All published articles of this journal are available on ScienceDirect.
Current Knowledge and Attitude to Exclusive Breastfeeding Practice among Lactating Mothers Visiting a Health Facility in Lagos State, Nigeria
Abstract
Background:
Information about maternal knowledge and attitude toward exclusive breastfeeding (EBF) practice is consequential to the actualization of the goals of the baby-friendly initiative and Millennium Development Goals (MDGs) 4 and 5. This paper assessed the current knowledge and attitude of EBF practices among nursing mothers attending a health facility in Lagos, Nigeria.
Methods:
The study employed a descriptive cross-sectional descriptive design. One hundred and twenty (120) nursing mothers attending the Isheri Olofin Primary Health Centre (IOPHC) and currently breastfeeding children between 0-24 months were interviewed. A pre-tested questionnaire that elicits information on maternal socio-demographic characteristics, child index, 24-point knowledge scale, 30-point attitude scale, and 12-point practice scale of EBF was employed. Data was analysed using descriptive, Chi-square, and adjusted odd ratios (aORs) generated from a logistic regression model.
Results:
About 89.2% of the respondents demonstrated good knowledge, while 81.7% depicted a positive attitude. All respondents (100%) had heard about EBF. About 86.7% believed that EBF is only adequate in the first six months of a newborn baby. Respondents with good knowledge of EBF were 3 folds more likely to have good EBF practice than those with poor knowledge (aOR=3.07, 95% confidence interval [CI]: 1.74, 9.52), while those with a positive attitude towards EBF were twice as likely to have good EBF practice than those with a negative attitude (aOR=2.17, 95% CI: 1.16, 5.73).
Conclusion:
Respondents had good knowledge and a positive attitude towards EBF practice. The study also affirmed a strong relationship between maternal EBF knowledge and attitude and current practice among the respondents.
Highlights:
Respondents exhibited good knowledge and a positive attitude toward exclusive breastfeeding (EBF) practice.
Respondents initiated breastfeeding within 24hrs of birth and fed their infants with colostrum.
Current practices have a significant relationship with maternal EBF knowledge and maternal attitude.
1. INTRODUCTION
The World Health Assembly (WHA) has set a global objective to increase exclusive breastfeeding (EBF) for infants 0 to 6 months of age to at least 50% between the years of 2012 and 2025 [1]. Only 38% of newborns are exclusively breastfed for the first six months of their lives globally, with variations by nations [1, 2]. Compared to poorer economies, breastfeeding is often stopped earlier in high-income countries like the United States (19%), the United Kingdom (1%), and Australia (15%) [3]. Nevertheless, only 37% of infants younger than six months are exclusively breastfed, even in low- and middle-income countries [4]. Recent papers in the sub-Saharan Africa region [5] stated that only 53.5% of newborns in East African nations had EBF for six months, which is much less than the WHO aim of 90% [6].
With a population of 220,277,215 or 2.64% of the world's population, Nigeria is the most populated black country in the world. The most recent estimate of Nigeria's Gross Domestic Product (GDP) per capita was $2429.59 in December, 2021. Its GDP per capita is equal to 19% of the average for the entire world. In the 2022 Gini coefficient study of wealth inequality, the nation received a score of 35.1. The country's estimated median income is equal to €PPP7,600, or $1,895,630, for the entire population. Nigeria has a life expectancy at birth of 60.87% and health expenditure as a percentage of GDP of 3.03% [7]. The act of breastfeeding has been a major part of infant nutrition in Nigeria, similar to what is available in other West African countries, but EBF practice is low. Data from the Multiple Indicator Cluster Survey [8] and the National Demographic Health Survey (NDHS) [9] demonstrated that the proportion of nursing mothers in Nigeria who practice EBF decreased from 17% in 2004 to 13% in 2018. The aforementioned clarifies the high rate of baby malnutrition and mortality observed in countries with weak economies, which is partially due to ineffective infant feeding techniques. According to previous studies, one-third of malnutrition cases seen in various settings around the world are caused by infants' incorrect feeding behavior combined with other factors like infection and a lack of food [10-14]. Numerous studies have found that complementary feeding (CF) introduced to infants before they were 4 months old or after they were 8 months old increased their risk of malnutrition, atopic disease development, gastrointestinal infections, obesity, and even adult chronic disease [11-14]. These findings were found in both Westernized countries and settings with limited resources.
According to numerous studies, cultural, socio-demographic, psychological, and biophysical factors (such as education, occupation, cultural beliefs, family support, and spouse support) have a significant impact on breastfeeding knowledge and practice in various societies [15, 16]. To optimize the benefits of the baby-friendly program, information on the knowledge and attitudes of EBF is needed, as these factors may operate as facilitators and consequently support its practices [17]. Mothers' positive attitudes and expertise are conducive to breastfeeding [18]. Mothers who were moreaware of EBF were 5.9 times more likely to practice it than their peers, as per a prior study (OR 5.9; 95% CI 2.6, 13.3; p 0.001) [19]. Additionally, a higher prevalence of exclusive breastfeeding was associated with higher scores on the knowledge, attitude, and practice control scales for breastfeeding [20]. As a result, several studies have examined the knowledge, attitudes, and practices around breastfeeding in many parts of the world; however, such studies are rare among Nigerian women [21-24]. Furthermore, observational reports on breastfeeding practices among nursing mothers in West Africa also seem to be scarce. As a result, this study is an important intervention that fills a knowledge vacuum for public health professionals, community health workers, and other EBF campaign stakeholders. The purpose of this study was to investigate breastfeeding mothers' current knowledge, attitudes, and behaviors about exclusive breastfeeding (EBF) at a postnatal, child welfare, and immunization clinic at a health center in Lagos, Nigeria.
2. MATERIALS AND METHODS
2.1. Study Design and Settings
The study was a cross-sectional survey conducted among nursing mothers utilizing the Isheri Olofin Primary Health Centre (IOPHC) in the Lagos State, Nigeria, Alimosho Local Government Area (LGA) of Egbe/Idimu Local Council Development Area (LCDA). Lagos State is located in the Western part of Nigeria and bordered by Benin Republic on the West, Ogun State, both in the North and Eastern parts, and the Atlantic Ocean in the south. It serves as a commercial nerve center and residential area for all Nigerians. Lagos State is the smallest state in Nigeria, yet it has the highest urban population, which is 27.4% of the national estimate (UN-Habitat). Administratively, it is divided into twenty (20) local government and thirty-seven (37) local council development areas, respectively, in accordance with Nigeria’s federal structure and the need to bring governance, development and participatory democracy to the grassroots. Statistics from the Healthcare Facilities Monitoring and Accreditation Agency, HEFAMAA, reported that in Lagos, there are 26 registered general hospitals, 329 public healthcare centers, 2,886 private hospitals or specialist clinics and laboratories or diagnostics centers in addition to an estimated 160 tradomedical centers [25].
2.2. Study Population
Mothers who are currently breastfeeding their children and who visit the postnatal clinic, vaccination unit, family planning unit, special care baby unit, and children outpatient clinic at IOPHC made up the study population. One hundred and eighty-seven (187) registered nursing mothers were present at the clinic. However, in order to provide adequate treatment due to space and staffing constraints, an average of twenty (20) nursing moms were seen each week. The Nigerian female population was estimated to be 109,047,418 in 2023, making up 49.4% of the nation's overall population, according to the United Nations Department of Economic and Social Affairs [26]. Women between the ages of 15 and 49 who are fertile are estimated to number 65 million.
2.3. Eligibility Criteria
The following factors were taken into account when choosing study participants:
• Must be breastfeeding mothers, with the youngest kid between 0 and 2 years old.
• Be a registered patient at the chosen medical center (IOPHC).
• Must have given permission to take part in the study.
• Not having any of the following medical conditions, such as galactosemia, HIV (not receiving antiretroviral therapy), HTLV-1/2 (human T-cell lymphotropic virus type I or type II), suspected or confirmed Ebola virus disease, or abusing illicit drugs like PCP (phencyclidine), cocaine, or opioids, which are contraindications to breastfeeding or feeding expressed breast milk.
2.4. Sample and Sample Size Determination
According to the information from the facility health record, there were a total of 187 registered nursing mothers present at the IOPHC when the study was being conducted. Only one hundred and twenty (120) of the respondents correctly filled out the questionnaires out of the sample frame's total of 133 participants who agreed to participate in the study. With the help of the health record officer, the names of the consented respondents were noted in the register to prevent the gathering of data from the same respondents twice or more.
2.5. Sampling Technique
During the study period, at each clinic visit, eligible individuals who expressed interest and gave their agreement to participate in the study were enrolled using a non-probability sampling (total sampling) technique. This involved the purposive selection of the entire population (nursing mothers) visiting the IOPHC at the time of study and who met the eligibility criteria. This sampling technique makes it possible to get deep insights into the phenomenon and make analytical generalizations about the population being studied. With such wide coverage of the population of interest, there is also a reduced risk of missing potential insights from members who are not included.
2.6. Definition of Variables
The study chose the following operational terms, which served as the foundation for developing the instrument in this regard:
2.6.1. Knowledge
Gained by nursing mothers through experience or education, facts or information on exclusive breastfeeding.
2.6.2. Attitude
A consistent way of thinking, feeling, or temperament by nursing mothers towards exclusive breastfeeding. Nursing mothers' propensity for or disposition toward EBF, especially in their minds.
2.6.3. Practices
Actual implementation or application of a theory or conviction that supports or aids exclusive breastfeeding among nursing mothers.
2.6.4. Good Practice
A technique that is recommended as a model because it is both good and has been shown to function well and have positive results.
2.7. Instrument for Data Collection
A pre-tested, structured, self-administered questionnaire was used to collect the data. The authors updated and adopted the questions from an earlier study [16]. The questionnaire's components were divided into five (5) sections: Section A, which asked about the respondents' socio-demographic characteristics; Section B, which asked about the respondents' children; Section C, which asked about the respondents' knowledge of EBF; Section D, which asked about the respondents' attitudes toward EBF; and Section E, which asked about the respondents' infant feeding practices.
a) Socio-demographic characteristics: This part featured information on factors, including age at last birthday, sex, ethnicity, educational level, marital status, kind of marriage, and religion.
b) Child's vital information: Age, birth order, and sex of the child.
c) Knowledge: The respondent's level of EBF knowledge is assessed in this area. EBF knowledge was divided into good and poor knowledge categories. A total of 26 points were awarded for correctly answering each of the thirteen (13) questions based on EBF knowledge. The 50th percentile (the mean) served as the benchmark for classifying knowledge as low or good. Based on prior research, the scoring and pass marks were determined.
d) Attitude: The purpose of this section is to ascertain the respondents' attitudes toward EBF. Positive and negative attitudes were used to categorize respondents' responses to EBF. The attitude scores were based on 10 items, with each correct response worth 3 points. The total score was 30 points. For scoring the negative/positive attitude, the 50th percentile was chosen as the reference point. The scoring system and passing grades were based on prior research.
e) Exclusive breastfeeding/current infant feeding practices of mothers: This is done to ascertain whether EBF is used and, if not, why. Poor and good practices were distinguished between the responses. EBF practice was evaluated using 7 items, with the correct responses earning 2 points each, for a total of 14 points. The 50th percentile served as the benchmark for classifying practices as bad or good. The scoring system and passing grades were based on prior research.
2.8. Validity and Reliability of the Instrument
A copy of the questionnaire was submitted to the research supervisor for modification in order to assess the instrument's validity. The study's validity was based on both face validity and content validity. The study supervisor and specialists in the field carefully examined the questionnaire to ensure its applicability to the topic at hand, as well as its scope and content.
The test-retest methodology was employed to assess reliability. The questionnaires were administered to twelve nursing mothers who visited the Egan Primary Health Centre in Lagos and shared similar characteristics with the study population, thus constituting 10% of the sample size as advised by earlier studies [27, 28]. Utilizing pre-testing, the consistency of the questionnaire was examined. The questionnaires were slightly modified as follows: modifications were made to two knowledge-related items, two attitude-related items, and three EBF practice items. Only semantic modifications were made. The revised questions were put to a new test. The pre-test's reliability value was 0.86, which demonstrated the validity of the questionnaire.
2.9. Data Collection Procedure
The questionnaires were self-administered over the ten (10) week data collection period, which ran from mid-March to mid-May, 2022.
2.10. Data Management and Statistical Analysis
The questionnaires were thoroughly reviewed for completeness after data collection. Using IBM Statistical Product and Service Solutions version 24 (SPSS, Inc.; USA), the manually entered data was analyzed. Results were reported using frequency tables, percentages, charts, and descriptive statistics (mean and standard deviation).
Inferential statistics Chi-square (χ2) was used to test for association between the independent variables (respondents’ knowledge and attitude) and the outcome variable (EBF practice). Also, a multiple logistic regression model was used to predict if the level of knowledge and attitude of respondents (nursing mothers) influence EBF practices. Statistical significance was placed at one-tailed, with a p-value less than 0.05 for all inferential analyses.
2.11. Ethical Considerations
Approval for the study was also obtained from the Local Authority of the Primary Health Care Board, Lagos State. Informed consent was obtained from individual participants before the commencement of data collection. In addition, respondents were informed of their right to voluntarily participate or withdraw from the study at any stage without adverse consequences. Confidentiality was also observed as the questionnaire bore no name of the respondent or any identifying information.
3. RESULTS
A total of 133 questionnaires were administered, of which only 120 were completed, correctly filled, returned, and subsequently analysed, giving a response rate of 90%.
3.1. Socio-demographic Characteristics of Nursing Mothers and Information on Respondents’ Child
A total of 120 nursing mothers were interviewed. The mean age of respondents was 28.7 ± 2.3 years. Almost 119 (99.2%) of the respondents were married, and 111 (92.5%) were in a monogamous marriage. One hundred and sixteen (96.7%) of the respondents had secondary education and above (Table 1).
| Variables | Frequency (N=120) | Percentage (%) |
|---|---|---|
|
Age Group (year) ≤29 30-34 ≥35 |
62 39 19 |
51.7 32.5 15.8 |
|
Marital Status Married Divorced/Widow/Separated/Co-habiting |
119 1 |
99.2 0.8 |
|
Types of Relationship Monogamous Polygamous |
111 9 |
92.5 7.5 |
|
Religion Christianity Islam Traditionalists (Idol worshipper, ritual practices) |
97 22 1 |
80.8 18.3 0.8 |
|
Ethnicity Yoruba Igbo Hausa Others |
63 29 6 22 |
52.5 24.2 5.0 18.3 |
|
Educational Status Primary Secondary Tertiary Postgraduate |
4 44 63 9 |
3.3 36.7 52.5 7.5 |
|
Residence Rural Urban |
12 108 |
10.0 90.0 |
|
Occupation Full-time housewife Trader Artisan Civil servant |
16 44 19 41 |
13.3 36.7 15.8 34.2 |
|
Number of living children 1 2 3 ≥4 |
37 38 31 14 |
30.8 31.7 25.8 11.7 |
|
Youngest Child Age <6 months 6 months – <12 months 12 – 24 months |
73 33 14 |
60.8 27.5 11.7 |
|
Youngest Child Birth Position First Second Third Fourth Fifth and above |
34 42 33 9 2 |
28.3 35.0 27.5 7.5 1.7 |
|
Youngest Child Sex Male Female |
63 57 |
52.5 47.5 |
|
Nature/Type of Delivery Normal delivery Surgical operation Traditional birth attendant |
101 17 2 |
84.2 14.2 1.6 |
Table 1 presents that 73 (60.8%) of the respondent’s children were less than 6 months of age, with a mean age of 90.4±7.1 days. There was a higher proportion of male children, i.e., 63 (52.5%), and the majority, i.e., 101 (84.2%), of the respondents had their child through vaginal delivery.
3.2. Knowledge of EBF among Respondents
The results in Table 2 showed that all the respondents, i.e., 120 (100%), had heard about EBF and the majority, i.e., 100 (83.3%), knew that breastfeeding should be initiated immediately after delivery without giving any other thing. Most, i.e., 106 (88.3%), reported that EBF is feeding the child with colostrums (first milk) and continuation with breast milk for the next six months. All of the respondents, i.e., 120 (100%), knew that EBF bonds mother and child together, and it gives protection against childhood diseases.
3.3. Knowledge Level of Respondents on EBF Practice
One hundred and seven (89.2%) respondents had a good knowledge of EBF, while 13 (10.8%) had poor knowledge of EBF (Fig. 1).
| Statement | Yes (%) | No (%) |
|---|---|---|
| Heard about exclusive breastfeeding | 120 (100.0) | 0 (0.0) |
| What exclusive breastfeeding is: Initiation of breastfeeding at any time after birth | 120 (100.0) | 0 (0.0) |
| Initiation of breastfeeding immediately after delivery without giving any other thing | 100 (83.3) | 20 (16.7) |
| Breastfeeding with the addition of water, glucose, or herb | 23 (19.2) | 97 (80.8) |
| Giving breast milk only from birth | 112 (93.3) | 8 (6.7) |
| Feeding the child with colostrums (first milk) and continuation with breast milk for the next six months | 106 (88.3) | 14 (11.7) |
| Giving grape water with breast milk immediately after birth | 18 (15.0) | 102 (85.0) |
| It is a natural food that costs no money, or unnecessary labour/stress to the mother | 120 (100.0) | 0 (0.0) |
| It bonds the mother and the child together | 120 (100.0) | 0 (0.0) |
| It is time-consuming and causes stress | 0 (0.0) | 120 (100) |
| Breast milk is not enough to satisfy hunger and thirsty | 36 (30.0) | 84 (70.0) |
| It gives protection against childhood diseases | 120 (100.0) | 0 (0.0) |
| It causes stunted growth in babies | 0 (0.0) | 120 (100.0) |
3.4. Attitude of Respondents towards EBF Practice
Ninety-seven (80.8%) of the respondents disagreed that infants should be given other fluids other than breast milk. Almost all the respondents agreed on the following items: EBF is only adequate in the first six months (104; 86.7%), and EBF babies develop healthier than infant-formula-fed babies (116; 96.7%) (Table 3).
3.5. Attitude Level of Respondents towards EBF Practice
Fig. (2) presents the attitudinal level of the respondents. Most of the respondents (98; 81.7%) had a positive attitude towards EBF practice.
3.6. Respondents' Infant Feeding Practice
The proportion of respondents that gave their infants breast milk only in the first 24 hours and 72 hours of birth were 109 (90.8%) and 97 (80.8%), respectively. About 69 (57.5%) of the respondents reported giving their infants breast milk on demand. One hundred and thirteen (94.2%) respondents reported feeding their infants with colostrums. Sixty-six (55.0%) reported giving their infants expressed breast milk if they stayed away for a long period, as mentioned in Table 4. Overall, 82 (68.3%) of the respondents had a good current EBF practice level.
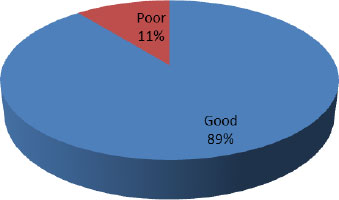
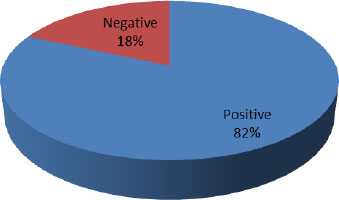
Table 3.
| Statement | Agree (%) | Not Sure (%) | Disagree (%) |
|---|---|---|---|
| Do you agree that EBF is only adequate in the first six months for a child? | 104 (86.7) | 5 (4.2) | 11 (9.1) |
| Do you believe EBF serves as an immunity to the child for the first six months of life? | 118 (98.3) | 2 (1.7) | 0 (0.0) |
| Do you think EBF babies grow healthier than formula-fed babies? | 116 (96.7) | 0 (0) | 4 (3.3) |
| Do you think EBF is time-consuming and more demanding? | 33 (27.5) | 0 (0.0) | 87 (72.5) |
| Do you believe that the first milk (colostrum) should be given to infants? | 98 (81.7) | 0 (0.0) | 22 (18.3) |
| Do you think babies should be given other fluids, e.g., water, glucose, etc., other than breast? | 16 (13.3) | 7 (5.8) | 97 (80.8) |
| Do you think mothers can breastfeed exclusively, even at work? | 105 (87.5) | 2 (1.7) | 13 (10.8) |
| Do you believe that EBF can help a mother maintain a good body and breast shape? | 59 (49.2) | 32 (26.7) | 29 (24.2) |
| Does EBF increase mother-infant bonding? | 116 (96.7) | 4 (3.3) | 0 (0.0) |
| Do you think EBF can be done without any financial cost? | 117 (97.5) | 3 (2.5) | 0 (0.0) |
| Infant Feeding Practice | Frequency (N=120) | Percentage (%) |
|---|---|---|
|
Food received by respondents' child in the first 24 hours of birth Breast Milk only Water only Water with glucose Nothing |
109 5 3 3 |
90.8 4.2 2.5 2.5 |
|
Food received by respondents' child in the first 72hrs of birth Breast milk only Breast milk with water Baby formula (S.M.A etc.) |
97 16 7 |
80.8 13.3 5.8 |
|
How often do you feed your child with breast milk? On-demand Randomly |
69 51 |
57.5 42.5 |
|
Did you feed this child with colostrum (first milk)? Yes No |
113 7 |
94.2 5.8 |
|
Do you breastfeed your baby exclusively? Yes No |
120 0 |
100.0 0.0 |
|
Have you given your last baby anything before initiating breastfeeding (Prelacteal food)? Yes No |
0 120 |
0.0 100.0 |
|
If you have to stay away from your infant for a long period, what feed will you make available for the baby? Formula food Expressed breast milk Water only |
48 66 6 |
40.0 55.0 5.0 |
3.7. Knowledge and Attitudes of Respondents towards Exclusive Breastfeeding (EBF) Practice
As mentioned in Table 5, there was a statistically significant relationship between respondents’ knowledge and EBF practice (p=0.00). The association between respondents’ attitudes and EBF practice was also significant (p=0.00). A higher proportion, i.e., 79 (73.83%), of those with good knowledge of EBF had good EBF practice compared to those with poor knowledge, i.e., 3 (p=0.00). About 74 (75.51%) of respondents with positive attitudes towards EBF had good EBF practice compared to 8 (36.36%) of those with negative attitudes (p=0.00).
3.8. Logistic Regression Model for EBF Practice
Table 6 presents that respondents with good knowledge of EBF were three times more likely to display good EBF practice than those with poor knowledge (OR=3.07, 95% CI: 1.74, 9.52), while those with a positive attitude towards EBF were twice more probable to have good EBF practice compared to those with a negative attitude (OR=2.17, 95% CI: 1.16, 5.73).
Table 5.
| - | Exclusive Breastfeeding Practice level | Total | Chi-square (χ2) | p-value | |
|---|---|---|---|---|---|
| - | Good | Poor | - | - | - |
| - | - | - | - | - | - |
|
Knowledge of EBF Good Poor |
79 (73.83) 3 (23.08) |
28 (26.17) 10 (76.92) |
107 (100) 13 (100) |
21. 08 | 0.00 |
|
Attitude to Exclusive Breastfeeding Positive attitude Negative attitude |
74 (75.51) 8 (36.36) |
24 (24.49) 14 (63.64) |
98 (100) 22 (100) |
17.69 | 0.00 |
| Characteristics | Adjusted Odds Ratio | 95% Confidence Interval | p-value | |
|---|---|---|---|---|
| - | - | Lower | Upper | - |
|
Knowledge on EBF Good Poor (ref) |
3.07 | 1.74 | 9.52 | 0.002* |
|
Attitude to EBF Positive attitude Negative attitude (ref) |
2.17 | 1.16 | 5.73 | 0.001* |
*Significant at p<0.05.
4. DISCUSSION
In this study, the opinions and current knowledge of 120 nursing mothers who visited the Isheri Olofin Primary Health Centre (IOPHC) in Lagos State, Nigeria, were assessed. The results of this study indicated that a larger percentage of respondents had a good awareness of EBF and that their attitudes regarding EBF were generally favourable. However, compared to WHO recommendations, the degree of existing EBF practice was below average. The results of the current study showed that people are more likely to practice EBF if they have good knowledge about it and a positive attitude toward it. The study also demonstrated a strong association between mother attitudes and knowledge and EBF practice.
The results showed that respondents had great levels of nursing knowledge on breastfeeding. This finding was consistent with the findings from other regions of the nation (Nigeria), including Owerri [29], Anambra [30], the Plateau, the North-Central [21, 31], and western Nigeria [32, 33]. The baby-friendly initiative program at the research location can be credited for the high degree of awareness regarding healthy breastfeeding and EBF among respondents. The majority of respondents in this study learned about EBF from healthcare facilities. In agreement with this study, several studies have found that baby-friendly hospitals are an essential channel for the distribution of information about breastfeeding [34, 35]. According to the findings of a study by Bartington et al. [36], mothers who give birth at baby-friendly medical facilities are much more likely to start breastfeeding than mothers who deliver elsewhere. Our results essentially refuted the conclusions of a study by Oche et al. [23], who claimed that their respondents had low levels of awareness.
International organizations have recommended the hour after delivery as the ideal time to start breastfeeding [37]. The value of maternal breastfeeding expertise has been supported by research [38, 39]. Despite the considerable percentage of mothers in this study who were very aware of starting breastfeeding within an hour of delivery, this percentage is still significantly lower than what Adhikari [40] revealed. This survey showed that a larger percentage of the respondents had sufficient knowledge of breastfeeding. This result was consistent with earlier research done in Nigeria, where it was found that breastfeeding mothers had a strong understanding of EBF [22-24, 30]. The majority of the respondents in this survey agreed with the following statements, which were consistent with previous studies on breastfeeding knowledge: breastfeeding fosters the mother-child bond [41], regular breastfeeding beginning in infancy can help reduce the incidence of jaundice (prevent childhood diseases) [42], and breastfed infants exhibit growth patterns that differ noticeably from those of formula-fed babies [43]. Hence, EBF was primarily thought by the respondents to benefit mother-child relationships, provide immunity against diseases that affect children, help babies develop healthier than they would from infant feeding formula, and be naturally accessible and free of charge.
This survey showed that a sizable fraction of the participants demonstrated a positive attitude towards breastfeeding. Optimal EBF practice and a supportive attitude toward breastfeeding have been linked explicitly in studies [44, 45]. It has been stated that good parental attitudes toward baby feeding are an essential component of a child's nutritional well-being [46]. Perceptions that breastfeeding is more convenient than infant formula, less expensive, provides immunity, strengthens mother-child bonds, and that breastfeeding is preferred over infant formula by health professionals were the study's major facilitators in assessing attitudes toward breastfeeding. Additionally, it was shown in this study that mothers' perceptions toward the claim that exclusively breastfed infants develop more healthfully than babies who are fed formula were in line with the findings of a study by Singh [47]. Numerous experts have pointed to a number of reasons as the cause of the varying attitudes mothers exhibit regarding breastfeeding. These include encouragement from a spouse, friend, or member of the family [48], worry about a lack of milk supply [17, 23], the connection between breastfeeding and sagging breasts [17, 49], and psychological and sociocultural factors [50, 17].
The important role that a mother's knowledge plays in assisting with newborn feeding practices has been articulated in previous studies [49-51]. According to the results of the current survey, there is a substantial link between mothers' understanding of EBF and the practices that follow regarding infant feeding. This result, however, deviates from earlier studies carried out in Nigeria, which found no link between breastfeeding habits and knowledge [25, 52]. Additionally, the study found a significant correlation between respondents' attitudes and EBF practice. This conclusion is in line with a report by Singh [47]. The results of the study's regression analysis showed that mothers who have high knowledge of EBF are three (3) times as likely to practice it as mothers who have poor knowledge. Similar to this, those who have a positive attitude about EBF are twice as likely to engage in good EBF as people who have a negative attitude.
According to the authors, “if baby-friendly hospitals improve the conditions for all women to breastfeed, then it would be predicted that those with typically lower BF rates would have above-average BF rates in the BFHI setting” [53]. In contrast, previous studies [54, 55] found no appreciable difference in the prevalence of EBF for infants delivered in BFHI maternity facilities compared to non-BFHI maternity facilities for mothers who were typically less likely to BF or EBF (mothers with lower education, no labor income, caesarean section, no BF decision prior to pregnancy). Furthermore, rates were higher in BFHI maternity facilities for women who delivered vaginally, delivered babies at term, chose their baby's feeding method before getting pregnant, and belonged to families with at least one wage earner. Frequently, increased BF rates accompany these “beneficial” characteristics [56, 15]. In such favourable circumstances, the BFHI maternity facilities could act as a catalyst, strengthening the women's pre-existing beliefs. Prospective studies are necessary [53, 57] to identify the factors that influence BF rates in hospitals that serve newborns. Like these authors, we think that a global rate-tracking system is crucial for determining the efficacy of the BFHI strategy as well as for monitoring all of the various aspects of its implementation. Without such information, it is impossible to monitor progress over time efficiently.
5. LIMITATIONS OF THIS STUDY
Despite the great response rate recorded in this study, there are some limitations to this research. First, because the data for this study came from only one (1) health institution, there are contextual differences that prevent conclusions from this survey from being applied to all nursing mothers in Lagos State or the entire nation. Second, thirteen (13) surveys were filled out incorrectly, making it impossible to analyze them. Thirdly, there was no provision for respondents to offer comments or express their viewpoints in addition to the questions that were asked; the survey was strictly quantitative. Therefore, in order to improve findings in this area, future research should use a qualitative methodology like focus group discussion (FGD). Fourth, the fact that the study was carried out at a BFHI health center may have had an impact on its findings (knowledge, attitude, and practices linked to EBF). Last but not least, the study used a cross-sectional study design, making it impossible to establish causal links between variables.
6. IMPLICATIONS OF FINDINGS AND RECOMMENDATIONS
The findings from this study have many implications for public health. First, having a high level of maternal understanding of EBF, its length, and its perceived benefits may make it easier for women to breastfeed their babies exclusively for six months. Second, mothers who have a favorable attitude toward breastfeeding are more likely to sustain it for a longer time and have a successful EBF for six months.
Regardless of the good knowledge, positive attitude and appreciable level of current EBF practice exhibited by respondents in this study, there is still an urgent need to improve the status quo in the health facility. First and foremost, the Medical Officer of Health (MOH) should develop more initiatives and plans to inform caregivers and nursing mothers about the value of EBF and its advantages. They should be informed of the risks and negative effects of improper newborn feeding techniques. Second, it is important to increase the implementation of treatments designed to increase mothers' self-confidence and dispel their misconceptions about expressing and preserving breast milk. Last but not least, the data on the state of infant feeding practices at the moment need immediate action to assess the materials for educating mothers and family members to better understand the advantages of nursing and encourage mothers to nurse infants exclusively for six months.
CONCLUSION
This study found that respondents had a good knowledge of EBF practice and a positive attitude toward it. Nearly all the respondents started breastfeeding their babies within 24 hours of delivery, and they gave colostrum to the babies. This study also confirmed a significant link between respondents' knowledge, attitudes, and practices regarding maternal EBF. There is still a pressing need to improve the current situation if the Millennium Development Goals (MDGs) 4 and 5 and Sustainable Development Goals (SDGs) 3 are to be realized in the nation, even though respondents in this study demonstrated an appreciable level of current EBF practice.
AUTHORS’ CONTRIBUTION
S.A.M.A. and S.A.A.A contributed to the conceptualization. S.A.M.A., S.A.A.A. and S.A.E.D. contributed to the methodology. S.A.M.A. participated in validation. S.A.M.A. and S.A.A.A. gathered resources. S.A.M.A., S.A.A.A. and S.A.E.D. carried out the investigation. S.A.M.A. contributed to the data curation. S.A.M.A., S.A.A.A., and S.A.E.D. performed data analysis. S.A.M.A. and S.A.A.A contributed to writing the original draft preparation. S.A.M.A., S.A.A.A., S.A.E.D., E.H., E.D.T., O.A.N., and R.C.G. participated in writing the review and editing. All authors read and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| EBF | = Exclusive breastfeeding |
| MDGs | = Millennium Development Goals |
| IOPHC | = Isheri Olofin Primary Health Centre |
| CI | = Confidence interval |
| WHA | = World Health Assembly |
| GDP | = Gross Domestic Product |
| IOPHC | = Isheri Olofin Primary Health Centre |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Local Authority of the Primary Health Care Board, Lagos State.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from individual participants before the commencement of data collection.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The datasets used for the current study are available from the corresponding author [D.E] upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
ACKNOWLEDGEMENTS
The authors are grateful and appreciative to all the nursing mothers who participated in the survey. The authors also extend our profound gratitude to the management and staff of Isheri Olofin Primary Health Centre for their assistance.


