All published articles of this journal are available on ScienceDirect.
Common Risky Sexual Behaviours Among Men Who Have Sex with Men using A Modified Delphi Technique
Abstract
Background:
The objective of this study is to obtain consensus for identifying sexual risk behaviors that are relevant among men who have sex with men (MSM), specifically in the context of Tshwane North, South Africa, in order to guide the development of a risk reduction intervention.
Methods:
The Delphi technique was employed to establish the top ten behaviours that are described as high risk by experts in sexual practices. The setting was a specialised clinic rendering health services to the lesbian, gay, bisexual and transgender (LGBT) communities. A sample of n=14 MSM participated in the panel interview and they were divided into three groups. The panel rated risky sexual behaviour according to a 10-point scale, with 1–3 signifying low-risk sexual behaviours, 4–6 signifying medium risk and 7–10 signifying high-risk sexual behaviours.
Results:
The mean age was 26.8 years old, with a standard deviation of 4. The initial list prioritised the 10 high-risk sexual behaviours as both receptive and insertive anal sex, having multiple partners, sex with a partner of unknown HIV status, sex with an HIV-positive partner without a condom, group sex, both receptive and insertive oral sex, sex without a condom, sex under the influence of alcohol, performing and receiving rimming, and sharing sex toys.
Conclusion:
The final list ranked the top ten risky sexual behaviours for MSM. It could be of use when counselling MSM during their healthcare visits about risk reduction to mitigate HIV acquisition.
1. INTRODUCTION
In South Africa, men who have sex with men (MSM) engage in sexual behaviours which elevate their risk of acquiring HIV and other sexually transmitted infections [1]. Men who engage in receptive anal intercourse are more likely to acquire HIV/STI than men who engage in only insertive anal intercourse [2]. Sexual positioning practices (i.e. receptive, insertive or both) are known to influence the likelihood of HIV transmission. Behavioural risk factors include condomless penile–anal intercourse, having multiple sex partners, and substance use in the context of sexual encounters [3].
Globally, HIV disproportionally affects men who have sex with men [4, 5]. Sub-Saharan Africa faces approximately one million new HIV infections every year [6]. Additionally, HIV incidence estimates among MSM in sub-Saharan Africa are 10 to 15 times higher than in the general population in the same region [7]. The risk of acquiring HIV is elevated by engaging in risky sexual behaviour, which could lead to death or compromise the quality of life. Interventions to reduce risks and mitigate the potential for HIV acquisition include motivational interviewing, among other strategies. However, to provide motivational interviewing, a counsellor needs to be trained in the practice and must learn ways to engage with the client. The training of counsellors and their success in using motivational interviewing is in part, a function of the comfort level of the counsellors with the particular subject matter. In order to provide counsellors with skills that would be appropriate for engaging with MSM, it is important for them to know the most common risky sexual behaviours that could be topics of discussion in a session with members of the MSM community.
The prevalence of different risk behaviours has been identified, but limited information is available about the extent to which that prevalence is applicable to local communities in sub-Saharan Africa because they are often done either in high-income countries or at the national level. Since the prevalence in local communities is still unknown, the aim of this study is to determine the most commonly practised risky sexual behaviours among MSM in the Tshwane community. When considering conducting a survey in the local MSM community, it was noted that the researcher might not have an opportunity to engage with enough appropriate community members to achieve a representative sample of the population. Additionally, participants might provide their opinions without thinking through the specific behaviours, or may not be fully honest if they do not know and trust the researcher. Therefore, with these potential limitations in mind, the researcher opted to use the Delphi technique, which engages MSM experts to identify the priority risky behaviours among MSM. The Delphi technique has been designed to obtain the consensus of opinion among a group of experts.
This study started with a literature review, the purpose of which was to draft a list of risky sexual behaviours that would be presented to the MSM experts. The objective of this study is to obtain consensus for identifying sexual risk behaviors that are relevant among men who have sex with men (MSM) specifically in the context of Tshwane North, South Africa, in order to guide the development of a risk reduction intervention.
2. METHODS
2.1. Study Design
A modified Delphi technique was employed to prioritise a listing of risky sexual behaviours among MSM and to solicit “group judgments” on the topic. Group judgments are said to be more reliable than individuals’ opinions when seeking to develop appropriate interventions for public health [8]. The technique used was to solicit input from a group of experts in a structured manner. The purpose of employing the technique was not only to solicit such input but also to establish the areas where the experts had consensus in their views. This consensus would be an important source of information to support decision-making about issues such as priority needs and goals.
2.2. Study Setting, Population, and Sample
The modified Delphi technique was employed to validate if the top ten most frequently reported sexual practices among MSM are aligned with the sexual practices of MSM in Tshwane North. The Non-Government Organisation (NGO) provides direct health services to the lesbian, gay, bisexual and transgender (LGBT) community in Tshwane North, to MSM, to sex workers, and to subjects who inject drugs. It also provides HIV testing, counselling, treatment and general lifestyle advice and support. The organisation has been in existence for more than 21 years and is dedicated to the building of healthy and empowered LGBT communities in South Africa and internationally, while reducing heterosexist homophobia in society. The organisation was selected for this study based on its experience in working closely with the MSM and the wider LGBT community in Tshwane North and the surrounding areas. The performance of the study was ethically cleared by Sefako Makgatho Health Science University Research Ethics Committee (SMUREC reference number: SMUREC/H/168/2019: PG).
2.3. Procedures of the Delphi Technique
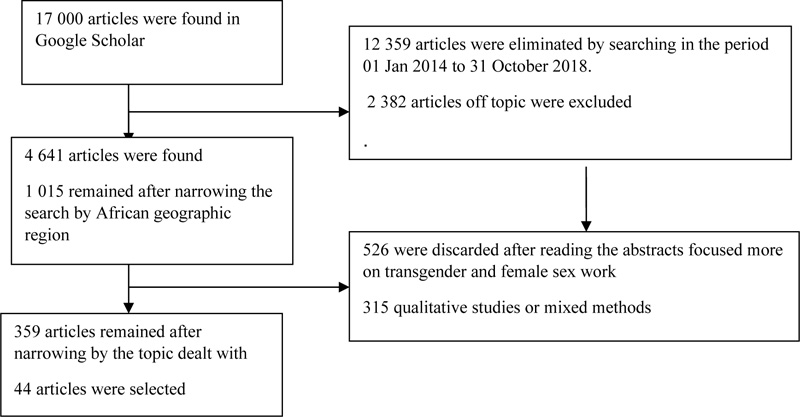
Based on a critical literature review about the risky sexual behaviours of MSM, the researchers drafted an initial list of risk behaviours. Studies were selected for review by using the Google Scholar search engine. Google Scholar is one of the most popular academic search engines used for scientific inquiries into academic works, and it has a high level of quality and reliability in terms of scope and content [9]. The keywords that were used for the search were “risky sexual behaviours” and “men who have sex with men or MSM” (N = 17 300 articles). The search was then narrowed to the period beginning 01 January 2014 and ending 31 October 2018 (N = 4 641 articles). We further narrowed the search according to geographic region - Africa (N = 1 015 articles). We then focused the search on sub-Saharan Africa, South Africa, and peri-urban and rural areas, so that 526 articles were eliminated. After the search had been further narrowed to risk-taking behaviours, sexual partners, unsafe sex, HIV-infection risk, HIV-infection transmission, men who have sex with men, and sexually transmitted diseases, there were 359 articles. The search was then narrowed to publications focusing on sexually transmitted infections: 2 382 articles were of the topic as they did not address risky behaviours practiced by MSM, and 315 were qualitative studies or relied on mixed methods. The remaining 44 articles dealt with MSM’s risky sexual behaviours. The review of the literature finally produced a list of 15 risky sexual behaviours for the initial priority list (Fig. 1).
2.4. Selection of MSM Experts
Selecting expert individuals who met the qualifications for panel membership was critical. They did not require any qualification other than self-identification as an MSM. It was their lived experiences and ability to represent the target population that would ultimately benefit from the intervention that made them valued experts. We used ranking response options to ensure that the panellists were clear about the consequences of their discussion, to make the interpretation clear, and to ensure that the results were actionable in terms of establishing a final priority list. The experts were given the option of providing comments to support their decisions or to suggest changes to the list. We also asked the panellists to give their opinions on the overall structure and completeness of the list.
2.4.1. Delphi Step 2
The NGO was contacted telephonically to arrange a meeting with the NGO’s programme director, managers and coordinators to discuss the proposal for the study. It was agreed during the meeting that the programme coordinator would invite MSM experts to meet the researcher so that the researcher could present the proposed study to them. Those who were interested in participating in the study signed the attendance register and informed consent. The NGO had invited twenty MSM experts, and fourteen volunteered to participate. During the meeting, the researcher presented the proposal to the experts, who were then divided into three discussion groups. They were given the initial list of 15 risky sexual behaviours. This list was developed from the literature review. All individuals were allowed to study the list for 5 minutes before discussing it in their groups. The groups were given 15 minutes to discuss and rank the list. One person per group was assigned to give feedback on behalf of the whole group. Each of these rapporteurs was given 5 minutes to present his/her report. Arising from this discussion, three items were added that had been missing from the initial list. The updated list was reviewed with the experts to ensure consensus before the list was finalised. The experts were then instructed to rank the items in the list using the 1-10 scale developed for this study.
2.4.2. Delphi Step 3
The items on the list were ranked. The experts were required to rank each item on a 10-point scale, 1–3 being low-risk sexual behaviour, 4–6 being medium risk, and 7–10 being high-risk sexual behaviour. After each group had ranked the items, they then gave feedback on their discussions, and the items were ranked in accordance with their opinions. The experts were then asked to review the feedback discussion's outcome and either agree with the outcome or recommend changes while giving their reasons for recommending changes.
2.4.3. Delphi Step 4
The feedback from the experts was discussed amongst the experts to enable them to reach consensus. The researcher asked questions and recorded, consolidated and transmitted the panel responses for each iteration until consensus was achieved. After intense discussion, the items were ranked accordingly and the final top 10 priority list was developed.
2.5. Data Capture and Analysis
Descriptive statistics were used to describe the participants’ demographic characteristics. The data were captured on an Excel spreadsheet and analysed. The data analysis developing the initial list was done manually by a panel of MSM experts during a face-to-face seminar.
3. RESULTS
3.1. Demographic Characteristics of the Experts
The demographic profile of the participants indicates that 10 of the 14 had completed high school, 3 had completed tertiary education, and only 1 had not completed high school. Three were in a steady relationship, 5 were in a casual relationship, and 6 reported being single at the data collection time. Out of 14, 10 reported practicing receptive anal sex and only 1 reported practising rimming, both top and bottom. The other characteristics of the participants are displayed in Table 1.
| Variable | N (%) |
| Mean Age = 26.8 years old; SD: 4 | |
| Highest level of education: | |
| Missing information | 1 (7.1) |
| High school completed | 10 (71.4) |
| Tertiary education completed | 3 (21.4) |
| Occupation: | |
| Not employed | 2 (14.3) |
| Employed | 8 (57.1) |
| Enrolled in a university | 4 (28.6) |
| Type of relationship: | |
| Stable relationship | 3 (21.4) |
| Casual | 5 (35.7) |
| Single | 6 (42.9) |
| Self-reported sexual orientation: | |
| Gay | 7 (58.3) |
| Bisexual | 2 (16.7) |
| Straight (practise anal sex occasionally) | 3 (25.0) |
| Sexual orientation disclosure: | |
| Yes | 9 (69.2) |
| No | 4 (30.8) |
| Who did you disclose your sexual orientation to: | |
| Friends | 4 (33.3) |
| Parents | 2 (16.7) |
| Relatives | 2 (16.7) |
| N/A | 4 (33.3) |
| Have you had sex with: | |
| Male | 3 (21.4) |
| Female | 1 (7.1) |
| Both male and female | 10 (71.4) |
| Insertive anal sex: | |
| Yes | 5 (35.7) |
| No | 9 (64.3) |
| Receptive anal sex: | |
| Yes | 10 (71.4) |
| No | 4 (28.6) |
| Both receptive and insertive anal sex: | |
| Yes | 4 (28.6) |
| No | 10 (71.4) |
| Oral insertive sex: | |
| Yes | 8 (57.1) |
| No | 6 (42.9) |
| Oral receptive sex: | |
| Yes | 4 (28.6) |
| No | 10 (71.4) |
| Both receptive and insertive oral sex: | |
| Yes | 3 (21.4) |
| No | 11 (78.6) |
| Rimming top (performed): | |
| Yes | 1 (7.1) |
| No | 13 (92.9) |
| Rimming bottom (received): | |
| Yes | 1 (7.1) |
| No | 13 (92.9) |
| Both performed and received rimming: | |
| Yes | 1 (7.1) |
| No | 13 (92.9) |
| Vaginal penetration: | |
| Yes | 8 (57.1) |
| No | 6 (42.9) |
| S.No. | - |
| 1 | Insertive anal sex – he put his penis into your anus |
| 2 | Receptive anal sex– you put your penis into his anus |
| 3 | Both receptive and insertive anal sex |
| 4 | Performed oral sex –you sucked his penis |
| 5 | Received oral sex–he sucked your penis |
| 6 | Both performed and received oral sex |
| 7 | Performed rimming (top) – you licked his anus |
| 8 | Received rimming (bottom) – he licked your anus |
| 9 | Both performed and received rimming |
| 10 | Vaginal penetration – you put your penis in her vagina |
| 11 | Had sex with multiple partners |
| 12 | Had penetrative sex without a condom |
| 13 | Had sex with a partner of unknown HIV status |
| 14 | Had sex with an HIV-positive partner without a condom |
| 15 | Had sex under the influence of alcohol or drugs |
3.2. The Initial Priority List from the Literature Review
Fifteen items were selected from the literature to include in the priority list, as they appeared to be common risk behaviours Table 2. Experts were given the initial list to discuss. The list guided the researcher on what to expect when discussing risk behaviours among MSM.
3.3. Expert Consensus List
The panel reached consensus, agreeing to keep fifteen and add four indicators to the list. The four indicators that were added to the list were group sex, licking the vagina, and sharing sex toys. The items in the list were categorised Table 3 from the lowest risk to medium risk and to high-risk behaviour. According to the experts, rimming appeared to be the least risky behaviour practised. Both receptive and insertive anal sex, vaginal penetration, and having multiple partners were the top five high-risk behaviours. Both receptive and insertive oral sex were a medium risk.
| Indicators | Consensus to Include or Exclude or add Indicators | Agreement (n) | Categorised as Inappropriate (low-risk) or Equivocal or Appropriate (high-risk) | Final Decision | Agreement (n) |
|---|---|---|---|---|---|
| Insertive anal sex – he put his penis into your anus | Included | 100% | High risk | Included | 100% |
| Receptive anal sex– you put your penis into his anus | Included | 100% | High risk | Included | 100% |
| Both receptive and insertive anal sex | Included | 100% | High risk | Included | 100% |
| Performed Oral sex – he sucked your penis | Included | 82% | Medium risk | Included | 75% |
| Having sex with multiple partners | Included | 100% | High risk | Included | 100% |
| Received oral sex– you sucked his penis | Included | 82% | Medium risk | Included | 85% |
| Both received and performed oral sex | Included | 82% | Medium risk | Included | 85% |
| Performed rimming – you licked his anus | Included | 65% | Low risk | Included | 71% |
| Received rimming – he licked your anus | Included | 65% | Low risk | Included | 71% |
| Both performed and received rimming | Included | 85% | Medium risk | Included | 93% |
| Vaginal penetration – you put your penis in a women’s vagina | Included | 100% | High risk | Included | 100% |
| Having sex without a condom | Included | 100% | High risk | Included | 100% |
| Having sex with a partner of unknown HIV status | Included | 100% | High risk | Included | 100% |
| Having sex with an HIV-positive partner without a condom | Included | 100% | High risk | Included | 100% |
| Having sex under the influence of alcohol or drugs | Included | 100% | High risk | Included | 100% |
| Group sex | Additional | 85% | High risk | Included | 93% |
| Licking vagina | Additional | 76% | Medium risk | Included | 76% |
| Sharing sex toys | Additional | 88% | High risk | Included | 91% |
3.4. Top 10 Priority Risk Behaviours
In response to comments and discussions from the Delphi experts, the consensus group made minor revisions to the list. Of the 13 items on the priority list only 10 were selected to be kept as top 10 priority-risk behaviours, which resulted in the final list. Through the Delphi process with the MSM experts, it was possible to develop a top 1 MSM risky sexual behaviour priority list. The results indicate that both receptive and insertive anal sex, having sex with multiple partners, having sex with a partner of unknown HIV status, having sex with an HIV-positive partner without a condom, and sharing needles appear to be the top 5 priority-risk behaviours. Table 4 captures the indicators submitted to the experts, the rates of both receptive and insertive anal sex (100% agreement), having multiple partners (100% agreement), having sex with a partner of unknown HIV status (100% agreement), having sex with an HIV-positive partner without a condom (100% agreement), group sex (93% agreement), both receptive and insertive oral sex (93% agreement), having sex without a condom (100% agreement), having sex under the influence of alcohol (100% agreement), both performed and received rimming (88% agreement), and the sharing of sex toys (95% agreement). The experts did not select nine suggested indicators during the Delphi process when selecting and developing the top 10 priority list. These indicators were excluded not because they were not important but for the sake of priority. Finally, a list of the top 10 indicators of MSM risky sexual behaviour was produced.
| Indicators | Consensus to Include, Exclude or add the Indicator | Agreement (n) | Categorised as Inappropriate (low risk), Equivocal, or Appropriate (high risk) | Final Decision | Agreement (n) |
|---|---|---|---|---|---|
| Insertive anal sex – he put his penis into your anus | Included | 93% | High risk | Not included | 93% |
| Receptive anal sex– you put your penis into his anus | Included | 86% | High risk | Not included | 93% |
| Both receptive and insertive anal sex | Included | 100% | High risk | Included | 100% |
| Performed oral sex – he sucked your penis | Included | 72% | Medium risk | Not included | 66% |
| Received oral sex– you sucked his penis | Included | 72% | Medium risk | Not included | 66% |
| Both received and performed oral sex | Included | 82% | High risk | Included | 93% |
| Performed rimming – you licked his anus | Included | 65% | Low risk | Not included | 71% |
| Received rimming – he licked your anus | Included | 65% | Low risk | Not included | 71% |
| Both performed and received rimming | Included | 85% | High risk | Included | 94% |
| Had sex with multiple partners | Included | 100% | High risk | Included | 100% |
| Vaginal penetration – you put your penis in a women’s vagina | Included | 80% | High risk | Not included | 82% |
| Had sex without a condom | Included | 100% | High risk | Included | 100% |
| Had sex with a partner of unknown HIV status | Included | 100% | High risk | Included | 100% |
| Had sex with a HIV-positive partner without a condom | Included | 100% | High risk | Included | 100% |
| Had sex under the influence of alcohol | Included | 100% | High risk | Included | 100% |
| Group sex | Added | 90% | High risk | Included | 95% |
| Licked a partner’s vagina | Added | 66% | Low risk | Not included | 76% |
| Shared sex toys | Added | 88% | High risk | Included | 95% |
| S.No. | - |
| 1 | Both receptive and insertive anal sex |
| 2 | Having sex with multiple partners |
| 3 | Having sex with a partner of unknown HIV status |
| 4 | Having sex with an HIV-positive partner without a condom |
| 5 | Group sex |
| 6 | Both receiving and performing oral sex |
| 7 | Having sex without a condom |
| 8 | Having sex under the influence of alcohol |
| 9 | Both performing and receiving rimming |
| 10 | Sharing sex toys |
4. DISCUSSION
The study aimed to identify risky sexual behaviour(s) commonly found among men who have sex with men (MSM) and prioritise them in order to guide the development of an intervention tool that could be used in the management of MSM risky sexual behaviours. When selecting the experts, we focused on the fact that the panel had to have a thorough knowledge of the topic of MSM risky sexual behaviour. The participation of as many as 14 MSM experts is evidence of good panel selection, interest in the subject, and the existence of active discussion related to the topic. To our knowledge and based on our literature review on this topic, this set of indicators consists of established MSM risky sexual practices. The experts were able to see and discuss one another’s responses, which allowed them to reflect on the views of others and reposition their own opinions accordingly [10]. The Delphi technique has been widely used in a large number of diverse domains such as the military, business, education, social science and health care [11]. It can be used in addressing a wide range of complex research aims, including forecasting, issue identification, issue prioritisation, ranking, policy formation and concept-framework development [12, 13]. It was possible to identify the top 10 priority-risk sexual behaviours of MSM Table 5 through the use of a Delphi-type process.
A study conducted in Dublin, Ireland found that MSM who engage in chemsex were more likely to have more sexual partners, more partners for anal intercourse and more condomless anal intercourse [14]. This is also revealed in this study, in that both receptive and insertive anal sex and having sex with multiple partners are considered most important among common MSM risky sexual practices.
The findings in this study are in line with the findings of Archteburg [1], where the participants reported experiencing varieties of anal, oral and vaginal sex, inconsistent condom use, and the use of alcohol or drugs when having sex. Their sexual partners have been shown to engage in patterns of sexual behaviour that place MSM at greater risk of contracting HIV. As indicated in the priority list, having sex without a condom is one of the priorities that need to be addressed. Studies conducted among Rwandan MSM and MSM students in South African higher education institutions have also found that risky sexual behaviour (unprotected anal sex or just unprotected sex) has major implications for HIV/STI transmission [15, 16].
In this study, both performed and received rimming were also found to be risky sexual behaviours. There was new evidence in one study, where it was found that oropharyngeal gonorrhoea can be transmitted by kissing through the established route of condomless oral sex, and anorectal gonorrhoea can be acquired when saliva is used as a lubricant for anal sex and rimming in condomless penile-anal sex among MSM [17]. This demonstrates the usefulness of relying on the expertise of MSM in developing a priority list of risky sexual behaviours in an attempt to minimise or reduce such practices among members of that population.
We also find that group sex is risky sexual behaviour that is practised by the MSM population. A study conducted in Bangkok, Thailand among HIV-positive MSM found that a rapidly emerging sexually transmitted hepatitis C virus (HCV) infection among MSM is fuelled by methamphetamine use and group sex [18]. Furthermore, Fulcher et al. (2018) found that group sex is a popular activity within certain sexual subcultures, including MSM. It has been differentiated by and described as Intensive Sex Partying, Party and Play, or Chemsex [19-21]. The evidence suggests that behavioural interventions to reduce the practice of risky sexual behaviours among MSM could be effective [22].
5. LIMITATION OF THE STUDY
This study cannot be generalised to the MSM population as a whole because the sample size was limited. Hence the priority list in this study cannot be used as a final list in other risky sexual behaviour contexts.
CONCLUSION
The consultation of MSM experts enabled us to prioritise the 10 most risky sexual behaviours of MSM. The list may be applied across or within countries when dealing with MSM risky sexual behaviours, taking the limitation described in 5 above into account. The study finds that the Delphi technique is useful in collecting expert opinions as to the priority of risky sexual behaviours. The list developed here will be used as a tool to develop motivational interviews to enable behaviour change among the MSM in the context of our project.
LIST OF ABBREVIATIONS
| LGBT | = Lesbian, Gay, Bisexual and Transgender |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The performance of the study was ethically cleared by Sefako Makgatho Health Science University Research Ethics Committee (SMUREC reference number: SMUREC/H/168/2019: PG).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
An approved consent form was given to the participants and signed by them.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The availability of the data will be available upon request from the corresponding authors [M.A.F].
FUNDING
None.
CONFLICT OF INTERESTS
The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ACKNOWLEDGEMENTS
We thank all members of the MSM expert group at the NGO clinic for their participation in this research and for the thoroughness and seriousness of their responses.
Appendix 1: List of Articles Selected through the Literature Review
Aho J, Hakim A, Vuylsteke B, et al. Exploring risk behaviors and vulnerability for HIV among men who have sex with men in Abidjan, Cote d'Ivoire: poor knowledge, homophobia and sexual violence. PLoS One. 2014;9(6):e99591. Published 2014 Jun 24. doi:10.1371/journal.pone.0099591
Assi R, Hashim PW, Reddy VB, Einarsdottir H, Longo WE. Sexually transmitted infections of the anus and rectum. World J Gastroenterol. 2014;20(41):15262-15268. doi:10.3748/wjg.v20.i41.15262
Braun DL, Marzel A, Steffens D, et al. High Rates of Subsequent Asymptomatic Sexually Transmitted Infections and Risky Sexual Behavior in Patients Initially Presenting With Primary Human Immunodeficiency Virus-1 Infection. Clin Infect Dis. 2018;66(5):735-742. doi:10.1093/cid/cix873
Cambou MC, Perez-Brumer AG, Segura ER, et al. The risk of stable partnerships: associations between partnership characteristics and unprotected anal intercourse among men who have sex with men and transgender women recently diagnosed with HIV and/or STI in Lima, Peru. PLoS One. 2014;9(7):e102894. Published 2014 Jul 16. doi:10.1371/journal.pone.0102894
Okafor CN, Christodoulou J, Bantjes J, et al. Understanding HIV Risk Behaviors Among Young Men in South Africa: A Syndemic Approach. AIDS Behav. 2018;22(12):3962-3970. doi:10.1007/s10461-018-2227-x
Chow EP, Lau JT, Zhuang X, Zhang X, Wang Y, Zhang L. HIV prevalence trends, risky behaviours, and governmental and community responses to the epidemic among men who have sex with men in China. Biomed Res Int. 2014;2014:607261. doi:10.1155/2014/607261
Closson K, Lachowsky NJ, Cui Z, et al. Does age matter? Sexual event-level analysis of age-disparate sexual partners among gay, bisexual and other men who have sex with men (GBM) in Vancouver, Canada. Sex Transm Infect. 2017;93(5):332-341. doi:10.1136/sextrans-2016-052721
de Voux A, Baral SD, Bekker LG, et al. A social network typology and sexual risk-taking among men who have sex with men in Cape Town and Port Elizabeth, South Africa. Cult Health Sex. 2016;18(5):509-523. doi:10.1080/13691058.2015.1096419
García MC, Duong QL, Mercer LC, Meyer SB, Koppenhaver T, Ward PR. Patterns and risk factors of inconsistent condom use among men who have sex with men in Viet Nam: Results from an Internet-based cross-sectional survey. Glob Public Health. 2014;9(10):1225-1238. doi:10.1080/17441692.2014.948481
Hakim AJ, Aho J, Semde G, et al. The Epidemiology of HIV and Prevention Needs of Men Who Have Sex with Men in Abidjan, Cote d'Ivoire. PLoS One. 2015;10(4):e0125218. Published 2015 Apr 24. doi:10.1371/journal.pone.0125218
Hambrick HR, Park SH, Goedel WC, et al. Rectal Douching Among Men Who Have Sex with Men in Paris: Implications for HIV/STI Risk Behaviors and Rectal Microbicide Development. AIDS Behav. 2018;22(2):379-387. doi:10.1007/s10461-017-1873-8
He J, Xu HF, Cheng WB, et al. Intimate relationship characteristics as determinants of HIV risk among men who have sex with regular male sex partners: a cross-sectional study in Guangzhou, China. BMC Infect Dis. 2018;18 (1):150. Published 2018 Apr 2. doi:10.1186/s12879-018-3044-6
Jaiswal, A.; Kirubakaran, A. Sexual risk behavior, Mobility and HIV infection among the Kothi (Men Sex with Men) in Puducherry. Scholedge International Journal of Multidisciplinary & Allied Studies, [s. l.], v. 3, n. 11, p. 231–237, 2016. DOI 10.19085/journal.sijmas031101.
Keshinro B, Crowell TA, Nowak RG, et al. High prevalence of HIV, chlamydia and gonorrhoea among men who have sex with men and transgender women attending trusted community centres in Abuja and Lagos, Nigeria. J Int AIDS Soc. 2016;19 (1):21270. Published 2016 Dec 7. doi:10.7448/IAS.19.1.21270
Lahuerta M, Patnaik P, Ballo T, et al. HIV Prevalence and Related Risk Factors in Men Who Have Sex with Men in Bamako, Mali: Findings from a Bio-behavioral Survey Using Respondent-Driven Sampling. AIDS Behav. 2018;22(7):2079-2088. doi:10.1007/s10461-017-1793-7
Li D, Li C, Wang Z, Lau JT. Prevalence and associated factors of unprotected anal intercourse with regular male sex partners among HIV negative men who have sex with men in China: a cross-sectional survey. PLoS One. 2015;10(3):e0119977. Published 2015 Mar 27. doi:10.1371/journal.pone.0119977
Mboumba Bouassa RS, Mbeko Simaleko M, Camengo SP, et al. Unusual and unique distribution of anal high-risk human papillomavirus (HR-HPV) among men who have sex with men living in the Central African Republic. PLoS One. 2018;13(5):e0197845. Published 2018 May 24. doi:10.1371/journal.pone.0197845
Meng X, Zou H, Fan S, et al. Relative Risk for HIV Infection Among Men Who Have Sex with Men Engaging in Different Roles in Anal Sex: A Systematic Review and Meta-analysis on Global Data. AIDS Behav. 2015;19(5):882-889. doi:10.1007/s10461-014-0921-x
Meredith G. B. Evans, Allanise Cloete, Nompumelelo Zungu and Leickness C. Simbayi (2016): HIV Risk Among Men Who Have Sex With Men, Women Who Have Sex With Women, Lesbian, Gay, Bisexual and Transgender Populations in South Africa: A Mini-Review; Institute for Humanities in Africa) and Department of Sociology, University of Cape Town, Cape Town, South Africa
Moore, A. R. et al. Sexual identity and risk behavior among men who have sex with men (MSM) in Accra, Ghana and Lomẻ, Togo. Cogent Medicine, [s. l.], v. 4, n. 1, p. 0, 2017. DOI 10.1080/2331205X.2017.1333696
Müller EE, Rebe K, Chirwa TF, Struthers H, McIntyre J, Lewis DA. The prevalence of human papillomavirus infections and associated risk factors in men-who-have-sex-with-men in Cape Town, South Africa. BMC Infect Dis. 2016;16(1):440. Published 2016 Aug 22. doi:10.1186/s12879-016-1706-9
Nelson LE, Wilton L, Agyarko-Poku T, et al. Predictors of condom use among peer social networks of men who have sex with men in Ghana, West Africa. PLoS One. 2015;10(1):e0115504. Published 2015 Jan 30. doi:10.1371/journal.pone.0115504
Newcomb ME, Ryan DT, Garofalo R, Mustanski B. The effects of sexual partnership and relationship characteristics on three sexual risk variables in young men who have sex with men. Arch Sex Behav. 2014;43(1):61-72. doi:10.1007/s10508-013-0207-9
Rebe K, Lewis D, Myer L, de Swardt G, Struthers H, Kamkuemah M, et al. (2015) A Cross Sectional Analysis of Gonococcal and Chlamydial Infections among Men-Who-Have-Sex-with-Men in Cape Town, South Africa. PLoS ONE 10(9):
e0138315. doi:10.1371/journal.pone.0138315
Remco Peters, Oscar Radebe, Thabo Hamiwe, Lerato Maboko, Helen Struthers, James Mcintyre, Marleen Kock.; (2017). High rate of repeatI sexually transmitted infections among men who have sex with men in South Africa, Anova Health Institute, Johannesburg, South African Republic; University of Pretoria, Pretoria, South African Republic. 10.1136/sextrans-2017-053264.425
Ross MW, Nyoni J, Ahaneku HO, Mbwambo J, McClelland RS, McCurdy SA. High HIV seroprevalence, rectal STIs and risky sexual behaviour in men who have sex with men in Dar es Salaam and Tanga, Tanzania. BMJ Open. 2014;4(8):e006175. Published 2014 Aug 28. doi:10.1136/bmjopen-2014-006175
Sadlier C; Rowley D; Morley D; Surah S; O'Dea S; Delamere S; O'Leary J; Smyth P; Clarke S; Sheils O; Bergin C; HIV Medicine. 2014;15(8):499-504. Prevalence of Human Papillomavirus in Men Who Have Sex with Men in the Era of an Effective Vaccine. www.medscape.com
Saha MK, Mahapatra T, Biswas S, Ghosh P, Kire M. Burden and correlates of HIV risk among men who have sex with men in Nagaland, India: analysis of sentinel surveillance data. PLoS One. 2015;10(2):e0117385. Published 2015 Feb 17. doi:10.1371/journal.pone.0117385
Sandfort TG, Lane T, Dolezal C, Reddy V. Gender Expression and Risk of HIV Infection Among Black South African Men Who Have Sex with Men. AIDS Behav. 2015;19(12):2270-2279. doi:10.1007/s10461-015-1067-1
Scott E R; John B. Jemmott III; Ann O’Leary; Larry D. Icard. (2018); What’s In an Identity Label? Correlates of Sociodemographics, Psychosocial Characteristics, and Sexual Behavior Among African American Men Who Have Sex with Men: Arch Sex Behav (2018) 47:157–167 https://doi.org/10.1007/s10508-016-0776-5
Semple SJ, Pitpitan EV, Goodman-Meza D, et al. Correlates of condomless anal sex among men who have sex with men (MSM) in Tijuana, Mexico: The role of public sex venues. PLoS One. 2017;12(10):e0186814. Published 2017 Oct 24. doi:10.1371/journal.pone.0186814
Sheehy M, Tun W, Vu L, Adebajo S, Obianwu O, Karlyn A. High levels of bisexual behavior and factors associated with bisexual behavior among men having sex with men (MSM) in Nigeria. AIDS Care. 2014;26(1):116-122. doi:10.1080/09540121.2013.802281
Yi S, Tuot S, Chhoun P, Brody C, Pal K, Oum S. Factors associated with recent HIV testing among high-risk men who have sex with men: a cross-sectional study in Cambodia. BMC Public Health. 2015;15:743. Published 2015 Aug 1. doi:10.1186/s12889-015-2096-4
Su X, Zhou AN, Li J, et al. Depression, Loneliness, and Sexual Risk-Taking Among HIV-Negative/Unknown Men Who Have Sex with Men in China. Arch Sex Behav. 2018;47(7):1959-1968. doi:10.1007/s10508-017-1061-y
Vagenas P, Ludford KT, Gonzales P, et al. Being unaware of being HIV-infected is associated with alcohol use disorders and high-risk sexual behaviors among men who have sex with men in Peru. AIDS Behav. 2014;18(1):120-127. doi:10.1007/s10461-013-0504-2
Dai W, Luo Z, Xu R, et al. Prevalence of HIV and syphilis co-infection and associated factors among non-commercial men who have sex with men attending a sexually transmitted disease clinic in Shenzhen, China. BMC Infect Dis. 2017;17(1):86. Published 2017 Jan 18. doi:10.1186/s12879-017-2187-1
Williams, P. P.; Carney, T.; Parry, C. D. H. Reducing substance use and sexual risk behaviour among men who have sex with men in South Africa. South African Journal of Science, [s. l.], v. 112, n. 9/10, p. 48–52, 2016. Disponível em: http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,sso&db=edb&AN=118506791&site=eds-live. Acesso em: 18 abr. 2021.
Williams, P. P. et al. Intervening to identify and reduce drug use and sexual HIV risk patterns among men who have sex with men in three provinces in South Africa. Journal of Substance Use, [s. l.], v. 19, n. 1/2, p. 141–146, 2014.
Xiaohong Pan et al. Sexual risk behaviour, sexual victimisation, substance use and other factors related to depression in men who have sex with men in Wenzhou, China: a cross-sectional study. BMJ Open, [s. l.], v. 8, n. 4, p. 1–10, 2018
Xu W, Zheng L, Liu Y, Zheng Y. Sexual sensation seeking, sexual compulsivity, and high-risk sexual behaviours among gay/bisexual men in Southwest China. AIDS Care. 2016;28(9):1138-1144. doi:10.1080/09540121.2016.1153587
Yang C, Latkin C, Tobin K, et al. An Event-Level Analysis of Condomless Anal Intercourse with a HIV-Discordant or HIV Status-Unknown Partner Among Black Men Who Have Sex with Men from a Multi-site Study. AIDS Behav. 2018;22(7):2224-2234. doi:10.1007/s10461-018-2161-y
Yi S, Tuot S, Chhoun P, et al. Improving prevention and care for HIV and sexually transmitted infections among men who have sex with men in Cambodia: the sustainable action against HIV and AIDS in communities (SAHACOM). BMC Health Serv Res. 2016;16(1):599. Published 2016 Oct 21. doi:10.1186/s12913-016-1857-9
Wang Y, Wang Z, Jia M, et al. Association between a syndemic of psychosocial problems and unprotected anal intercourse among men who have sex with men in Shanghai, China. BMC Infect Dis. 2017;17(1):46. Published 2017 Jan 7. doi:10.1186/s12879-016-2132-8
Yang Z, Huang Z, Dong Z, Zhang S, Han J, Jin M. Prevalence of high-risky behaviors in transmission of HIV among high school and college student MSM in China: a meta-analysis. BMC Public Health. 2015;15:1272. Published 2015 Dec 21. doi:10.1186/s12889-015-2614-4


