imported from other provinces or locally acquired), daily life track and itinerary, date of symptom onset, and date of diagnosis. The data were analyzed using descriptive statistical methods, one-way analysis of variance, independent t-test, and Chi-square tests. Histograms and percentage stacked area plots were used to describe the epidemiological characteristics of the outbreaks.
Results:
The COVID-19 outbreak associated with the tourist groups has involved 551 COVID-19 cases, with a median age of 44 years (interquartile range: 30-59 years), gradually spreading from the northwestern region to the national level across 15 provinces of China. One-fifth of the cases (16.0%) had traveled to Ejin Banner, resulting in 68 second-generation cases. We estimated an outbreak on 11 flights and 19 trains, accounting for a total of 27 confirmed cases. In addition, 42 clusters of outbreak cases were also reported to occur, 21 (50.0%) in households and 10 (23.81%) in restaurants. About 106 confirmed cases were related to the gatherings in restaurants. The median incubation period for this COVID-19 outbreak was 7 days (inter-quartile range: 5-10 days).
Conclusion:
The survey results indicated that this COVID-19 outbreak originated in Ejin Banner and was spread by tourist groups, which was a typical infection outbreak promoted by travel. Our results further confirmed that travel needs to be more strictly weighed in pandemics like COVID-19, and people need to pay more attention to the prevention against infectious diseases, particularly when traveling in a tourist group.
1. INTRODUCTION
Coronavirus disease 2019 (COVID-19), caused by the emergence of the novel pathogen severe acute respiratory syndrome coronavirus 2 (SARS-COV-2), has spread with alarming speed and on an extensive scale since it was first reported in Wuhan, Hubei Province, China, in late December 2019 [1]. On March 11th, 2020, following the outbreak of COVID-19, World Health Organization (WHO) declared the current situation as a pandemic [2]. So far, 476,374,234 cases have been confirmed, causing 6108,976 deaths (WHO) [3].
A great deal of studies have confirmed that the two primary transmission routes of SARS-CoV-2 spread are through contact (direct and indirect contact) or droplets [4-6]. The official reports of WHO announced that virions through airborne transmission in droplet nuclei with a particle size of < 5 µm can exist for long periods of time, with travel distances > 1 m [7]. These aerosols with virions attached may travel through ventilation systems in buildings and enclosed spaces, eventually invading other areas away from any infected individual [5]. Furthermore, a recent study has even suggested that airborne transmission may be the dominant mode of transportation [6].
Multiple studies have shown that novel coronavirus transmission may be travel-related [8-10]. The human infection risk could be extremely high due to the length of the exposure time window, transmission routes, and structural characteristics during travel or work [11, 12]. Public transport might have been less safe to use during the COVID-19 pandemic due to the enclosed space and the difficulty to maintain social distancing [8]. Zhu's investigation in the early periods of the COVID-19 outbreak showed that high-speed rail (HSR) and air connectivity with Wuhan resulted in 25.4% and 21.2% increases in the average number of daily new confirmed cases, respectively, while their suspension led to 18.6% and 13.3% decreases in that number [13]. Researchers performed correlation analysis based on the data released by the Chinese National Health Commission, and showed that the incidence rate was higher in the regions receiving the largest number of travelers during this period, further confirming the epidemiological characteristics [14]. Travel restrictions have been used in many countries around the world to stop the epidemic, and a combination of non-pharmaceutical interventions, such as early detection, isolation of cases, and travel restrictions, has been found to be more effective [14-16].
Recent studies have indicated SARS-CoV-2 to demonstrate 10-20 times greater affinity to angiotensin-converting enzyme 2 (ACE2) receptors compared to SARS-CoV-1, making it a much more virulent virus [17, 18]. This means fewer SARS-CoV-2 virions are necessarily needed to establish a successful infection in humans. Currently, the most common novel coronavirus strain is the Delta variant, which is characterized by strong infectivity, high viral load, and shortened incubation period [19], and is gradually becoming the main cause of the high incidence of COVID-19. It has been reported that the Delta strain can infect even after 14 seconds without contact [16]. Individuals infected with Delta variant could develop typical clinical symptoms 2 to 3 days after infection and could cause five generations of cases within 10 days with a R0 (basic infected population) of 4.04 to 5.0. This has been reported to be much higher than that of the prototype strain that was isolated in Wuhan (2.2 to 3.77) [19, 20].
The current outbreak has spread rapidly, but the causes of the rapid occurrence of the outbreak and its spread to several provinces have not been reported. Therefore, the purpose of this study is to understand the epidemiological characteristics of COVID-19 cases in a typical tourist-related outbreak and explore the possible route for its transmission, so as to provide a reference for the prevention and control of COVID-19 in the post-pandemic era.
2. METHODS
2.1. Inclusion Criteria
COVID-19 confirmed cases were defined according to the guidelines of the Novel Coronavirus Pneumonia Prevention and Control Program, eighth edition [21]. Asymptomatic infected persons were not included. A selection of 551 COVID-19-confirmed cases directly or indirectly related to tourist groups in Inner Mongolia and Gansu was reported by provincial and urban (county) Centers for Disease Control and Prevention and Health Commissions nationwide from October 16th to November 5th, 2021. Among these COVID-19 cases, investigated by questionnaires, 441 COVID-19-confirmed cases were collected with specific information, including information on gender, age, source of infection (imported from other provinces or locally acquired), daily life track and itinerary, date of symptom onset and date of diagnosis.
2.2. Definition of Cluster Outbreaks
Cluster outbreaks were defined in accordance with the Guidelines for the Epidemiological Investigation of Outbreaks of Novel Coronavirus Pneumonia (Trial Version 1) [22]. The “small area” of an outbreak is not limited to homes, workplaces, and units, but also includes places, such as nursing homes, hospitals, laboratories, or transport, such as planes, trains, automobiles, and ships [22].
2.3. Definition of Incubation Period
The incubation period was defined as the interval between the source of transmission (wildlife or people with suspected or confirmed cases) and the earliest date of symptom onset (i.e., cough, fever, fatigue, or myalgia) [23]. Symptomatic episodes in patients with COVID-19 were defined as one or more of the following symptoms: cough, dyspnea, fever, chest tightness, muscle aches, chills, fatigue, and diarrhea.
To estimate the incubation period of COVID-19, the exposure periods were inferred from the travel history to Ejin Banner and the exposure history of the confirmed cases, as follows: (i) If the patients had a travel history in Ejin Banner two weeks before symptoms onset and stayed in Ejin Banner for less than a week, the left and right endpoints of the suspected infection date window were set to the date of entry and exit from Ejin Banner, respectively; (ii) If the patients had no travel history in Ejin Banner two weeks before symptoms onset and had clear contact periods with the confirmed patients, the left and right endpoints of the suspected infection date window were set to the date of initial exposure and the date of last exposure, respectively; (iii) If the patient had a history of staying in Ejin Banner for more than one week or had unclear contact periods with the confirmed patients, the exposure periods could not be recorded [24]. The summary statistics for the incubation period were calculated from 312 patients who had clear information about the date of exposure.
2.4. Statistical Analysis
The data were analyzed using descriptive statistical methods [mean±SD and frequency (%)], one-way analysis of variance (for group comparison), independent t-test, and Chi-square tests (for comparing qualitative data). Histograms and percentage stacked area plots were used to describe the epidemiological characteristics of the outbreaks. Basic characteristics of confirmed COVID-19 cases were analyzed by gender in subgroups. The incubation periods of confirmed COVID-19 cases were stratified for different generations. All data were processed with SPSS 26.0 statistical software, and GraphPad prism 8.0.2, R 4.1.2, and ArcGIS 10.8.2 software were used to draw statistical graphs.
3. RESULTS
3.1. Overview of the Outbreak
3.1.1. National COVID-19 Epidemiological Trends
From October 16th to November 5th, 2021, the outbreak associated with the tourist groups involved 551 COVID-19-confirmed cases, spreading across 15 provinces of China. The number of new confirmed cases per day rose significantly on October 21st and peaked on November 2nd. The daily number of new cases has gradually decreased since November 2nd, as shown in Fig. (1).
3.1.2. Temporal Distribution
In terms of the national trend, after the first case was reported on October 16th, 2021, cases reported in Gansu, Inner Mongolia and Ningxia were found at an early stage, and the second peak appeared successively with the nucleic acid screening of all staff. The epidemic was found to be basically controlled after November 5th, as shown in Fig. (2).
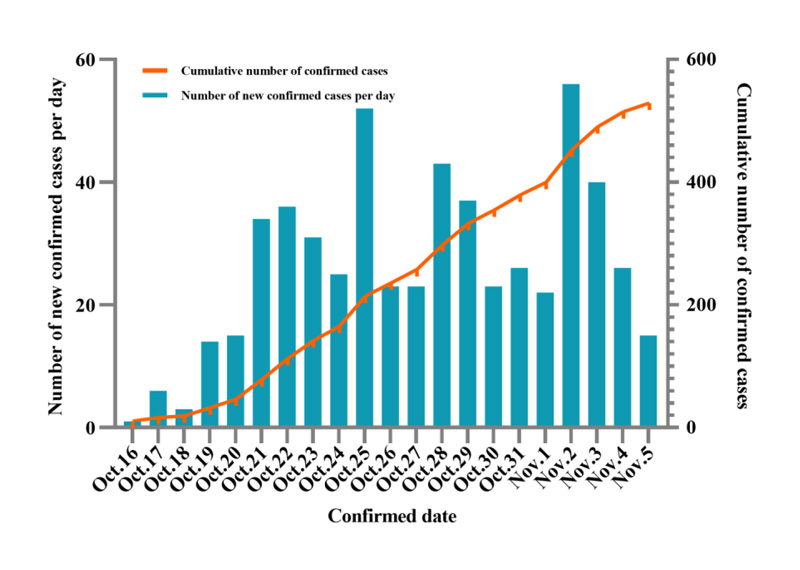 |
Fig. (1). The trend of COVID-19-confirmed cases in 15 provinces of China from October 16th to November 5th, 2021. |
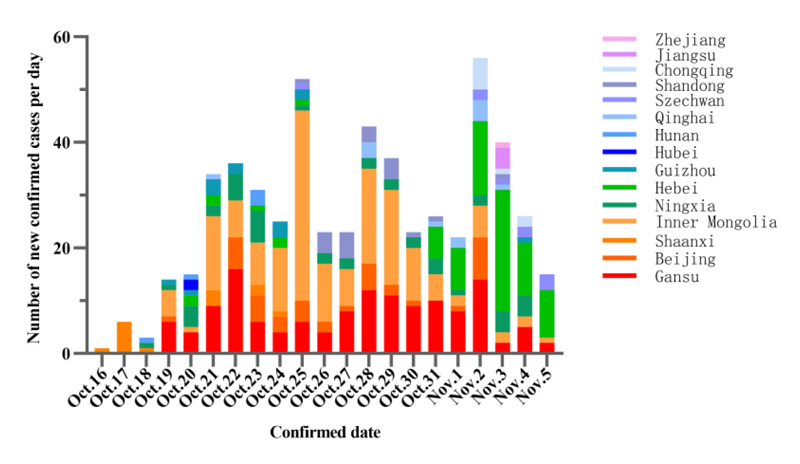 |
Fig. (2). Temporal distribution of COVID-19-confirmed cases in 15 provinces of China from October 16th to November 5th, 2021. |
3.1.3. Spatial Distribution
In accordance with spatial distribution, COVID-19 cases were mainly concentrated in five provinces, namely, Inner Mongolia (165 cases), Gansu (136 cases), Hebei (78 cases), Ningxia (44 cases) and Beijing (39 cases), accounting for 83.85% (462/551 cases) of the total number of confirmed cases. The overall trend was a gradual spread from the northwestern region to the national level, as shown in Fig. (3).
3.1.4. Population Distribution
The personal information of 441 confirmed cases was collected, with a gender ratio of 221 (male):220 (female). The oldest age was 87 years and the youngest age was 1 year, with a mean of 43.84 ± 20.45 years and a median age of 44 years (interquartile range: 30-59 years). The median age was 44 years (interquartile range: 30-59 years), but there was a difference in the age of the infected population by gender (p< 0.05), and the age of female cases was significantly older than that of male cases. Patients over 50 years old accounted for the largest proportion (40.14%), as shown in Fig. (4).
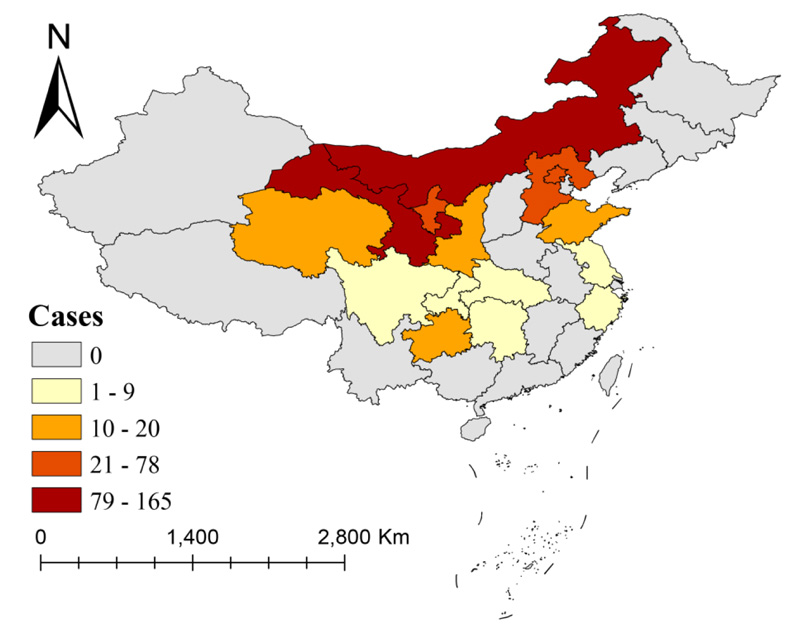 |
Fig. (3). Regional distribution of COVID-19 confirmed cases in 15 provinces of China from October 16th to November 5th, 2021. |
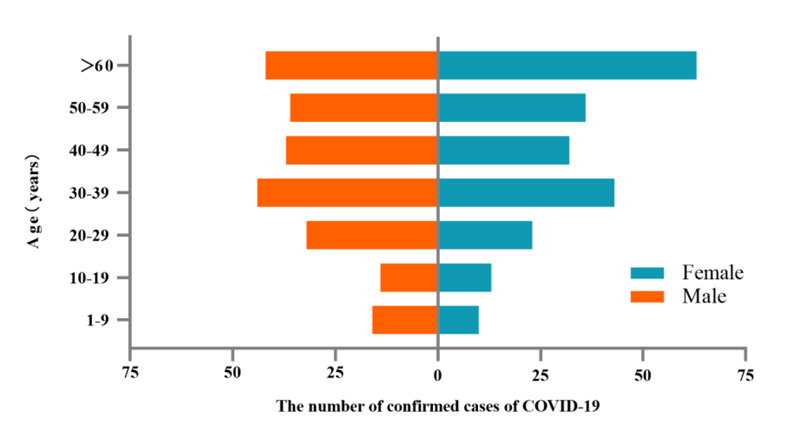 |
Fig. (4). Gender and age distribution of confirmed COVID-19 cases in 15 provinces of China from October 16th to November 5th, 2021. |
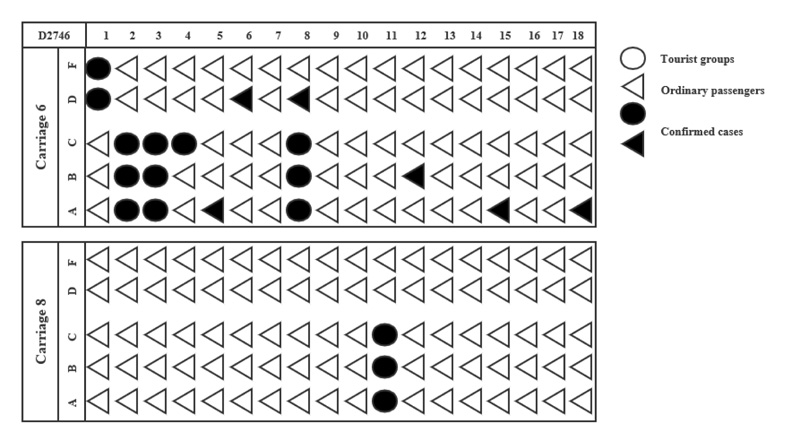 |
Fig. (5). Seats distribution of COVID-19 confirmed cases on train D2746 in China. |
3.2. Transmission Pathway
3.2.1. COVID-19 Transmission through Public Places
The analysis revealed many secondary cases to spread through gathering in restaurants. A total of 42 clusters of cases have been reported. There were 21 cases reported due to family gathering (50.0%), 10 due to restaurant gathering (23.81%), 5 due to work gathering (11.9%), 2 of train gathering (4.76%), 2 of entertainment gathering (4.76%), and 2 of mixed gathering (4.76%). Among them, the restaurant cluster involved the most cases, up to 106.
The current round of outbreak included 11 flights and 19 trains, with a total of 27 confirmed cases. Among them, there were 21 (77.78%) cases reported on the train D2746 from Yumen to Lanzhou West on October 15th, 2021. The number of cases on this train involved 18 in carriage 6 and 3 in carriage 8. No confirmed cases were found in carriage 7 and other carriages. The distribution of seats is shown in Fig. (5). The ratio of male to female cases in this train was 1:1.1, and the average age was 55.62 years. All members of the tourist groups were diagnosed, and there was a cluster of cases in carriage 6, where all six non-tourist-group members were found to be infected.
3.2.2. The Coronavirus Spread through Tourist Groups
The main transmission line of this round of epidemic was tourist groups. In 8 out of the 15 provinces (53.33%), more than half of the first cases had a history of travel to Inner Mongolia, such as Ejin Banner. The transmission within three generations of COVID-19 cases is shown in Fig. (6), and each line represents a different mode or route of transmission.
3.3. Incubation Period
The incubation period was calculated using 312 confirmed cases with a clear time of exposure and symptoms onset, and included six generations of cases. The mean and median incubation periods were 7.6 ± 3.4 days and 7.0 (5.0-10.0) days, respectively. The incubation period for first-generation cases was relatively short, with a median of 5.0 (4.0-6.5) days, which were 6.0 (5.0-8.0) days and 9.00 (7.0-11.0) days in the second and the third generation cases. Also, there was no significant difference found between the fourth-generation and the fifth-generation cases in the incubation time, with a median time of 8.0 (5.0-11.0) days. The shortest incubation period was only 1.0 day, and the longest incubation period reached 19.0 days. There were 50 cases (16.0%) with Ejin Banner travel history, resulting in 68 second-generation cases. In addition, some COVID-19 cases with unknown trajectories were not included. 188 cases (60.3%) had an exposure interval of less than one day and were mostly secondary cases, as shown in Fig. (7).
4. DISCUSSION
The COVID-19 virus sequencing results from the provincial CDC in China showed the virus responsible for the spread of the outbreak to be a Delta variant strain (B.1.617.2 evolutionary branch). Previously, no strains of this type of mutant virus have been found in China's indigenous new coronaviruses, suggesting the outbreak to be caused by the spread of an imported virus from outside China. Information on the local trajectory of confirmed cases in Ejin Banner, Inner Mongolia, pointed to the Cek port (a bilateral year-round land port open to China and Mongolia), which is a well-known tourist attraction, and multiple local coal drivers have been diagnosed.
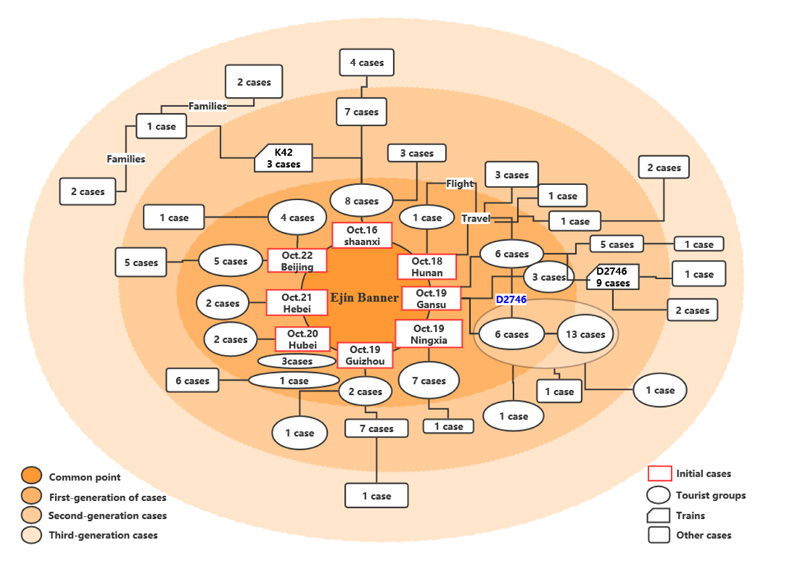 |
Fig. (6). Schematic diagram of the transmission chains of the relevant parts of the COVID-19 tourist groups within three generations of cases in China. |
The National Day holiday of China ushered in the peak of tourism in the area, and frequent activities of foreign tourists, who traveled between various scenic spots, hotels and restaurants, exacerbated the local epidemic. There were 50 cases (16.0%) with Ejin Banner tourism history, resulting in 68 second-generation cases, which accounted for about 1/3 of the total confirmed cases. The rest 2/3 were spread by subsequent crowd activities, so it can be seen that timely isolation of the source of infection is a significant prevention and control measure. In addition, the weather during that period was cooler and dryer, which may also have accelerated this outbreak, since cooler and dryer environments may possibly prolong the viruses' survival [1].
The transmission of the current outbreak spread between different tourist groups was mainly through public transport, involving multiple flights and trains. Among them, train D2746 had the largest number of cases, mainly found in carriage 6 with 18 confirmed cases and carriage 8 with 3 confirmed cases. Considering the ventilation system of trains [25], it is reasonable to believe that all these cases in carriage 8 were infected in the tourist area or waiting hall at the train station. Six ordinary passengers in carriage 6 who were not part of tourist groups were infected in the carriage. Experimental work by Doremalen et al. suggested that aerosol transmission of SARS-CoV-2 is plausible because the virus could survive in aerosols for hours and remain infectious on the surface of objects for up to several days, causing more severe transmission, especially in confined spaces [26]. Tourists from the same group often stayed in the same confined spaces, such as attractions, public transport means, hotels and restaurants, which led to the rapid spread of COVID-19. Besides, during train rides, passengers would like to talk, eat, and move, which may promote virus transmission in such proximity to viruses attached to aerosols and droplets [27]. In addition, frequent contact with surfaces, such as armrests and seats, could also be a potential route for COVID-19 infection [28]. The study by Hu et al. showed that the limited time interval between repeated seat use, disinfecting seats, and improving hand hygiene may help reduce the risk of transmission [29]. All of the evidence suggests the possibility and danger of COVID-19 transmission in public transportation, like train carriages. But whether or not being infected in the carriages could be related to many factors, such as indoor airflow, virus-specific factors, aerosol properties, host-specific factors, and so on [30]. The cases in carriage 8 did not cause secondary cases. We suspect that the ventilation system of the carriage was in continuous operation, which cause the indoor airflow to be in a state of circulation, making the virus concentration low and the masks and the bodies' own immunity sufficient to resist.
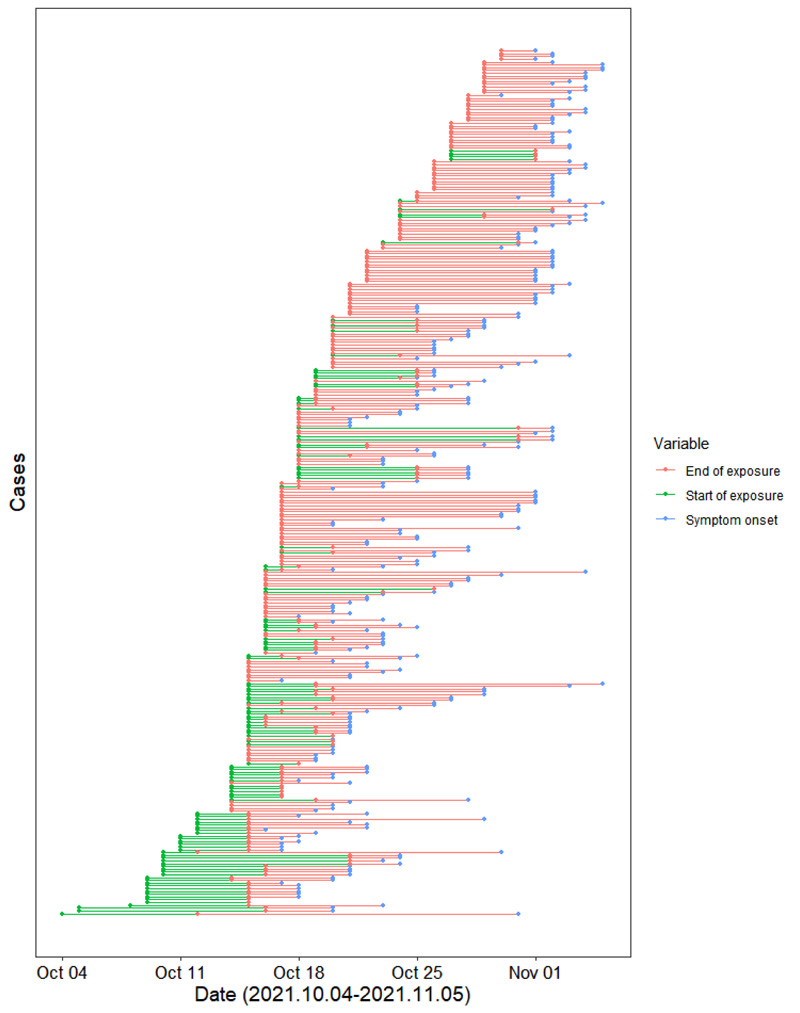 |
Fig. (7). 312 SARS-COV-2 exposure and timing of symptom onset in confirmed cases of China. |
The median incubation period for the generation of cases in the current COVID-19 outbreak was 5 days, similar to pneumonia with β-attributable novel coronavirus infection [20]. Generally, the incubation period depends on the amount of virus reaching the body. The higher the viral load in the body, the shorter the incubation period [31]. Cases with no travel or residence history in the Ejin Banner tended to experience a longer incubation period and more dispersed distribution, whereas cases with a history of travel and residence in the Ejin Banner showed a shorter incubation period. This may be explained by their repeated exposure to the source of infection during their stay. As the number of infectious generations increased, the incubation period gradually lengthened, reaching about 9 days by the third generation of cases, and the longest incubation period reached 19 days, suggesting that the pathogenicity of the virus would become weaker generation by generation [32].
As the outbreak began in elderly tourist groups, the majority of infected in the early stages of the outbreak were aged 50 and older. Some studies have shown that the elderly population and those with an underlying disease are generally more susceptible to the virus [33]. The response and course of infectious diseases may be altered in the elderly due to immune senescence and the common occurrence of secondary immuno-deficiencies in old age [34]. Moreover, our study showed aged females to be more infected than males. This may have something to do with more females in the infected tourist groups. Some studies have investigated the population in mainland China, and the results showed females to be more susceptible than males [35]. In general, females are more susceptible to SARS-CoV-2 infection, especially in certain age groups. Infection with SARS-CoV-2 occurs primarily through the angiotensin-converting enzyme 2 (ACE2) receptor, which acts as a gateway for the virus to enter tissues [36]. ACE2 gene is located on the X chromosome. Therefore, female individuals should have a higher ACE2 level [37], which may be the reason why they are more likely to be infected with SARS-CoV-2 compared to males. Further studies on sex-related ACE2 enzyme activity are needed to test this hypothesis. In China, 90% of COVID-19 deaths occur in people over 60 years of age, and 20% of deaths are in people over 80 years of age [38]. But with the inter-generational spread of the epidemic, there is a tendency to infect younger people, even children under the age of 1. This is most likely related to the infection of their parents or family members [39, 40].
The limitations of this study mainly come from three aspects. First, although the sample size of 312 cases could meet the basic needs of estimating the incubation period, a more effective sample size would be stronger in inferring the conclusion. Second, the classification of a case as a primary or secondary case was based only on the time of symptom onset, which might lead to misclassification due to delayed symptom onset for some primary cases than that of secondary cases. Third, all the data were collected from the publicly available epidemiological survey and supplementary materials in the journal literature. Thus, there may be recall bias over the exposure time and onset time of cases.Finally, this study has analyzed a typical COVID-19 outbreak spread by tourist groups, which may give us some tips for future COVID-19 prevention to some degree.
CONCLUSION
In conclusion, the current outbreak occurred in Ejin Banner, suggesting it to be caused by an imported virus from abroad and spread throughout the country by tourist groups, making it a typical infection outbreak promoted by travel. Considering the faster spread and stronger infection rate, the regular surveillance of the epidemic situation should be strengthened so as to cut off the routes of mobile clusters of infection in a timely manner. Besides, data have proved the lower rate of serious illness among the newly infected COVID-19 cases, so there is a necessity to readjust the prevention and control measures in order to adapt the economic development, like higher precision of surveillance and prevention, strengthening effective ventilation in public places, and so on [21]. Our results further confirm that travel needs to be more strictly weighed in pandemics like COVID-19, and people need to pay more attention to the prevention against infectious diseases, particularly when traveling in a tourist group.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus Disease 2019 |
| SARS-COV-2 | = Severe Acute Respiratory Syndrome Coronavirus 2 |
| WHO | = World Health Organization |
| ACE2 | = Angiotensin-converting Enzyme 2 |
AUTHORS’ CONTRIBUTION
Ling Zheng collected and analyzed the data, and wrote the original draft; Jinxi Yao contributed to the writing and investigation of the survey; Yunhui Yu contributed to the collection and sorting of the data; Bo Wang revised the manuscript; Bin Luo contributed to the conceptualization, methodology, writing review and editing. All authors have read and approved the final version to be submitted.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was exempted from institutional review board approval. All data were supplied and analyzed in an anonymous format without access to personal identifying information. At the same time, according to the law on public health response in China, formal ethical review and approval of this outbreak investigation were not required.
HUMAN AND ANIMAL RIGHTS
No animal/human studies are presented in this manuscript.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
STROBE guidelines and methodologies were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [B.L], on special request.
FUNDING
This study was funded by the Gansu Key Research and Development Program (Grant No. 20YF2FA028) and the Fundamental Research Funds for the Central Universities, Lanzhou University, China (Grant number: lzujbky-2021-ey07).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors acknowledge the Gansu Provincial Center for Disease Control and Prevention for providing partial COVID-19 cases data.
REFERENCES
| [1] | Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382(8): 727-33. |
| [2] | World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19. 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 (Accessed on: 11 March 2020). |
| [3] | World Health Organization. WHO Coronavirus (COVID-19) Dashboard | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data. 2022. Available from: https://covid19.who.int/ Accessed on: 25 March 2022). |
| [4] | Kaur H, Thakur JS, Paika R, Advani S. Impact of underlying comorbidities on mortality in SARS-COV-2 infected cancer patients: A systematic review and meta-analysis. Asian Pac J Cancer Prev 2021; 22(5): 1333-49. |
| [5] | Correia G, Rodrigues L, Gameiro da Silva M, Gonçalves T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med Hypotheses 2020; 141: 109781. |
| [6] | Bazant MZ, Bush JWM. A guideline to limit indoor airborne transmission of COVID-19. Proc Natl Acad Sci USA 2021; 118(17): e2018995118. |
| [7] | World Health Organization. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations: scientific brief. 2020. Available from: https://apps.who.int/iris/handle/10665/331616 (Accessed on: 29 March 2020). |
| [8] | Zhao S, Zhuang Z, Ran J, et al. The association between domestic train transportation and novel coronavirus (2019-nCoV) outbreak in China from 2019 to 2020: A data-driven correlational report. Travel Med Infect Dis 2020; 33: 101568. |
| [9] | Bogoch II, Watts A, Thomas-Bachli A, Huber C, Kraemer MUG, Khan K. Pneumonia of unknown aetiology in Wuhan, China: Potential for international spread via commercial air travel. J Travel Med 2020; 27(2): taaa008. |
| [10] | Findlater A, Bogoch II. Human mobility and the global spread of infectious diseases: A focus on air travel. Trends Parasitol 2018; 34(9): 772-83. |
| [11] | Shen J, Duan H, Zhang B, et al. Prevention and control of COVID-19 in public transportation: Experience from China. Environ Pollut 2020; 266(Pt 2): 115291. |
| [12] | Li Q, Guan X, Wu P, et al. Early transmission dynamics in wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med 2020; 382(13): 1199-207. |
| [13] | Zhu P, Guo Y. The role of high-speed rail and air travel in the spread of COVID-19 in China. Travel Med Infect Dis 2021; 42: 102097. |
| [14] | Chen J, Feng Z, Ye L, et al. Travel rush during Chinese Spring Festival and the 2019-nCoV. Travel Med Infect Dis 2020; 37: 101686. |
| [15] | Devi S. Travel restrictions hampering COVID-19 response. Lancet 2020; 395(10233): 1331-2. |
| [16] | Lai S, Ruktanonchai NW, Zhou L, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 2020; 585(7825): 410-3. |
| [17] | Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020; 181(2): 271-280.e8. |
| [18] | Wrapp D, Wang N, Corbett KS, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 2020; 367(6483): 1260-3. |
| [19] | von Massow G, Oh S, Lam A, Gustafsson K. Gamma delta T Cells and their involvement in COVID-19 virus infections. Front Immunol 2021; 12: 741218. |
| [20] | Shiehzadegan S, Alaghemand N, Fox M, Venketaraman V. Analysis of the Delta Variant B.1.617.2 COVID-19. Clin Pract 2021; 11(4): 778-84. |
| [21] | Beijing: Office of the National Health Commission. Notice on the publication of COVID-19 Prevention and Control Programme (Eighth edition). Joint Prevention and control Mechanism. 2021. Available from: http://www.gov.cn/xinwen/2021-05/14/content_5606469.htm (Accessed on: 14 May 2021). |
| [22] | Beijing: Chinese Center for Disease Control and Prevention. Notice on the publication of guidelines on epidemiological Investigation of COVID-19 Clusters (trial version 1). 2020. Available from: https://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11815/202003/t20200309_214241.html (Accessed on: 9 March 2020). |
| [23] | Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382(18): 1708-20. |
| [24] | Dai J, Yang L, Zhao J. Probable longer incubation period for elderly COVID-19 cases: Analysis of 180 contact tracing data in Hubei Province, China. Risk Manag Healthc Policy 2020; 13: 1111-7. |
| [25] | Shinohara N, Sakaguchi J, Kim H, et al. Survey of air exchange rates and evaluation of airborne infection risk of COVID-19 on commuter trains. Environ Int 2021; 157: 106774. |
| [26] | van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020; 382(16): 1564-7. |
| [27] | Zhen J, Chan C, Schoonees A, Apatu E, Thabane L, Young T. Transmission of respiratory viruses when using public ground transport: A rapid review to inform public health recommendations during the COVID-19 pandemic. S Afr Med J 2020; 110(6): 478-83. |
| [28] | Morawska L, Milton DK. It is time to address airborne transmission of coronavirus disease 2019 (COVID-19). Clin Infect Dis 2020; 71(9): ciaa939. |
| [29] | Chen J, He H, Cheng W, et al. Potential transmission of SARS-CoV-2 on a flight from Singapore to Hangzhou, China: An epidemiological investigation. Travel Med Infect Dis 2020; 36: 101816. |
| [30] | Berry G, Parsons A, Morgan M, Rickert J, Cho H. A review of methods to reduce the probability of the airborne spread of COVID-19 in ventilation systems and enclosed spaces. Environ Res 2022; 203: 111765. |
| [31] | Hu M, Lin H, Wang J, et al. Risk of Coronavirus Disease 2019 transmission in train passengers: An epidemiological and modeling study. Clin Infect Dis 2021; 72(4): 604-10. |
| [32] | Brufsky A, Lotze MT. Ratcheting down the virulence of SARS-CoV-2 in the COVID-19 pandemic. J Med Virol 2020; 92(11): 2379-80. |
| [33] | Huang S, Li J, Dai C, Tie Z, Xu J, Xiong X, et al. Incubation period of coronavirus disease 2019: New implications for intervention and control. Int J Environ Health Res 2021; 4: 1-9. |
| [34] | Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect 2020; 80(6): e14-8. |
| [35] | Qian J, Zhao L, Ye RZ, Li XJ, Liu YL. Age-dependent gender differences in COVID-19 in Mainland China: Comparative study. Clin Infect Dis 2020; 71(9): ciaa683. |
| [36] | Batlle D, Wysocki J, Satchell K. Soluble angiotensin-converting enzyme 2: A potential approach for coronavirus infection therapy? Clin Sci (Lond) 2020; 134(5): 543-5. |
| [37] | Bhatia K, Zimmerman MA, Sullivan JC. Sex differences in angiotensin-converting enzyme modulation of Ang (1-7) levels in normotensive WKY rats. Am J Hypertens 2013; 26(5): 591-8. |
| [38] | Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. JAMA 2020; 323(13): 1239-42. |
| [39] | Chen ZM, Fu JF, Shu Q, et al. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr 2020; 16(3): 240-6. |
| [40] | Zimmermann P, Curtis N. Coronavirus infections in children including COVID-19. Pediatr Infect Dis J 2020; 39(5): 355-68. |









