All published articles of this journal are available on ScienceDirect.
Families Taking Care of Individuals with Schizophrenia: A Mixed Method Resilience Study
Abstract
Background:
Schizophrenia, a debilitating disease, causes affected individuals to have personal and social function impairment. As a consequence, affected individuals rely on family caregivers most of the time. Access to mental health care is still limited in Lubuk Pakam, with only one district hospital providing psychiatric care. Therefore, the family must play a great role in providing care for schizophrenic individuals. The aim of our study was to investigate resilience and assess the efficacy of the family empowerment module among families taking care of individuals with schizophrenia.
Methods:
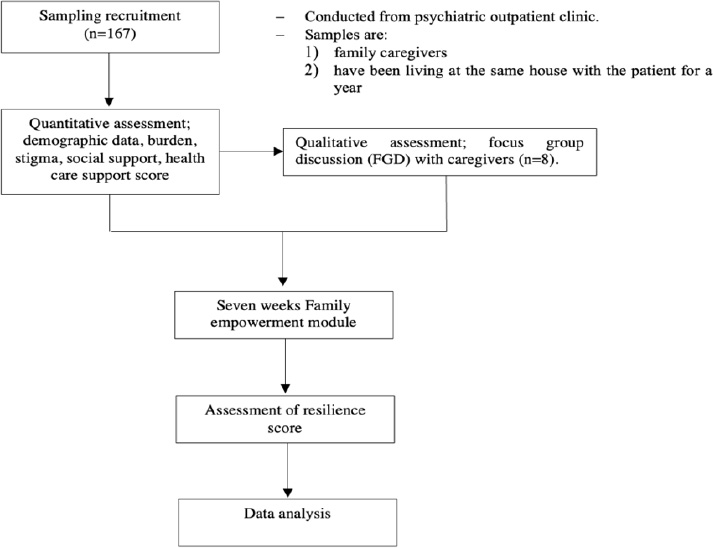
We conducted two sequential studies, both quantitative and qualitative studies (mixed method), to investigate the family resilience profile. The family empowerment module was asserted and efficacy was measured using a dependent t-test. Multivariate analysis with linear regression was used to assess the relationship between independent variables (burden, stigma, social, and health care support) and the dependent variable (family resilience).
Result:
The family burden has shown a negative coefficient regression score of 0.130, which means that family burden has an impact of 13%, leading towards the decline of family resilience. A considerable increase in family resilience was noted after the implementation of the family empowerment module (p = 0.001).
Conclusion:
Implementation of the family empowerment module has helped in increasing family resilience. We suggest that this implementation can also be carried out, especially in other county hospitals with similar relatable situations.
1. INTRODUCTION
Schizophrenia, as a multifaceted disease, affects the cognitive and psychosocial aspects of individuals [1]. It is estimated that nearly 20 million people suffer from schizophrenia worldwide with the incidence of disability-adjusted life year reaching nearly 1.13 million cases in 2017 [2, 3]. Relapse poses a challenge in treating individuals with schizophrenia and it has been associated with a lack of family support. Relapse in schizophrenia contributes to aggravated consequences of the disease course, such as worsening cognitive symptoms and reduced quality of life, resulting in even more devastating impacts on the families taking care of individuals with schizophrenia [4]. Family caregivers are individuals asserting either physical or psychological needs and are usually not paid. They not only ensure the fulfillment of basic needs but also the continuity of treatment, and serve as communicators, bridging the gap between patients and therapist [5]. Approximately, 60.6% of families taking care of individuals with schizophrenia experience escalating negative emotions, such as anger and sadness, frequently resulting in fights among family members or spouses [6]. Individuals with schizophrenia are also not always welcomed and the disease itself is perceived with less respect, resulting in stigma. Stigmatization may manifest in the form of social isolation or discriminating statements, which later affects families with schizophrenic family members. Taking care of individuals with schizophrenia is an exhausting responsibility. Therefore, caregivers are not only exposed to strenuous physical burden, but also psychological burden, including shame and lack of social support [7]. Data from Riskesdas (Basic Health Research) of Indonesia showed the prevalence of schizophrenia/other psychotic disorders extend to 6.7 per 1000 households in 2018. In the Sumatera Utara province, the prevalence was 6.3/1000 households, in which nearly half of this population did not adhere to appropriate treatment [8]. Our study was conducted in one of Sumatra Utara’s counties, Lubuk Pakam, which is approximately 40 km from Medan, the capital of Sumatra Utara province. Access to mental health care is still limited with only one hospital providing psychiatric care. Therefore, the family must play a great role in taking care of individuals with schizophrenia, particularly those with predominantly positive symptoms and poor insight. There are various intervention models related to resilience, such as the Stress Management and Resiliency Training/Relaxation Response Resiliency Program (SMART-3RP), Acceptance and Commitment Therapy, Mindfulness-based Cognitive Therapy strategies, Transactional Model of Stress and Coping, Attention and Interpretation Therapy, and the Families OverComing Under Stress program (FOCUS) for resilience training [9-13]. Meanwhile, in Indonesia, especially in North Sumatra province, these intervention models, particularly directed to families/caregivers, are still limited. Therefore, the aim of our study was to investigate resilience and measure the effectiveness of family empowerment module implementation among families taking care of individuals with schizophrenia.
2. METHODS
2.1. Study Design
We conducted two sequential studies, both quantitative and qualitative studies (mixed method), to investigate family resilience in taking care of individuals with schizophrenia. The study was conducted from May to August 2022 in the Hospital of Drs. Haji Amri Tambunan of Lubuk Pakam. Lubuk Pakam is a county in Sumatera Utara province with limited mental health facilities. Hospital of Drs. Haji Amri Tambunan is the only health facility that serves psychiatric patients and is equipped with only 10 beds for psychiatric inpatients. In this study, we investigated several independent factors that we hypothesized to be related to family resilience, including burden, stigma, social support, and health care support (Fig. 1).
| Material | Summary |
|---|---|
| 1. Schizophrenia | Given in 4 sessions. Caregivers are provided with information related to schizophrenia, including definition, prodromal symptoms, positive and negative symptoms, disease course, relapse prevention, treatment, and possible side effects of medication. The goal is to provide facts to caregivers and educate them to not doubt seeking professional medical help when dealing with individuals with schizophrenia. |
| 2. Increasing family resilience | Given in 6 sessions. Session 1: peer group sharing – the caregivers share their experiences in taking care of individuals with schizophrenia. The purpose of this session is to create a sense of inclusivity. Sessions 2 and 3: identification – the caregivers are taught to identify the problems in dealing with schizophrenic family members, then sort out between objective and subjective problems, and plan the strategy to solve the problems. Session 4 – 6: solving and evaluating – the caregivers are taught to restructure their mindset, apply their plan/strategy, and evaluate their decision. |
| 3. Utilization of the healthcare facility | Given in 2 sessions. Session 1: Role play workshop (between caregivers and medical personnel) in dealing with agitated schizophrenic individuals. Session 2: seminar and workshop on schizophrenia, agitation treatment, and assessment with PANS-EC (Positive and Negative Syndrome Scale-Excited Component), conducted for medical officers from Puskesmas (Public Health Center) and emergency unit. |
The empowerment for caregivers is implemented with FGD sessions and counseling with a total of 12 sessions for 7 weeks period. In these sessions, caregivers are provided with informative and applicable material in caring for schizophrenic family members. Table 1 summarizes the materials of a given module.
2.2. Sampling
This study obtained approval in accordance with the Declaration of Helsinki from the Ethical Committee of Health Research, Universitas Sumatra Utara (Letter number: 281/KEPK/USU2022). Informed consent was obtained from each respondent. Non-probability consecutive sampling was conducted to select 167 respondents for the quantitative study. Respondents were family caregivers of individuals with schizophrenia who had at least spent one year living at the same house with the patient. Recruitment was conducted at the psychiatric outpatient clinic. Prior to recruitment, a written informed consent explaining the objectives, confidentiality, and authority to withdraw participation, was addressed, and only those who had given consent were included in the study. On the other hand, for the qualitative study, 8 respondents were purposely selected.
2.3. Instruments
2.3.1. Family Resilience Assessment Scale (FRAS)
This questionnaire was adapted from Walsh’s concept of family resilience, consisting of families' belief system, organizational patterns, and communication processes. FRAS consists of 54 questions addressed to family caregivers that are scored from 1 (strongly agree) to 4 (strongly disagree). FRAS psychometric properties have been investigated and found to be a valid and reliable questionnaire that can be used in the general population without gender, race, or any social background limitation [14]. A study by Chew et al. found FRAS to have a high internal consistency of 0.92 when used among families of young people with chronic illness [15].
2.3.2. Zarit Burden Interview (ZBI)
ZBI was developed to assess the burden of caregivers and has been adapted in various languages. A validated Indonesian version of this questionnaire was completed by Rachmat et al. in 2009 with a reliability of 0.837 and an accuracy of 79.2%. ZBI serves as a self-reporting questionnaire consisting of 22 questions that assess the burden in the context of physical health, emotional health, and social and financial context of the caregivers. There are two main dimensions measured in ZBI, personal strain that reflects personal burden perceived subjectively by the caregivers, and role strain that reflects stress due to role conflicts or burden directly experienced from the activity of taking care. ZBI is interpreted as follows: 0–20 (no burden), 21–40 (mild-moderate burden), 41–60 (moderate-severe burden), and 61–88 (severe burden) [16].
2.3.3. Devaluation of Consumer Families Scale (DCFS)
DCFS is used to assess the stigma received by family caregivers of individuals with mental illness. The questionnaire consists of 7 items that highlight 3 domains, community refusal, causal attribution, and neglect. All items are scored by a four-point Likert scale with a maximum score of 28. A higher score indicates a higher level of stigma perceived by caregivers [17].
2.3.4. Social Support Scale (SSS)
This questionnaire consists of 4 domains, emotional, informational, instrumental, and esteem support, in which each domain comprises 5 question items. SSS is scored on a 5-point Likert score and reflects the degree of agreement. It was first developed by Grant Macdonald in 1998 and aimed to measure the extent of social support perceived by caregivers. It is a 10-minute self-reporting questionnaire that is appropriate for persons over the age of 16 [18].
2.3.5. Family Perceived Support Questionnaire (FPSQ)
FPSQ is used to measure the extent of family support from healthcare providers. It consists of 14 questions with two subscales, cognitive and emotional support. The cognitive subscale reflects the extent of support perceived by families that contributes to families’ independency [19].
2.4. Analysis
Bivariate analysis with dependent t-test was initially used; furthermore, multivariate analysis with linear regression was used to assess the relationship of independent variables (burden, stigma, social, and health care support) with dependent variable (family resilience). Qualitative data were analyzed by using several approaches described by Streubert and Carpenter [20].
3. RESULTS
Table 2 presents the characteristics of caregivers and their schizophrenic family members and their association with family resilience scores. In this study, we found that vast proportions of caregivers were elderly and female (67.1% and 53.3%, respectively), and were married (81.4%). The majority were siblings (31.7%) to individuals with schizophrenia. The vast majority of family caregivers completed senior high school (42.5%) and were currently employed (50.9%). We also found that family caregivers received monthly income that was above the county’s regulated minimum wage and that most of them have been taking care of schizophrenic individuals for more than 10 years (34.2%). We collected data regarding the schizophrenic patients taken care of by family caregivers participating in the study. The majority of them were at productive age with less than half of them being elders (34.1%) and experiencing more frequent relapse (54.4%).
| Characteristics | Frequency (n=167) | Percentage (%) | COR (95%CI) | AOR (95%CI) |
|---|---|---|---|---|
| Age (Years) | ||||
| Adolescence (<20) | 9 | 5.4 | Ref. | Ref. |
| Adult (20-59) | 46 | 27.5 | 1.26 | 1.35 |
| Elderly (> 60) | 112 | 67.1 | 2.35* | 2.17* |
| Gender | ||||
| Male | 78 | 46.7 | Ref. | - |
| Female | 89 | 53.3 | 0.47** | - |
| Marital Status | ||||
| Not married yet | 15 | 9.0 | Ref. | Ref. |
| Married | 136 | 81.4 | 2.50 | 2.22 |
| Widow/widower | 16 | 9.6 | 3.12* | 3.25* |
| Level of Education | ||||
| Did not finish school | 2 | 1.2 | 5.72 | 5.21 |
| Elementary | 33 | 19.8 | 4.52* | 3.81* |
| Junior high school | 39 | 23.4 | 1.02 | 1.34 |
| Senior high school | 71 | 42.5 | 0.74 | 0.52 |
| College/university | 22 | 13.2 | Ref. | Ref. |
| Employment | ||||
| Yes | 85 | 50.9 | Ref. | - |
| No | 82 | 49.1 | 4.95* | - |
| Relationship with the Patient | ||||
| Father | 17 | 10.2 | Ref. | - |
| Mother | 28 | 16.8 | 1.06 | - |
| Child | 43 | 25.7 | 1.03 | - |
| Husband | 18 | 10.8 | 2.20 | - |
| Wife | 8 | 4.8 | 1.53 | - |
| Sibling | 53 | 31.7 | 1.65** | - |
| Income | ||||
| Below minimum wage | 77 | 46.1 | 4.65* | - |
| Above minimum wage | 90 | 53.9 | Ref. | - |
| Length of Care (Years) | ||||
| <5 | 55 | 32.9 | Ref. | - |
| 5 – 10 | 55 | 32.9 | 1 | - |
| >10 | 57 | 34.2 | 0.48** | - |
| Age of the Patient | ||||
| Adolescent | 55 | 32,9 | Ref. | - |
| Adult | 55 | 32,9 | 1.03 | - |
| Elderly | 57 | 34, 2 | 1.07** | - |
| Patients’ Relapse Frequency | ||||
| < once/year | 76 | 45.5 | Ref. | - |
| >once/year | 91 | 54.5 | 3.68* | - |
*, p<0.05, **, p>0.005
| Average Scores | Means | SD |
|---|---|---|
| Family resilience | 143.49 | 4.90 |
| Social support | 50.82 | 7.91 |
| Health service support | 29.65 | 8.79 |
| Family burden | 29.72 | 10.28 |
| Stigma | 23.91 | 23.91 |
| Linear Regression Multivariate Analysis of Factors Affecting Family Resilience | ||
| B | p-value | |
| Family burden | -0.130 | 0.001 |
| Stigma | -0.499 | 0.001 |
| Health service support | 0.272 | 0.007 |
| Social support | 0.118 | 0.011 |
This present study indicated that the caregiver’s gender, relation with the patient, length of care, and age of the patient that was taken care of were not associated with a low family resilience score. Yet, unemployment, below minimum wage, and more frequent relapse were significant factors in developing low family resilience scores with odds ratios of 4.95, 4.65, and 3.68, respectively. In multivariate analysis (with the backward method), age, marital status, and level of education appeared as significant predictors for low family resilience scores. Particularly, elderly caregivers were 2.17 times (95%CI: 1.57-8.07) more likely to have low resilience than younger caregivers. Also, caregivers who were widowed/widower were 3.25 (95%CI: 1.29-12.05) times at higher risk of developing low family resilience. Furthermore, caregivers who did not complete elementary school were 5.21 times (95%CI: 2.17-18.26) at greater risk, and higher education emerged as a protective factor from developing low family resilience.
Table 3 shows the average score of family resilience to be 143.49, indicating a moderate level of family resilience. The average scores of social support (50.82) and health service support (29.65) were also moderate. The average score of family burden was 29.72, indicating a low to moderate score, and the average score of stigma experienced by the family was 23.91, also indicating moderate stigma. This present study showed family burden to have a negative coefficient regression score of 0.130, which means that family burden has an impact of 13% towards the decline of family resilience. A similar result has been reported with respect to other variables, such as stigma, health service support, and social support, which have also shown negative coefficient regression scores (0.499, 0.272, and 0.118, respectively).
Qualitative analysis result has been obtained after conducting an exploration of caregivers’ experience in treating individuals with schizophrenia. A total of 8 daily caregivers, directly related to caring for individuals with schizophrenia, were recruited. The thematic analysis yielded 5 central themes:
1) Family’s experience in taking care of individuals with schizophrenia:
In general, participants could identify the symptoms experienced by individuals with schizophrenia, predominantly the positive symptoms (i.e., hallucination, talking or giggling by themselves, being irritable or even violent). Yet, all participants did not realize that self-withdrawal, unable to take care of one’s self, lack of motivation, and lack of talking/socialization, are also part of the symptoms. When patients were agitated, all caregivers were terrified and half (n=4) would first call shaman (dukun, orang pintar) or preachers for help. Relapse situation often makes it difficult for family caregivers to entirely trust the medical treatment, so 2 of the caregivers reported routinely bringing the patient to the shaman and only going to the hospital when positive symptoms reappear.
2) Stigma during taking care:
All of the participants reported experiencing direct discrimination, both from their own family as well as society. Individuals with schizophrenia are generally known as crazy or considered unlucky. Most people avoid these individuals because they are worried about contamination. Families also have a hard time bringing the individuals who are in treatment to mingle in society, since many of them drop out of school and cannot work, as well as do not play any role in society. Families of individuals with schizophrenia are also ostracized by other family members, they are considered humiliating, and even rarely invited to family events.
3) Burden during taking care:
All of the participants reported experiencing psychological burdens, such as stress as a consequence of the individual’s behavior. Guilt, sadness, anger, and despair have been reported to be experienced by all participants. Six participants confessed that taking care of schizophrenic individuals is also energy-draining because they must help the individuals to bath/eat/defecate daily (there are individuals who will defecate carelessly if they are not reminded), so participants express exhaustion and other physical symptoms (headache, myalgia). The other burden is related to economic issues. Even though all the participants had access to BPJS (Indonesia’s national health insurance), they reported that taking schizophrenic individuals to the hospital requires a lot of money, particularly when the individuals display severe positive symptoms and need to be hospitalized.
4) The belief system in the family:
Having family members with schizophrenia and being caregivers for them were interpreted in different ways by participants. Five of them considered it as punishment from God and admitted to surrendering to the situation, in fact, they said that they would keep surviving and not give up. Three other participants regretted this condition; thus, in order to calm themselves down, they often prayed and attended church service for the purpose of being blessed and reducing the burdensome sins that have resulted in one of the family members suffering from schizophrenia.
5) Support during taking care of individuals with schizophrenia:
Only one participant stated that their neighbors are willing to help when individuals with schizophrenia experience relapse. At the health service facility, all participants have experienced exclusion (i.e., the medical officers running away terrifyingly instead of helping to calm down/manage the individuals, the security officers prohibiting the individual to enter the ER, medical officers tending to be unsympathetic and not interactive at the out-patient clinic, and other people/patients refusing to sit beside the caregivers with schizophrenic patients). Only very little information about the individuals’ treatment has been reported to be received by the family, for example, the information related to how the disease appears, the length of treatment, and the side effects of treatment.
After all of the module sessions were implemented, the test to assess the effectiveness of the family empowerment model in increasing family resilience was conducted. We found that implementing the family empowerment module significantly increased family resilience across all aspects (belief system, family structure, and family communication). A comparison of family resilience before and after the intervention is summarized in Table 4.
| Average Scores (Mean+SD) | Before | After | p-value |
|---|---|---|---|
| Family resilience | 158.53 ± 8.32 | 170.05 ± 12.32 | 0.003 |
| • Belief system | 40.20 ± 6.05 | 60.15 ± 5.25 | 0.001 |
| • Organization pattern | 53.40 ± 2.13 | 54.60 ± 2.12 | 0.705 |
| • Family communication | 50.45 ± 4.20 | 54.25 ± 7.23 | 0.001 |
Table 4 above shows a significant difference between family resilience before and after the implementation of the family empowerment module, exhibiting a p-value of 0.003. Therefore, it can be concluded that there is an impact of the family empowerment model on the family resilience of individuals with schizophrenia.
4. DISCUSSION
This study has observed that participants taking care of individuals with schizophrenia are faced with many obstacles, such as emotional, physical, and economic burdens. The emotional burden comes in the form of boredom, sad, stress, anxiety, annoyance, and feeling forced. Participants have also reported experiencing economic struggles related to the expensive cost of treatment. This is in line with a study by Urizar et al., which stated that the burden in taking care of individuals with schizophrenia includes objective burden (related to the negative impact that is experienced by the family, i.e., expensive cost of treatment and fulfilling daily needs of schizophrenic individuals), and subjective burden (related to sadness, feeling lost and worried) [21]. Feeling sad is a normal reaction when someone experiences losing another person or something they love. Individuals with schizophrenia have a thought disorder that poses a difficulty for them in doing normal activities, resulting in finding it difficult to live independently without people's help. These dramatic changes can also reflect a sense of loss, experienced by participating caregivers, as they lose their loved ones to schizophrenia. This causes family caregivers to eventually worry over the conditions and future of their loved ones living with schizophrenia [22].
Factors significantly associated with lower resilience in this study were older age, widowhood, lower education level, unemployed status, lower income, and more frequent relapses. In this study, older age was associated with lower resilience. In older individuals, there is an increased sensitivity to environmental impacts, which then causes individuals to become more vulnerable to change. The influence of social and environmental factors and subjective perceptions of declining health have been associated with decreased psychological resilience in the elderly [23]. The findings in this study have also shown that widowhood status affects resilience, which is in line with previous literature stating that widowhood is a phenomenon that is intimately linked to loneliness and a lack of social support, as well as dysfunctional coping and avoidance methods, all of which contribute to poor mental health. Although elevated depression symptoms are common following widowhood, they may signal a problem with adaption because they are related to poor long-term physical and mental health outcomes. Acceptance of death in a neutral state and a sense of control over death may enhance adaptation to the changing demands of widowhood throughout time, supporting initial resilience and eventual recovery. Lower levels of maladaptive avoidant coping may help to explain the link between neutral death acceptance and early bereavement resilience [24, 25]. Lower education level has been found to be associated with lower resilience in this study, which is in line with research by Deng et al., who found that lower educational attainment may explain deficiencies in resilience [26]. Conversely, a higher educational level is associated with better resilience. Higher levels of education have been linked to improved medical knowledge, allowing individuals to access coping techniques and resources, social support, and problem-solving and cognitive abilities to deal with negative health implications, such as stress. Knowledge as a success promoter is a potent individual factor that can boost resilience [27, 28]. Employment status has been linked to an increase in external resources, and access to external resources, such as financial assistance, has been highlighted as critical for career resilience. Employment represents a normal existence and supports functional recovery for many people with schizophrenia and other serious mental disorders, allowing them to build self-esteem, gain meaningful social integration, shed the stigmatized identity of a mental patient, and become more self-sufficient [29, 30]. Accordingly, unemployment was found to be related to lower resilience in this study. Resilience is a critical element in maintaining remission and reducing recurrence in schizophrenia patients. Carers of patients with schizophrenia experience a similar phenomenon, as living with schizophrenic patients can be a difficult scenario due to the chronicity and severity of the disease. Frequent relapses have been linked to pessimism and a lack of involvement in the relationship, which is thought to be a barrier to family resilience, which is consistent with the findings of this study that families with the lower resilience experience more frequent relapse episode [22, 31].
Financial circumstances may also become a burden in taking care of individuals with schizophrenia. Medication and taking care of individuals with schizophrenia cost a lot of money [32]. The family has an economic function where the family members must be capable of providing financial resources and allocate them to fulfill the family’s needs, as well as the need for healthcare [33]. In general, individuals with schizophrenia seek treatment by using healthcare insurance (i.e., BPJS in Indonesia); however, certain limitations may vary, such as limited treatment options and limited healthcare facilities that can be appointed. The caregivers also need transportation to the healthcare facility, which also involves cost. This poses a difficulty for the patients and their families to visit the healthcare facility for regular appointments.
Therefore, family empowerment is required to strengthen the family of schizophrenic patients so that the family members can endure such conditions. Family empowerment is a mechanism that encourages transformation in the family’s ability and skill, centering on family culture, which affects the family’s therapeutic behavior and dynamics [34]. Increasing resilience can improve the ability of the family to adapt to the disease by managing stress and anxiety [35]. The implementation of the module described in this paper has served this purpose. Material 1 is based on helping the family to refocus on planning, hence being able to take care of individuals with schizophrenia, while material 2 focuses on perspective adoption. We have, herein, tried to educate family caregivers with a peer group discussion session so that they can attain a variety of perspectives from other family caregivers who also have similar experiences as theirs. It was thought that this session would help family caregivers overcome their anxiety or anger. Material 3 of the module focuses on improving ability; family caregivers have been taught to identify agitation and decide whether or not to practice restraint, and they were also taught to be able to practice restraint if needed. We collaborated with hospital security and healthcare professionals at the emergency unit and psychiatry clinic as well.
CONCLUSION
This present study indicates that taking care of schizophrenic individuals poses a burden for the family and, hence, this may negatively affect family resilience. Implementation of the family empowerment module has helped in increasing family resilience. We suggest that this implementation be carried out in other county hospitals as well, having similar relatable situations.
AUTHOR’S CONTRIBUTION
EE as the corresponding author conceived and designed the study and was a major contributor to the research, as well as writing of the original and revised draft. Initial conceptualization, methodology, and validation were conducted by MMA. SAM helped with data collection and interpretation of the statistical data obtained in the study. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript. All authors have also read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This present study has gained approval from the Institutional Review Board of Universitas Sumatra Utara with statement letter number 281/KEPK/USU2022.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees, and with the Declaration of Helsinki.
CONSENT FOR PUBLICATION
Before participation, an informed consent has been obtained from each subject.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
Data and materials of this study can be requested for appropriate purposes directly from the corresponding author [E.E].
FUNDING
This study was funded by the TALENTA grant from Universitas Sumatra Utara with contract number 300/UN5.2.3.1/PPM/KP-TALENTA/2022.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGEMENTS
The authors are thankful to all resident doctors of the Department of Psychiatry, Faculty of Medicine, Universitas Sumatra Utara, for their contributions to this study.


