All published articles of this journal are available on ScienceDirect.
Public Health Career Perceptions and COVID-19 Pandemic: A Cross-sectional Study on Views of Graduates from a Community-oriented Medical School
Abstract
Background:
Recent pandemics, particularly COVID-19, have alerted the international community about the importance of encouraging doctors to choose public health and its subspecialties as their main career.
Objective:
To explore the influence of the COVID-19 pandemic on the views of medical graduates towards public health specialty.
Methods:
An online questionnaire was emailed to the medical graduates enrolled in the Arabian Gulf University Alumni Association. Data was sought on the doctors’ demographic characteristics, medical career status, and their perceptions of public health and its subspecialties. Responses were categorized into two subgroups and analyzed based on doctors’ year of graduation, i.e., before the COVID-19 pandemic (before 2019) and during the COVID-19 pandemic (2019 to 2021).
Results:
Two-thirds of medical graduates stated that the COVID-19 pandemic didn’t influence their choice of specialization program, 48.9% agreed that their view towards public health and its subspecialties has changed positively while 34.2% indicated that their view towards the specialty remained the same. Most of the graduates were not willing to consider changing their career to public health. A significant association was found between the perspectives of doctors who graduated before the COVID-19 outbreak compared to those who graduated during the pandemic towards the public health specialty and its subspecialties (p=0.028).
Conclusion:
Although the number of doctors who positively view public health and its subspecialties has increased during the COVID-19 pandemic, it remains an unattractive career choice. Medical schools should consider public health as part of clinical clerkship rotations and in career day activities.
1. INTRODUCTION
Attracting medical graduates to specialize in public health has been a global challenge for decades. Doctors traditionally found clinical subspecialties much more attractive than the non-clinical ones, particularly public health [1]. Since the turn of the century, the World Health Organization (WHO) has been warning of worldwide shortages in public health personnel and have consistently emphasized the urgent need for training and capacity building in the field of public health [2, 3]. Moreover, the recent pandemics and epidemics particularly COVID-19, along with the breakdown of the healthcare systems, even in the industrially developed countries [4], have put the field of public health on the spotlight as communities faced the reality of how short we are in public health specialists. The role of public health specialists and health workers in combating the recent COVID-19 pandemic has been highlighted in numerous literature publications [5, 6].
Studies from different parts of the world continued to demonstrate a lack of interest of doctors to choose public health and its subspecialties (community medicine and epidemiology) as a lifelong career [7]. Part of the blame for this apparent lack of enthusiasm towards specializing in public health has been directed at medical schools’ curricula which mostly disadvantage non-clinical fields and produce doctors who have flawed perceptions about what a public health specialty is and what it is not [8-10]. This is further emphasized in a BEME systematic review which has indicated that medical career decisions are formed by a matching of medical students’ perceptions with the characteristics of medical specialty [11].
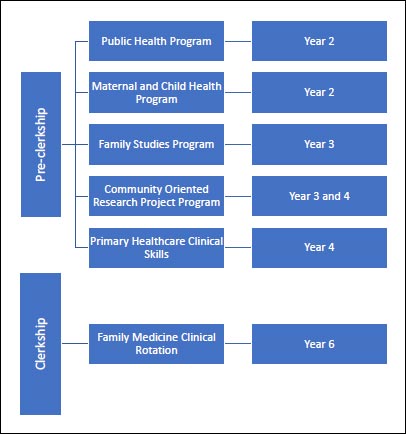
The College of Medicine and Medical Sciences (CMMS) at the Arabian Gulf University (AGU) since its inception in 1982 has been a community-oriented medical school. The curriculum comprises of six academic years and includes several compulsory community health programs. The programs comprise of public health, family studies, maternal and child health, community-oriented research project, and primary healthcare clinical skills in the pre-clerkship phase; along with family medicine clinical rotation in the clerkship phase (Fig. 1) [12, 13]. Subsequently, medical graduates from AGU would be anticipated to have positive views towards public health and its subspecialties in view of the medical students’ early exposure to the concepts of public health (Fig. 1). In addition, it would be expected that the ongoing pandemics made the doctors more appreciative of the importance of the field. This study addresses the research question of what is the influence of the COVID-19 pandemic on the views of AGU medical graduates towards public health and its subspecialties? The aim of this investigation is to develop strategies that would attract higher numbers of doctors to join the field of public health and its subspecialties.
2. MATERIALS AND METHODS
2.1. Study Population and Data Collection
AGU is a regional university based in the Kingdom of Bahrain and hosts students of both genders from Gulf Cooperation Council (GCC) countries (Bahrain, Saudi Arabia, Kuwait, Oman, United Arab Emirates and Qatar) [12]. A cross-sectional study (since it was viewed as the most suitable study design to address the research question) was undertaken among the Doctor of Medicine (M.D.) program graduates from the CMMS at the AGU. An online self-administered questionnaire was emailed in February 2022. The questionnaire was tested and piloted by the authors and modifications were made accordingly. The sampling frame was based on the list of doctors who had active email addresses on the AGU Alumni Association database. Information was sought from the doctors on their (Independent variables: demographic characteristics, medical career status) along with (Dependent variable: their perceptions on public health and its subspecialties) in view of the recent COVID-19 pandemic.
2.2. Statistical Analysis
Descriptive statistical analysis of counts for each question were calculated using an appropriate software (Statistical Package for Social Science (SPSS) software version 28). Cross-tabulated frequencies and percentages were produced. Responses were categorized into two subgroups based on the year of graduation of the doctors, i.e., before COVID-19 pandemic (before 2019) and during COVID-19 pandemic (2019 to 2021). Subsequently, all potential associations between the subgroup of graduation year and the doctors’ characteristics were tested using the chi-square test. A p value of less than 0.05 was considered statistically significant.
2.3. Ethical Considerations
This research project was approved by the Research and Ethics Committees of CMMS at AGU (approval number: E36-PI-6-22). The names and email addresses of the doctors who completed the questionnaire were kept anonymous. Furthermore, in order to ensure confidentiality, data was analyzed as a total sample population and not as individual doctors’ responses. In line with the recommendation of the committee, online consents were obtained from the potential participants and who were assured of their rights to withdraw from the study.
3. RESULTS
A total of 190 completed forms were received. Table (1) presents the description of the frequency distribution of the demographic variables of the respondents. The mean age of the doctors was 29.93±7.03 years and 43.7% were males. The sample represented doctors from the main Arab Gulf countries; Bahrain (48.4%), Saudi Arabia (26.3%), and Kuwait (18.4%). A large proportion of the respondents (62.1%) were at entry level of their career.
Fig. (2) shows that 56.8% have graduated from AGU before 2019 (before the COVID-19 pandemic) and the remaining (43.2%) graduated during the pandemic (2019-2021).
| Characteristics | Frequency (n=190) |
Percent (%) |
|---|---|---|
| Gender | ||
| Male | 83 | 43.7 |
| Female | 107 | 56.3 |
| Nationality | - | - |
| Bahrain | 92 | 48.4 |
| Saudi Arabia | 50 | 26.3 |
| Kuwait | 35 | 18.4 |
| Other | 13 | 6.8 |
| Career level | - | - |
| Entry | 118 | 62.1 |
| Developing | 25 | 13.2 |
| Advanced | 47 | 24.7 |
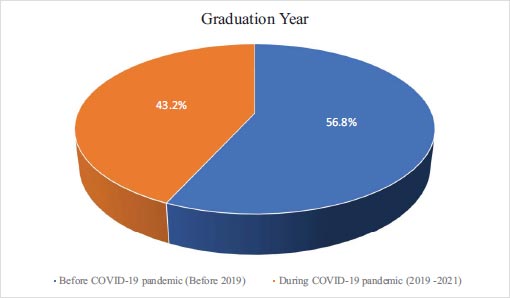
Table 2 shows that more than two-thirds of graduates (67.9%) indicated that their choice of specialization program was not affected by the COVID-19 pandemic. 48.9% of medical graduates agreed that their view toward the specialty of public health and its subspecialties (community medicine/epidemiology) programs has changed positively, while 34.2% of medical graduates indicated that their view towards the specialty has not changed. 63.2% of medical graduates said that they will continue with their specialization as they prefer specialties that have direct contact with patients due to COVID-19. Most of the medical graduates (81.1%) have not considered changing their current specialty and commencing specialization in public health and its subspecialties (community medicine/epidemiology) programs.
Table 3 reveals a statistically significant association between the view of doctors who graduated before the COVID-19 outbreak compared to those who graduated during the pandemic towards the public health specialty and its subspecialties (community medicine/epidemiology) (χ2=9.116, df=3; p=0.028). However, their perceptions appeared largely negative. Trends was also observed in doctors’ on whether COVID-19 pandemic has affected the selection of their specialty and willingness to continue their career in the current specialty (p= 0.071) and (p=0.078), respectively.
| Item | Frequency (n=190) | Percent (%) |
|---|---|---|
| Did your specialty selection affected because of COVID-19 pandemic? | ||
| No | 129 | 67.9 |
| Yes, and I want to change my specialty | 9 | 4.7 |
| Yes, but I want to continue in the same specialty | 52 | 27.4 |
|
Did COVID-19 pandemic change your views towards the specialty of Public Health / Community Medicine / Epidemiology? |
||
| No, still negative | 18 | 9.5 |
| No, still positive | 65 | 34.2 |
| Yes, negatively | 14 | 7.4 |
| Yes, positively | 93 | 48.9 |
|
Because of COVID-19 pandemic, do you prefer the specialties that have direct contact with patients (Clinical specialties)? |
||
| No | 61 | 32.1 |
| Yes, and I want to change my specialty | 9 | 4.7 |
| Yes, but I want to continue in the same specialty | 120 | 63.2 |
|
Because of COVID-19 pandemic, do you prefer the specialties that have no direct contact with patients (e.g. Radiology, Lab Medicine, Pathology, Public Health)? |
||
| No | 130 | 68.4 |
| Yes, and I want to change my specialty | 9 | 4.7 |
| Yes, but I want to continue in the same specialty | 51 | 26.8 |
| Variable |
Before COVID-19 Pandemic (Before 2019) n=108 (%) |
During COVID-19 Pandemic (2019-2021) n=82 (%) |
P-value |
|---|---|---|---|
| Gender | |||
| Male | 44 (40.7) | 39 (47.6) | 0.348 |
| Female | 64 (59.3) | 43 (52.4) | |
| Nationality | - | - | - |
| Bahrain | 55 (50.9) | 37 (45.1) | 0.061 |
| Saudi Arabia | 27 (25) | 23 (28) | |
| Kuwait | 15 (13.9) | 20 (24.5) | |
| Other | 11 (10.2) | 2 (2.4) | |
| Did your specialty selection affected because of COVID-19 pandemic? | - | - | - |
| No | 66 (61.1) | 63 (76.8) | 0.071 |
| Yes, and I want to change my specialty | 6 (5.6) | 3 (3.7) | |
| Yes, but I want to continue in the same specialty | 36 (33.3) | 16 (19.5) | |
| Did COVID-19 pandemic change your views towards the specialty of Public Health /Community Medicine / Epidemiology? | - | - | - |
| No, still negative | 7 (6.5) | 11 (13.4) | 0.028 |
| No, still positive | 34 (31.5) | 31 (37.8) | |
| Yes, negatively | 5 (4.6) | 9 (11) | |
| Yes, positively | 62 (57.4) | 31 (37.8) | |
| Because of COVID-19 pandemic, do you prefer the specialties that have direct contact with patients (Clinical specialties)? | - | - | - |
| No | 36 (33.3) | 25 (30.5) | 0.354 |
| Yes, and I want to change my specialty | 7 (6.5) | 2 (2.4) | |
| Yes, but I want to continue in the same specialty | 65 (60.2) | 55 (67.1) | |
| Because of COVID-19 pandemic, do you prefer the specialties that have no direct contact with patients (e.g. Radiology, Lab Medicine, Pathology, Public Health)? | - | - | - |
| No | 67 (62) | 63 (76.9) | 0.078 |
| Yes, and I want to change my specialty | 7 (6.5) | 2 (2.4) | |
| Yes, but I want to continue in the same specialty | 34 (31.5) | 17 (20.7) |
4. DISCUSSION
This study is the first published report from a Middle Eastern population that provides novel data on the potential impact of the COVID-19 pandemic on the perceptions of medical graduates towards public health and its subspecialties. The study provides an insight on the potential impact of the recent COVID-19 pandemic on the career choices of medical graduates in the GCC who were primarily trained during their undergraduate program to become practicing clinicians rather than working in the field of public health. Although the work of experts in public health has become more appreciated during the COVID-19 era as people all around the world see these specialists as persons who are directly entrusted in managing the crisis [14-16], the option of specializing in the field of public health remains a largely an unattractive career choice for most medical graduates. It is not surprising then, to find that despite the significant increase in the number of doctors who positively view the field of public health and its subspecialties, this did not materialize into an actual career choice. These findings are in line with published scientific reports from high-income [17, 18] as well as low income-countries [19]. Further, doctors who responded to this questionnaire indicated that they have no intention to consider changing their current specialty into public health field, which may reflect their negative convictions towards the public health career. However, looking to the future, it would be plausible to expect that medical students who have been subjected to social, psychological and health traumas as a result of the social isolation during the COVID-19 pandemic [20], would appreciate the field of public health.
There are limitations in the study which we acknowledge and have endeavored to address. Firstly, the findings may not be generalizable to doctors in other parts of the world. However, since our results are consistent with those from western countries [17], we believe that there is a genuine global shift towards a more positive view of the public health career in the post-COVID-19 era, at least within the high-income GCC countries and probably in those Middle Eastern populations with lower income levels as well. Secondly, since a cross-sectional design was employed in this study, one cannot be certain on whether this influence of COVID-19 on the perceptions towards career choices in public health of medical graduates is permanent or is merely a short-term change that will fade away with time nor that we can establish a cause-effect relationship. This would justify the need for a further follow-up research investigation to confirm the findings. Nevertheless, by collecting the data from the doctors in this project after more than two years (February 2022) of the COVID-19 pandemic, it would be reasonable to accept this impact as a true long-term change between the influence of the pandemic and the subsequent views towards public health and its subspecialties.
The recent COVID-19 pandemic has highlighted the extent to which healthcare systems are vulnerable, even in wealthy industrially developed countries [21-24]. One of the main lessons that we learned from this crisis, is the need to reshape the medical syllabus into a more population-based curriculum that integrates public health rotation within the medical courses of clinical reasoning and professional skills [25-27]. The recommendations from this study give further support to this notion that medical schools should rise to the challenge and take a lead in rethinking the appropriate approach they need to adopt when introducing public health rotations within their undergraduate clerkship curriculum. Studies have pointed out that Career Day has an impact on shaping the future career choices of the undergraduate medical students [28, 29]. We propose that presentations on the role and scope of the careers in public health should become an integral part of career day activities in medical schools. In addition, health policy makers should consider appropriate career incentives to attract medical graduates to specialize in the field of public health. Earlier experiences indicate that incentives were one of the effective tools in shaping doctors’ decisions to join medical subspecialties [30, 31].
CONCLUSION
Although the number of doctors who positively view public health and its subspecialties has increased during the COVID-19 pandemic, it remains an unattractive career choice. Health policy experts should capitalize on this opportunity to provide enough public health human resources to face any future health challenges. In addition, medical schools should consider introducing public health as part of clinical clerkship rotations and in career day activities.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This research project was approved by the Research and Ethics Committees of CMMS at AGU (approval number: E36-PI-6-22).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Online consents were obtained from the potential participants and who were assured of their rights to withdraw from the study.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and analyzed during the current study are available from the corresponding author [S.A] on reasonable request.
ACKNOWLEDGEMENTS
Declared none.


