All published articles of this journal are available on ScienceDirect.
Magnitude of Tetanus Toxoid Immunization and Associated Factors among Pregnant Women in Ethiopia
Abstract
Background:
Maternal and neonatal tetanus remains a major global health problem. Two-thirds of the cases of neonatal tetanus occur in the poorest and least developed countries, including Ethiopia.
Objective:
This study aimed to calculate the magnitude and identify associated factors of tetanus toxoid immunization among pregnant women in Ethiopia.
Methods:
The 2016 Ethiopian demographic and health survey data were accessed and used for the analysis. A total of 7193 pregnant women were included in this study. A multilevel hurdle Poisson model was conducted to identify factors associated with tetanus toxoid immunization among pregnant women.
Results And Discussion:
Only 41.6% of pregnant women had received at least two doses of tetanus vaccine, while 58.4% received less than two doses. The multilevel hurdle Poisson model showed that residence, wealth index, education level of women, occupation of women, education level of husbands, ANC, presence of mobile phones, region, frequency of listening radio and frequency of watching television were significantly associated with tetanus toxoid immunization.
Conclusion:
Tetanus toxoid immunization coverage in Ethiopia was low. The concerned governmental organization sought to resolve enumeration area variation in tetanus toxoid immunization and closely monitored its implementation. Providing quality antenatal care, enhancing women’s educational level, and involving husbands in tetanus toxoid immunization are effective strategies to increase tetanus toxoid immunization coverage. Besides, the low-income households and the rural settings should also be given special consideration.
1. INTRODUCTION
Tetanus is an infectious disease caused by a toxin produced by the bacterium Clostridium Tetani, whose spores are commonly found in soil, dust, and manure that can enter the body through any skin injury [1, 2]. Untreated neonatal tetanus case fatality rates can be as high as 85-100% [3-5]; hospitalized case fatality rates differ significantly (depending on the quality of care) [5, 6] and non-neonatal case fatality rates can be 50-60% [7]. Most cases occur during the neonatal period, but disease surveillance in low and middle-income countries in other age groups is suboptimal [2, 8, 9].
Maternal and neonatal tetanus remains a public health problem in developing countries [10]. In 2017, 38,000 people worldwide died from tetanus. Around half of them (49%) were under five years of age. Most new tetanus cases occurred in South Asia and Sub-Saharan Africa in 2017. The two regions account for 82% of all tetanus cases globally. Likewise, 77% of all tetanus deaths occur in South Asia and Sub-Saharan Africa with 29,500 lost lives. Tetanus cases are still more common in Sub-Saharan Africa than everywhere else in the world. In 2017, South Sudan and Somalia had rates of tetanus cases greater than 10 per 100,000 people [11-13]. Ethiopia is one of 18 countries where maternal and neonatal mortality remains a public health problem. The maternal and neonatal mortality rates in Ethiopia are 412 per 100,000 live births and 29 per 1000 live births, respectively. This mortality rate is the highest maternal and neonatal death rate in comparison to other Sub-Saharan African countries [13, 14].
TT immunization can be given safely during pregnancy to protect both the mother and the baby [10, 15, 16]. Vaccines containing tetanus have been part of the WHO Extended Program on Immunization since its inception for babies and pregnant women [10, 17]. To prevent maternal and neonatal tetanus, the World Health Organization (WHO) recommends five doses of tetanus toxoid vaccine for previously unvaccinated women or those with unknown immunization status [15, 18]. Getting two doses of the tetanus toxoid vaccine during the first pregnancy is recommended. The first dose is given at the time of initial contact with healthcare services, and the second dose is given four weeks later, at least two weeks before delivery. The third dose should be given at least 6 months after the second, although the last two boosters can be given during subsequent pregnancies or at least one year later [18, 19].
Immunization against maternal tetanus was still required for 40 million pregnant women worldwide. TT immunization coverage among pregnant mothers currently stands at 75% worldwide, with rates ranging from 95% in Southeast Asia to 53% in the East Mediterranean and 63% in Africa [20, 21]. It was concluded that most countries would fail to meet the WHO global immunization target of at least 90% national TT vaccine coverage and at least 80% coverage in each district [21, 22]. Due to low TT immunization coverage, Ethiopia has the world's highest rates of maternal and neonatal tetanus morbidity and mortality. The 2016 Ethiopian Demographic and Health Survey (EDHS) showed that only 49% of pregnant women were immunized against tetanus [14].
Previous TT immunization studies in developing countries considered only prevalence alone (i.e whether or not women received TT immunization and used a logistic regression model to evaluate such prevalence [13, 21, 23-28]. Although the number of TT immunization is undercounted by binary logistic regression since multiple immunizations are collapsed into a single unit to satisfy binary logistic regression criteria, adequate information is given to analyze the pattern of multiple TT immunization [29, 30]. The count regression model is the preferred model of analysis in this study. The most well-known technique for modeling count data is the Poisson regression model. Although, it is appropriate only for modeling equi-dispersed distribution (i.e., the variance is equal to the mean). Many real data do not conform to this assumption (over- or under-dispersed data) and the improper imposition of Poisson regression model may underestimate the standard errors and overestimate the significance of regression coefficients [30, 31]. Over dispersion mainly happens for two reasons. The first is apparent over-dispersion; it arises when the model has been poorly defined (not including significant variables, interactions between predictors that have already been measured or by specifying the incorrect link function). The second is real over-dispersion; it can also occur when the count data is clustered (measurements are not completely independent of each other), when there is an excess number of zeros in the data (zero-inflation), and when the response variance is truly greater than the mean (i.e., the Poisson process is not accurately described) [30, 32, 33]. By adding a dispersion parameter to accommodate unobserved heterogeneity in count data, the negative binomial model addresses the issue of over-dispersion [34]. For under-dispersed data, the negative binomial models are not sufficient. Under-dispersed data is less commonly observed. In regard to analytical application with zero values in the data, the negative binomial model may be inadequate. By allowing over-dispersion, zero-inflated models provide a way of modeling the excessive proportion of zero. If the number of zero values is high in the data, a zero-inflated model provides a good fit as compared to the Poisson or negative binomial model [35, 36]. Nevertheless, the zero-inflated model is not sufficient for under-dispersed data. The hurdle-based model is a versatile alternative that captures both over and under-dispersion data [37]. Moreover, heterogeneity in the enumeration area of the study could be responsible for the variation in the determinants of the number of TT immunization. We also suggested a two-level random effect count model for TT immunization to resolve this [38]. Therefore, this study aimed to calculate the magnitude and identify associated factors of tetanus toxoid immunization among pregnant women in Ethiopia.
2. METHODS
2.1. Data Source
An in-depth analysis of the EDHS 2016 data was undertaken for this study. The EDHS 2016 was a population-based cross-sectional study conducted across the country. It is the fourth national survey conducted to provide estimates in representative rural and urban areas of Ethiopia about the targeted health and demographic variables. In the 2016 EDHS, stratified and cluster multistage sampling was used, and it was intended to be representative at the regional and national level in terms of appropriate demographic and health indicators. In the first stage, 645 clusters of enumeration areas (EAs) (202 urban and 443 rural) were identified using probability proportional to the size of EAs. In the second stage, random samples of 18,008 households were selected from all the identified EAs.
2.2. Study Variables
The outcome variable of this study was a count response of the number of times they have immunized against tetanus toxoid during their last pregnancy. The explanatory variables of this study were selected by reviewing related work of the literature [13, 21, 23-28]. Age of women, wealth index, marital status, number of living children, family size, religion, region, residence, husband education level, women education level, women occupation, radio use, TV use, internet use, mobile and ANC visit was the possible predictors of TT immunization.
2.3. Statistical Software
The secondary data were extracted and managed in SPSS software version 21 and then exported to R software version 3.5.3 for analysis.
2.4. Data Management and Analysis
After extracting data using SPSS statistical software version 21, the data were weighted using sampling weight (v005), main sampling unit (v023), and strata (v021) to draw appropriate inferences. The data were described using descriptive statistics such as percentages, bar charts, and frequency tables. Women were nested within a cluster in the DHS data, and they may have shared common characteristics within the cluster. Since the data are hierarchical, the standard count regression model's assumptions of independence of observations and equal variance were violated. This means that advanced models must take into account the heterogeneity between clusters. The multilevel count regression model was used to identify the individual and community-level factors associated with tetanus toxoid immunization among pregnant women. Multilevel count data also exist in public health studies on health care, behavioral research, and epidemiology example, mothers nested within enumeration area. The consequences of clustering of the respondents within the enumeration area are that respondents from the same enumeration area may have outcomes that are more similar than will respondents from different enumeration area. Multilevel Hurdle Poisson count regression models incorporate cluster specific random effects that account for the dependency of the data.
The two level Poisson Hurdle model can be defined as
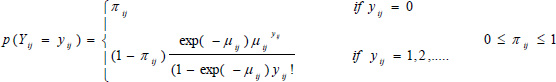 |
(1) |
The two level Poisson hurdle regression model is
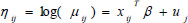 |
(2) |
 |
(3) |
Where xij and zij are respectively, vectors of covariates for the NB and the logistic components, and β and γ are the corresponding vectors of regression coefficients. The random effects uj and wj are assumed to be independent and normally distributed with mean 0 and variance δu2 and δw2, respectively [39]. The two sets of covariates might or might not be the same. Furthermore, using the Poisson and Bernoulli regression models' assumptions, the adjusted odd ratio (AOR) and incidence rate ratio (IRR) with a 95% confidence interval were used to examine the strength of relationships between the outcome and the independent variables. P values of < 0.05 were considered statistically significant.
3. RESULTS
3.1. Magnitude of Tetanus Toxoid Immunization among Pregnant
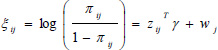
A total of 7193 pregnant women were studied. Only 41.6% of pregnant women have received at least two doses of tetanus vaccine, while 58.4% have received less than two doses. Since there are a large number of zero outcomes, the histograms are highly picked at the beginning (the zero outcomes). Further inspection, the variance (1.394) of the response variable is greater than the mean (1.239). This indicated that there is over-dispersion due to an excess of zeroes (Fig. 1).
3.2. Socio-demographic Characteristics of the Respondents
The majorities, 79.0% of women, were urban residents and more than two-thirds (70%) of the participants were housewives. With regard to their ANC visit, about 34.5% of women had no ANC visit, whereas 36.4% had four and above ANC visits. About 32.9% of the study participants were Orthodox Christian and almost all women (91.5%) were currently married. Largest proportions of women (48.8%) were in the age group of 20–29 years. Regarding educational status, 60.6% of the respondents never attended any formal education and about 30% of husbands had attended primary education. More than fifty-one percent of households had a poor wealth index (Table 1).
3.3. Determinants of Tetanus Toxoid Immunization among Pregnant Women in Ethiopia
The result of the Poisson hurdle model is presented in Table 2. Compared with urban residence, the rates of non-zero TT immunization for rural residents decreased by 6.5% (IRR=0.935, 95% CI; 0.876, 0.999). With regard to women occupation, the incidence rates of non-zero TT immunization for employed women was increased by 7.5% (IRR = 1.075; 95%CI: 1.009, 1.145) as compared to those housewife women. Compared with women who did not receive any antenatal visit during pregnancy, the incidence rate of non-zero TT immunization whose women who attended at least four ANC visits during pregnancy was increased by 20.3% (IRR=1.203, 95% CI; 1.081,1.338). As the husband’s education level increases, the number of TT immunization also increases. Compared to women from the Tigray region, the incidence rate of non-zero TT immunization was 1.620 times (IRR=1.620, 95% CI; 1.366, 1.921) higher than mothers from Dire Dawa city of administration (Table 2).
| Variables | Categories | Frequency | Percentage |
|---|---|---|---|
| Women educational level | No education | 4,359 | 60.6 |
| Primary | 1,942 | 27.0 | |
| Secondary and above | 892 | 12.4 | |
| Women age | 15-19 | 358 | 5.0 |
| 20-29 | 3,509 | 48.8 | |
| 30-39 | 2,675 | 37.2 | |
| 40-49 | 651 | 9.1 | |
| Women working status | Housewife | 5,033 | 70.0 |
| Employed | 2,160 | 30.0 | |
| Region | Tigray | 772 | 10.7 |
| Afar | 647 | 9.0 | |
| Amhara | 764 | 10.6 | |
| Oromia | 1,031 | 14.3 | |
| Somali | 806 | 11.2 | |
| Benshangul-Gumuz | 576 | 8.0 | |
| SNNPR | 893 | 12.4 | |
| Gambela | 534 | 7.4 | |
| Harari | 411 | 5.7 | |
| Addis Adaba | 375 | 5.2 | |
| Dire Dawa | 384 | 5.3 | |
| Place of residence | Urban | 1,512 | 21.0 |
| Rural | 5,681 | 79.0 | |
| Family size | Less than 3 | 206 | 2.9 |
| 3-4 | 2,140 | 29.8 | |
| 4 and above | 4,847 | 67.4 | |
| Wealth index | Poor | 3,607 | 50.1 |
| Middle | 1,028 | 14.3 | |
| Rich | 2,558 | 35.6 | |
| ANC | No antenatal visits | 2,481 | 34.5 |
| 1-3 | 2,092 | 29.1 | |
| 4 and above | 2,620 | 36.4 | |
| Number of children | 0-2 | 3,173 | 44.1 |
| 3-4 | 2,226 | 30.9 | |
| 5 and above | 1,794 | 24.9 | |
| Husband education level | No education | 3,719 | 51.7 |
| Primary | 2,160 | 30.0 | |
| Secondary and above | 1,314 | 18.3 | |
| Religion | Orthodox | 2,369 | 32.9 |
| Muslin | 3,324 | 46.2 | |
| Protestant and other | 1,500 | 20.9 | |
| Use of internet | No | 6,945 | 96.6 |
| Yes | 248 | 3.4 | |
| Mobile use | No | 5,312 | 73.8 |
| Yes | 1,881 | 26.2 | |
| Reading newspaper | No | 6,590 | 91.6 |
| Yes | 603 | 8.4 | |
| Frequency of listening to radio | Not at all | 5,343 | 74.3 |
| Less than once a week | 924 | 12.8 | |
| At least once a week | 926 | 12.9 | |
| Frequency of watching television | Not at all | 5,511 | 76.6 |
| Less than once a week | 628 | 8.7 | |
| At least once a week | 1,054 | 14.7 | |
| Marital status | Married | 6,579 | 91.5 |
| Others | 614 | 8.5 |
* Significant at 5% level of significance;
ANC, antenatal care; AOR, adjusted odd ratio; IRR, incidence rate ratio
The Bernoulli part is used to show the probability of receiving TT immunization. The estimated odds that the number of TT immunization becomes zero with rural women was 2.734 (AOR=2.734; 95% CI; 2.169, 3.447) times higher than urban women. The estimated odds that the number of TT immunization becomes zero with women’s from the richer wealth index decreased by 37% (AOR=0.630; 95% CI; 0.522, 0.761) compared to the poorest wealth index. The estimated odds that the number of TT immunization becomes zero with mothers who attend primary education level had 0.534 (AOR = 0.534; 95%CI: 0.468, 0.610) and mothers who attend secondary and higher education level had 0.455 (AOR = 0.455; 95%CI: 0.368, 0.563) times mothers who did not attend any formal education, respectively. The odds of the number of TT immunization became zero with mothers who attended at least four ANC visits during the pregnancy was 0.048 (AOR=0.048; 95% CI: 0.040, 0.059) times that of mothers who have not attended ANC visits. The estimated odds that the number of TT immunization becomes zero with husbands who have attend secondary and above education was 0.400 (AOR=0.400; 95% CI: 0.337, 0.474) times that of husbands who did not attend any formal education. The estimated odds of the number of TT immunization becoming zero with mothers who have a mobile phone was 0.621 (AOR=0.621; 95% CI: 0.530, 0.728) times that of mothers without mobile phone. Furthermore, the variance components for the random effects revealed that the substantial difference in TT immunization between the communities (enumeration area) was calculated to be 0.698 (95% CI: 0.635, 0.769) while the severity of the variance was 0.488 (95% CI: 0.412, 0.569) (Table 2).
4. DISCUSSION
Tetanus remains a significant public health problem in low and middle-income countries. This study has focused on assessing the magnitude of TT immunization and identifying associated factors of tetanus toxoid immunization among pregnant women. The study showed that 53.2% of pregnant women received at least one dose of TT immunization. This TT immunization converge was lower than, 72.5% in Damboya Woreda, South Ethiopia [21], 97.8% in Sierra Leone [25], 79% in Pakistan [27], 61.4% in Kenya [40] and 68% in India [41]. This coverage was also higher than 51.8% in Errer district, Somali Regional State, Eastern Ethiopia [23], 40.2% in Hawzen, Eastern Zone of Tigray, Ethiopia [13], 37.1% in Rivers State, Nigeria [28]. This may be attributable to disparities in cultural and socio-economic factor such as healthcare delivery systems, the availability of immunization in the health center, the degree of vaccination awareness and information, the incidence of vaccine-preventable diseases, the obtainable political climate and methodological variation in vaccination status assessment.
Place of residence is significantly associated with the utilization of TT immunization. Relative to rural women, women living in urban areas were more likely to obtain TT immunization. This finding was in agreement with a study done in Errer district, Somali Regional State, Eastern Ethiopia [23], Dukem town, Eastern Ethiopia [42] and Gondar comprehensive specialized hospital, northwest Ethiopia [43]. The justification for this might be that urban women have a better education, have better access to health care, and are more aware of the necessity of TT immunization.
Women's educational level was significantly associated with the utilization of TT immunization. As compared to non-educated women, educated mothers were more likely to receive a proper dose of TT immunization. This finding was supported by studies conducted in Somali Regional State, Eastern Ethiopia [23], Damboya Woreda, South Ethiopia [21], Dukem town, Eastern Ethiopia [42], Rivers State, Nigeria [28] and Ivory Coast [26]. This may be because of easy access to information and awareness of immunization program for educated women. Education is likely to improve the independence of women so that women can gain greater trust and the ability to make decisions about their own well-being.
This study revealed that the ANC visit was positively associated with the usage of TT immunization. Hence, it is learned that increasing the number of antenatal visits during pregnancy raises the usage of TT immunization. Previous studies conducted in the Eastern Zone of Tigray, Ethiopia [13], Damboya Woreda, South Ethiopia [21], Dukem town, Eastern Ethiopia [42], Sierra Leone [25], Ivory Coast [26], Pakistan [27] and Kenya [40] also supported our findings and reported that women who attended ANC program follow-ups frequently had a higher chance of TT immunization usage. The possible explanation for this might be women receiving more ANC visits are more likely to be told about the value of TT immunization.
There was a significant association between the usage of TT immunization and the household wealth index. Relative to the lower household wealth quintile, women who belong to the higher household wealth quintile had higher odds of TT immunization usage. This finding is consistent with the results of previous studies conducted in Sierra Leone [25], Alexandria [44], Kenya [40], Peshawar [45], and developing African and Asian countries [46], where TT vaccination was found to be positively associated with higher wealth index. The possible explanation for this might be women with the lowest family income status were disadvantaged and it was difficult to receive TT immunization because low-income families could spend high costs and time on maintaining their everyday lives. Women from high-income families would be able to meet the needs of TT immunization and health services.
The findings of this study also revealed that the employment status of the respondents was found to have a significant association with the usage of TT immunization. Employed women had a higher chance of using TT immunization than that housewife women. This result is consistent with studies conducted in Somali Regional State, Eastern Ethiopia [23] and Rivers State, Nigeria [28], and Kenya [40], which indicated that employed women had higher odds of receiving adequate doses of TT immunization. It may be that working women have more access to better awareness and contact about health care services in general and TT immunization as compared to housewife women [42]. Religion was another determinant factor for the utilization of TT immunization. Compared to other religious groups, women from the Orthodox Christian religion were more likely to receive TT immunization. This finding is similar to studies conducted in Rural North India [47]. The attribute of this result needs further investigation.
Husband's education level was also positively associated with the utilization of TT immunization. The likelihood of receiving TT vaccination increases as the husband's educational level rises. This result is consistent with studies conducted in Damboya Woreda, South Ethiopia [21], Somali Regional State, Eastern Ethiopia [23] and Peshawar [45]. This could be because educated husbands are more aware of the importance of TT vaccination and other maternal health services than uneducated husbands. Educated husbands may communicate better with their wives and provide their wives more freedom to receive tetanus toxoid immunization and other maternal health care [22].
When compared to women who had no media exposure, women who had media exposure were more likely to use tetanus toxoid vaccination. This is in line with the studies carried out in Hawzen, Eastern Zone of Tigray, Ethiopia [13], Dukem town, Eastern Ethiopia [42] and Sierra Leone [25]. This could be due to the reason that the media may supply crucial information that will raise women's awareness of the benefits of tetanus toxoid immunization. Besides, women who own a cell phone are more likely to have tetanus toxoid immunization than women who do not own a cell phone. The mobile phone alert also made it easier to schedule a visit to the health institution on the day indicated by the medical staff.
Furthermore, the regional variation was a significant predictor of TT immunization. Women live in Afar, Oromia, Somali, Gambela, Harari, Addis Adaba and Dire Dawa had a higher probability of receiving TT immunization compared to women living in the Tigray region. The result is consistent with a previous study done in Ethiopia [48, 49]. The reason for this regional difference is that there is a gap between regions in the coverage of health services, including the implementation of vaccine program.
5. STRENGTHS AND LIMITATION OF THE STUDY
EDHS is a national representative household survey with a high response rate and the findings are generalized to the national populations. The findings of the study also give up to date evidence for policymakers and program managers to understand how to adopt effective intervention methods to reduce high levels of maternal and newborn mortality. In addition, multilevel modeling was used to account for the hierarchical nature of the EDHS data. The study shows that other researchers will be able to understand how to use over-dispersed excess zeroes and the hurdle Poisson count regression model. Because of the cross-sectional nature of the data, it is difficult to measure the causal effect and it is not possible to know if the data depends on time or not. Another drawback was that DHS did not offer data on accessibility (i.e., distance to a health facility) or the quality of healthcare professionals, both of which could influence the use of Tetanus Toxoid Immunization among pregnant women. The relationship between the number of ANC visits, distance from health facility and TT vaccination, it would be important to note that this study includes women sampled from different regions, so presumably, their health-seeking behaviors are relatively different. Moreover, important variables such as previous vaccination history, presence of vaccination card and child mortality were not included in the analysis due to a large number of missing observations and the difficulty in dealing with those missing observations.
CONCLUSION
Only 41.6% of pregnant women received at least two doses of tetanus vaccine, while 58.4% received less than two doses. The utilization of the recommended number of tetanus immunization is low in Ethiopia. The multilevel hurdle Poisson model showed that residence, wealth index, education level of women, occupation of women, education level of husbands, ANC, presence of mobile phones, region, frequency of listening radio and frequency of watching television were significantly associated with tetanus toxoid immunization. The random effect model also showed significant differences in TT immunization between enumeration areas. The concerned governmental organization sought to resolve enumeration area variation in tetanus toxoid immunization and closely monitored its implementation. Providing quality antenatal care, enhancing women’s educational level and involving husbands in tetanus toxoid immunization are effective strategies to increase tetanus toxoid immunization utilization. Besides, the poorest people and the rural environment should also be given special consideration.
LIST OF ABBREVIATIONS
| AIC | = Akaike’s information criterion |
| AOR | = Adjusted odds ratio |
| ANC | = Antenatal Care |
| BIC | = Bayesian information criterion |
| CSA | = Central Statistical Agency |
| CI | = Confidence intervals |
| DIC | = Deviance information criterion |
| EDHS | = Ethiopian Demographic and Health Survey |
| HNB | = Hurdle negative binomial |
| HP | = Hurdle Poisson |
| NB | = Negative binomial |
| SNNPR | = Southern Nations, Nationalities, and People Region |
| TT | = Tetanus Toxoid |
| ZINB | = Zero-inflated negative binomial |
| ZIP | = Zero-inflated Poisson |
AUTHORS’ CONTRIBUTION
SM drafted the proposal, did the analysis, wrote the results and prepared the manuscript. HM participated on editing, analysis and write up of the result. All authors read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study used secondary data available and released under the National Data Sharing and Accessibility Policy (NDSAP) of Government of Ethiopia. The data set had no identifiable information on the survey participants; therefore no ethical approval is required for this work.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
STANDARD OF REPORTING
STROBE Guideline were followed.
AVAILABILITY OF DATA AND MATERIALS
The dataset was accessed from the Measure DHS website: (http://www.measuredhs.com).
FUNDING
None.
CONFLICT OF INTEREST
The authors declare that no competing interests exist.
ACKNOWLEDGEMENTS
We would like to thank Ministry of Health and Central Statistical Agency, Government of Ethiopia, for making the data freely available for research purposes.


