All published articles of this journal are available on ScienceDirect.
Health Tourism Prevalence among Western Balkans Citizens During the COVID-19 Pandemic Period
Abstract
Background:
This study seeks to evaluate the prevalence of and the association between receiving medical care abroad and the level of trust that citizens from the Western Balkans—Albania, Bosnia and Herzegovina, Kosovo and Montenegro—have in their healthcare systems.
Methods:
The study is cross-sectional and was carried out during three months (July 25-October 30, 2021) through a self-reported questionnaire administered through the Google Forms platform. The study included approximately two-thousand citizens (N=2,356) aged eighteen (18) to seventy (70).
Results:
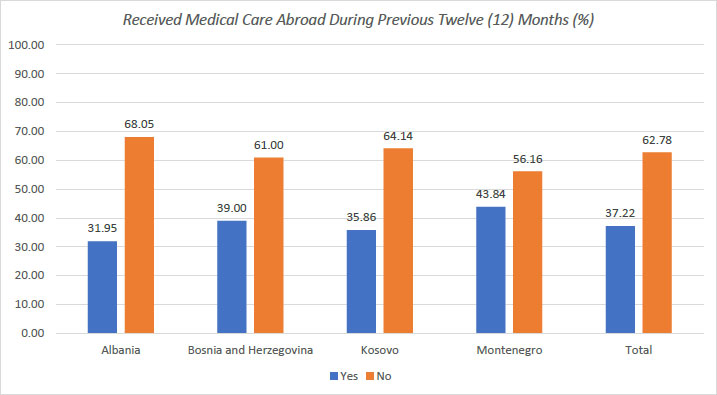
More than one-third (37.2%) of respondents stated that they or a relative had received healthcare services abroad during the last twelve (12) months. Citizens of Montenegro had the highest prevalence of receiving healthcare services abroad at 43.8%, followed by those from Bosnia and Herzegovina at 39%. No statistically significant difference was found in the level of trust in the healthcare system in the country between those who received healthcare services abroad (4.41±2.88) (out of 10) and those who did not (4.48±2.81) (t= -0.587, p=0.557).
Conclusion:
We ultimately conclude that more than one-third of the participants in our study have traveled abroad for healthcare purposes, with females, those living in urban areas, and those who have previously had a negative healthcare experience in their home country all being more likely to rely on health tourism.
1. INTRODUCTION
The ease of travel today has encouraged people to move more frequently and for a greater variety of reasons, including the pursuit of relaxation, health, fitness, and well-being [1]. Sandberg (2017) describes the medical tourism industry as a phenomenon concerning the number of resources that countries around the world are investing in attracting medical tourists by offering high-quality, low-cost, specialized care with concierge and hospitality benefits [2]. Many definitions exist for health tourism. For instance, Carrera and Bridges (2006) identified health tourism as one’s organized travel outside his or her local environment for the maintenance, enhancement, or restoration of his or her well-being in mind and body [3]. It covers medical tourism, which is defined as planned travel outside of one's usual scope of medical care for the purpose of enhancing or restoring one's health through medical treatment [4]. As contrasted with Smith and Puczkó (2015), who describe health tourism as “those forms of travel that place a primary emphasis on physical health but also enhance mental and spiritual well-being and boost people's ability to meet their own needs and function better in their environment and society” [5]. Medical, wellness, and spa tourism are all included in the subsector of health tourism that comprises tourism more broadly, while people who travel specifically for medical treatment are said to be engaging in medical tourism. For the purpose of preserving or improving their own health and well-being, people engage in wellness tourism. Spa travel focuses on preventative and/or curative physical healing, relaxation, or beautification [6]. Additionally, according to the United Nations World Tourism Organization, tourism can contribute to health and well-being in a variety of indirect ways, including strategic reinvestment of tourism-generated income in health-related services [7, 8].
On the basis of health tourism, promotion, and the development of a favorable image, several nations in this field are forging their identities as touristic places and offering medical packages for foreigners [2, 9, 10]. According to the World Travel and Tourism Council, international spending on medical tourism services increased as a percentage of total international visitor spending from 0.6% in 2000 to 1.2% in 2017, totaling nearly US$11 billion in 2017 [11]. It is well known that citizens of the Balkan countries often travel abroad to receive medical care. For instance, the citizens of Kosovo spend approximately 150 million Euros per year on medical treatment in other countries [12]. In less than a year from the beginning of the COVID-19 pandemic, Albanians have paid more than 6.7 million euros for medical travel by air ambulance [13]. Additionally, medical treatment outside of Montenegro cost 4.3 million Euros in 2018, accounting for more than two percent (2%) of total healthcare expenditures [14].
The medical tourism industry will experience a significant lag in its projected expansion as a result of the COVID-19 pandemic [15]. However, the COVID-19 pandemic has caused the movement of people and goods around the world to take on a new dimension by adapting to the circumstances and decisions of different governments to prevent the spread of SARS-COV-2 infection. For countries that have high transmission and mortality rates, the COVID-19 pandemic may also damage their reputations as attractive tourist destinations [16]. Golets et al. stated in their research that perceptions of the severity of the COVID-19 pandemic, the perceived risk of infection, and the estimated duration of the pandemic are important predictors of Brazilians' intentions to travel throughout the pandemic's 2020–2021 period [17]. The COVID-19 pandemic, on the other hand, is driving the expansion of telemediated service delivery, particularly in the diagnostic and rehabilitative phases of the care continuum for patients who may travel, leaving behind many of the traditional models [18].
The purpose of this study is to assess the prevalence and relationship between receiving medical care abroad and citizens' trust in their healthcare systems in the Western Balkans (Albania, Bosnia and Herzegovina, Kosovo, and Montenegro). The analysis in this paper adds to previous knowledge by revealing that, despite difficulties during the pandemic, and governmental restrictions on travel meant to reduce the spread of infection, Balkan citizens were able to cross the border and seek healthcare abroad.
2. MATERIALS AND METHODS
The cross-sectional study was carried out over three months (July 25-October 30, 2021) through a self-reported questionnaire administered through the Google Forms platform. The study included approximately two-thousand citizens (N = 2,356) aged eighteen (18) to seventy (70) from Albania, Bosnia and Herzegovina, Kosovo, and Montenegro. According to the 2011 census, there were over 8700000 people living in Albania, Bosnia and Herzegovina, Kosovo, and Montenegro, with roughly seventy-five percent (75%) of them being above the age of eighteen (18). Based on a sample size calculation with a 99% confidence level and a population proportion response of 50%, it was determined that the sample size of 2356 participants had an error margin of 2.66%. Furthermore, the study adhered strictly to the provisions of the Helsinki Declaration on Research on Human Participants, and all subjects provided informed consent electronically prior to participation. The study protocol was approved by the ethical commission of Heimerer College (Protocol no: 619/22). The questionnaire was originally written in Albanian, and an identical version was translated using the double-forward-backward approach into Montenegrin and Bosnian for use in the respective countries [19, 20]. The questionnaire's reliability was assessed, and its internal consistency was found to be acceptable [19]. In contrast to the dichotomous (Yes or No) response to the question about receiving medical care abroad, respondents were asked to rate their level of trust in the healthcare system on a scale of 1 to 10, with 1 representing “no trust at all” and 10 representing “a lot of trusts”. A detailed methodology of the study is explained elsewhere [19].
The Statistical Package for the Social Sciences was used to analyze the data (SPSS version 21.0) [21]. Frequencies and percentages (%) were used to represent count data. The mean±SD (standard deviation) is used to summarize continuous variables. Variables were analyzed using the independent samples t-test, Chi-square test, and linear regression (β and 95%CI). A p-value of 0.05 was considered statistically significant for all statistical tests.
3. RESULTS
Sixty-seven percent (n=1594) of the participants in the study were female, 54.4% had completed university education, 63% were married, 70.8% had an average income, and 79.6% lived in an urban residence. 37.2% of respondents stated that they or a relative of theirs had received healthcare services abroad during the last twelve (12) months. Citizens of Montenegro had the highest prevalence of receiving services abroad with 43.8%, followed by those from Bosnia and Herzegovina with 39% (p<0.05) (Fig. 1 and Table 1).
| - | Received Medical Care Abroad During Previous Twelve (12) Months | ||||
|---|---|---|---|---|---|
| - | - |
Total N (%) |
Yes n (%) |
No n (%) |
- |
| Country | Albania Bosnia and Herzegovina Kosovo Montenegro |
601 (25.5%) 700 (29.7%) 633 (26.9%) 422 (17.9%) |
192 (8.1) 273 (11.6) 227 (9.6) 185 (7.9) |
409 (17.4) 427 (18.1) 406 (17.2) 237 (10.10) |
x2=16.513 p = 0.001 |
| Gender | Male Female |
762 (32.3%) 1594 (67.7%) |
314 (13.3) 563 (23.9) |
448 (19.0) 1031 (43.8) |
x2=7.647 p = 0.006 |
|
Age Range (in Years) |
18-30 31 - 40 41 - 50 51 - 60 61 - 70 |
702 (29.8%) 641 (27.2%) 536 (22.8%) 341 (14.5%) 136 (5.8%) |
254 (10.8) 256 (10.9) 182 (7.7) 133 (5.6) 52 (2.2) |
448 (19.0) 385 (16.3) 354 (15.0) 208 (8.8) 84 (3.6) |
x2=5.318 p = 0.256 |
| Education | Secondary School University MSc or PhD |
642 (27.2%) 1282 (54.4%) 432 (18.3%) |
227 (9.6) 479 (20.3) 171 (7.3) |
415 (17.6) 803 (34.1) 261 (11.1) |
x2=1.996 p = 0.369 |
| Marital Status | Single Married Divorced Widowed |
688 (29.2%) 1484 (63.0%) 63 (2.7%) 121 (5.1%) |
253 (10.7) 555 (23.6) 23 (1.0) 46 (2.0) |
435 (18.5) 929 (39.4) 40 (1.7) 75 (3.2) |
x2=0.126 p = 0.989 |
| Income | Low Medium Good |
334 (14.2%) 1668 (70.8%) 354 (15.0%) |
113 (4.8) 618 (26.2) 146 (6.2) |
221 (9.4) 1050 (44.6) 208 (8.8) |
x2=4.113 p = 0.128 |
| Living Setting | Urban Rural |
1875 (79.6%) 481 (20.4%) |
717 (30.4) 160 (6.8) |
1158 (49.2) 321 (13.6) |
x2=4.056 p = 0.044 |
| Negative Experience in Healthcare services in their Country | Yes No |
1440 (61.1) 916 (38.9) |
556 (23.9) 313 (13.3) |
876 (37.2) 603 (25.6) |
x2=5.981 p = 0.014 |
| - | Received Medical Care Abroad During Previous Twelve (12) Months | ||
|---|---|---|---|
| - | Yes Mean±SD |
No Mean±SD |
- |
| Albania | 4.25 ± 2.67 | 4.28 ± 2.66 | t= 0.956 p=0.903 |
| Bosnia and Herzegovina | 3.78 ± 2.70 | 3.51 ± 2.44 | t= 0.072 p=0.173 |
| Kosovo | 5.61 ± 2.87 | 5.80 ± 2.75 | t= - 0.842 p=0.400 |
| Montenegro | 4.04 ± 2.93 | 4.32 ± 2.93 | t= 0.860 p=0.336 |
| Total | 4.41 ± 2.88 | 4.48 ± 2.81 | t= -0.587 p=0.557 |
No significant statistical difference was found in the prevalence of one’s receiving healthcare services abroad and his or her age group, education, marital status, and/or economic status (p>0.05). Citizens living in urban environments had a higher prevalence of receiving services outside the country compared with those living in rural settings (p<0.05); similarly, women had a higher predilection for receiving healthcare services outside the country compared to their male counterparts. No significant statistical difference was found in the level of trust in the healthcare system in the country between those who received healthcare services abroad (4.41 ± 2.88) (out of 10) and those who did not (4.48 ± 2.81) (t= -0.587, p = 0.557) (Table 2). In the logistic regression analysis, it was determined that the likelihood of receiving healthcare services abroad increases by approximately twenty-nine percent (29%) among females (Exp (B): 1.294, 95% CI: 1.083-1.546, p=0.004), twenty-five percent (25%) among those living in urban environments (Exp (B): 1.258, 95% CI: 1.017-1.555, p=0.034), and twenty-three percent (23%) among those who had a negative healthcare experience in their own country at some point during the previous year (Exp (B): 1.230, 95% CI: 1.034-1.463, p=0.019).
4. DISCUSSION
Our primary findings indicate that nearly one-third of the research participants claim to have received medical care overseas during the previous twelve (12) months, either for themselves or a family member. The highest prevalence of health services abroad last year was found among citizens of Montenegro (43.8%) and the lowest among citizens of Albania (31.9%). This time frame coincides with the COVID-19 Pandemic, i.e. when restrictions on citizen mobility were enforced to prevent the spread of the Sars-Cov-2 infection.
The study conducted during COVID-19 by Pu, Du, Zhang and Qiu, discovered that perceived behavior control acted as a moderator between perceived usefulness and health tourism intention [22]. During the COVID-19 Pandemic, the lack of trust had a large impact on tourist behavior, and it is believed that it will take a long time for that trust to return to healthcare institutions [23]. Additionally, according to Nazneen, Hong, and Ud Din's study, tourists believe that COVID-19 has made traveling unsafe, increased concerns about the hygiene and safety of public transportation, tourist spots, and hotels, and reduced tourists' trip plans, particularly to large, congested cities [24].
According to the findings from Singh and Gill (2011), the top three considerations before traveling abroad are “competent doctors,” “high quality medical treatment facility,” and “rapid medical treatment when needed” [25]. Gan and Frederick's (2013) study found that a significant number of un(der)insured Americans sought medical care outside the USA in countries with significantly lower labor costs and correspondingly lower medical procedure costs [26]. Furthermore, Sandberg (2017) indicates in his study that medical tourism provides access to low-cost, high-quality care without lengthy waiting periods for people who require surgery or other treatments but may have to pay for or wait for them [2].
The top three countries in 2020-2021, according to the Medical Tourism Index (MTI), which ranks citizens' impressions based on 41 factors and offers insight into how travelers perceive particular locations, are Canada, Singapore, and Spain [27]. An important factor in defining the degree of medical service at the destination for medical tourism will be the medical response system to reduce the pandemic risk associated with international travel [28]. In their study, Mosazadeh et al. offer two strategic approaches, a country-based and a hospital-/clinic-based strategy, that can transform a risky COVID-19 destination into a safe COVID-19 destination for international medical tourists [29].
According to a report released by the Dubai Health Authority (DHA) during the ongoing Arab Travel Market in Dubai, Dubai received 630,000 international health tourists in 2021. Despite the global COVID-19 pandemic, international patients spent close to AED 730 million ($198 million) in the previous year [30]. According to a recent study, up to 44 million people will travel across borders each year for healthcare, and developing healthcare markets may capitalize on this trend to attract lucrative patients from developed nations. This would increase the global medical tourism market to more than $180 billion in the next three years [31].
While the majority of Balkan countries contain thermal and mineral waters that have historically been utilized for treatment and are frequently now used as the foundation for health and wellness travel. Although only a very small portion of the accessible waters are actually used for health tourism, this is frequently the case. In addition to a healing climate, several nations also have therapeutic mud or gas [32].
Our findings are limited by our search techniques, which include the use of an online questionnaire as a data collection tool and the lack of a qualitative analytic design approach. The collection of data online is justified during this period of the pandemic when the risk of COVID-19 infection spreading through direct contact with study participants is estimated to be high. Another limitation of our study is the lack of data comparison with the pre-pandemic period in Western Balkans. As a result, we cannot estimate the pandemic's impact. Nonetheless, repeating the study at regular intervals can help in tracking the trend of health tourism among Western Balkan citizens.
CONCLUSION
The measures taken by the governments of the Balkan countries to limit the movement of people and goods in order to prevent the COVID-19 pandemic spread have not largely stopped the movement of people seeking healthcare services abroad. Citizens have discovered, in one form or another, the ability to receive health care services at their request outside of the country, regardless of the economic costs. We ultimately conclude that more than one-third of the participants in our study have traveled abroad for healthcare purposes, with females, those living in urban areas, and those who have previously had a negative healthcare experience in their home country all being more likely to rely on health tourism.
AUTHORS’ CONTRIBUTIONS
Concept and design: Drita Maljichi, Bernard Tahirbegolli, Driton Maljichi, Iliriana Alloqi Tahirbegolli, Ahmed Kulanić, Irida Agolli Nasufi. Acquisition, analysis or interpretation of data: Drita Maljichi, Bernard Tahirbegolli, Driton Maljichi, Iliriana Alloqi Tahirbegolli, Ahmed Kulanić, Irida Agolli Nasufi, Milica Kovač-Orlandić. Drafting of the manuscript: Drita Maljichi, Troy E. Spier, Iliriana Alloqi Tahirbegolli, Bernard Tahirbegolli, Ahmed Kulanić, Milica Kovač-Orlandić. Critical revision of the manuscript for important intellectual content: Driton Maljichi, Troy E. Spier, Bernard Tahirbegolli, Milica Kovač-Orlandić. Statistical analysis: Irida Agolli Nasufi and Bernard Tahirbegolli. Administrative, technical or material support: Driton Maljichi, Troy E. Spier, Drita Maljichi, Iliriana Alloqi Tahirbegolli, Ahmed Kulanić, Irida Agolli Nasufi, Milica Kovač-Orlandić. Supervision: Drita Maljichi, Bernard Tahirbegolli, and Driton Maljichi.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol was approved by the ethical commission of Heimerer College (Protocol no.: 619/22).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants of this study.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author [B.T] upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflicts of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to thank the following individuals for their support while conducting the research for this article: Mrs. Merva Kelmendi (Heimerer College), Mrs. Klara Cahani (Heimerer College), Mrs. Leonora Paice (Norfolk County Council), Mrs. Besarta Taganovic (Heimerer College), Mr. Gezim Qerimi (University of Prishtina) and Mrs. Milka Todorova (Institute for Sociological, Political and Juridical Research).


