All published articles of this journal are available on ScienceDirect.
Determinant Infection Prevention and Control Practices among Nurses during COVID-19 Pandemic
Abstract
Background:
Most of the nurses’ duties require direct contact with patients. Nurses with a high vulnerability to COVID-19 should have the self-awareness to reduce and avoid the risk of infection transmission. It is significant to know the factors that influence the practice of infection prevention and control in nurses while treating COVID-19 patients.
Objective:
This study aims to determine the factors that influence the practice of infection prevention and control in nurses.
Methods:
This study was a descriptive survey conducted in 4 hospitals in Makassar City, South Sulawesi, Indonesia, with a sample of 360 nurses in January-June 2021. The data were analyzed using the canonical multivariate test.
Results:
This study finds a strong correlation between the self-labeling of nurses as at-risk individuals (.703) and taking actions (.707). In addition, there is a strong correlation between self-justification (.925) and obtaining remedies (.995), and there is a strong correlation between commitment (.791) and information seeking (.884) (ρ= < .05).
Conclusion:
Strengthening the commitment and self-labeling of nurses as individuals at risk of being exposed to COVID-19 is very important for infection prevention and control practices.
1. INTRODUCTION
The COVID-19 pandemic in 2020 has significantly impacted hospital care [1]. Moreover, COVID-19 has raised concerns about the healthcare sector due to the increasing number of confirmed cases worldwide [2]. One of the most critical situations of plague and new infectious diseases is preventing the spread of these agents in healthcare settings [3]; [4]. Patients or healthcare workers could be the source of infection or a susceptible host for infection. Every person or worker in health care facilities risks infection and transmission. Infection control is the responsibility of each individual and could be done by understanding the disease transmission model and knowing the basic principles of prevention and successful infection control [5].
Nurses have always played an important role in infection prevention, infection control, isolation, containment, and public health [6, 7]. Other study found that 11.2% of people work at COVID-19 referral hospitals, and 61% of them probably or certainly have been contacted with COVID-19 and suspected positive patients [8]. Meanwhile, 36.2% of health staff work on the front line handling positive COVID-19 patients, and 75.3% feel that they have been exposed to COVID-19. In addition, most health workers experience depression (52.1%), anxiety (57.6%), and insomnia (47.9%). Moreover, 73.3% of health workers have psychological disorders because they feel at risk of being exposed to COVID-19.
When nurses work in an environment with high job demands and low resources, higher job stress and greater physical and psychological stress symptoms could affect their health and prosperity [9, 10]. Nursing roles also bring psychological impacts to all members of the community; these impacts include fear of contracting pathogens, worries about family, and social isolation [11, 12]. They are at high risk of infection and experience depression, anxiety, insomnia, stigma, and frustration [13]. Nurses should adapt to work in a setting or system of care during the pandemic [14]. Maintaining the nursing staff’s mental health is pivotal to controlling infectious diseases [15, 16].
Preventive behavior is defined as individual behavior that is primarily motivated by the goal of reducing the risk of COVID-19 infection [17]. Preventing the spread of infection to and from healthcare workers and patients depends on the effective use of personal protective equipment (PPE), such as gloves, face masks, air-purifying respirators, protective eyewear, face shields, respirators, and protective clothing [18, 19]. Protecting health workers is very important to maintain continuous care and ensure that nurses do not become infected agents [20]. Based on those reasons, knowing the factors that influence the practice of infection prevention and control in nurses and how much nurses carry out those factors is significant. Therefore, this study aims to measure nurses’ infection prevention and control practices and investigate the factors that influence those factors.
2. MATERIALS AND METHODS
2.1. Study Area and Design
This research employed a descriptive survey and employed cross-sectional approach. This research was conducted in 4 government hospitals in Makassar City, South Sulawesi, Indonesia, in January-June 2021.
2.2. Participants
The samples were selected using purposive sampling techniques. These techniques selected samples from a population by considering the research objectives. Therefore, the sample could represent the population's characteristics previously known [21]. The sample size employed sample size determination in health studies. The total samples of this research were 360 nurses. The inclusion criteria for the research samples were registered nurses who had cared for COVID-19 patients in hospitals and voluntarily participated in the studies. Nurses who cared for patients with other illnesses were excluded from the study.
2.3. Research Instrument and Data Collection
The research instruments were questionnaires and observation sheets according to the number of variables. Researchers adopted six sets questionnaires of self-justification, labeling, commitment, information seeking, obtaining remedies, and taking action [22]. Self-justification category (internal: if the total score of the respondent's answers is < 56, external ≥ 56); labeling category (strong if the total score of the respondent's answers is ≥ 20, weak < 20), commitment category (strong if the total score of the respondent's answers is ≥ 7, weak < 7), information seeking category (strong if the total score of the respondent's answers is ≥ 3, weak < 3), obtaining remedies (strong if the total score of the respondent's answers is ≥ 7, weak < 7), and taking action (strong if the total score of the respondent's answers is ≥ 50, weak < 50).
The data were taken and obtained directly using questionnaires and observation sheets. The primary data were collected from nurses, preceded by asking for informed consent. The researcher considered the condition of the nurses’ activities before giving the questionnaire.
2.4. Statistical Analysis
This research employed a quantitative method with Canonical analysis to discover the greatest correlation of pairs of combined variables. Research variables include self-justification (refers to the nurse's self-justification for how to reduce the risk of COVID-19 transmission), labeling (when a nurse labels or identifies himself as a risky individual), commitment (when a nurse decides with multiple outcomes), information seeking (nurses collect information on how to modify behaviors that increase the risk of contracting COVID-19), obtaining remedies (nurses enact strategies to modify risky behavior), and taking action (nurses take precautions to reduce the risk of infection COVID-19). All analyses were performed using the Statistical Package for the Social Sciences (version 22.0; IBM, Armonk, NY, USA). The data with a p-value < .05 was considered statistically significant.
3. RESULTS
The characteristics of respondents are shown in Table 1. The majority of respondents (46.9%) are between the ages of 31 and 40. The majority of respondents (78.6%) are female, and the majority of respondents most recent education is Professional Nurses (58.3%). According to the data on length of employment, the majority of respondents (54.2%) have worked in the hospital for more than 6 years. The majority of respondents (84.4%) work as Nurse Practitioners.
| Criteria | Frequency (n) | Percentage (%) |
|---|---|---|
| Ages | ||
| 20-30 years old | 129 | 35.8 |
| 31-40 years old | 169 | 46.9 |
| 41-50 years old | 52 | 14.4 |
| 51-60 years old | 10 | 2.8 |
| Total | 360 | 100 |
| Gender | ||
| Male | 77 | 21.4 |
| Female | 283 | 78.6 |
| Total | 360 | 100 |
| Marital Status | ||
| Married | 273 | 75.8 |
| Unmarried | 87 | 24.2 |
| Total | 360 | 100 |
| Latest Education | ||
| Nursing Diploma | 101 | 28.1 |
| Bachelor of Nursing | 43 | 11.9 |
| Professional Nurse | 210 | 58.3 |
| Master of Nursing | 6 | 1.7 |
| Total | 360 | 100 |
| Employment Status | ||
| Permanent Employees/Civil servant | 134 | 37.2 |
| Contract employees | 224 | 62.2 |
| Internship | 2 | 0.6 |
| Total | 360 | 100 |
| Work Duration | ||
| 1-3 years | 93 | 25.8 |
| 4-6 years | 72 | 20.0 |
| >6 years | 195 | 54.2 |
| Total | 360 | 100 |
| Occupations | ||
| Head of Nurse | 15 | 4.2 |
| Team Leader | 41 | 11.4 |
| Nurse Practitioner | 304 | 84.4 |
| Total | 360 | 100 |
| Income | ||
| >3,500,000 | 168 | 46.7 |
| 2,500,000-3,500,000 | 246 | 40.6 |
| 2,500,000-1,500,000 | 46 | 12.8 |
| Total | 360 | 100 |
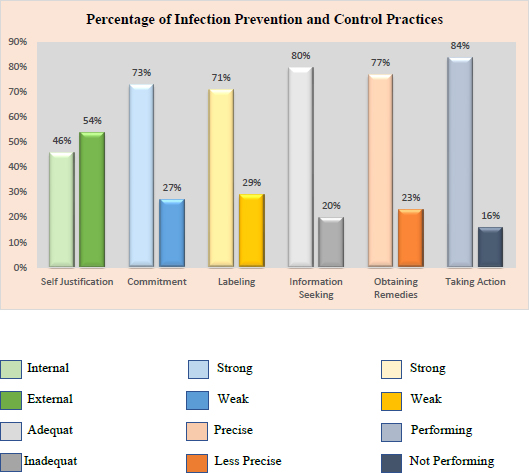
According to the findings of this study, nurses performed well on the majority of infection prevention and control practices while caring for COVID-19 patients. The application of safe behavior in preventing the transmission of COVID-19 (taking action) has the highest percentage (84%), followed by related information-seeking actions in preventing the transmission of COVID-19 (80%), and finally determining ways to change risks (obtaining remedies) (77%). Furthermore, the majority of nurses (73%) are committed to infection prevention and transmission practices, and nurses who label themselves as individuals (71%) are at risk of contracting COVID-19 (labelling) (Fig. 1).
The results of the multivariate significance tests using Pillai's trace, Hotelling's rules, Wilk's formula, and Roy's adaptation model are shown in Table 2. Each test has a significance value of.000. This value denotes a significant correlation between the first, second, and third canonical functions. Furthermore, the first pair of canonical functions with the strongest correlation is taking action (.70760) and labeling (.70760). (.70317). The second pair of canonical functions with the strongest correlation is obtaining remedies (.99513) and self-justification (.92553). The third pair of canonical functions with the strongest correlation is information seeking (.88455) and commitment (.79143) (Table 3).
| Self Justification | Information Seeking | Obtaining Remedies | Taking Action | Pillai | Hotelling | Wilk | Roy | ρ | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adequate | Inadequate | ρ | Precise | Less Precise | ρ | Performing | Not Performing | ρ | ||||||||||||
| n | % | n | % | .025 | n | % | n | % | .030 | n | % | n | % | .022 | .33297 | .45599 | .67879 | .29341 | .000 | |
| Internal | 123 | 74.5 | 42 | 25.5 | 136 | 82.4 | 29 | 17.6 | 131 | 79.4 | 34 | 20.6 | ||||||||
| External | 164 | 84.1 | 31 | 15.9 | 142 | 72.8 | 53 | 27.2 | 172 | 88.2 | 23 | 11.8 | ||||||||
| Total | 287 | 79,7 | 73 | 20,3 | 278 | 77.2 | 82 | 22.8 | 303 | 84.2 | 57 | 15.8 | ||||||||
| Commitment | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||
| Strong | 225 | 85.2 | 39 | 14.8 | .001 | 210 | 79.5 | 54 | 20.5 | .081 | 243 | 92.0 | 21 | 8.0 | .001 | |||||
| Weak | 62 | 64.6 | 34 | 35.4 | 68 | 70,8 | 28 | 29.2 | 60 | 62.5 | 36 | 37.5 | ||||||||
| Total | 287 | 79,7 | 73 | 20,3 | 278 | 77.2 | 82 | 22.8 | 303 | 84.2 | 57 | 15.8 | ||||||||
| Labeling | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||
| Strong | 225 | 87,5 | 32 | 12,5 | .001 | 212 | 82,5 | 45 | 17,5 | .001 | 235 | 91,4 | 22 | 8,6 | .001 | |||||
| Weak | 62 | 60,2 | 41 | 39,8 | 66 | 64,1 | 37 | 35,9 | 68 | 66,0 | 35 | 34,0 | ||||||||
| Total | 287 | 79,7 | 73 | 20,3 | 278 | 77,2 | 82 | 22,8 | 303 | 84,2 | 57 | 15,8 | ||||||||
| Variable | Canonical Weight | Canonical Loading | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Canonical Function 1 | Canonical Function 2 | Canonical Function 3 | Canonical Function 1 | Canonical Function 2 | Canonical Function 3 | |||||||
| Independent | - | - | - | - | - | - | ||||||
| Self Justification | .054 | -.925 | -.425 | .224 | -.920 | -.318 | ||||||
| Commitment | -.634 | .119 | -.791 | -.708 | .259 | -.655 | ||||||
| Labeling | -.703 | -.382 | .608 | -.764 | .259 | -.655 | ||||||
| Dependent | - | - | - | - | - | - | ||||||
| Information Seeking | -.497 | .183 | .884 | -.677 | .104 | .728 | ||||||
| Obtaining Remedies | -.195 | -.995 | -.038 | -.353 | -.935 | -.005 | ||||||
| Taking Action | -.707 | .271 | -.696 | -.840 | .184 | -.510 | ||||||
According to these findings, nurses who take precautions to reduce the risk of COVID-19 infection are strongly influenced by labeling themselves as at-risk individuals. Furthermore, nurses enacting risky behavior modification strategies are closely related to nurses' self-justification in reducing the risk of COVID-19 transmission, and nurses seeking information about reducing the risk of COVID-19 transmission are closely related to their commitment. As a result, it is critical for nurse managers to reinforce all aspects of disease transmission in daily nursing practice.
4. DISCUSSIONS
This study shows the strongest correlation between nurses self labeling and infection prevention and control (taking action). In determining the status of self-recognition at risk of health workers regarding COVID-19 disease, A previous study has revealed that health workers have a high level of perception or self-recognition of risk. It means that the labeling of the COVID-19 disease must be very good so that health workers could provide the best efficiency for behavior change [23]. This current study has revealed that half of the participants consider COVID-19 a deadly disease, label themselves at risk of COVID-19, and are worried about COVID-19. Meanwhile, approximately 70% of the respondents have performed preventive measures to prevent COVID-19 and consider it a serious and dangerous disease; thus, most people feel responsible in their lives to follow the steps to reduce the risk of transmission [24].
A strong correlation is also found in self-justification by establishing ways to change the risk of transmission [obtaining remedies]. It means that nurses who have positive perceptions or acknowledgments about their ability to prevent infection tend to behave more positively than those who have negative perceptions [25]. Moreover, nurses should learn about COVID-19, prevention, and transmission mechanisms as self-copping strategies to reduce stress [26].
Moreover, nurses’ commitment to infection prevention and control practices is positively correlated with their information-seeking actions. The nurses’ decision to behave safely at work is determined by their self-commitment because low commitment tends to have a negative impact on their service quality, job satisfaction, and work safety; thus, low commitment is not significant for controlling the risk of disease transmission [27]. Commitment is a decision-making stage that could produce several outcomes, such as making firm decisions to overcome problems. It is believed that when an individual thinks about the problem and its consequences, the commitment to implement risk reduction measures will be higher [28].
The commitment to infection management aims to improve care by early detecting signs and symptoms, using standard diagnostic criteria, implementing adequate preventive measures, and establishing systems for surveillance and control. Similar actions could help nurses achieve desired outcomes, such as patient safety, worker welfare, reduced risk of infection, and improved organizational performance [29, 30]. This result is in line with those of several other studies that investigate the correlation of organizational factors, commitment, and different factors [31]. Organizational support, such as sufficient personnel, a sufficient number of PPE, reasonable working hours, and psychological support systems, are the key factors [32, 33].
Measures to control and prevent infectious diseases should be implemented. Interactions between humans and pathogens could be facilitated or avoided depending on the presence or absence of infectious disease control and prevention measures [34, 35]. Standard precautions are a key component of healthcare worker safety and should be implemented at every encounter with every patient to protect all healthcare workers and patients in all healthcare settings [36]. Standard precautions refer to minimum infection prevention practices applicable to patient care [37]. Centers for Disease Control and Prevention (CDC) recommends several points: implementing the standard, using contact and air precautions, and designing education and training programs [38]. Maintaining the quality of nursing of the multidisciplinary primary health care team potentially addresses many health and social problems; this maintenance could reduce secondary morbidity and mortality and improve health [39]. It has been shown that adherence to infection control measures reduces transmission [40].
CONCLUSION
Nurses’ compliance in taking measures to reduce the risk of transmission of COVID-19 could not be separated from their self-labeling and commitment; the stronger their labeling and self-commitment, the better and more appropriate their actions in reducing risk.
LIMITATIONS
This study used a relatively small sample size, so it cannot be generalized out of Indonesia. In addition, investigation on the determinants of infection prevention and control practices was limited to internal factors in nurses. Future research on external factors is needed to obtain comprehensive results.
IMPLICATION
For nurse managers, these findings can be used to strengthen infection prevention and transmission practices in hospitals. Interventions to strengthen nurses’ commitment and self-awareness as individuals at risk can be an option in optimizing infection prevention and transmission practices.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This trial obtained ethical approval from the institutional review boards of Nani Hasanuddin Institute (0169/STIKES-NH/KEPK/VI/2021).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for experimentation (institutional and national) and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
The purpose of the study was explained to the participants and the consent form was obtained. Confidentiality, voluntary participation, and anonymity were maintained.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
Data are available by contacting the corresponding author [S.S] with reasonable reasons.
FUNDING
None.
CONFLICT OF INTERESTS
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We thank all the nurses who participated in this study for their contribution and dedication.


