All published articles of this journal are available on ScienceDirect.
Searching the Blood Lead Level in Children with Attention Deficit Hyperactivity Disorder: A Case-control Study in Tehran, Iran
Abstract
Background:
Attention deficit hyperactivity disorder (ADHD) is a common behavioral problem in children. Identifying the associated risk factors of ADHD is very important for the prognosis and early diagnosis of the disease. Here, we evaluated the association between lead exposure and growth indexes in children with ADHD.
Materials and Methods:
This case-control study was conducted on 30 children with ADHD and 50 healthy subjects. The patient’s age was between 5-12 years. Demographic and clinical information of children were recorded. Blood lead levels were measured in all samples by atomic absorption spectrometry.
Results:
Children with ADHD had significantly higher mean BMI than the control group (16.54 ± 2.8 kg/m2vs. 14.82 ± 1.68 kg/m2; p=0.001). The mean of blood lead in children with ADHD was significantly higher than the normal group (10.58 ± 8.06 μg/dl vs. 7.52 ± 2.26 μg/dl; p=0.01). Multiple logistic analysis revealed one unit increase in BMI was associated with a higher risk of ADHD by 1.5 times (P=0.005; OR = 1.50), while one unit increase in blood lead level increased the risk of ADHD by 1.15 times (P=0.03, OR=1.15).
Conclusion:
Higher BMI and blood lead concentration are risk factors for ADHD among Iranian children.
1. INTRODUCTION
Attention deficit hyperactivity disorder (ADHD) is a prevalent disorder among children. Approximately 3-7% of children in school and 2-4% of adults have ADHD, according to the report provided by the American Psychiatric Association’s Diagnostic and Statistical Manual Fifth Edition 1]. The incidence of ADHD is higher in boys than girls (10% vs. 8%). This disorder can lead to multiple personality disor-ders after puberty, especially antisocial personality disorder.
Recent evidence has revealed that approximately 20% of children with ADHD have antisocial behavior [2, 3]. Although some ADHD symptoms may disappear with time, a person will show symptoms such as a lack of concentration throughout their lifetime. Therefore, the early diagnosis of the disease and finding the associated risk factors involved in ADHD are very important.
Recent evidence has revealed environmental exposure to some toxicants, dangerous chemicals, and heavy metals may be responsible for ADHD occurrence in children [4, 5]. Lead is a systemic toxicant that is widely widespread around our environment. This heavy metal can affect different organs in the human body and cause a broad spectrum of complications, such as hemolytic anemia, bone injury, neurological damage, renal and liver failure, reproductive disorders, cardiovascular disease, and cancers [6, 7]. Some studies indicated that lead exposure may be associated with some serious behavioral problems in children. For example, Wasserman et al. [8], reported that higher exposure to lead increased behavior problems in preschool children. A cohort study on Chinese preschool children demonstrated that blood lead concentrations, even at mean values of 6.4 µg/dl, were associated with a higher risk of behavioral problems such as internalizing and pervasive developmental problems [9]. Sciarillo et al. [10], found that lead exposure is associated with higher Total Behavior Problem Score in children. Besides, some studies proposed that environmental exposure to lead can be associated with obesity or overweight; however, there are conflicting results in this regard among individuals with ADHD. Wang et al. [11], demonstrated that blood lead level was independently associated with BMI in women but not in men. Other studies did not find a significant relationship between lead exposure and BMI in adults [12, 13]. Therefore, this cross-sectional study sought to characterize the association between ADHD in children with relative lead exposure and BMI.
2. METHODS
This case-control study was conducted on 30 children with ADHD and 50 healthy children who were referred to Rasoul Akram Hospital from 2017 to 2019. There were 13 girls and 17 boys in the case group. The age of patients was between 5-12 years with a mean age of 8.1 ± .225.
The control group was randomly selected based on the children who had been referred for growth and developmental milestone assessment with an approximate ratio of two to one. In the control group there were 21 girls and 29 boys with a mean age of 7.6 ± 2.85 years. Based on similar studies and the appropriate formula, the sample size was calculated. ADHD was identified based on DSM-5 criteria by an expert child psychiatrist [14]. All patients in the case group were included in the study before starting the treatment. Healthy children were those with normal growth and without ADHD or other abnormalities in their physical examination or laboratory results. Both groups had similar aged range and socioeconomic levels and had been living in Downtown areas.
The present study was approved by the institutional review board and ethical committee of the Iran University of Medical Sciences. Written informed consent were signed by all parents. Children with a history of previous brain injuries, absence seizures, complicated delivery, maternal toxemia, maternal hyperthyroidism, autistic spectrum disorders, maternal smoking, or alcohol consumption during pregnancy and children with low socio-economic family level (based on the amount of the poverty line) were excluded. All patients with abnormal reports of electroencephalography and epilepsy, complete blood cell count, thyroid test, and serum ferritin or abnormality in blood sugar level or biochemical tests were also excluded. 9 patients were excluded from study based on exclusion criteria. After the selection process, the weight (Kg), height (cm), and BMI (Kg/M2) of all participants were measured. Then, 2 cc of peripheral blood was collected from all children in both groups and used for the measurement of lead by using atomic absorption spectrometry.
2.1. Statistical Analysis
The results of this study were analyzed by SPSS software (IBM, version 19). Quantitative data were analyzed using the descriptive program and presented as Mean ± SD. The comparison of the mean of parametric data between cases and controls was analyzed using an independent student sample-t-test. Multivariate analysis and logistic regression model were applied to consider the relationship between growth indicators and hyperactivity. A p< 0.05 was considered statistically significant.
3. RESULTS
A total of 30 children with ADHD and 50 healthy children entered study aged between 5-12 years old. A comparison of the basic demographic findings between the two groups is summarized in Table 1. There was no significant difference in the mean of age (p=0.54), sex (p=0.65) and weight between the two groups; however, a trend was observed for higher mean weight in the ADHD group (p=0.053). Children with ADHD had significantly higher mean BMI values compared to the control group (16.54 ± 2.8 kg/m2vs. 14.82 ± 1.68 kg/m2; p=0.001). The mean of blood lead in children with ADHD was significantly higher than the normal group (10.58 ± 8.06 μg/dl vs. 7.52 ± 2.26 μg/dl; p=0.01) (Table 1).
| Variable | Case (n=30) | Control (n=50) | p-value |
|---|---|---|---|
| Age Sex Height (cm) |
5-12 (8.1 ± 2.25) Male 17 (0.56%) Female 13 (0.44%) 116.62 ± 11.62 |
5-12 (7.6 ± 2.85) Male 29 (0.58%) Female 21 (0.42%) 114.82 ± 13.95 |
0.54 0.65 0.65 0.58 |
| Weight (kg) | 23.26 ± 7.28 | 20.1 ± 6.19 | 0.053 |
| BMI (kg/m2) | 16.54 ± 2.8 | 14.82 ± 1.68 | 0.001 |
| Lead level (μg/dl) | 10.58 ± 8.06 | 7.52 ± 2.26 | 0.01 |
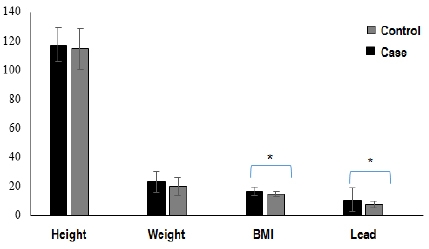
Logistic regression analysis showed a significant correlation between BMI and blood lead levels with a higher risk of ADHD in children Table 2. One unit increase in BMI was associated with a higher chance of ADHD by 1.5 times (P=0.005; OR = 1.50). Furthermore, one unit increase in blood lead concentration enhanced the chance of hyperactivity disorder by 1.15 times (P=0.03, OR=1.15). Therefore, these two variables were considered as risk factors for ADHD. The relationship of Height, Weight, BMI and Lead level in the case and control group was shown in Fig. (1).
| Variable | Odd Ratio | Confidence Interval | p-value |
|---|---|---|---|
| BMI (kg/m2) | 1.50 | 1.12-1.97 | 0.005 |
| Lead level (μg/dl) | 1.15 | 1.01-1.30 | 0.03 |
4. DISCUSSION
In this research, we considered the relationship between blood lead levels and growth indicators
in children with ADHD. Our data revealed that blood lead concentration in children with ADHD was significantly higher than normal group. Logistic regression analysis showed that higher blood lead levels were significantly associated with a higher risk of ADHD occurrence. This data indicates that lead may be a serious risk factor for ADHD occurrence in children. Several studies considered the relationship between blood lead levels and other behavioral and brain activity in children to support this finding. For example, Roy et al. [15], considered the relationship between blood lead levels with behavior and cognition in 756 children. They found a higher mean level of blood lead in these children. Additionally, an increased level of blood lead was significantly associated with higher anxiety, social problems, and higher scores in the ADHD index. This result is inconsistent with the finding of our study that revealed an association between blood lead and the risk of ADHD.
In another study, Palaniappan et al. [16], demonstrated that lead exposure is significantly associated with decreased neurologic function, loss of IQ, and adverse behavior. Similarly, Froehlich et al. [17], investigated the relationship between prenatal tobacco and childhood lead exposures to ADHD in children. Their findings revealed that higher blood lead concentrations were independently associated with ADHD. Compared with children with neither exposure, children with a history of exposure to prenatal tobacco lead had a significantly greater risk of ADHD. In another study, the association between ADHD and blood lead levels was evaluated among Chinese children [18]. The results showed a significant difference in the blood lead levels between ADHD cases and normal children. ADHD cases were more likely to have been exposed to lead during childhood than the non-ADHD group. Another research examined the association of exposure to tobacco smoke and environmental lead with ADHD in US Children [19]. The results showed that prenatal tobacco exposure and higher blood lead concentration were significantly associated with ADHD. These data are in close agreement with the findings of our study and indicate that exposures to prenatal tobacco and environmental lead are risk factors for
ADHD. In another study that was conducted among Iranian children, the results revealed that the
the mean level of serum lead was significantly higher in the ADHD group in comparison to the control group [20]. The authors concluded that higher blood lead levels can be associated with an increased incidence of ADHD [20]. Hong et al. [4], demonstrated that environmental lead exposure is associated with lower IQ and higher risk of ADHD in school-age children. Therefore, these data indicate that higher blood lead level in children is associated with an increased risk of neurobehavioral deficits and ADHD. However, the exact mechanism by which lead exposure enhances the risk of ADHD is not well understood. Nigg et al. [21], concluded that lead exposure is an important contributor to ADHD and lower IQ, which is mediated by less effective cognitive control. Other studies conducted on animal models suggested that lead exposure may be associated with permanent failures in the hypothalamic-pituitary axis, glucocorticoid deregulation, changed γ-aminobutyric acid-containing, and dopaminergic systems, which are correlated to higher anxiety and lower socializing behavior [22]. Therefore, reducing lead exposure may be an important avenue for preventing ADHD among children.
Another main finding of the present study is that patients with higher BMI values had a significantly higher risk of ADHD incidence. Children with ADHD had significantly higher mean BMI compared to normal subjects, indicating BMI can be considered a risk factor for ADHD occurrence in children. In this regard, some studies considered higher BMI values as a risk factor for ADHD incidence among children. For example, Dubnov-Raz et al. [23], reported that children with ADHD had significantly higher weight and BMI compared to a normal subject. More recently, Cortese [24] found a significant link between ADHD and obesity. Martins-Silva et al. [25], showed that a higher BMI value is significantly associated with ADHD in children. In another recent study, Li et al. [26], concluded that pre-pregnancy overweight or obesity was significantly correlated to a higher risk of ADHD in children. According to these results, increased BMI can be indicated as a risk factor for ADHD; therefore, clinicians should consider it from the beginning of diagnosing ADHD. However, the underlying mechanism has remained unclear. It appears that the associations of ADHD with BMI could be attributed to genetic factors shared by the two conditions. Therefore, further studies are necessary to consider this relationship.
CONCLUSION
This case-control study demonstrated that higher BMI and blood lead concentration are risk factors for ADHD among Iranian children. Our findings emphasize the importance of public health policies that reduce environmental lead exposure. Therefore, the reduction of lead exposure and also obesity may be an important avenue for ADHD prevention among children. Future studies may be required to evaluate the underlying mechanisms of the effects of BMI and lead to ADHD occurrence.
AUTHORS' CONTRIBUTION
VM, NS, and SHE designed and managed the study. PM and RA analyzed and interpreted the patient's data and performed follow with the patients, GHS were major contributors in writing the manuscript. All of the authors read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTI-CIPATE
The medical ethics committee of Iran University of Medical Sciences with the ethics ID of IR approved the thesis.IUMS.REC 1396.32102.
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
The consent for the publication of detailed personal data was obtained from parents.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIAL
The datasets used during the current study are available from the corresponding author [S.N] upon reasonable request.
FUNDING
Funding for this study was provided by the Pediatric Growth and Development Research Center of the Institute of Endocrinology and Metabolism of Iran University of Medical Sciences which we are grateful.
CONFLICT OF INTEREST
The authors declare no conflict of interest in preparing this study.
ACKNOWLEDGEMENTS
The authors would like to thank Rasoul Akram Hospital for their technical assistance. This study was supported by a grant received from the Iran University of Medical Sciences, Tehran, Iran.


