RESEARCH ARTICLE
An Exploration of System Factors Influencing Older Adults’ Initial Engagement with Physical Activity Interventions
Andrew Powell1, *, Samuel Nyman1, #
Article Information
Identifiers and Pagination:
Year: 2022Volume: 15
E-location ID: e187494452212191
Publisher ID: e187494452212191
DOI: 10.2174/18749445-v15-e221219-2022-147
Article History:
Received Date: 15/9/2022Revision Received Date: 12/12/2022
Acceptance Date: 15/12/2022
Electronic publication date: 22/12/2022
Collection year: 2022

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Previous work has highlighted the need for researchers to look beyond the behavioural, cognitive, and motivational components of physical activity interventions for older adults, and to investigate the ‘system-related’ factors that may influence physical activity behaviour, which pertain to their social, physical, and operational contexts.
Objective:
This qualitative study aimed to explore the system factors influencing older adults’ initial engagement with physical activity interventions.
Methods:
Semi-structured one-to-one telephone interviews were conducted with 12 individuals aged 55 and over to gather their views on the subject. The study employed a qualitative descriptive approach, and a thematic analysis was carried out.
Results:
Participants identified various system factors they felt could influence older adults’ engagement with physical activity interventions, particularly relating to social support and relationships (e.g. being able to bring a friend to the first session), and the physical, social, and information environments (e.g. venues being reachable by bus or car).
Conclusion:
This study highlights system factors as a potentially important yet largely unexplored concept in the field of physical activity promotion. The findings provide practical information for public health practitioners to use when attempting to design physical activity interventions that older adults will willingly engage with, and the rationale for future research seeking to expand understanding of the influence of system factors on older adults’ initial engagement with physical activity interventions, as well as their subsequent physical activity behaviours beyond this.
1. INTRODUCTION
Vast evidence suggests that regular physical activity (PA) participation brings many protective health and quality of life benefits for ageing populations [1]. For instance, PA participation has been found to result in improvements in cardiorespiratory fitness, neuromuscular strength and function, mobility, and balance in older adults, which in turn are associated with a lower risk of falls and cognitive decline, diseases such as cardiovascular disease, and improved quality of life [2-4]. The latest guidelines published by the World Health Organisation advise that to gain these benefits, 55–64-year-olds should perform at least 300 weekly minutes of moderate-intensity PA, with at least 150 minutes per week recommended for over 65s [5]. However, recent figures based on self-reported levels of leisure, sport, and fitness activity participation have revealed that in the UK currently, only approximately 60% of over 55s are achieving these standards [6]. This is not a new concern, though; increasing the PA levels of older adults is a long-standing public health priority in the UK [7], and there is a need for evidence on the most important factors to consider when designing PA interventions that aim to change older adults’ PA behaviour and sustain this change [8].
The findings of a systematic umbrella review conducted by Zubala et al. [9], which synthesised evidence from 19 previous reviews on the effectiveness of multi-modal and multi-component PA interventions for increasing the PA levels of community-dwelling older adults, pointed towards the importance of three components of interventions for their role in influencing PA: behavioural (e.g. to directly facilitate behaviour), cognitive (e.g. to enhance comprehension of behaviour and awareness), and motivational (e.g. to increase readiness and desire to change behaviour). However, the authors also highlighted in their conclusions the need for researchers to look beyond just these aspects of PA promotion in the future, and to investigate the role of extrapersonal ‘system-related’ factors. System factors are elements of interventions pertaining to their social, physical, and operational contexts, such as the operating procedures, policies, actions and communications of the organisations and professionals involved in their delivery, and the environmental-level characteristics and components [10]. The potential importance of system factors to PA promotion is based on the idea that the person most directly connected to a health behaviour or outcome is not necessarily at the root of its cause and that the latent systemic conditions that it occurred in may have caused or contributed to it [11].
Zubala et al. [9] further noted that system factors may be particularly relevant to facilitating older adults’ ‘initial engagement’ with PA interventions. Initial engagement is the entry-point of intervention participation, often capped by the attendance of an appointment such as an assessment, induction, or taster session, which is usually preceded by some form of registration or sign-up process once an individual has become aware of the intervention. As noted by Pavey et al. [12], initial engagement is an important consideration for PA interventions because, without it, their motivational, cognitive, and behavioural components will logically never be able to exert their intended effects further downstream. Zubala et al. [9] observed that PA interventions for older adults are often developed by public health organisations using a top-down approach lacking end-user involvement, a process that tends to result in an overlooking of the system-related factors that might impact on the acceptability, accessibility, and appropriateness of interventions to potential participants, and therefore their likelihood to initially engage.
No studies to date appear to have directly examined the influence of system-related factors on PA intervention initial engagement in older adults. However, the findings of both a previous umbrella review conducted by Olanrewaju et al. [13] that synthesised the findings of nine qualitative reviews examining the barriers and facilitators of older adults’ PA behaviour, and a subsequent systematic review of 49 qualitative studies on the same topic conducted by Spiteri et al. [14], support the notion of the potential link between system factors and initial engagement and indicate a need for further research on the topic. For instance, system-related elements of PA interventions relating to communication of information on the risks and benefits of participation to potential participants; involvement of healthcare professionals in information provision, signposting, and referral processes; provision of social support to encourage and support participation; cost; timings; and convenience, safety, and accessibility of environments, venues, and facilities were all reported to be important influencers of engagement with PA interventions across both reviews. Furthermore, the findings of a recent qualitative study conducted by the lead researcher (AP), which investigated how a lifestyle behaviour change service in the South-West of England influenced older adults’ PA behaviour, also lend credence to the idea. Across the 12 participants that were interviewed, it was frequently mentioned that system-related intervention elements such as the advertising methods and routes used to create initial awareness of the intervention, the involvement of healthcare professionals in signposting processes, ease of registration procedures, cost, and the personal characteristics and communication styles of the professionals responsible for conducting initial conversations with potential participants all influenced their engagement with the intervention [15].
The aim of this study was to explore the system-related factors influencing older adults’ initial engagement with PA interventions.
2. MATERIALS AND METHODS
2.1. Research Approach
A qualitative study was conducted, involving semi-structured one-to-one telephone interviews. Ethical approval was obtained from Bournemouth University (ref. 41323). The study employed a qualitative descriptive approach. Qualitative descriptive research, “is typically directed toward discovering the who, what, and where of experiences”, as opposed to seeking to, “describe an event in terms of a conceptual, philosophical or other highly abstract framework” [16]. Thus, qualitative descriptive research entails low-inference interpretation, and is said to be, “especially amenable to obtaining straight and largely unadorned answers to questions of special relevance to practitioners and policy makers” [16].
2.2. Participants and Recruitment
The aim was to conduct telephone interviews with a convenience sample of 12 individuals aged 55 and over to gather their views and reflections on the potential influence of system-related factors on older adults’ initial engagement with PA interventions. A sample size of 12 was selected based on resource availability, but also with consideration to the previous recommendation that this should be an adequate number to achieve data saturation in qualitative studies that seek to understand common perceptions, on clearly defined topics, among relatively homogenous sets of individuals [17].
Participants were recruited by an invitation email containing an attached recruitment poster, seeking individuals aged 55 and over to participate in a telephone interview to help the study team learn more about the different factors that might make older adults more or less likely to engage with PA interventions. The email and poster were sent to members of two local community groups based in Dorset, South-West England, with a primary interest in health-related research, via the groups’ administrators. Individuals interested in participating in the study were asked to email the lead researcher (AP), and then in a response email from AP, were asked to provide their telephone number so they could be called to discuss their interest in the study. AP called potential participants to explain the study and answer any queries. If willing to participate, a telephone interview was subsequently arranged for a date and time of their convenience, and a participant agreement form and a participation information sheet were sent to them via email.
2.3. Interview Procedures
AP conducted all telephone interviews. AP answered any queries that participants had about either the participant information sheet or the participant agreement form on the day of the interview, and verbal consent was recorded prior to the interview commencing. A topic guide was utilised for interviews to ensure areas of key interest were covered, while still allowing for the emergence of unprompted content. Table 1 summarises the content of the topic guide. It was informed by the evidence relating to system factors from both the previous reviews on the barriers and facilitators of older adults’ PA behaviour [13, 14] and the previous study conducted by AP [15], as well as the practical experiences of AP. To provide additional context to participants’ views and reflections, questions were also included pertaining to their PA habits and demographic characteristics. All telephone interviews were audio-recorded using a digital audio-recorder and transcribed verbatim. After each interview, AP made reflective notes detailing impressions of the data collected and the effectiveness of data collection techniques [18].
| Topic Area |
|---|
| Demographic information Physical activity habits Modes and methods of creating initial awareness of physical activity interventions Registration processes of physical activity interventions Support required to engage with physical activity interventions Involvement of professionals in physical activity interventions Environmental and logistical elements of physical activity interventions Technology and physical activity interventions. |
2.4. Analysis
A thematic analysis was conducted by AP, using a hybrid approach incorporating both inductive and deductive processes [19]. The interview transcripts were initially read once through to gain familiarity with the data. At that point, a priori subthemes were added to a codebook in Microsoft Word [20], largely derived from the original interview topic guide. To identify emerging posteriori subthemes, the transcripts were then read twice more, this time with seemingly relevant passages of text colour highlighted and notes made describing their noteworthiness. Common patterns and important threads were then searched for in the highlighted interview data, with each passage coded, and then categorised with other similar passages into subthemes and added to the codebook. The list of a priori and posteriori subthemes were then clustered into overarching themes. Themes and subthemes, and the strength and accuracy of the interpretations underpinning them, were then critically discussed and evaluated in a debrief session with the co-author (SN), who vetted all content. To enable summarising, reporting, and interpretation, the indexing and collation of illustrative quotations was subsequently carried out.
3. RESULTS
Twelve telephone interviews were conducted in February 2022. Study recruitment ended when the target of 12 interviews had been completed. Data saturation, defined as the point at which no new posteriori subthemes emerged from the data, was detected after nine analysed transcripts, with the final three transcripts substantiating findings [17, 21]. Interview durations ranged from 31 to 57 minutes (mean 48 (SD 7.5) minutes). Four participants were male and eight were female, with participants aged 56 to 86 years (mean 71 (SD 10.5) years) (Table 2). Ten participants reported currently participating in some form of regular PA, with activities including walking, croquet, swimming, aqua aerobics, sailing, yoga, tai chi, and pilates. The remaining two participants reported physical disabilities that limited their ability to perform regular PA.
| Participant | Sex | Age | Ethnicity | Employment Status |
|---|---|---|---|---|
| Mary | Female | 75 | White | Retired |
| Brian | Male | 81 | White | Retired |
| Diane | Female | 71 | Missing | Retired |
| Amanda | Female | 79 | White | Retired |
| Jean | Female | 86 | Missing | Retired |
| Simon | Male | 64 | White | Retired |
| Grace | Female | 69 | White | Working part time |
| Rosie | Female | 57 | White | Unable to work due to ill health/disability |
| Charlotte | Female | 56 | White | Working full time |
| Colin | Male | 80 | White | Retired |
| Elsie | Female | 78 | Missing | Retired |
| Poppy | Female | 57 | White | Unable to work due to ill health/disability |
3.1. Qualitative Themes
Four themes encapsulated participants’ views on the system-related factors influencing older adults’ initial engagement with PA interventions, with the themes largely corresponding to the different stages of the engagement process: facilitating initial awareness; advertising content; facilitating initial contact; and facilitating initial attendance.
3.2. Facilitating Initial Awareness
Many participants stated that leaflets could be a very effective means of making older adults aware of PA interventions as the first step toward their engagement. Participants suggested it was important to strategically place them in locations where older adults regularly frequent, spend time and linger, such as libraries, surgeries, bus stops, garden centres, churches, community centres, and coffee shops. Nearly all participants alluded to the frequency with which most older adults visit their general practitioner (GP), and suggested that GPs could play a key role in the process of providing leaflets and information to facilitate awareness of PA interventions:
The [GP] could be such a critically important instrument in all of this, you know, there's so much that could be done, because when you think about it, they are such a central part of our lives. When you get older, you are going to your GP regularly. I'm a pretty fit guy, touch wood. But I go to my GP surgery quite regularly. I go there for my medication. I go there for my annual check-ups. I go there for when anything goes wrong. And I think this aspect has been almost ignored in terms of [creating awareness of PA interventions]. So getting in touch with your GP, who should then [have leaflets] particularly for the older people like me, [saying], “this is where you can go and exercise” [Brian].
The potential effectiveness of GPs was felt to be due to the trust and respect that older adults tend to have for health professionals and the advice and information they offer:
I would sit up and take notice if it was a health professional giving me information [about a PA intervention]. I think it would have more clout if you like. Because I like to think that they know what they're talking about, and that if they do recommend anything, it's of value [Poppy].
Third sector societies and clubs, including the University of the Third Age (U3A), churches, arts groups, and carer support groups, were also cited by various participants as potentially effective sources of PA intervention awareness:
Now there are loads of associations [that cater to older adults] everywhere in the country. Now, if you could get to them, to [provide information on] your flyers, your services, whatever it is, to be able to impart that to the people of their community. You are going to have a far higher hit rate. If you can get through to those bodies to get through to people, they may be able to assist you in getting to the target that you want to get to. If this comes through an association that you are already involved with and trust, you're more likely to give it a look aren't you? [Grace].
Regarding social media, though nearly all participants felt it could be an effective medium through which to facilitate awareness of PA interventions, and reported that Facebook was the platform most used by older adults, they were also unanimous in their view that social media could not be relied upon to any great degree due to its varied use and acceptance among older adults:
I think for some people, [social media] is wonderful because they understand it. I mean, I know older people who are far better than I am. I know, equally, some people that they wouldn't dream of sitting in front of a computer. [Social media], I could certainly think… 60% of people would find it very useful, but then you're not going to conquer all of them, certainly not. But a percentage of people would really like it [Mary].
3.3. Advertising Content
When talking about the content that should be included in PA intervention advertising such as leaflets and social media advertisements, numerous participants felt it was important to first acknowledge their belief that the primary reason most older adults would consider engaging with a PA intervention is to gain access to social opportunities. Therefore, they felt that at the heart of advertising to make older adults aware of PA interventions should be an emphasis on the social benefits potentially offered:
That is the most important [motivation to engage with a PA intervention], that they meet people. There are an awful lot of older people who would love to have the opportunity to meet people, have a talk, and do some exercise afterwards. The social element I think for older people is absolutely imperative, that is your number one thing before any activity or anything. The most important criteria [to emphasise in advertising therefore] is you can go out and meet someone. I think if you say to somebody now, an elderly person, “right, we're going to do a bit of exercise and then we'll meet for coffee”, whereas if you said, “we're going to have a coffee and socialise and we will do a little bit of exercise”. I think that the second [message] will be more successful. I'm not sure if you said to an older person, “you need to exercise, you need to walk”, I don't think they prioritise it like that. The exercise must be point number two or three, not number one [Mary].
A number of participants also stated that older adults would consider engaging in a PA intervention to gain physical health benefits. Therefore, they felt that PA intervention advertising should also make explicit the specific health benefits on offer that are most important to older adults, such as improved balance, lowered blood pressure and cholesterol, weight loss, and medication reduction. Numerous participants also noted that older adults are often concerned about the safety and potential risks posed by exercise due to their physical limitations or health issues. Thus, they felt that advertising should contain further information explaining who activities are suitable for and reassuring them that activities will be safe and practical, appropriate in intensity, and with the flexibility to be tailored to any special needs, preferences, or restrictions:
I love ballet. So I got their leaflet and it says they've got a ballet bar for over 50s or something and it says very, very gentle exercise, and I wanted to go there. I haven't been, but I love the way they advertised it. Gentle exercise. I think that's very important. I think I felt that I wouldn't be pushed too hard, and that they would understand if I had limitations. I suppose [advertising] could say something like at your own pace or, if it's a class, then it's kind of, everybody does what they can. I think maybe just language, like at your own pace, or support if needed, is available [Poppy].
3.4. Facilitating Initial Contact
Nearly all participants commented that a straightforward process should be provided to encourage and make it easy for older adults to make their first contact with PA interventions:
It's got to be easy. If there's a link, it has to work. If there's a phone number, somebody needs to respond. People don't want to put a lot of effort in. So, if you're going to offer things to people, it's got to be fairly easy to pick it up. And the GPs or whoever, they can say, look, this is a number, here's a piece of paper, give this person a ring. Make it easy [Grace].
Telephone was cited by the majority of participants as the most preferred and acceptable method due to its usability. Furthermore, it was frequently noted that older adults would highly value an invitation to call and speak on the telephone because it would provide them with the chance to find out more information about the PA intervention, ascertain their suitability, ask questions and gain reassurance about any physical limitations or health issues they may have, and make a personal connection, all of which would potentially provide them with the confidence to move forward further:
I think [the value of a telephone call would be] just to explain my situation and to say something like, well, this looks good. I think it might be possible. What do you think, do you think that given my situation, do you think it is something I would be able to do? I think if there's been that human interaction, then you feel like you've communicated with a proper human being and you've kind of made some sort of connection before you've turned up at the activity. I think my generation, we're just so used to meeting people, talking to people, seeing people [Poppy].
3.5. Facilitating Initial Attendance
It was suggested by a number of participants that an invitation to attend a taster session following the phone call could be welcomed by older adults, by providing a non-threatening and low-commitment way of experiencing the activity and ascertaining its suitability and potential benefits. However, participants frequently pointed out that mobility restrictions, social anxiety, and fear of uncertainty could all serve as a barrier to attendance for many older adults:
I can understand that people who think, oh, that would be nice, [but] no, I can't do that. I wouldn't know anybody. I'm going to feel stupid. What if there's nobody there? You know what it's like, all the negative thoughts. Well, if you've never done [the activity], that would be quite scary and you'd think, oh, I can't do that. I can barely walk to the shops and back. Well actually, you're absolutely right for that [activity], but you might not think it. I think sometimes people need their hand held to get started [Grace].
The ability for an individual to attend their first session with a friend, and the offer of a ‘buddy’, someone already attending the PA intervention, to accompany them, were both suggested as potential social support-based solutions that could overcome these barriers and facilitate attendance:
[Some people] very often have to take somebody along to that first session. That is such a huge step and they will very often carry on without you after that. I took my friend [to aqua aerobics] the other day and she said, oh God, just the thought of having a communal shower sends horrors down my spine. And when I said to her, you do not have to do that, not everybody has a shower, they go home, you don't have to do it - people don't believe you. So, that myth was dispersed [Charlotte].
All participants stated that cost was a very important consideration that could influence the attendance of older adults and stressed that PA interventions had to be affordable for those on a tight monthly budget, and also provide value for money:
If it’s [going to cost] too much money, they're not going to do it are they. I’ve said that the most important thing is to meet people, fine, that’s good, but then, money. You often hear about the grey pound, for instance, the fact that people are now on retirement incomes and those that have been fortunate to be in final salary schemes are on an income with less outgoings, so they're far better off than they ever were. But having said that, most elderly people have come from the post-war years. So they're used to things like rationing. So although they may have more money in their pockets, they're less inclined to want to spend it and are looking for bargains and watching the pennies [Brian].
In addition to making PA interventions low cost, also suggested ways to help overcome any potential financial concerns were offering the first session free and providing low-commitment payment options such as ‘pay-on-the-day’. Numerous participants also stated that certain venue characteristics could influence older adults’ initial decision to attend a PA intervention. Being local, convenient and easy to access; being on a bus route and having car parking available; offering disability access; and providing facilities such as toilets and a coffee shop were all mentioned. Finally, nearly all participants stressed that the time of day that sessions took place could influence attendance. It was frequently mentioned that early mornings could be off-putting for older adults due to the time needed to wake up, as well as evenings due to tiredness and safety concerns about being out after dark. Mid-morning and early afternoon appeared to be the preferable session times to facilitate attendance.
4. DISCUSSION
Through conducting telephone interviews with 12 individuals aged 55 and over, the potential influence of a range of system-related factors on older adults’ initial engagement with PA interventions has been highlighted. With a need for evidence on the most important factors to consider when designing PA interventions that aim to change older adults’ PA behaviour and sustain this change [8], this information is of high relevance.
4.1. Principal Findings
Participants alluded to a wide array of system-related factors that they felt could influence older adults’ engagement with PA interventions. These included the modes, methods, and routes used to create awareness of interventions; the messages and content of marketing materials such as leaflets; environmental and logistic elements of interventions such as costs, timings, and venue characteristics; and availability of social support. Zubala et al. [9] previously asserted that researchers should look beyond the cognitive, motivational, and behavioural-focused components of PA promotion to also investigate the extrapersonal, system-related elements that might influence older adults’ initial engagement with PA interventions. Previous qualitative reviews and research indirectly supported this notion, suggesting that system-related elements largely mirroring those mentioned by participants in the present study could all act as barriers and facilitators of older adults’ PA behaviour [13-15]. The present study now provides primary research evidence directly supporting the novel idea that system factors are a potentially important influence on older adults’ initial engagement with PA interventions, and the findings lend credence to the basic concept underlying this idea; that the person most directly connected to a health-related behaviour such as PA intervention engagement should not be assumed to be the sole root of its enactment, and that latent systemic conditions may also contribute [11].
Many of the system factors mentioned by participants related to tailoring certain elements of PA interventions around older adults’ existing social and domestic environments. For instance, participants stated that strategies such as advertising in locations regularly visited by older adults, and via health professionals and societies that they are already members of; offering an easy and acceptable mode of making initial contact such as the telephone; and being located at local venues conveniently reachable by bus or car, could all positively influence older adults’ initial engagement with PA interventions. These system factors relate to the approach of choice architecture theory, or ‘nudge’, for behaviour change [22]; adaptions to the physical, social, and/or information environment can prompt individuals to adopt health-promoting behaviours. Underpinning this theory is the principle that people often make health-related decisions based on context-dependent automatic thought processes rather than deliberate cognitive processes, and thus tailoring interventions to suit the micro-environments in which individuals make these decisions can trigger desirable behavioural responses [23, 24]. A recent systematic review of 88 studies that examined the effectiveness of choice architecture-centered techniques for encouraging PA in adults [24], and an earlier scoping review that sought to provide an overview of interventions using choice architecture techniques to promote PA in the general population [23], both inferred that a lack of studies exist to draw firm conclusions from and that research in the area is still in its infancy. However, the findings of the present study provide support for this idea that system-related elements pertaining to the physical, social, and information environments could influence older adults’ PA behaviours, namely those relating to initial intervention engagement.
Participants also talked about the importance of several system factors related to social support and social relationships. These included the potential social benefits of interventions being conveyed through advertising messages; individuals having the opportunity to speak on the phone with a professional involved in the intervention prior to attending to create a social connection; and being able to bring a friend, or be accompanied by a ‘buddy’, to the first session to ease uncertainty and anxiety. The importance participants attached to these system factors again supports existing theory and evidence in the area of PA promotion. According to the socioemotional selectivity theory [25], social support and social relationships are significant behavioural motivators for older adults, because they play a vital role in two of their key priorities in life: the regulating of emotions and the optimising of emotional experiences. Thus, it is thought social elements have the potential to influence older adults’ initiation and maintenance of PA and should be at the forefront of thinking when designing PA interventions [26, 27]. A previous review by Lindsay Smith et al. [28] supports this assertion. Through synthesising 27 quantitative studies that had examined the association between social support and PA in older adults, it was found that emotional support from other people links to intrinsic motivation to engage in PA, and subsequent PA participation. The present study further supports these findings, suggesting that socially themed system factors could be an important influencer of older adults’ initial engagement with PA interventions.
4.2. Applications
Increasing the PA levels of older adults is a long-standing UK public health priority [7], with a need existing for evidence on the most important elements to consider when designing PA interventions [8]. The findings of the present study highlight that system-related factors, particularly those relating to social support and social relationships, and the physical, social, and information environments, could play an important role in influencing older adults’ initial engagement with PA interventions. The present study is the first known to directly examine the influence of system-related factors on PA behaviour in older adults. In doing so, it highlights them as a potentially important, yet largely unexplored concept in the field of PA promotion. Furthermore, through critically looking beyond the traditionally behavioural, cognitive, and motivational-focused components of PA interventions for older adults, and bringing together various disparate pieces of existing knowledge, the present study lends evidence to a novel system-based perspective that can potentially aid their future conceptualisation, design and development. A person-focused philosophy arguably predominates the PA intervention field at present. This views people as agents free to choose between desirable and undesirable behaviours, and that undesirable behaviours relating to things such as initial intervention engagement are largely isolated from context and result from aberrant mental processes such as inattention, lack of knowledge, forgetfulness, lack of motivation, and negligence [29]. Conversely, a system-focused perspective puts forward the idea that behaviours such as intervention engagement are influenced by the latent systemic conditions in which they occur, and don’t just solely arise out of people’s personal psychological, emotional, and behavioural characteristics. Behaviours are thus seen as consequential and non-random, highlighted by the fact that they tend to fall into patterns, rather than being mere reflections of defects in the human condition [11, 29].
The information provided by the present study can now be incorporated into the thinking of ‘real-world’ public health practitioners when attempting to develop PA interventions that older adults will willingly engage with. Fig. (1) depicts the different system factors alluded to by participants in the present study that can be readily applied by practitioners to the design of PA interventions. In addition, the present study also provides a rationale for future, more systematic, research to further elucidate the role of system factors in influencing older adults’ PA behaviour. In another health-related field, Duah-Owusu White et al. [10] recently proposed that a system-based model could be applied to the design of acute hospital settings to reduce adverse outcomes in dementia patients, incorporating the following elements: environment (e.g. the functionality of the physical and operational environment), equipment (e.g. the use of equipment and technology, and the functions served), organisational policies (e.g. the impact of organisational processes and protocols that arise from established policies), and human aspects (e.g. the communications and relationships between people). This model could readily be applied to future qualitative PA intervention research, perhaps being used as a coding framework, to help further identify the system-factors most important in facilitating older adults’ initial engagement, as well as their subsequent behaviours beyond this.
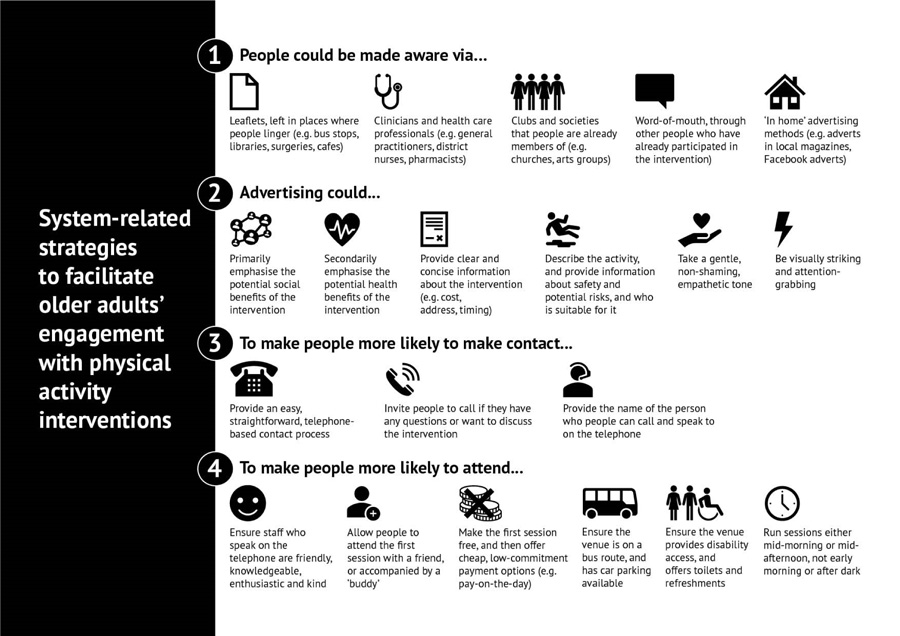 |
Fig. (1). System-related strategies to facilitate older adults’ initial engagement with physical activity interventions. |
4.3. Limitations
Participants all reported engaging in regular PA, perhaps suggesting that their choice to participate in the study, and their resultant views and reflections on the factors influencing initial engagement with PA interventions, reflected their pre-existing positivity, and predisposition, towards PA. In addition, the sample consisted predominantly of retired individuals of White British ethnicity, hailing from a rural geographic region, with eight of the 12 participants aged 69 or above. Furthermore, only information pertaining to participants’ age, sex, ethnicity, and employment status was formally recorded. These points arguably limit the generalisability of the findings to other older adults. Therefore, future research on the potential influence of system factors on initial PA intervention engagement could seek to gain insights into equally represented sub-groups of older adults (e.g. 55-64 years, 65+ years) with different characteristics and backgrounds and formally record information such as specific health conditions, and current PA levels and socioeconomic status using validated measurement tools, to characterize the sample.
CONCLUSION
This qualitative study has highlighted that a range of system-related factors could potentially influence older adults’ initial engagement with PA interventions. The factors identified particularly relate to focusing on aspects of social support and social relationships, and adapting the physical, social, and information environments, to influence behaviour. This study lends evidence to a novel system-based perspective of PA promotion. The findings provide practical information for public health practitioners on the system factors they may need to consider when attempting to design and develop PA interventions that older adults will willingly engage with and provide the rationale for future research that seeks to expand our understanding of the role of system factors in influencing the initial engagement of older adults with PA interventions.
LIST OF ABBREVIATIONS
| PA | = Physical Activity |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by Bournemouth University (ref. 41323).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
Verbal consent was recorded prior to the interview commencing.
STANDARDS OF REPORTING
COREQ guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated and analysed during the study are not publicly available on the grounds of the potential commercial sensibility to the data due to the naming of organisations and services.
FUNDING
No funding was received for the study. The authors conducted it in the course of their employment at Bournemouth University.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
REFERENCES
| [1] | Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol 2012; 2(2): 1143-211. |
| [2] | Cunningham C, O’ Sullivan R, Caserotti P, Tully MA. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand J Med Sci Sports 2020; 30(5): 816-27. |
| [3] | Paterson DH, Jones GR, Rice CL. Ageing and physical activity: Evidence to develop exercise recommendations for older adults. Can J Public health 2007; 98(Suppl 2): S69-108. |
| [4] | Taylor AH, Cable NT, Faulkner G, Hillsdon M, Narici M, Van Der Bij AK. Physical activity and older adults: A review of health benefits and the effectiveness of interventions. J Sports Sci 2004; 22(8): 703-25. |
| [5] | World Health Organization. WHO guidelines on physical activity and sedentary behaviour. 2020. Available from: https://www.who.int/publications/i/item/9789240015128 (Accessed on: 3rd Aug 2022). |
| [6] | Sport England. Active Lives adult survey November 2019/20 report. 2021. Available from: https://www.sportengland.org/know-your-audience/data/active-lives (Accessed on: 3rd Aug 2022). |
| [7] | Public Health England. Everybody active, every day. 2014. Available from: https://www.gov.uk/government/publications/everybody-active-every-day-a-framework-to-embed-physical-activity-into-daily-life (Accessed on: 3rd Aug 2022). |
| [8] | Sport England. Active Ageing Prospectus. 2016. Available from: https://sportengland-production-files.s3.eu-west-2.amazonaws.com/s3fs-public/active-ageing-prospectus.pdf (Accessed on: 3rd Aug 2022). |
| [9] | Zubala A, MacGillivray S, Frost H, et al. Promotion of physical activity interventions for community dwelling older adults: A systematic review of reviews. PLoS One 2017; 12(7): e0180902. |
| [10] | Duah-Owusu White M, Vassallo M, Kelly F, Nyman S. Can a systems approach reduce adverse outcomes in patients with dementia in acute settings? (innovative practice). Dementia 2020; 19(4): 1280-6. |
| [11] | Zecevic AA, Salmoni AW, Lewko JH, Vandervoort AA. Seniors Falls Investigative Methodology (SFIM): A systems approach to the study of falls in seniors. Can J Aging 2007; 26(3): 281-90. |
| [12] | Pavey T, Taylor A, Hillsdon M, et al. Levels and predictors of exercise referral scheme uptake and adherence: A systematic review. J Epidemiol Community Health 2012; 66(8): 737-44. |
| [13] | Olanrewaju O, Kelly S, Cowan A, Brayne C, Lafortune L. Physical activity in community dwelling older people: A systematic review of reviews of interventions and context. PLoS One 2016; 11(12): e0168614. |
| [14] | Spiteri K, Broom D, Hassan Bekhet A, Xerri de Caro J, Laventure B, Grafton K. Barriers and motivators of physical activity participation in middle-aged and older adults - A systematic review. J Aging Phys Act 2019; 27(6): 929-44. |
| [15] | Powell AJ, Thomas S. How the LiveWell Dorset lifestyle behaviour change service influences older adults’ physical activity behaviour: A generic qualitative study. Public Health in Practice 2021; 2: 100164. |
| [16] | Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000; 23(4): 334-40. |
| [17] | Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006; 18(1): 59-82. |
| [18] | Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf 2004; 22(2): 63-75. |
| [19] | Swain J. A hybrid approach to thematic analysis in qualitative research: Using a practical example. Sage Publications Limited 2018. |
| [20] | Mihas P. Learn to build a codebook for a generic qualitative study. Sage Publications Limited 2019. |
| [21] | Braun V, Clarke V. To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qual Res Sport Exerc Health 2021; 13(2): 201-16. |
| [22] | Thaler R, Sunstein C. The politics of libertarian paternalism. New Haven 2008. |
| [23] | Forberger S, Reisch L, Kampfmann T, Zeeb H. Nudging to move: A scoping review of the use of choice architecture interventions to promote physical activity in the general population. Int J Behav Nutr Phys Act 2019; 16(1): 77. |
| [24] | Landais LL, Damman OC, Schoonmade LJ, Timmermans DRM, Verhagen EALM, Jelsma JGM. Choice architecture interventions to change physical activity and sedentary behavior: A systematic review of effects on intention, behavior and health outcomes during and after intervention. Int J Behav Nutr Phys Act 2020; 17(1): 47. |
| [25] | Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: A theory of socioemotional selectivity. Am Psychol 1999; 54(3): 165-81. |
| [26] | English T, Carstensen LL. Selective narrowing of social networks across adulthood is associated with improved emotional experience in daily life. Int J Behav Dev 2014; 38(2): 195-202. |
| [27] | Whaley DE. Social Relationships and Promoting Physical Activity Among Older People. In: Nyman SR, Barker A, Haines T, Eds. The Palgrave Handbook of Ageing and Physical Activity Promotion. Palgrave Macmillan 2018; pp. 317-35. |
| [28] | Smith G, Banting L, Eime R, O’Sullivan G, Van Uffelen JG. The association between social support and physical activity in older adults: A systematic review. Int J Behav Nutr Phys Act 2017; 14(1): 1. |
| [29] | Reason J. Human error: Models and management. BMJ 2000; 320(7237): 768-70. |









