All published articles of this journal are available on ScienceDirect.
Explaining the Performance of Nurses in Order to Prevent Nosocomial Infections in Urmia City Hospitals: Application of the Health Belief Model
Abstract
Background
Nosocomial infections (NIs) are one of the medical, social, and economic problems in developing countries and can be prevented. Studying the etiology of NI is one of the most essential activities for designing prevention programs. The purpose of this study was to explain the constructs of the health belief model (HBM) regarding nurses' compliance with standard precautions for the prevention of NI in Urmia hospitals.
Methods
This cross-sectional study was conducted on 224 nurses of Urmia hospitals who were selected by employing the multi-stage method. The data collection tool was a questionnaire containing demographic characteristics, an HBM questionnaire associated with the prevention of NI, and questions related to the observance of nurses in the field of standard precautions to prevent NI. Data were analyzed using descriptive and inferential statistical methods in SPSS software version 22.
Results
The results of this study showed the average performance score of nurses in relation to adopting preventive behaviors against NI (71.97 ± 11.08) as acceptable. Also, the results of the study showed that among the constructs of the HBM, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cue to action, and self-efficacy are the most important predictors of adopting preventive behaviors against NI with a variance of 52% among the nurses.
Conclusion
According to the results of this study, the constructs of self-efficacy, perceived barriers, cue to action, perceived benefits, and perceived intensity are, respectively, the strongest predictors of compliance with standard precautions to prevent hospital infections. Therefore, the results of this study can be useful for health service providers in planning and designing interventions, and determining appropriate strategies for the prevention and control of NI.
1. INTRODUCTION
Nosocomial infections are defined as those infections that occur after 48-72 hours of hospitalization and have not been present when the patient has been admitted or during hospitalization. In addition to that, infections that occur among employees in the hospital environment can also be considered NI. The NI is one of the social and economic medical problems in developing countries, which causes the spread of infectious diseases, longer duration of hospitalization, and the death of patients [1]. The NI in the United States alone leads to 88,000 deaths and incurs more than 4.5 billion dollars in medical care costs per year [2]. At the same time, the sum of the total cost spent on NI control is much less compared to the cost required for treatment [3].
According to the report of the World Health Organization (WHO), approximately 15% of hospitalized patients suffer from this infection [4]. According to a survey conducted under the supervision of the WHO on 55 hospitals in 14 representative countries in four regions (Europe, Eastern Mediterranean, Southeast Asia, and the Western Pacific), an average of 8.7% of hospitalized patients had NI and more than 1.4% of million people around the world suffered from the complications of this disease; these studies have reported the highest frequency of NI from hospitals in the Eastern Mediterranean and Southeast Asian regions with 11.8 and 10% of prevalence, respectively. The prevalence rate is 7.7% for the European regions and 9% for the Western Pacific Ocean [5, 6]. The studies conducted in Iran have shown NI as one of the most important causes of medical, social, and economic problems in the country and a cause of great loss to society [7, 8]. In a meta-analysis study conducted in Iran from 1997-2012, the prevalence rate of NI was reported as 30.4% [9]. Also, Amini et al. [10] and Haji Bagheri et al. [9] reported the prevalence rate of NI as 15.6%.
Considering that prevention of NI is a global priority for members of the health team, nurses can play an active role in preventing and controlling these infections because they have the highest contribution to the treatment and care of the patient. Since nurses play a key role in the healthcare team, their knowledge and observance of standard precautions to prevent hospital and occupational infections is essential [11]. Considering the direct role of people in adopting preventive behaviors against infection, examining the psychological aspects and internal capabilities of people to comply with health behaviors can play a useful role in assessing needs and providing systematic educational interventions. One of the effective methods for controlling and preventing NI and reducing its subsequent complications is increasing the awareness of nursing personnel regarding it [3]. Based on the report of the World Health Organization (WHO), one of the vital principles in prevention is education [12]. The tendency to follow the principles of infection control after education and increasing awareness regarding the risks of infection transmission has been proven in the study of Ghanbari [3] and Gillespie [13].
The first and most important action in educational planning is to select a model or theory on the conditions, and to recognize the problem and the goal of the desired educational program [14]. Choosing an educational model directs the program on the right track and keeps it moving in the right direction [15]. In the meantime, one of the most useful models for preventing infections is the HBM, and the philosophy of this model emphasizes on the logical reason for people's decisions. However, what factors influence risky behaviors and health risk factors should also be understood [16, 17].
This model states that a person adopts preventive health behavior when he/she believes that he/she is at risk of disease (perceived susceptibility) and that the disease can cause serious complications and consequences for him/her (perceived severity). In addition, some behaviors are effective for preventing diseases and reducing the severity or complications of the disease (perceived benefits), but there are physical, psychological, or financial barriers to adopting these behaviors (perceived barriers); on the other hand, a person must commit to performing the behaviors able to understand proactively (perceived self-efficacy), and another concept is the presence of accelerating forces that make a person feel the need to perform a behavior (cue to action) [18, 19]. According to the above, this study tries to answer the key question as to what is the explanatory power of the various constructs of the HBM with regards to the prevention of NI; by answering this question, we can find appropriate solutions and strategies to plan for the promotion of intervention programs to prevent and control the burden of diseases resulting from this problem.
2. METHODS
This cross-sectional study was conducted on 224 nurses working in public hospitals affiliated with Urmia University of Medical Sciences, Iran (Motahari Hospital, Ayatollah Taleghani Hospital, and Arefian Hospital) in 2021-2022. The sample size was determined by using the following formula:
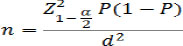 |
Also, the following have been considered: α = 0.05 confidence level and 95% confidence level, P as 15% prevalence of NI [ 20 ], and d = 0.05 as an acceptable error in estimating the desired ratio; considering the possibility of 15% drop in samples, a total sample of 224 was estimated.
The sample of this research was selected by multi-stage probability sampling, so first, a list of all public hospitals in Urmia was prepared. Then, from among these hospitals, three hospitals (Motahari Hospital, Ayatollah Taleghani Hospital, and Arefian Hospital) were selected by simple random method and then by stratified sampling method, and according to the nurses working in different departments of the selected hospitals who have met the criteria for entering the study.
The inclusion criteria were having a bachelor's and higher degree in nursing, midwifery, and at least a diploma in healthcare, and the exclusion criterion was the disinclination of the nurses to participate in this research. The research environment included the emergency section, the women and pediatric wards, the internal medicine department, the surgery room, the operation theater, the special cardiac care ward, the nursing office, and the dialysis and maternity departments of the three mentioned hospitals.
The data collection tool was a standard questionnaire used in Ghanbari et al.’s research [3], which included the following: demographic questions and a knowledge scale (14 items) on public awareness about NI, precautions related to safe injection, precautions related to dressing, and hygienic hand washing. For example, the nurses may suffer from the complications of hospital infections due to not following the correct principles of hand hygiene.
The perceived severity construct of the model explored in this study involves 6 items, for example, “NI can lead to worsening of patients' illness and even death.” The perceived benefits construct involves 5 items, for example, “preventing NI reduces the burden of disease in society.” The perceived barriers construct includes 5 items, for example, “I don't do it due to lack of access to health facilities and equipment.” The perceived self-efficacy construct involves 10 items, for example, “I apply the correct principles of hand hygiene in emergencies.” The cue to action construct includes 6 items, for example, “To what extent does the educational supervisor play a role in observing the principles of hand hygiene according to you?”
The response scales of the questionnaire are based on a 5-point Likert scale as follows: strongly disagree, disagree, neither disagree nor agree, agree, and strongly agree. The fourth part comprises a checklist with 21 items that measure the individual's observance regarding the adoption of preventive behaviors from NI based on standard precautions. Each question requires a response of true and false. The correct responses are allocated a score of 1, while the incorrect ones are given a score of 0. At the end, the individual score is calculated based on the score of 100, in such a way that the number of correct answers is multiplied by 100 and divided by the total number of questions. In total, the total points obtained by the person in each construct are calculated out of 100 points. In the part of the checklist based on the Likert scale, the observance score of the person is based on the number of cases in which he has tried to perform preventive behaviors from NI (based on standard precautions), and calculated by dividing these from the total number of mentioned behaviors and multiplying by 100.
The validity and reliability of the measurement tool have been evaluated in the study of Ghanbari et al. [3]. Content validity was ensured in such a way that the questionnaire was prepared based on the study of the national guidelines for the NI care system, reliable sources and books, as well as a survey of 15 experienced professors and faculty members. In this regard, the panel of experts was asked to evaluate each of the statements based on the clarity and simplicity of the statements and their relevance, and after checking by removing some items and adjusting other narrative statements, the tools were approved. The analysis of data was carried out on all three parts of knowledge, aspects of the HBM, and observance of nurses in the field of standard precautions. Based on the opinion of the researchers, a score ≤50 has been considered weak, 50-75 has been considered moderate, and a score ≥75 score has been considered a good condition.
2.1. Data Analysis
The data analysis was conducted using SPSS software version 22, and descriptive statistics, such as frequency percentage, mean, and standard deviation have been taken into account; as the score of the Smirnoff cosmography test was more than 0.05, the normality of the data was confirmed. Pearson's correlation coefficient and linear regression tests were tested at a significance level of 0.05.
3. RESULTS
The response rate was 96.4% as 241 out of 250 participants responded to the questionnaire; 17 (6.8%) questionnaires were incompletely answered, and thus were excluded from the study. The mean age was 38.28±8.76 years. 82.1% of the sample participants were female (N=184) and 17.9% were male (N=40).
The average score of nurses in terms of compliance with standard precautions to prevent NI was 71.97 ± 11.08 (Table 1).
The average score of various dimensions of the constructs of the HBM for the samples in relation to the observance of standard precautions in order to prevent NI was estimated to be acceptable and the most challenging were, respectively, the variable of knowledge, the construct of perceived barriers with an average score of 42.72 ± 18.80, perceived susceptibility construct with an average score of 61.77 ± 9.35, perceived severity with an average score of 74.49 ± 8.22, and cue to action with an average score of 77.58 ± 13.17 (Table 2).
| Variable | N | (%) | |
|---|---|---|---|
| Educational level | Diploma | 18 | 8 |
| Bachelor's degree | 198 | 88.5 | |
| Master’s and higher | 8 | 3.5 | |
| Recruitment status | Contractual | 31 | 13.8 |
| Corporative | 118 | 52.7 | |
| Designated | 38 | 17 | |
| Agreement | 31 | 13.8 | |
| Official hiring | 6 | 2.7 | |
| Marital status | Single | 52 | 23.2 |
| Married | 172 | 76.8 | |
| Workplace | Internal surgery | 81 | 36.2 |
| CCU | 54 | 24.1 | |
| Emergency | 21 | 9.4 | |
| Obstetrics and Gynecology | 19 | 8.5 | |
| Dialysis | 34 | 15.2 | |
| Operating room | 10 | 4.4 | |
| ICU | 5 | 2.2 | |
| Total | 224 | 100 | |
|
Statistical Index Desired Variable |
Mean | Standard Deviation | Maximum | Minimum |
|---|---|---|---|---|
| Awareness | 34.32 | 8.53 | 85.71 | 14.29 |
| Perceived susceptibility | 61.77 | 9.35 | 92 | 40 |
| Perceived severity | 74.49 | 8.22 | 100 | 20 |
| Perceived benefits | 89.29 | 10.18 | 100 | 60 |
| Perceived barriers | 47.72 | 18.80 | 100 | 20 |
| Self-efficacy | 84.93 | 12.50 | 100 | 24 |
| Cues to action | 77.58 | 13.17 | 100 | 36.67 |
| Behavior | 71.97 | 11.08 | 100 | 15.87 |
| - | Knowledge | Perceived Susceptibility | Perceived Severity | Perceived Benefits | Perceived Barriers | Self-efficacy | Cues to Action | Behavior | |
|---|---|---|---|---|---|---|---|---|---|
| Awareness | r | - | - | - | - | - | - | - | - |
| p | 1 | - | - | - | - | - | - | - | |
| Perceived susceptibility | r | .067 | - | - | - | - | - | - | - |
| p | .355 | 1 | - | - | - | - | - | - | |
| Perceived severity | r | .184 | .086 | - | - | - | - | - | - |
| p | .011 | .208 | 1 | - | - | - | - | - | |
| Perceived benefits | r | .187* | .092 | .451** | - | - | - | - | - |
| p | .009 | .181 | .000 | 1 | - | - | - | - | |
| Perceived barriers | r | .067 | -.306** | -.179* | -.387** | - | - | - | - |
| p | .354 | .000 | .009 | .000 | 1 | - | - | - | |
| Self-efficacy | r | .137 | -.198** | .376** | .536** | -.587** | - | - | - |
| p | .059 | .004 | .000 | .000 | .000 | 1 | - | - | |
| Cues to action | r | .002 | .067 | .221** | .405** | -.208** | .393** | - | - |
| p | .980 | .327 | .001 | .000 | .002 | .000 | 1 | - | |
| Behavior | r | .031 | .113 | .353** | .330** | -.547** | .659** | .393** | - |
| p | .673 | .102 | .000 | .000 | .000 | .000 | .000 | 1 | |
Pearson's correlation coefficient showed a positive and significant relationship between the constructs of the HBM (except for the construct of perceived barriers) and the level of observance of nurses in relation to compliance with standard precautions to prevent NI in the sample. The correlation coefficients of the HBM constructs and individual factors related to compliance with standard precautions to prevent NI are shown in Table 3.
Regression analysis and the step-wise method were used to determine the predictive power of nurses' observance in relation to compliance with standard precautions to prevent NI. In this regression analysis, the constructs of the HBM were considered based on the results, self-efficacy, perceived barriers, cue to action, perceived benefits, and perceived susceptibility as final predictors of changes in nurses' observance in relation to compliance with standard precautions to prevent NI. These variables were able to explain about 52% (R2=0.521) of the changes in nurses' observance related to NI (Tables 4 and 5).
| Criterion Variable | Predictor Variable | Correlation (R) | Coefficient of Explanation (R2) | Adjusted Coefficient of Explanation (R2) |
|---|---|---|---|---|
| Constructs of the HBM | Self-efficacy | 0.667 | 0.445 | 0.442 |
| Self-efficacy and perceived barriers | 0.690 | 0.476 | 0.470 | |
| Self-efficacy, perceived barriers, and cue to action | 0.703 | 0.414 | 0.485 | |
| Self-efficacy, perceived barriers, cue to action, and perceived benefits | 0.718 | 0.515 | 0.503 | |
| Self-efficacy, perceived barriers, cue to action, perceived benefits, perceived susceptibility, and perceived severity | 0.731 | 0.535 | 0.521 |
| Stage | Source of Change | Non-standard Coefficients | Standard Coefficients | t-value | Significance Level | |
|---|---|---|---|---|---|---|
| 1 | B | Std.Error | Bata | |||
| Constant | 20568 | 4.465 | - | 4.607 | 0.000 | |
| Self-efficacy | 0.606 | 0.052 | 0.667 | 11.684 | 0.000* | |
| 2 | Constant | 35.600 | 6.485 | - | 5.489 | 0.000 |
| Self-efficacy | 0.493 | 0.062 | 0.543 | 7.916 | 0.000* | |
| Perceived barriers | -0.126 | 0.040 | -0.214 | -3.127 | 0.002* | |
| 3 | Constant | 29.980 | 6.795 | - | 4.412 | 0.000 |
| Self-efficacy | 0.441 | 0.065 | 0.486 | 6.797 | 0.000* | |
| Perceived barriers | -0.128 | 0.040 | -0.218 | -3.223 | 0.002* | |
| Cue to action | 0.130 | 0.053 | 0.145 | 2.438 | 0.016* | |
| 4 | Constant | 39.640 | 7.571 | - | 5.236 | 0.000 |
| Self-efficacy | 0.513 | 0.069 | 0.565 | 7.429 | 0.000* | |
| Perceived barriers | -0.141 | 0.039 | -0.239 | -3.577 | 0.000* | |
| Cue to action | 0.158 | 0.053 | 0.176 | 2.959 | 0.004* | |
| Perceived benefits | 0.195 | 0.072 | 0.181 | 2.699 | 0.008* | |
| 5 | Constant | 33.947 | 7.733 | 000 | 4.390 | 0.000 |
| Self-efficacy | 0.459 | 0.071 | 0.505 | 6.483 | 0.000* | |
| Perceived barriers | -0.159 | 0.039 | -0.270 | -4.054 | 0.000* | |
| Cue to action | 0.161 | 0.052 | 0.180 | 3.080 | 0.002* | |
| Perceived benefits | 0.254 | 0.074 | 0.237 | 3.427 | 0.001* | |
| Perceived severity | 0.217 | 0.081 | 0.166 | 2.679 | 0.008* | |
The reliability of the mentioned questionnaire was also measured by Cronbach's alpha test on 30 nurses similar to the study population in terms of demographic characteristics. Its value has been estimated for awareness questions (α=0.71), questions related to HBM dimensions (α=0.79), questions regarding self-efficacy constructs (α=0.71), and observance checklist (α=0.73).
4. DISCUSSION
This study was conducted to investigate predictive factors related to compliance with standard precautions in order to prevent NI in nurses based on the HBM model. The result of this research was a statistical model consisting of five variables, including perceived severity, perceived barriers, perceived benefits, self-efficacy, and cues to action, which was able to describe 52% of nurses' observance in relation to compliance with standard precautions to prevent NI. The results showed the power of each of the above five variables in explaining the observance of nurses in relation to the adoption of precautions against NI to be different.
In the study carried out by Kohi et al. [21], the explanatory power of the HBM constructs in relation to the observance of health workers was reported to be 31%, confirming the effectiveness of the HBM in determining effective strategies for health workers' functional improvement programs in relation to the adoption of behaviors for preventing NI. Through continuing education, knowledge and fair practice and adherence to standard precautions are possible.
Our study showed the observance of nurses in relation to standard precautions for the prevention of NI to be at an average level, which is consistent with the results of the studies by Kohi et al. [21], NavabAzam et al. [22], and Yang Leo et al. [23]. However, Nazari et al. [24], Ghanbari et al. [3], and Bischoff et al. [25] concluded the level of compliance with standard precautions among nurses and doctors to be weak and unacceptable, and this difference and inconsistency can be explained by prioritizing the discussion. To increase the effectiveness of interventions to adopt standard precautions in order to prevent hospital infections in health workers and patients, it is necessary to identify the factors that determine compliance with standard precautions to deal with hospital infections in this segment of the population. In the present study, self-efficacy construct, cue to action, perceived benefits, and perceived severity were positively correlated with nurses' observance of preventing NI, and perceived barriers were negatively correlated. However, this correlation was not observed between individual factors, such as marital status, age, different working environments in the hospital, and the type of employment. In the current study, the self-efficacy construct was the strongest and most effective with respect to the observance of standard precautions in order to prevent NI, predicting the relationship between the optimal observances of nurses and a change variance of about 44%. Perceived self-efficacy has been reported to be a strong source of motivation and a judgment of people's ability to achieve certain goals [26].
Research shows that people who have high perceived self-efficacy have more commitment to perform activities in times of challenges and problems and they spend more time and effort on activities [27]. Such people are more likely to participate in maintaining healthy behaviors and recovering them even after failure, and they have stronger intentions and motivation, which not only improves goals, but also leads to achieving them and stability in pursuing them [28]. The use of self-efficacy resources in clinical learning environments can be a stimulus in the professional development of nursing [29]. The relationship between self-efficacy in nursing and nursing education has also been mentioned in the research. Patterson has mentioned its association with predicting the academic success of nurses, and Pisanti has pointed out its effect on the ability to cope with stress in nurses working in stressful situations [30-31]. Self-efficacy and self-belief are factors that increase in clinical learning environments [32]. Also, these are mentioned as one of several important individual factors in improving nurses' healthy behaviors [33]. Yang Leo and his colleagues considered self-efficacy to be the most influential construct with respect to the observance of standard precautions and pointed out that strengthening this construct can be an effective step in improving the behaviors for dealing with NI [34].
According to the results of this study, among the investigated constructs, perceived barriers are the second predictor of adopting preventive behaviors against NI. Some studies have pointed out the high workload of nurses as the main risk factor and the main obstacle in the prevention of NI [35]. They have considered the suitability of nurses to hospital beds as one of the factors reducing the barriers in the way of positive observance in the field of NI [36]. However, the results of various studies regarding the constructs of perceived barriers have been very contradictory. The reason for this may be the significant variety of perceived barriers, including material, physical, psychological, and social barriers. Such findings reveal the necessity of designing and implementing appropriate interventions at all levels. Perceived barriers are considered the most important predictors of behavior in the HBM. Therefore, they must be resolved, and to resolve them, a needs assessment must be conducted, and based on that, strategies must be determined and interventions must be applied to the target group.
The cue to action, another predictor of NI in the present study, was evaluated with an average score. The cue to action construct is independently related to the improvement of observance of standard precautions to prevent NI, and cues to action, such as posters, brochures, and guides installed near the patient's bed or fixed, or portable pocket alcohol solutions can have a significant impact [37]. In the study conducted by ParMaghiani and his colleagues, nurses received most of the information from training courses and scientific journals [38]. Basch also pointed out that those nurses who hold training workshops and are associated with print and visual media are effective in taking precautions to prevent NI [39]. With regards to internal cue to action, Ghanbari, in a study carried out in Iran, showed that nothing can play a role in preventing NI as much as individual commitment and conscience [3]. Conscientiousness and individual conscience are effective in choosing health behaviors through a diverse set of mechanisms [40].
Also, the research findings have shown a high percentage of benefits to be perceived by nurses working in different departments of the hospital, and a high percentage of nurses to believe that by following the standards of infection prevention, the patient's health can be improved and the patient's satisfaction can be increased. At the same time, this can guarantee the personal health of the nurse. Based on the HBM, high attitudinal items (perceived susceptibility, perceived severity) are necessary to improve people's motivation to adopt preventive health behavior. If nurses themselves perceive the prevention of NI as a necessary principle, then they would apply the principles of precautions to reduce the complications caused by NIs in hospitalized patients and increase the quality of care provided [41].
Therefore, the attitude of care workers towards preventive strategies can motivate and enable preventive behaviors, such as hand hygiene [37]. It is worth noting that although training can lead to an increase in the level of awareness, changing attitudes is very vital to improving people's reactions [42]. The results of the research are consistent with the study of Vakil and Efstathiou [43, 44]. Also, the results of the present study regarding the constructs of perceived susceptibility have not indicated the existence of a correlation and relationship with the observance of nurses with respect to NI, but the research of Jellispai et al. has shown the item of perceived severity to be directly related to an increase in the preventive observance of NI [3]. Considering that in the present study, there was no positive and significant correlation between the knowledge of nurses and the observance of standard precautions to prevent NI, it should be noted that in developing countries (with Iran being one of them), the level of awareness and the low readiness and observance of employees are one of the basic issues that have led to the poor control of NI [45]. Yang Leo et al. conducted a study on 1444 nurses to evaluate the role of awareness in increased observance of standard precautions, and stated it as very important [23].
CONCLUSION
According to the results of this study, HBM has predicted 52% of the variance in nurses' observance related to compliance with standard precautions to prevent NI. The constructs of self-efficacy, perceived barriers, cue to action, perceived benefits, and perceived intensity have been, respectively, found to be the strongest predictors of compliance with standard precautions to prevent hospital infections. Considering the crucial role of behavior in prevention of the hospital infections and the complex reasons for non-adoption of it among healthcare employees as well as the inevitable role of education, the authorities must regard the problem more seriously and adopt multiple approaches to promote the nurses' knowledge of the emerging hospital infections.
LIMITATIONS AND SUGGESTIONS
However, this study, like other studies, has its limitations. To begin with, this study was a cross-sectional study and did not examine the cause-and-effect relationship. Accordingly, stronger studies can be conducted for this purpose. Furthermore, the obtained results cannot be generalized beyond the study sample, and can, therefore, be generalized only to populations with similar features. Finally, the data collection tool in this study was a self-report questionnaire and the participants may have underestimated or overestimated their preventive behavior for nosocomial infections, which may have affected the outcomes.
LIST OF ABBREVIATIONS
| NI | = Nosocomial infections |
| HBM | = Health belief model |
| SPSS | = Statistical Package for Social Sciences |
| WHO | = The World Health Organization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research was approved by the ethics committee of Urmia University of Medical Sciences and received the code of ethics (IR.UMSU.REC.1399.225).
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study. In this study, all provisions of the Declaration of Helsinki were observed.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants of this study.
STANDARDS OF REPORTING
STROBE guidelines were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and/or analyzed during the current study will be available from the corresponding author [N.S] upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
This article is the result of a research project approved by the Research Vice-Chancellor of Urmia University of Medical Sciences. In this way, the authors express their gratitude to the Department of Research and Management of the university and the participants of this study.


