All published articles of this journal are available on ScienceDirect.
Prospective Health Professionals’ Knowledge, Awareness, Attitude, and Practice Concerning MRI Safety
Abstract
Background:
Magnetic resonance imaging (MRI) has been applied widely in clinical practices to acquire cross-sectional images of the body. Although MRI uses non-ionizing radiation, there are serious bioeffect hazards that can be associated with the use of strong electromagnetic fields (EMFs).
Purpose:
This study aims to explore prospective health professionals’ knowledge, awareness, attitude, and practice levels concerning MRI safety.
Methods:
This cross-sectional study was conducted on medical and allied medical students at Taibah University using an online questionnaire survey. Data were reported using descriptive statistics and Chi-squared tests to determine the differences based on selected demographic variables.
Results:
120 Prospective healthcare professionals completed the questionnaire. In the knowledge domain, 50% of participants agreed that patients with tattoos could be scanned. In the awareness domain, roughly 40% of participants reported being unaware of the new compatible pacemakers. In the attitude domain, less than 50% of participants were interested in attending MRI safety seminars. Only one significant borderline finding was identified concerning the awareness level between genders (P=0.053).
Conclusion:
This study showed that the knowledge level of MRI safety among prospective health professionals is within the acceptable level and also showed a high level of awareness and a moderately positive attitude regarding MRI safety. The results of this study are helpful for higher education institutions which will enable them to modify their curriculum content to fill the knowledge gaps in this area.
1. INTRODUCTION
Magnetic resonance imaging (MRI) is utilized widely in clinical practices to acquire cross-sectional imaging of different body parts. Although MRI uses non-ionizing radiation, there are serious bioeffect hazards that can be associated with the use of strong electromagnetic fields (EMFs). MRI safety-related events (e.g., projectile, equipment labeling, unauthorized access, burn, noise complaint, unable to confirm safety, implant /device-related issue, faulty oxygen monitor) were reported in 7.5% of the total number of incident reports submitted within a UK independent sector provider of diagnostic services. The MR safety-related incidence report rate was relatively low (0.05%) [1].
The magnetic field is always (ON) even when the scanner is not in use; the field is invisible and can turn ordinary objects into unsafe projectiles, which can cause equipment damage, personal injuries, and even death [2]. Therefore, MRI safety is a critical consideration that every person entering the EMF should pay attention to this issue. Pre-scanning screening assessment is a critical step that is performed for every person who is authorized to enter the EMF. Non-MRI personnel and patients must be screened before entering the MRI scanner room. Individuals who frequently visit the MRI unit to support or transport patients should have a minimum level of knowledge in MRI safety to avoid potential dangers in the magnetic environment, such as projectile incidents.
Implementing comprehensive MR safety for medical students is essential to ensure that medical students gain a basic understanding of MR principles and safety considerations [3]. Referring physicians who recognize the principles of MRI safety can support and contribute to MRI safety screening since they know the patient’s medical history better than radiologists or technologists, who will only meet a patient briefly during screening and preparation for an exam [3]. Other healthcare professions, such as nursing, provide patient care during MRI examinations. Alghamdi et al. (2021) reported that nurses had limited knowledge regarding MRI and moderate adherence to MRI safety procedures [4]. Therefore, including learning modules on MR safety for facility employees is essential to prevent fatal incidents induced by incorrect practices in the MR environment [5].
Non-MR healthcare providers are essential in completing MR imaging procedures with MR staff in a safe environment. To deliver safe MR imaging services, there is a minimum level of knowledge that MR and non-MR healthcare providers must achieve to prevent devastating consequences such as injuries and, in some cases, death. This study aims to determine prospective health professionals’ knowledge, awareness, attitude, and practice in MRI safety. The results of this study can provide valuable information to higher education institutions (e.g., universities) about the knowledge level of prospective healthcare professionals regarding MR safety and highlight the modifications in curriculum content that are required to fill the gaps of knowledge in this area.
2. MATERIALS AND METHODS
The methodological orientation of this study is phenomenology which aims to investigate the MRI safety knowledge and practice of medical and allied medical students at Taibah University, Saudi Arabia, by utilizing an online questionnaire survey.
2.1. Ethical Considerations
This study has obtained ethical approval from the Scientific Research and Ethics Committee of the Applied Medical Sciences College (Ref. 2021/112/303/DRD). All the participants were recruited voluntarily who received the research aim and objectives and signed the consent form (electronically) to participate in this study.
2.2. Participants
Participants were approached through Taibah University’s advertisements site and social media applications. This study’s population was split into age groups: 18–20, 21–23, 24–26, and 27 years and older. The population covers both genders (female and male), all the medical colleges affiliated with Taibah University (College of Medicine, College of Dentistry, College of Nursing, College of Pharmacy, College of Applied Medical Sciences, and College of Medical Rehabilitation Sciences) and all academic years from the first year to the internship year (Table 1). The inclusion criterion of this study was students from the College of Medicine, College of Dentistry, College of Pharmacy, College of Medical Rehabilitation Sciences, and College of Applied Medical Sciences at Taibah University, Saudi Arabia. The exclusion criteria of this study were as follows: academic staff, technicians, administrators, students from other colleges or students who do not attend Taibah University, and students from the Department of Diagnostic Radiology Technology. There was no presence of non-participants present beside the participants and researchers in this conducted research.
| Study Variables | |
| Age groups | 1. 18–20 |
| 2. 21–23 | |
| 3. 24–26 | |
| 4. 27 and older | |
| Gender | Male or female |
| Affiliation | 1. College of Medicine |
| 2. College of Dentistry | |
| 3. College of Nursing | |
| 4. College of Pharmacy | |
| 5. College of Applied Medical Sciences | |
| 6. College of Medical Rehabilitation Sciences | |
| Academic Year | 1st year / 2nd year / 3rd year / 4th year / 5th year / 6th year / Internship year |
| - | Domains | Questions | |
|---|---|---|---|
| 1.0 | Knowledge | K1.1 | To what extent do you agree or disagree with using MRI to scan patients with a pacemaker (an electrical device implanted into their chest to control their heartbeat)? |
| K1.2 | To what extent do you agree or disagree with using MRI to scan pregnant patients? | ||
| K1.3 | To what extent do you agree or disagree with using MRI to scan patients with metallic objects? | ||
| K1.4 | To what extent do you agree or disagree with using MRI to screen patients who have tattoos? | ||
| K1.5 | To what extent do you agree or disagree that the MRI magnet is always kept ON? | ||
| 2.0 | Awareness | AW2.1 | Are you aware of the biohazard effects that might be caused when using a strong magnetic field in hospitals? |
| AW2.2 | Are you aware of the MRI safety zones in hospitals? | ||
| AW2.3 | Are you aware that the new pacemaker may be compatible with the MRI machine? | ||
| AW2.4 | Are you aware that some patients might get claustrophobic from the MRI scanner? | ||
| 3.0 | Attitude | AT3.1 | To what extent do you agree or disagree that your specialty may require you to attend MRI safety seminars to expand your knowledge of MRI safety? |
| AT3.2 | Within your specialty, to what extent do you agree or disagree that you may have to attend MRI safety training and emergency procedures in an MRI suite? | ||
| AT3.3 | Within your specialty, to what extent do you agree or disagree that your major has an influential role in the MRI department? | ||
| 4.0 | Practice | P4.1 | To what extent do you agree or disagree that all MRI scan rooms should contain an oxygen monitor that sounds an alarm if the oxygen falls below a certain level? |
| P4.2 | In your opinion, to what extent do you agree or disagree that using headphones for hearing acuity protection is vital during MRI examinations? | ||
The study population of about 1000 Students (a total number of medical and allied health students in Taibah University), with a margin of error of 5% and a level of confidence of 95% in sampling. After performing the sample size calculation, the target sample size is 110 students that are needed, the real value is within ±/- 5% of the measured/surveyed.
2.3. Study Design
In this cross-sectional study, the purpose of the questionnaire was to assess the knowledge and awareness of students at medical colleges at Taibah University regarding safety in magnetic resonance imaging. It was clarified to the students that participation was voluntary and that any information and data collected for this scientific research would be confidential. The questionnaire was divided into two main parts: the first part was designed to collect demographic information, which included age, gender, collegiate affiliation, and academic year, while the second part covered the four main domains that the research was investigating – knowledge (K), awareness (AW), attitude (AT) and practice (P) (Table 2). All questions were from the closed-question category and were multiple choice, with respondents able to select only one response for each answer. The Visual analog scale (VAS) was applied to measure subjective and behavior experiences regarding MRI safety.
2.4. Data Collection
The colleges' representatives distributed the online questionnaire during the academic year. Responses began to be collected on 31 January 2022 and were closed on 4 April 2022. A pilot survey was conducted on five prospective medical and allied medical students at Taibah University to establish the survey instrument's validity, evaluate the questionnaire clarity and improve the study design before starting the research study. Minor corrections were made to the questionnaire based on the pilot feedback.
2.5. Data Analysis
The raw data were exported from the Google Forms and converted into Microsoft Excel and Jeffreys’ Amazing Statistics Program (JASP) formats. Data were reported using descriptive statistics and Chi-squared tests to determine the differences based on selected demographic variables. Data analysis for this study included the demographic characteristics of the participants concerning their collegiate affiliation, gender, age group, and academic year, which were obtained through descriptive analysis using frequencies and percentages. Statistical tests were conducted at a significance level of 0.05.
3. RESULTS
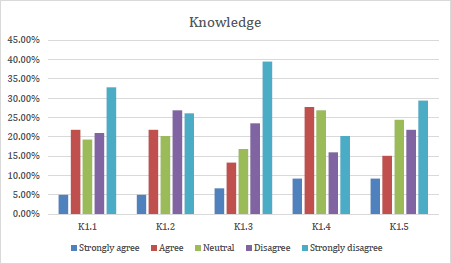
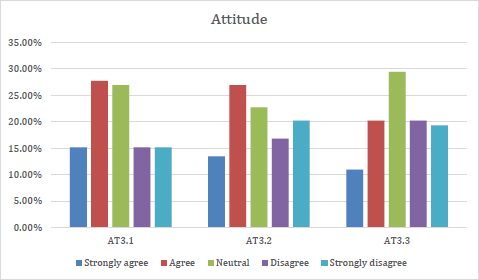
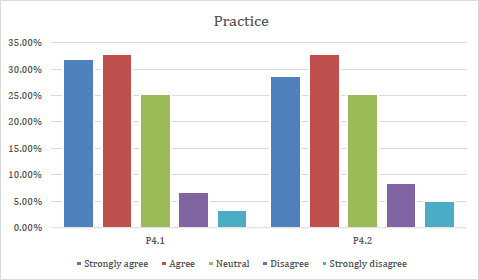
A total of 120 participants agreed to participate and completed the questionnaire in this study. The participants’ demographic information is presented in Table 3. Data were analyzed to determine the level of knowledge and awareness among medical students about MRI safety, and the results are listed in Tables 4 and 5 and illustrated in Figs. (1 to 4).
In the knowledge domain, an equal number of participants agreed and disagreed with K1.4, while more respondents disagreed with questions K1.1, K1.2, K1.3, and K1.5. For question K1.1, the highest percentage was for ‘strongly disagree’ (33.3%) and the lowest for ‘strongly agree’ (5%). For K1.2, the highest percentage was for ‘disagree’ and ‘strongly disagree’ (26.7%), while the lowest was for ‘strongly agree’ (5%). The highest percentage for K1.3 was for ‘strongly disagree’ (40%), and the lowest was for ‘strongly agree’ (6.7%). For K1.4, there were two equal groups: 44 people (36.7%) responded 'strongly agree' and 'agree', and the same number responded 'strongly disagree' and 'disagree', while the remaining 32 (26.7%) responded 'neutral'. For K1.5, 24.2% of respondents were ‘neutral,' and the largest proportion (30%) answered ‘strongly disagree’.
| Characteristics | Subgroups | Frequency | Percentage |
|---|---|---|---|
| Age | 18–20 | 32 | 26.7% |
| 21–23 | 55 | 45.2% | |
| 24–26 | 17 | 14.2% | |
| 27 and older | 16 | 13.3% | |
| Total | 120 | 100% | |
| Gender | Male | 72 | 60% |
| Female | 48 | 40% | |
| Total | 120 | 100% | |
| Affiliation | College of Medicine | 27 | 22.5% |
| College of Dentistry | 9 | 7.5% | |
| College of Nursing | 25 | 20.8% | |
| College of Pharmacy | 11 | 9.2% | |
| College of Applied Medical Sciences | 35 | 29.2% | |
| College of Medical Rehabilitation Sciences | 13 | 10.8% | |
| Total | 120 | 100% | |
| Academic year | First-year | 23 | 19.2% |
| Second year | 24 | 20% | |
| Third year | 23 | 19.2% | |
| Fourth-year | 21 | 17.5% | |
| Fifth year | 11 | 9.2% | |
| Sixth year | 5 | 4.2% | |
| Internship year | 13 | 10.8% | |
| Total | 120 | 100% |
| - | Domain | Question | Visual Analogue Scale (VAS) | ||||
|---|---|---|---|---|---|---|---|
| 1.0 | Knowledge | Strongly agree | Agree | Neutral | Disagree | Strongly disagree | |
| K1.1 | 6 (5%) | 26 (21.7%) | 23 (19.2%) | 25 (20.8%) | 40 (33.3%) | ||
| K1.2 | 6 (5%) | 26 (21.7%) | 24 (20%) | 32 (26.7%) | 32 (26.7%) | ||
| K1.3 | 8 (6.7%) | 16 (13.3%) | 20 (16.7%) | 28 (23.3%) | 48 (40%) | ||
| K1.4 | 11 (9.2%) | 33 (27.5%) | 32 (26.7%) | 19 (15.8%) | 25 (20.8%) | ||
| K1.5 | 11 (9.2%) | 18 (15%) | 29 (24.2%) | 26 (21.7%) | 36 (30%) | ||
| 2.0 | Awareness | Extremely aware | Very aware | Moderately aware | Slightly aware | Not aware at all | |
| AW2.1 | 35 (29.2%) | 27 (22.5%) | 35 (29.2%) | 15 (12.5%) | 8 (6.7%) | ||
| AW2.2 | 36 (30%) | 31 (25.8%) | 26 (21.7%) | 19 (15.8%) | 8 (6.7%) | ||
| AW2.3 | 26 (21.7%) | 23 (19.2%) | 18 (15%) | 17 (14.2%) | 36 (30%) | ||
| AW2.4 | 46 (38.3%) | 31 (25.8%) | 21 (17.5%) | 14 (11.7%) | 8 (6.7%) | ||
| 3.0 | Attitude | Strongly agree | Agree | Neutral | Disagree | Strongly disagree | |
| AT3.1 | 18 (15%) | 33 (27.5%) | 32 (26.7%) | 18 (15%) | 19 (15.8%) | ||
| AT3.2 | 16 (13.3%) | 32 (26.7%) | 27 (22.5%) | 20 (16.7%) | 25 (20.8%) | ||
| AT3.3 | 13 (10.8%) | 24 (20%) | 35 (29.2%) | 24 (20%) | 24 (20%) | ||
| 4.0 | Practice | Strongly agree | Agree | Neutral | Disagree | Strongly disagree | |
| P4.1 | 39 (32.5%) | 39 (32.5%) | 30 (25%) | 8 (6.7%) | 4 (3.3%) | ||
| P4.2 | 35 (29.2%) | 39 (32.5%) | 30 (25%) | 16 (8.3%) | 6 (5%) | ||
| - | Domain | Question | Age | Gender | Affiliation | Academic Year |
|---|---|---|---|---|---|---|
| 1.0 | Knowledge | K1.1 | 0.819 | 0.473 | 0.073 | 0.067 |
| K1.2 | 0.827 | 0.185 | 0.667 | 0.076 | ||
| K1.3 | 0.736 | 0.319 | 0.429 | 0.078 | ||
| K1.4 | 0.955 | 0.888 | 0.109 | 0.963 | ||
| K1.5 | 0.545 | 0.077 | 0.234 | 0.675 | ||
| 2.0 | Awareness | AW2.1 | 0.895 | 0.053* | 0.636 | 0.482 |
| AW2.2 | 0.862 | 0.357 | 0.089 | 0.344 | ||
| AW2.3 | 0.384 | 0.571 | 0.076 | 0.188 | ||
| AW2.4 | 0.789 | 0.847 | 0.845 | 0.515 | ||
| 3.0 | Attitude | AT3.1 | 0.132 | 0.435 | 0.483 | 0.666 |
| AT3.2 | 0.329 | 0.307 | 0.402 | 0.089 | ||
| AT3.3 | 0.537 | 0.251 | 0.238 | 0.460 | ||
| 4.0 | Practice | P4.1 | 0.591 | 0.305 | 0.624 | 0.311 |
| P4.2 | 0.516 | 0.716 | 0.856 | 0.335 |
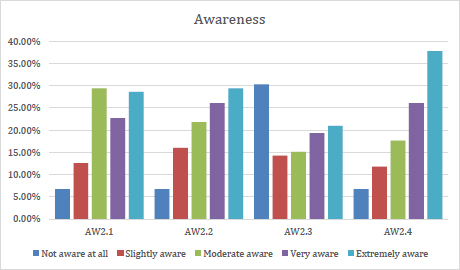
Participants gave broad responses across the first two questions in the awareness domain. AW2.1 had two equally large groups: 'extremely aware' (29.2%) and 'moderately aware' (29.2%). On the other hand, only eight respondents (6.7%, a minor proportion for each question) showed no awareness of AW2.1 and AW2.2. On the third question (AW2.3), the highest proportion of responses (30%) was for 'not aware at all' (30%), while the second-largest group (21.7%) were 'extremely aware' – in other words, at the opposite end of the scale. In the final question of the awareness domain (AW2.4), the largest proportion of participants (38.3%) showed the highest awareness level.
In the attitude domain, more participants agreed than disagreed. On the first question, AT3.1, the largest proportion of participants chose either the ‘agree’ option (27.5%) or the ‘neutral’ option (26.7%). On the second question (AT3.2), participants gave similar responses to AT2.1; again, the largest proportions chose either ‘agree’ (26.7%) or ‘neutral’ (22.5%). On the other hand, for the final question of the attitude domain (AT3.3), most of the participants were ‘neutral’ (29.2%), and the lowest proportion (10.8%) selected ‘strongly agree’.
Participants showed the biggest agreement (roughly 62.5%) on the practice domain compared to the other three domains. Most participants were either 'agree' or 'neutral' in the practice domain. A quarter of participants (25%) were 'neutral' for both practice domain questions, while only a small proportion disagreed or strongly disagreed (10% for P4.1 and 13.3% for P4.2).
The Chi-squared test (Table 5) revealed no significant differences between the level of agreement based on the age, affiliation, gender, and academic year of participants. Only one significant borderline finding was identified about the awareness level (AW2.1) between genders (P=0.053).
4. DISCUSSION
This study aimed to determine the knowledge, awareness, attitude, and practice level of prospective healthcare professionals regarding MRI safety. Additionally, the study investigated the influence of age, gender, affiliation, and academic year on the knowledge, awareness, attitude, and practice level of prospective healthcare professionals regarding MRI safety. To the best of the authors’ knowledge, this is the first study that examines the knowledge, awareness, attitude, and practice level of prospective healthcare professionals regarding MRI safety in the western region of Saudi Arabia.
Participants were asked about pacemakers, pregnancy, metallic objects, tattoos, and the magnetic field in the knowledge domain. This study found that more than 50% of participants disagreed that pregnant patients and patients with a pacemaker or a metallic object should be scanned. More than 50% of participants agreed that patients with tattoos could be scanned. No significant differences were found between different affiliations regarding the knowledge level. Alghamdi et al. assessed Saudi Arabian nurses’ knowledge and attitudes regarding MRI safety and found that nurses have limited knowledge of MRI and moderate adherence to MRI safety procedures [4]. MRI in patients with a pacemaker is considered a general contraindication to examining due to the risk of life-threatening interference with the device. However, new developments have been achieved in this area, which provides pacemakers compatible with the magnetic field under certain conditions, such as magnetic field power, radiofrequency sequences, and gradient slew rates [6]. Even though there is no significant evidence of harm or injury to the fetus from magnetic field exposure, long-term safety regarding the magnetic field, radiofrequency field, and loud acoustic environment is under investigation [7]. Thus, MRI in pregnancy is a required checking point before entering the magnetic field environment. Scanning patients with metallic objects requires further investigations to identify the object's type and nature, which may pose a risk for patients and often cause artifacts [8]. Also, scanning patients with tattoos have been associated with adverse reactions, and tattoos are a potential source of risks, such as skin burn [9]. Scanning pregnant patients and patients with a pacemaker, metallic objects, or tattoos could cause adverse reactions under certain circumstances [10]. Therefore, increasing the knowledge level of MRI safety for those who might be involved in the MR environment is essential to avoid any complications.
In the awareness domain, participants showed a high level of awareness regarding the bioeffect hazards caused by the strong magnetic field, MRI zones, and claustrophobic patients. On the other hand, roughly 40% of participants reported that they need to be made aware of the new compatible pacemakers. Regarding claustrophobic patients, it is estimated that more than half of the participants were aware that some patients might be claustrophobic from the MRI scanner. Claustrophobia is considered a common issue in MRI examinations [11], which is estimated to occur in 2.1 to 14.3% of all MRI examinations [12, 13], and could lead to some negative consequences, such as the need for conscious sedation; in some cases, alternative medical imaging modalities could be required [14]. Raising prospective healthcare professionals’ awareness of MRI zones, claustrophobic patients, and the bioeffect hazards caused by the strong magnetic field is essential to inform and educate them about MRI safety to influence their attitudes [15]. Alelyani et al. assessed patients' perceptions and attitudes toward MRI safety and reported a moderately positive attitude level about MRI safety [16].
In the attitude domain, less than half of the participants were interested in attending MRI safety seminars and training to expand their knowledge regarding MRI safety. They expressed that their specialties do not have an influential role in the MRI department. Also, Alelyani et al. assessed Saudi Arabian health workers' perceptions and attitudes toward MRI safety. They reported that the overall knowledge score of the health workers was 60%, and the attitude score was 71.4% for the perception of MRI safety [17]. Attendance at regular scientific seminars and training is important in increasing knowledge and awareness regarding MRI safety. This may increase the need to introduce this critical aspect to prospective health professionals who could enter the MRI environment.
In the practice domain, more than half of the participants showed a high awareness of the practical aspects of MRI safety, which may reflect our study population's knowledge and awareness levels. Hearing protection during the MRI examination is not optional, as the noise might affect a patient’s hearing [18-20]. Thus, prospective health profes-sionals must know the basic practical aspects of MRI safety to ensure patient safety.
MR healthcare workers are usually familiar with MR safety considerations and aware of the potential hazards and risks in the MR environment. Despite the fact that MR technologist have extensive experience working alone without supervision in Saudi Arabia, most of the MR technologists are unaware of lone working regulations, that raised concerns regarding to the MR accidents [21].
5. STRENGTHS AND LIMITATIONS
The strength of this study includes being the first study identifying the knowledge, attitude, and practice related to MRI safety among health Professionals in the west region of Saudi Arabia. The limitations of this study are mainly centered on the sample size and the single-site study – these need to be addressed in future studies to include a broader population. Additionally, academic perceptions and insights from leaders across the academic programme were not included in our study, which surely would reflect the importance and benefits of including MRI safety topics in academic curricula. In addition, it would be recommended to add the multivariate analysis in the future study, in order to explain and predict the probability of a “objective variable” occurring from several factors (explanatory variables).
CONCLUSION
This research study explored prospective healthcare professionals’ level of knowledge, awareness, attitude, and practice concerning MRI safety. The research found that prospective healthcare professionals showed an acceptable level of knowledge and practical understanding, a high level of awareness, and a moderately positive attitude level regarding MRI safety. The findings of this study are valuable for higher education institutions (e.g., universities), as the information will help them to modify their curriculum content to fill the gaps of knowledge in this area. Further studies are required to investigate the knowledge level of prospective healthcare professionals regarding MR safety in a larger and broader population.
Implication: The results of this study are helpful for higher education institutions, enabling them to modify their curriculum content to fill the gaps of knowledge in this area.
LIST OF ABBREVIATIONS
| MRI | = Magnetic Resonance Imaging |
| JASP | = Jeffreys’ Amazing Statistics Program |
| VAS | = Visual Analog Scale |
| EMFs | = Electromagnetic Fields |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has obtained ethical approval from the Scientific Research and Ethics Committee of the Applied Medical Sciences College (Ref. 2021/112/303/DRD).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants of this study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
STANDARDS OF REPORTING
COREQ guidelines were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


