All published articles of this journal are available on ScienceDirect.
Profile of Preeclampsia Patients with Aggravating Factors: A Retrospective Study
Abstract
Introduction:
Preeclampsia contributes to 9-26% of maternal deaths in developing countries.
Methods:
This study was conducted to present the profile of preeclampsia patients with aggravating factors. A retrospective study was performed on preeclampsia patients admitted to the Obstetrics and Gynecology Department of Cipto Mangunkusumo Hospital from January to June 2021. A total of 109 participants who met the specified criteria were included in this study. The prevalence of pre-eclampsia was 12.9%. The common aggravating factors were multiple pregnancies (10.1%), chronic hypertension (5.5%), and diabetes (5.5%). Two subjects (1.8%) had eclampsia, and 13 (11.9%) were diagnosed with HELLP syndrome.
Results:
Most subjects gave birth via caesarean section (79.8%). More than 50% gave birth at 35 years of age, nullipara, with a Body Mass Index (BMI) > 30 kg/m2, multiple pregnancies, chronic hypertension, and type 2 diabetes mellitus.
Conclusion:
Outcomes of studies that have been conducted include survival, complications, eclampsia, HELLP syndrome, caesarean delivery, delivery at < 34 weeks GA, and prolonged hospitalization.
Impact Statement
• What is already known about this topic?
• What did the results of this study add?
• What are the implications of these findings for clinical practice and further research?
1. INTRODUCTION
Preeclampsia, or pregnancy-induced hypertension, is a condition when systolic blood pressure ≥140 mmHg and diastolic blood pressure ≥90 mmHg at gestational age > 20 weeks accompanied by organ disturbance/damage [ 1, 2]. The prevalence of preeclampsia worldwide is around 2-8%, but in developing countries, the prevalence can reach 1.8-16.7% [ 3, 4]. Preeclampsia is characterized by various risk factors and causes. Some risk factors that can aggravate preeclampsia include multigravida, age > 35 years, in vitro fertilization, comorbidities in the mother, and other reproductive technologies [ 5-7].
Common comorbidities include chronic hypertension, chronic kidney disease, diabetes mellitus, thrombophilia, obstructive sleep apnea, and obesity with BMI > 30 kg/m2. Risk factors that increase a person's likelihood of developing preeclampsia include a family history of preeclampsia, a history of preeclampsia in a previous pregnancy, a history of placental rupture, and delayed fetal development [ 5, 8]
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
|
Age (years) <20 20-34 ≥35 |
3
66 40 |
2.8
60.6 36.7 |
|
Place of Origin Urban Rural |
109
0 |
100
0 |
|
Level of Education Elementary Junior High Senior High Associate Degree Bachelor |
7
14 50 11 27 |
6.4
12.8 45.9 10.1 24.8 |
|
Occupation Housewife Entrepreneur Employee Others |
78
1 14 16 |
71.6
0.9 12.8 14.7 |
|
Labuor Assurance Yes No |
106
3 |
97.2
2.8 |
More than 1/3 of the subjects were aged 35 years, with a fairly good level of education, able to complete high school and pursue both D3 and undergraduate higher education. Most participants were housewives (71.6%). Most of the participants used national health insurance (JKN) and regional health insurance (Jamkesda). Clinical data of the patients are shown in (Table 2).
Due to the high rate of maternal morbidity and mortality due to preeclampsia and the importance of identifying risk factors, we were interested in understanding the profile of preeclampsia patients, especially preeclampsia with weight loss. Previous research [ 9] regarding the characteristics of pregnant women with preeclampsia showed that most preeclampsia patients were in the 31-35 age group (28.3%), the primigravida group (61.6%), the obese group/BMI > 30 (53.3%), and the group without a history of hypertension (91.7%). A similar study [ 10] stated that maternal age, occupation, BMI, gestational interval, and history of hypertension in pregnancy had a 74.5% probability of the incidence of preeclampsia with complications [ 11, 12]. However, to the best of our knowledge, no epidemiological study has been conducted at the Cipto Mangunkusumo Hospital, a national referral center in Indonesia.
The objective of this study was to determine the prevalence of preeclampsia with aggravating factors, accompanying aggravating factors, and patient profiles at a national referral center.
2. MATERIALS AND METHODS
This observational study was conducted to determine the profile of preeclampsia patients with aggravating factors treated at the Department of Obstetrics and Gynecology, University of Indonesia, tertiary hospital from January to June 2021. The research subjects included in the study were patients with severe preeclampsia with one of the following risk factors: age 35 years, previous history of preeclampsia, history of preeclampsia in mother or sister, nullipara, multiple pregnancies, obesity (BMI > 30 kg/m2), gestational interval > 10 years, comorbidities such as chronic hypertension, type 1 diabetes mellitus or 2, kidney disease, and autoimmune disease (systemic lupus erythematous, antiphospholipid syndrome). Exclusion criteria included gestational age < 20 weeks and incomplete research data on the subject. This study included all patients who met the criteria; therefore, the minimum sample size was not calculated.
Research findings are Between January and June 2021, secondary data were taken from the tertiary hospital's medical records.. Medical records will be processed and presented in the form of sociodemographic characteristics, risk/weight factor data, clinical data, and outcomes of pregnant women. Patient data were kept confidential and processed using statistical analysis. This study was approved by the Department of Obstetrics and Gynecology and the Ethics Committee.
3. RESULTS
3.1. Overview of Patient Profiles
The results showed that 109 subjects met the specified criteria and research time. The total number of patients seeking treatment at the Department of Obstetrics and Gynecology, University of Indonesia, from January to June 2021 was 839; therefore, the prevalence of subjects with preeclampsia was 12.9%. The demographic characteristics of the study participants are shown in Table 1.
Table 2.
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
|
Blood Pressure <160/110 SBP 160-179 or DBP 110-119 ≥180/120 |
15 51 43 |
13.8 46.8 39.4 |
|
Proteinuria Yes No |
89 20 |
81.7 18.3 |
|
Nutritional Status Underweight (BMI <18,5) Normal Overweight (BMI >25) Obesity (BMI >30) |
0 31 39 39 |
0 28.4 35.8 35.8 |
|
Diagnosis Preeclampsia Severe Preeclampsia |
8 101 |
7.3 92.7 |
|
Gravidity 1 2-4 ≥5 |
35 67 7 |
32.1 61.5 6.4 |
|
Parity <2 2-4 ≥5 |
65 43 1 |
59.6 39.4 1 |
|
Abortion History Yes No |
79 30 |
72.5 27.5 |
|
Antenatal Care History Yes No |
105 4 |
96.3 3.7 |
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
|
Age >35 years old Yes No |
33
76 |
30.3
69.7 |
|
Nullipara Yes No |
35
74 |
32.1
67.9 |
|
BMI >30 kg/m
2 Yes No |
39
70 |
35.8
64.2 |
|
Multiple Pregnancy Yes No |
11
98 |
10.1
89.9 |
|
Chronic Hypertension Yes No |
6
103 |
5.5
94.5 |
|
Diabetes Mellitus Yes No |
6
103 |
5.5
94.5 |
3.2. Factors Aggravating Preeclampsia
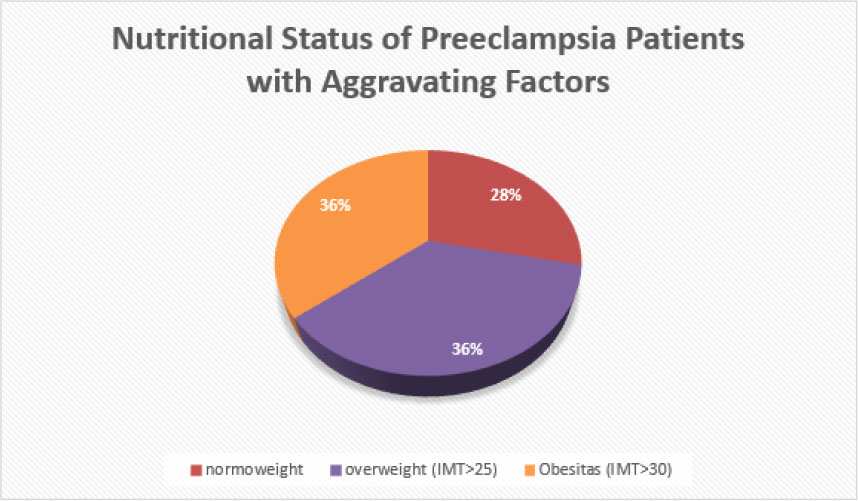
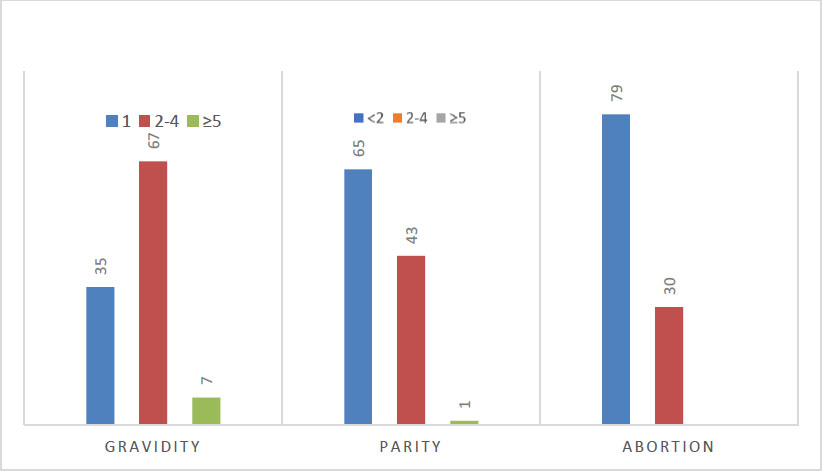
Assessment of nutritional status in preeclampsia patients with aggravating factors, mostly overweight and obese, was comparable (36% for each category). None of the subjects were underweight. The distribution of clinical characteristics of patients according to gravidity, parity, and the presence or absence of abortion. In addition, 32.1% of preeclampsia patients with Aggravating Factors included primigravida, while grand multigravida was only found in seven subjects (6.4%) with a maximum pregnancy 7th. Grande multipara was still found in 1% of subjects with a history of giving birth 6 times. The rest were pre-eclamptic mothers with Aggravating Factors who gave birth to their children (Figs. 1 and 2, Table 3).
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
|
Survival Alive Die |
109
0 |
100
0 |
|
Complication Yes No |
27
82 |
24.8
75.2 |
|
Eclampsia Yes No |
2
107 |
1.8
98.2 |
|
HELLP Syndrome Yes No |
13
96 |
11.9
88.1 |
|
Labor Caesarean Section Vaginal Delivery Not yet Labor |
87
20 2 |
79.8
18.3 1.8 |
|
Gestational Age at Delivery ≥37 weeks 34-36 weeks <34 weeks |
23
29 57 |
21.1
26.6 52.3 |
|
Post-partum Care Time <4 days 4-7 days >7 days |
66
36 7 |
60.6
33.0 6.4 |
3.3. Maternal Outcome
As expected, 100% of the subjects survived and were able to return home after undergoing treatment. Only a quarter of the participants experienced complications during pregnancy. Two subjects had eclampsia, and 13 were diagnosed with HELLP syndrome. Most pregnant women with preeclampsia with Aggravating Factors gave birth by caesarean section (79.8%). More than 50% of the subjects gave birth at < 34 weeks of gestation, and only 21.1% gave birth at term or at 37 weeks of gestation. On average, the patients were treated for less than 4 days. For the maternal outcomes, (Table 4).
4. DISCUSSION
Preeclampsia is classified as severe asymptomatic preeclampsia or severe preeclampsia [ 1]. Both can be exacerbated by the presence of risk factors. This group is included in the research subject, namely preeclampsia patients with aggravating risk factors. In this study, the incidence of preeclampsia with aggravating factors from January to June 2021 was 12.9%. This figure is higher than the incidence of preeclampsia in the United States, Canada, and Western Europe [ 13]. Patients with preeclampsia with the greatest aggravation were in the age group of 20-34 years, 60.6%). This result is in accordance with a study conducted in Sragen in 2018 that reported a 64.4% incidence of preeclampsia aged 20-35 years [ 14]. This age group is the productive age, which is considered safe for pregnancy and is not a risk group. That is, subjects of productive age in this study had other risk factors that influenced the onset of preeclampsia. The distribution of education levels in this study is much better than that in Bangladesh in 2021 regarding the prevalence of preeclampsia and its influencing factors [ 15].
In this study, most of the subjects were found to be working as housewives (71.6%). These results are consistent with those of a study in Jaipur, India, which reported that 88.9% of subjects in the preeclampsia group worked as housewives. The study showed that there was no significant difference between occupation and preeclampsia (P >0.05) [ 16]. The nutritional status of pregnant women before pregnancy and weight gain during pregnancy are known to affect the incidence of preeclampsia. In this study, statistics showed that the majority of preeclamptic pregnant women with Aggravating Factors had a BMI >25 and a BMI >30, namely 35.8% for each category. A 2016 meta-analysis of risk factors for preeclampsia reported that a BMI of 26 University of Indonesia >25 had a 2.1 times greater risk of preeclampsia, while a BMI >30 had a 2.8 times higher risk of preeclampsia than a normal BMI [ 17, 18].
Among 109 subjects with aggravation of preeclampsia, 92.7% had severe preeclampsia, while less than 10% had preeclampsia without severe symptoms. This result was higher than that of the study conducted by Yang et al. in 2021. In this study, only 6.6% of the subjects had preeclampsia aggravated by chronic hypertension, or as many as six subjects. These results are supported by research at Airlangga University in 2017-2018, which reported that there were 8 (14.55%) preeclampsia patients with chronic hypertension [ 19]. Complications of preeclampsia can occur and even lead to death [ 19-22]. In this study, 24.8% of the subjects had complications, but all subjects survived. Eclampsia causes a significant increase in the maternal morbidity and mortality rates. Maternal mortality due to eclampsia can reach 0-14%, mainly due to permanent sequelae in the brain. The outcome of preeclampsia in the form of postpartum hospitalization in this study was mostly as expected (< 4 days of hospitalization). Only 39.4% of the subjects had prolonged hospitalization (≥ 4 days). This result was higher than that of a similar study in Brazil in 2019, which reported a prolonged hospitalization time of 5 days by 23% [ 19]. This is because the subjects of this study were specific for preeclampsia with aggravating conditions, so more complications caused longer hospitalization times.
CONCLUSION/HYPOTHESES
Age > 35 years, nullipara, Body Mass Index (BMI) > 30 kg/m2, multiple pregnancies, chronic hypertension, and type 2 diabetes mellitus are the factors that aggravate preeclampsia in patients who seek treatment at a tertiary hospital from January to June 2021. Therefore, these risk factors should be considered when planning and caring for pregnant women with and without preeclampsia. The outcomes of studies that have been conducted include survival, complications, eclampsia, HELLP syndrome, caesarean delivery, gestational age < 34 weeks at delivery, and prolonged hospitalization (4-7 days). Furthermore, further research and a longer follow-up are needed to determine the relationship between the factors in the study and the incidence of preeclampsia with aggravating factors.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Department of Obstetrics and Gynecology and the Ethics Committee.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were by the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this study are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


