All published articles of this journal are available on ScienceDirect.
Comparing Continuity of Midwifery Care Model with the Mother-child Health Book: Enhancing Knowledge for Adolescent Pregnancy in Indonesia
Abstract
Introduction:
Adolescent pregnancy poses a significant concern in Indonesia, particularly in some regions, namely West Sumatra and Padang City. This issue has been addressed with two prominent approaches, the Continuity of Midwifery Care (CMC) model and the Mother-Child Health (MCH) Book.
Objective:
This study aims to compare the effectiveness of these approaches in enhancing knowledge about adolescent Pregnancy, including several aspects, such as domestic violence, substance risks, reproductive health, pregnancy, childbirth, and parenting roles.
Material and Methods:
A quantitative research approach was applied by utilizing a quasi-experimental design, conducting pre- and post-tests with the validated questionnaires during the third trimester of pregnancy, postpartum days 31 and 43. Conducted in Padang City, the research involved 70 young primiparous mothers, categorized into groups using the CMC model and MCH Book. The collected data analyzed the generalized linear models repeated measures.
Results:
Both groups exhibited a significant knowledge enhancement, with the CMC model yielding more substantial enhancement. The focused and continuous care approach in the CMC model effectively enhanced the knowledge across various aspects, compared to the MCH Book.
Conclusion:
The CMC model stands out as an effective means to enhance knowledge among young pregnant mothers, addressing their distinct challenges during their transition to parenthood. We suggest that the health authorities and policymakers consider the implementation of the CMC model alongside the existing MCH book as a more effective approach to enhance the knowledge of Adolescent mothers.
1. INTRODUCTION
The issue of adolescent pregnancy is a significant public health concern in low and middle-income countries [1]. This problem has far-reaching implications for the health of young mothers, the development of infants, and broader societal impacts [2, 3]. Pregnant adolescents often face stigmatization from various quarters, including their families, peers, society, and even healthcare providers. Besides, they tend to have lower levels of family and social support, leading to reduced access to healthcare facilities [4]. Data from previous studies emphasize that millions of girls aged 15 to 19 years get pregnant every year [5-7].
Maternal mortality rates were alarmingly high in 2020, with approximately 287,000 women losing their lives during or after pregnancy and childbirth. Most of these deaths occurred in low and lower-middle-income countries, with Sub-Saharan Africa and Southern Asia being the hardest-hit regions, collectively accounting for about 87% of the global maternal deaths. Indonesia's maternal mortality ratio decreased from 299 in 2000 to 173 in 2020. However, there was a significant increase in maternal mortality rate in 2021. Women in low-income countries, especially those under the age of 20 years, face a much higher risk of maternal mortality, which is 1 in 49, compared to a ratio of 1 in 5,300 in high-income countries [8, 9]. In fact, these mortality rates are three times higher, compared to women aged 20-24 [10]. The elevated maternal mortality rate among adolescent mothers, within the age range of 15-19 years, required serious attention in this context [4, 11].
World Health Organization (WHO) reported that around 16 million girls aged 15 to 19 years and two million girls under 15 years of age worldwide give birth every year. In impoverished regions, more than one out of three girls becomes a mother before turning 18 years. Nearly 95% of the adolescent births occurred in the low- and middle-income countries [12]. Indonesia faces similar challenges, with an estimated 9.1% prevalence of adolescent pregnancy, meaning approximately 1 in 11 Indonesian adolescents aged 15-19 years have experienced or are experiencing pregnancy [13].
Besides the direct health risks faced by mothers, infants born to adolescent mothers encounter heightened risks. The infant mortality rates within this group are 50% higher than those of infants born to mothers aged 20-29 years. Adolescent pregnancies are also linked to various pregnancy-related complications, including gestational diabetes, anemia, and hypertension disorders [3]. These complications have potentially resulted in premature birth, low birth weight, infant mortality, and respiratory issues in babies [11, 12]. Several factors, namely early marriage, limited access to sexual and reproductive health services, cultural norms, and gender disparities, contribute to the prevalence of adolescent pregnancies [14]. These rates tend to be lower in certain regions within West Sumatra, compared to the national average rate. However, the rates exceed other areas, namely Riau Islands, North Sumatra, Yogyakarta, and the Special Capital region of Jakarta [13, 15]
Confronting these challenges demand a comprehensive approach to address the stigma and negative attitudes towards pregnant adolescents and to ensure their well-being throughout their pregnancy and childbirth processes [16]. The pivotal role of midwifery care in providing education and preventive reproductive health measures for adolescents is widely recognized. Through effective education, midwives can assist adolescents in understanding the implications of early pregnancy, promoting the use of effective contraceptive methods, and providing relevant information on the preparation to be responsible parents. Efforts are underway to address these issues through comprehensive sexual education, access to contraceptives, and support for young mothers to continue their education and access the necessary health services [17]. In the pursuit of enhancing care and support for pregnant adolescents, it often employs two main approaches, namely CMC and the Utilization of MCH book [18, 19].
MCH Book serves as an official guide issued by the Indonesian government for healthcare professionals and pregnant women in all conditions, not specifically for Adolescent pregnancies. This comprehensive guide provides the evidence-based information crucial for the proper care of all pregnant women. It includes standardized examination protocols, health-related guidelines, and indicators of dangers associated with pregnancy, childbirth, and postpartum recovery, as well as the well-being of infants and children. Pregnant women receive the MCH Book during their first Antenatal Care (ANC) visit. They can use it as a valuable reference at home, for sharing essential insights with their families throughout the process of pregnancy and child care. For healthcare professionals, this guidebook holds significant importance for serving as a vital health record, meticulously documenting and monitoring the healthcare services provided to patients. Simultaneously, it functions as a crucial resource within healthcare facilities, by enriching the clinical decision-making process for medical professionals. Furthermore, it facilitates effective communication of critical messages to their clients [20]. In 2021, 90.28% of the deliveries occurred in healthcare facilities, a significant increase attributed to cross-sector support, real-time reporting, regulatory measures, and the issuance of Regulation No. 21 in 2021 by the Ministry of Health, promoting healthcare facility deliveries and services, including ANC and MCH book utilization [21, 22].
The CMC model emphasizes on establishing personal connections between midwives and expectant mothers, ensuring consistent care throughout pregnancy, childbirth, and the postpartum period. This model comprises three main aspects, namely continuity management, informational continuity, and relational continuity. The first aspect, continuity management, involves a consistent, clear, and responsive case management approach following midwifery care guidelines. The second aspect, informational continuity, includes the delivery of relevant information through modules or books covering several topics, such as gender equality, domestic violence, reproductive health, the risks of smoking and substance abuse, as well as preparation for pregnancy and parenthood. This information is typically provided through modules or books that allow pregnant women to learn it at home. Lastly, relational continuity emphasizes on the strong professional relationships within the healthcare team, in which comprehensive midwifery care is provided to pregnant women. The modules and information are gradually provided from the third trimester of pregnancy to the end of the postpartum period. Pregnant women are guided to study this information at home through the provided module, as a part of the informational continuity. Additionally, midwives actively participate in providing health education during visits and offer support through phone calls and WhatsApp messages to address any questions from pregnant women and their families [17].
This study aims to bridge the knowledge gap and identify which approach is more effective in enhancing the knowledge of pregnant adolescents to address crucial issues, namely Domestic Violence, the dangers of smoking, Narcotics, Psychotropic substances, and Addictive substances (NAPZA), reproductive health, pregnancy, childbirth, and parenthood [23]. This research offers a potential approach to promote healthy pregnancies among adolescents, aiming to enhance their success in the role of parenthood. It involves the provision of culturally sensitive and age-appropriate care, to optimize outcomes for both young mothers and their infants and young families [24]. By achieving a more profound understanding of the comparative effectiveness of these two approaches, the study's findings are expected to give concrete recommen- dations for the development of programs and policies focused on enhancing the well-being and preparedness of pregnant adolescents while facing the challenges of parenthood.
2. MATERIALS AND METHODS
2.1. Study Design and Sampling Techniques
This study employed a quantitative research approach, by utilizing a quasi-experimental design with pre-post tests and a control group arrangement. The primary aim is to compare the efficacy of the MCH book and CMC model in enhancing the knowledge of young primiparous mothers. The areas of focus encompass domestic violence, the dangers of smoking, Narcotics, Psychotropic substances, and Addictive substances (NAPZA), reproductive health, pregnancy, childbirth processes, and parenting roles. The study aims to empower young primiparous mothers with knowledge enhancement, allowing them to adeptly embrace their pivotal roles as parents. Participants were meticulously chosen through purposive sampling, specifically from the Independent Midwifery Practice (IMP), comprising 20 midwives with the qualification of Bidan Delima. The term Bidan Delima itself stands for the standardization system for the service quality of private midwives emphasizing the monitoring and evaluation activities. The allocation into intervention and control groups was meticulously accomplished via proportional random sampling, based on the number of pregnant women receiving ANC at the midwife's private clinic.
Independent Midwifery Practice (IMP) is the independent practice of midwives outside of hospitals or primary health care, for providing pregnancy, childbirth, and postpartum care. IMP emphasizes holistic and personalized maternity care with a focus on the relationship between midwives and patients. “Bidan Delima” is an independent midwifery practice that emphasizes quality care. This program adheres to a standardized system for ensuring the quality of independent midwifery practice, with a focus on continuous monitoring, evaluation, mentoring, and ongoing training. This ensures that independent midwifery practice in Bidan Delima provides high-quality midwifery services to pregnant women, during childbirth, the postpartum period, and newborns. The study design can be represented as follows:
Group A (Control) ------------------------ O1* Group B (Intervention)------------------------ O2*
Explanation:
A = Group without intervention (MCH book approach).
B = Group with the intervention (CMC approach).
O1* = Post-test measurement for the control group.
O2* = Post-test measurement for the intervention group.
2.2. Study Location and Duration
The study was scheduled to be conducted from December 2022 to March 2023, across 20 Standardized Independent Midwives' Practices, recognized as Bidan Delima situated within Padang City.
2.3. Population and Sample
The population of this study comprised all young pregnant women in their third trimester of pregnancy residing in Padang City. The sample of this study included all primiparous women in their third trimester of pregnancy aged under 20 years, who resided in Padang City and were willing to participate in the study and undergo ANC at the selected IMP locations of Bidan Delima. The sampling technique used was purposive sampling, in which the respondents were selected based on predefined criteria as set by the researchers in every Bidan Delima IMP.
Inclusion Criteria were pregnant women aged under 20 years in their third trimester of pregnancy; primiparous women (first-time pregnancies) in their third trimester; pregnant women who were residents or domiciled in Padang City; pregnant women having MCH book; pregnant women who have undergone at least three ANC visits; married women living with their partner; willingness to participate as research subjects; and being capable of effective communication. Meanwhile, the Exclusion Criteria are babies who passed away during the study period.
2.4. Sample Size Consideration
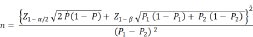
The minimum sample size was calculated using the Lemeshow formula, as represented below [25].
 |
 |
Explanation:
n = Minimum sample size
α = probability of type 1 error (5% = 0.05)
β = probability of type 2 error (β) (10% = 0.10)
Z1- α/2= 1.96
Z1- β/2= 1.28
P1 = the proportion in the intervention group (P1) (6.10% = 0.06), (2017)
P2 = the proportion in the control group (P2) (39.4% = 0.39), Setiawati, et al (2017) [26]
P = (P1 + P2)/2 = 0.225
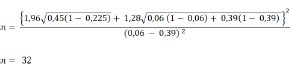
Using the Lemeshow formula, the minimum sample size obtained was 32 subjects for each group. To account for the potential dropouts, an additional 10% of the sample size was added, resulting in a total of 35 participants per group. Thus, the required total sample size for this study was 70 participants.
2.5. Data Collection
The data collection process involved a pre-test conducted through questionnaire responses to measure variables related to maternal role readiness (knowledge of domestic violence, the dangers of smoking, Narcotics, Psychotropic substances, and Addictive substances (NAPZA), reproductive health, pregnancy, childbirth processes, and parenting roles). The intervention was carried out during pregnancy until the postnatal period, specifically up to 42 days after childbirth. Post-tests were conducted during the third trimester of pregnancy on the 31st and 43rd day postpartum using the same questionnaire.
2.6. Research Instrument, Validity, and Reliability Test
The research instruments, comprising of questionnaires and surveys, were meticulously prepared and underwent a comprehensive review by a competent and experienced Midwife Lecturer, who also served as a reviewer for the Midwives Competency Test. The knowledge section of the questionnaire comprised 45 questions, out of which 40 questions were considered suitable and appropriate for use after a comprehensive review.
To ensure the validity of the questionnaires, a meticulous validity and reliability test was conducted with a sample of 30 young pregnant women from two health centers, namely Padang Pasir Health Center and Air Dingin Health Center. The validity assessment was based on the Pearson Product Moment correlation coefficient, with a critical value of the r-table for 30 samples (df = n-2 = 28) set at 0.361 (at α = 5%). After conducting the validity test, all questionnaire items were found to have correlation values > 0.361, affirming the validity of the questionnaires used in the research. Subsequently, the reliability of the questionnaires was assessed using Cronbach's alpha coefficient, a widely accepted measure of internal consistency. The questionnaires were found to be highly reliable, as evidenced by Cronbach's alpha value being greater than 0.60, signifying the consistency and stability of the measurement items in capturing the intended constructs
2.7. Data Analysis
This study utilized a generalized linear model with repeated measures to compare the effectiveness of CMC and MCH 2020 groups in enhancing the knowledge related to parental roles at three time points (third trimester of pregnancy, and postpartum days 31 and 43). This statistical method controlled for the unobserved variables, ensuring a reliable analysis. Before the analysis, data underwent normality and homogeneity tests. The generalized linear model was then employed for multivariate analysis, examining the interventions' effects on knowledge in fulfilling parental roles, covering some aspects, namely domestic violence, the dangers of smoking, Narcotics, Psychotropic substances, and Addictive substances (NAPZA), reproductive health, pregnancy, childbirth processes, and parenting roles. The results of this analysis provide insights into differences in the effectiveness of CMC and MCH 2020 book groups regarding knowledge acquisition in the parental roles. The study aims to determine the approach that best fulfills the research objectives, considering a significance level of α < 0.05. SPSS 25 software was used for accurate and robust data analysis.
2.8. Ethical Approval
The research was conducted after obtaining an ethical clearance from the Research Ethics Committee of the Faculty of Medicine, Andalas University, with approval number 736/UN.16.2/KEP-FK/2022, dated May 23, 2022. Additionally, research permits were obtained from the Integrated Licensing and One-Stop Service Agency of Padang City, with permit number 070.1000/DPMPTSP-PP/VI/2022, dated June 7, 2022, the Health Department of Padang City, with permit number 891/4382/DKK/2022, dated May 31, 2022, and the Director of the Health Polytechnic of the Ministry of Health in Padang, with permit number DP.02.01/03657/2022, dated June 8, 2022.
3. RESULTS
After data collection, the data was processed and analyzed. The normality test was conducted on the numerical data using the Kolmogorov-Smirnov test. The variables of family support, husband support, and attitude were found to not follow a normal distribution. To address this issue, the standardized residual linear regression was performed. The standardized residual values were then subjected to a normality test, which yielded a normal distribution with a p-value of 0.200. Once the numerical data met the normality assumption and all other assumptions were fulfilled, the Generalized Linear Model Repeated Measures analysis was conducted. Based on Table 1, it is evident that the knowledge variable with its sub-scales, including Knowledge of Gender and Domestic Violence, Knowledge of the dangers of smoking and Substance Abuse, Knowledge of reproductive health, Knowledge of healthy pregnancy, Knowledge of childbirth, and Knowledge of the parenting roles, had an increase in average scores in the intervention group (CMC model) that exceeded those in the control group (MCH book).
According to Table 2, the measurements taken after 1 month postpartum (day 31) and at the end of the postnatal period (day 43), there was an increase in the knowledge observed in the CMC model group and MCH 2020 book group. This enhancement was evident in the measurements on day 31 (p = 0.000) and on day 43 (p = 0.000). In this study, it was revealed that both the CMC model and the MCH book were equally effective in enhancing the knowledge of young pregnant mothers, as indicated by the p-value for the group factor is 0.00. The General Linear Model-Repeated Measures analysis in Table 3 reveals significant knowledge variations among young pregnant mothers across three measurement points, namely the third trimester, postpartum day 31, and postpartum day 43 [27]. This was observed in the intervention (CMC Model) and control (MCH book) groups. Notably, the intervention group showed a greater knowledge enhancement compared to the control group in the second and third
| - | Variable/Subscale | Control Group (MCH book) (n=35) | Intervention Group (CMC model) (n=35) | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | N | Mean | SD | N | ||
| Third Trimester of Pregnancy | Knowledge of Domestic Violence | 1.57 | 0.502 | 35 | 3.51 | 0.562 | 35 |
| Knowledge of the dangers of smoking, NAPZA | 1.23 | 0.426 | 35 | 2.49 | 0.507 | 35 | |
| Reproductive Health Knowledge | 1.26 | 0.443 | 35 | 2.40 | 0.604 | 35 | |
| Pregnancy Knowledge | 10.63 | 1.330 | 35 | 5.86 | 1.396 | 35 | |
| Childbirth Process Knowledge | 0.20 | 0.406 | 35 | 0.66 | 0.482 | 35 | |
| Parenting Role Knowledge | 3.09 | 0.781 | 35 | 3.89 | 0.718 | 35 | |
| Postpartum Day-31 | Knowledge of Domestic Violence | 2.06 | 1.027 | 35 | 3.86 | 0.355 | 35 |
| Knowledge of the dangers of smoking, NAPZA | 2.00 | 0.542 | 35 | 2.80 | 0.406 | 35 | |
| Reproductive Health Knowledge | 1.97 | 0.664 | 35 | 2.83 | 0.382 | 35 | |
| Pregnancy Knowledge | 8.09 | 1.358 | 35 | 7.94 | 1.984 | 35 | |
| Childbirth Process Knowledge | 0.23 | 0.426 | 35 | 0.91 | 0.284 | 35 | |
| Parenting Role Knowledge | 4.29 | 1.017 | 35 | 5.11 | 0.676 | 35 | |
| Postpartum Day-43 | Knowledge of Domestic Violence | 2.34 | 0.838 | 35 | 3.97 | 0.169 | 35 |
| Knowledge of the dangers of smoking, NAPZA | 1.77 | 0.731 | 35 | 2.97 | 0.169 | 35 | |
| Reproductive Health Knowledge | 1.83 | 0.785 | 35 | 2.97 | 0.169 | 35 | |
| Pregnancy Knowledge | 9.60 | 0.881 | 35 | 9.23 | 1.573 | 35 | |
| Childbirth Process Knowledge | 0.43 | 0.502 | 35 | 1.00 | 0.000 | 35 | |
| Parenting Role Knowledge | 4.43 | 0.917 | 35 | 5.54 | 0.611 | 35 | |
| Effect | Value | F | Hypothesis df | Error df | Sig. | |
|---|---|---|---|---|---|---|
| Factor 1 | Pillai’s Trace Wilks’Lambda Hotelling’s Trace Roy’s Largest Root |
0.871 0.129 6.733 6.733 |
225,533 225,553 225,533 225,533 |
2,000 2,000 2,000 2,000 |
67,000 67,000 67,000 67,000 |
0.00 0.00 0.00 0.00 |
| Factor 1 * group | Pillai’s Trace Wilks’Lambda Hotelling’s Trace Roy’s Largest Root |
0.635 0.347 1,886 1,886 |
63,176 63,176 63,176 63,176 |
2,000 2,000 2,000 2,000 |
67,000 67,000 67,000 67,000 |
0.00 0.00 0.00 0.00 |
| Contrasts | Times | F | Sig. |
|---|---|---|---|
| Knowledge | Level 2 vs. Level 1 | 173.490 | .000 |
| Level 3 vs. level 2 | 452.895 | .000 | |
| Knowledge * Group (MCH book and CMC) | Level 2 vs. Level 1 | 48.200 | .000 |
| Level 3 vs. Level 2 | 126.936 | .000 |
measurements. The CMC Model's impact started in the second measurement, with the most substantial knowledge increase occurring in the third measurement compared to the second.
4. DISCUSSION
The research findings confirm that the CMC model significantly outperforms the MCH book in enhancing the knowledge of young pregnant mothers. This result can be attributed to the unique approach of the CMC model, specifically designed to address the transition from adolescence to adulthood experienced by young pregnant mothers [28-30]. The CMC model is an approach to pregnancy care led by midwives that places a strong emphasis on establishing personal connections with expectant mothers. This approach ensures that pregnant women receive care from the same midwife consistently throughout their pregnancy, childbirth, and postpartum period. The CMC model is structured around three primary components, namely Continuity Management, Informational Continuity, and Relational Continuity. Continuity Management involves clear case management to meet each mother's unique needs, following established guidelines for diagnosis, problem anticipation, care planning, implementation, and evaluation. Informational Continuity focuses on providing essential information through modules or books covering various topics like gender equality, domestic violence, reproductive health, smoking risks, and pregnancy preparation. Pregnant women can study this material at home. Relational Continuity highlights the establishment of strong professional relationships within the healthcare team to ensure comprehensive care.
CMC aims to enhance support and knowledge for young pregnant women from the third trimester through postpartum. Midwives guide, educate, and provide continuous support with privacy and compassion. Information is gradually provided through modules, and midwives engage in health education during visits, offering support through calls and messages. Privacy, kindness, comprehensive care, prompt issue resolution, and follow-up are core principles to build trust among pregnant women and their families when accessing healthcare services [17, 24]. The significance of this approach is evident in the results, which indicate an enhancement in the positive attitudes of young pregnant mothers towards pregnancy and child care [28-30].
This factor includes the principles of management continuity, information continuity, and relationship continuity within the CMC module. Consistent midwifery care and enduring relationships contribute to providing better support and guidance to young pregnant mothers [16, 31, 32]. Furthermore, the CMC module successfully strengthens family and spousal support for young pregnant mothers, which is crucial for navigating pregnancy and preparing for parenthood [33]. Previous research has shown that the CMC model, which is evidence-based and provides high-quality midwifery services, yields better clinical outcomes, higher satisfaction with care, and enhanced caregiving experiences. CMC reduces interventions and enhances normal physiological processes such as natural childbirth and breastfeeding. It is established on a positive relationship between midwives and women, aiming to establish this relationship through frequent care contact with the same midwife throughout a woman's care journey. This relationship results in the enhancement of clinical outcomes and a better care experience for women [34]. Previous research has also indicated that the utilization of a specific model and the provision of training can enhance the self-confidence of pregnant mothers [35]
This study aligns with previous research that demonstrates continuous care models like the CMC to be more effective in meeting the needs of young pregnant mothers and enhancing midwifery services compared to other service models. However, challenges pertaining to training sound the ization of healthcare services for pregnant adolescents need to be addressed through holistic approaches and the establishment of a trust-based relationship between pregnant mothers, families, and healthcare providers [16, 19, 36]. Based on the findings of previous research, 79.6% of respondents effectively utilize the MCH handbook, and 64.8% of respondents hold a positive attitude toward pregnancy and childbirth complications. The results of this study indicate that there is a correlation between the utilization of MCH handbooks and the attitudes of pregnant women regarding complications during pregnancy and childbirth [37]. When comparing the benefits of the MCH book and the CMC model in enhancing the knowledge of young primiparous mothers on several aspects such as domestic violence, the risks of smoking and harmful substances, reproductive health, healthy pregnancy, the childbirth process, and the role of a parent, CMC model presents a more effective approach. Research findings indicate that the group following the CMC model experienced a significantly greater enhancement in knowledge compared to the group using the MCH book [25].
This success is achieved through the specialized and relevant approach of the CMC model. Specifically designed to cater to the unique needs of young primiparous mothers, particularly during the transition from adolescence to adulthood, the CMC model provides comprehensive coverage of crucial issues. Besides, the CMC model encompasses three fundamental aspects, namely management continuity, information continuity, and relationship continuity, all directed towards addressing challenges faced by young primiparous mothers [17]. In contrast, the MCH book may provide only general information, while the CMC model offers in-depth and relevant explanations tailored to individual needs. The sustainable care approach of the CMC model holds the potential to effectively facilitate a thorough understanding of the role of young primiparous mothers as parents [38].
In conclusion, the CMC model has proven to be more effective in enhancing knowledge, attitudes, and support for young pregnant mothers compared to the MCH book. The specific and continuous care approach embedded in the CMC model assists young pregnant mothers in embracing their roles as mothers and preparing for parenthood. Nonetheless, addressing challenges related to access and utilization of healthcare services remains crucial through efforts to foster a trusting relationship between pregnant adolescents, their families, and healthcare providers [36, 39] The strengths of this study encompass a thorough evaluation of knowledge among young pregnant mothers, addressing various critical topics, and utilizing repeated measurements to gain long-term insights. This approach helps in addressing issues related to young pregnant women, allowing them to have a healthy pregnancy and prepare for parenthood. However, the study has certain limitations, including its narrow focus on Padang City, the possibility of recall bias due to the self-reported data, and the lack of consideration for external factors, such as economic conditions, psychological factors, socio-cultural variances, or healthcare accessibility that might impact knowledge and attitudes.
CONCLUSION
This study underscores the effectiveness of the CMC model in enhancing the knowledge of young primiparous mothers when anticipating parenthood. The CMC model addresses critical topics, such as gender equality, recognizing domestic violence, understanding the risks of smoking and substance abuse, sexual and reproductive health, maintaining a healthy pregnancy, the childbirth process, and preparing for parenthood. Its targeted and continuous approach significantly empowers adolescent mothers to embrace their new parental roles due to its specific focus. In light of these findings, we recommend that health authorities and policymakers consider implementing the CMC model alongside the existing MCH book as a more effective approach to enhance the knowledge of adolescent mothers.
AUTHORS’ CONTRIBUTIONS
Concept – D.S., H., Y., M., D.G.A.N., Y.M., E.H.; Design – D.S., H.; Supervision – H., Y., M.; Data collection – D.S.; Analysis and Interpretation – D.S., H., R.M.; Writing – D.S., Critical Review and Editing– H., Y., M., R.M., D.G.A.N., Y.M., E.H.
LIST OF ABBREVIATIONS
| ANC | = Antenatal Care |
| CMC | = Continuity of Midwifery Care |
| IMP | = Independent Midwives' Practices |
| MCH | = Maternal-Child Health |
| NAPZA | = Narcotics Psychotropic Substances, and Addictive Substances |
| WHO | = World Health Organization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Research Ethics Committee of the Faculty of Medicine, Andalas University, with approval number 736/UN.16.2/KEP-FK/2022, dated May 23, 2022; the Integrated Licensing and One-Stop Service Agency of Padang City, with permit number 070.1000/DPMPTSP-PP/VI/2022, dated June 7, 2022; the Health Department of Padang City, with permit number 891/4382/DKK/2022, dated May 31, 2022, and the Director of the Health Polytechnic of the Ministry of Health in Padang, with permit number DP.02.01/03657/2022, dated June 8, 2022.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The relevant additional data is available from the corresponding author [D.H] upon reasonable request, given approval provided by our university’s institutional review board.
FUNDING
None.
CONFLICT OF INTEREST
The authors certify that they have no financial or other conflicts of interest.
ACKNOWLEDGEMENTS
We want to thank all subjects who participated in this research.


