All published articles of this journal are available on ScienceDirect.
A Study of how the Serum Levels of Inflammatory Markers Correlate with Hemoglobin Oxygen Saturation Percentage and the Type of Respiratory Support Received by Covid-19 Patients Hospitalized in Intensive Care Units
Abstract
Aim
This study aimed to shed light on how serum levels of interleukin-6 (IL-6), lactate dehydrogenase (LDH), and C-reactive protein (CRP) correlate with hemoglobin oxygen saturation percentage (SpO2) and the type of respiratory support received among COVID-19 patients hospitalized in COVID-19 intensive care units.
Background
The clinical care of patients who suffer from COVID-19 requires knowledge of laboratory findings and the way these findings are linked with the type of respiratory support.
Methods
This descriptive-analytical study was conducted using data from the clinical records of 31 patients hospitalized in the intensive care unit at 22nd-Bahman Hospital in Khaf, Eastern Iran, during the first half of 2021. The study utilized a checklist developed by the researcher for data collection. The data were analyzed with Kolmogorov-Smirnov, independent t, one-way analysis of variance, and Tukey's post hoc statistical tests in the SPSS-22 statistical package. The significance level was established at p <0.05.
Results
The mean CRP, LDH, and serum levels of IL-6 were significantly higher in COVID-19 patients with SpO2 <93 than in patients with SpO2 ≥93 (p <0.05). Patients receiving intubation and non-invasive respiratory support exhibited significantly greater serum levels of IL-6, CRP, and LDH than patients receiving other respiratory support (p <0.05). The mean CRP, serum levels of IL-6, and LDH were significantly lower among survivors than those who died (p <0.01).
Conclusion
Understanding the relationship between the serum levels of IL-6, CRP, LDH, and SPO2 and the type of respiratory support can help predict the management of acute respiratory patients, but this decision-making method based on serum levels should be further investigated. and to be compared with the current methods of management of treatment of acute respiratory patients.
1. INTRODUCTION
In Wuhan, Hubei Province, China, a new coronavirus known as SARS-CoV-2 emerged toward the end of 2019 and caused severe and widespread respiratory disease. The disease was later dubbed as COVID-19. The most significant COVID-19 clinical manifestations leading to hospitalization are shortness of breath, dry and persistent coughs, fever, and fatigue [1]. The respiratory system is one of the first organ systems affected by this virus. Numerous in vitro studies have demonstrated that the virus utilizes the angiotensin-converting enzyme-2 (ACE2) to enter lung cells [2]. This protein is abundant in the liver, heart, intestine, kidney, stomach, and lung tissues [3].
One of the first organs susceptible to infection by this virus is the lung. A large portion of lung tissue can come into contact with the virus as a result of breathing, which is why the lung is the virus's primary target organ [2]. On the other hand, type 2 alveolar cells express ACE2 protein to a high degree, making them the virus's primary and most significant entry point into these cells [4, 5]. The respiratory tract and lungs are, therefore, the first sites where a virus may initiate pathogenesis and cause disorders related to the respiratory system's structure and function.
The lung is one of the primary sites of infection for COVID-19, where it can cause irreversible damage to the respiratory membrane and an increased risk of acute respiratory failure, both of which can be fatal [6]. Extensive alveolar damage, accumulation of fibromyxoid cellular secretions, and chronic inflammation in the lungs and airways have been found in histological examinations of lung tissue samples from patients with COVID-19 [6-9]. Microscopic examination of lung tissue reveals reactive hyperplasia of type 2 alveolar cells, fibrinous secretions within the alveoli, interstitial fibrosis with exudation of inflammatory fluid, and fibrotic plaques within the alveoli. In addition, loose fibrotic plaques within the alveoli causing pneumonia and organizing fibrin have been observed in the majority of lung foci. Examination of the patient's lung tissue reveals signs of acute respiratory distress syndrome, including pneumocyte detachment, the development of lung edema with the formation of a hyaline membrane, and the presence of inflammatory filtered fluid in the interstitial space of the lung, all of which are suggestive of acute respiratory distress syndrome. The presence of multinucleated senescent cells with enlarged and unusual pneumocytes, large prominent nuclei, and amphophilic granular cytoplasm in the intra-alveolar space is conclusive evidence of viral infection-induced cellular damage. In the advanced stages of the disease, the presence of fibrosis in lung tissue, as well as extensive bleeding and tissue necrosis, may result in severe impairment of respiratory function [10]. Fluid accumulation and extensive edema in this tissue, along with structural changes and extensive damage to the lung's functional units (respiratory bronchioles, alveolar ducts, and alveoli), can have a profound effect on the respiratory membrane's ability to serve as the site of gas exchange and disrupt the transfer of respiratory gases, especially oxygen molecules, from the respiratory membrane in COVID-19 patients [11].
When COVID-19 is severe, structural alterations in the lung tissue and damage to the respiratory membrane can predict impairment in the primary and ultimate function of the respiratory system, namely, the exchange of respiratory gases from the respiratory membrane. This is one of the most significant effects of the disease. The clinical data on COVID-19 patients indicate that their arterial oxygen pressure and, consequently, their percentage of tissue oxygen saturation are significantly low, which is strongly correlated with the severity of the disease and lung damage and may be hazardous to the patient's health [12].
A high-flow oxygen nasal tube and oxygen masks with a reservoir bag can be used to increase the gas's partial pressure in the alveoli and relieve the symptoms [13, 14]. However, in cases of more severe disease, mechanical ventilation may be required for these patients [13, 15, 16].
Studies indicate that age, gender, underlying diseases, breathing rate, hemoglobin oxygen saturation percentage (SpO2), level of consciousness, serum level of lactate dehydrogenase (LDH), interleukin-6 (IL-6), and C-reactive protein (CRP) are risk factors for death among hospitalized COVID-19 patients [17-19]. Typically, the disease is described as one with two distinct phases. During the first week of illness, cough, fever, and other symptoms are present with the highest viral load. Viruses can be detected in the respiratory tract for as long as nine days, and most patients experience improvement after the first week [20, 21]. However, the infection may be accompanied by an ineffective inflammatory response, lung inflammation, and lung damage in certain patients [21, 22]. The moderate to severe inflammatory response caused by COVID-19 is a proinflammatory cytokine storm or a presentation of profound immunosuppression. Despite this, the available evidence indicates activation of coagulation pathways, as evidenced by increased markers such as neutrophil recruitment, D-dimer, decreased production of antiviral defense mediators like autoimmunity and T-cell activation, interferon-α and -β, and increased systemic inflammatory markers like IL-8, IL-1, IL-6, and CRP, among other mechanisms [23].
IL-6 contributes significantly to the immune response against viral infections. In COVID-19-infected patients, however, its elevated levels can cause severe side effects. IL-6 is a soluble cytokine that is generated in response to tissue damage and infection. Its primary function is to serve as an early warning signal to the body by activating and enhancing the host's immune response via a variety of mechanisms. IL-6 induces acute phase reactants in the liver, including CRP, serum amyloid A, and others [17]. Despite the fact that these functions contribute to a robust host response and survival in the face of infection, they require a highly regulated process in which IL-6 levels are rapidly increased and regulated. This process is crucial because uncontrolled expression of IL-6 can lead to a severe inflammatory state with devastating consequences. Elevated levels of IL-6 can raise the risk of respiratory failure and death among COVID-19 patients. Findings indicate that COVID-19 patients who have uncontrolled rises in IL-6 levels have a poor prognosis for treatment [19, 24].
The IL-6 assay is an in vitro diagnostic test to quantitatively determine IL-6 levels in human serum and blood plasma. It helps detect a severe inflammatory reaction in COVID-19 patients, also known as a cytokine storm. As such, the most suitable respiratory support devices can be used immediately for these patients [25, 26].
According to studies, IL-6 and CRP levels are useful for diagnosing the severity of COVID-19, as their elevated levels indicate an exaggerated immune response and, as a result, the severity of the cytokine storm in these patients. CRP is a protein of the acute phase that is secreted by the liver in response to IL-6; its elevation is indicative of inflammatory reactions in the body. In a healthy state, the CRP level is negligible and undetectable. Nonetheless, it increases dramatically during inflammatory processes. According to studies, the degree of CRP elevation, such as IL-6, can indicate systemic cytokine release and disease progression [23, 27, 28].
Hospitalization and mortality are associated with older age, respiratory failure, loss of lymphocytes, and elevated serum levels of CRP and LDH enzymes in COVID-19 patients hospitalized in intensive care units (ICUs) [26, 28, 29].
LDH is one of the intracellular enzymes whose measurement can help the treatment team handle COVID-19 patients more effectively. LDH intracellular enzyme is widely present in body tissues. The kidney, liver, heart, skeletal muscles, brain, and lungs are among these tissues. Typically, an increase in LDH concentration is the result of cell apoptosis and the subsequent release of this enzyme into the bloodstream. LDH alone is not a differential test, as this enzyme can be measured in a variety of types of tissue damage. However, elevated LDH levels in the blood can be used in conjunction with other clinical symptoms and additional tests to diagnose respiratory failure and assess its prognosis [28, 29].
A crucial aspect of caring for COVID-19 patients is understanding the relationship between laboratory findings and variables such as the patient's SpO2 and type of respiratory support. Knowledge of this relationship facilitates the timely and appropriate use of the type of respiratory support to be provided to these patients, allowing for the provision of efficient treatment in the shortest amount of time and the most suitable clinical situation. In this study, we seek to answer the following question: “How are IL-6, CRP, and LDH serum levels related to SpO2 and the type of respiratory support received by COVID-19 patients?”
2. MATERIALS AND METHODS
A retrospective descriptive-analytical study was conducted to investigate associations between CRP, IL-6, LDH, SpO2, and the type of respiratory support received by COVID-19 patients admitted to the ICU. The study location was the ICU of 22nd-Bahman Hospital in Khaf, which is affiliated with Mashhad University of Medical Sciences. Based on the information available in the patients' clinical records, 31 eligible patients were recruited by the census in 2021.
An official letter of introduction was provided to the researcher to present to the appropriate staff at Khaf's 22nd-Bahman Hospital after the research protocol was accepted and authorization to perform the study was granted by the research ethics committee at Mashhad University of Medical Sciences. Subsequently, the researcher contacted the hospital's medical records office and reviewed the files of all eligible patients who were diagnosed with COVID-19 and admitted to the hospital's ICU during the specified period. A positive PCR test for COVID-19, at least 18 years of age, a history of COVID-19 ICU admission, and requests for CRP, LDH, IL-6, and ABG tests were among the inclusion criteria (to measure the SpO2 percentage level from the ABG test results).
The data collection instrument was a researcher-created checklist that comprised patient demographic details (namely, gender, age, history and type of underlying disease, history of COVID-19 vaccine injection, length of hospitalization) and tables for recording laboratory test results of patients upon admission to the COVID-19 ICU (including CRP, IL-6, LDH, and ABG tests). The initial biochemical tests requested for patients were serum IL-6, LDH, and CRP measurements. Moreover, the first ABG test requested for arterial blood gas respiration was used to determine the SpO2 percentage. As such, the initial tests requested by patients upon admission were examined and statistically analyzed. It should be noted that these tests were performed before any therapeutic intervention and therapeutic decision-making on how to manage patients' respiratory problems. So it can be said that first the tests requested by the doctor were taken by the nurses from the patients, and then the respiratory support interventions were applied to the patients.
The data were analyzed in the SPSS-22 statistical package using a one-way analysis of variance, the independent t, and Tukey's post hoc tests because the data followed a normal distribution. The significance level was established at p <0.05. Charts (1-4).
3. RESULTS
The current study analyzed data from 31 COVID-19 patients admitted to the COVID-19 ICU at the 22nd-Bahman Hospital. They were predominantly male (51.6%), married (80.6%), and illiterate (61.3%). In terms of age range and occupation, the highest frequencies concerned patients between 40 and 60 years (n=15, 48.4%) and homemakers (n=15, 48.3%). Twenty-three patients (74.2%) stayed in the hospital for more than three days, and they primarily (80.6%) had a history of diabetes. Additionally, four patients (12.9%) had no underlying disease, while fourteen (45.2%) had a history of two underlying diseases. Furthermore, 16 patients (61.3%) had a history of smoking, while 16 patients (51.6%) had never received the COVID-19 vaccine. Lastly, 23 patients (74.2%) made a full recovery and were allowed to leave the hospital, compared to eight patients (24.8%) who passed away (Table 1).
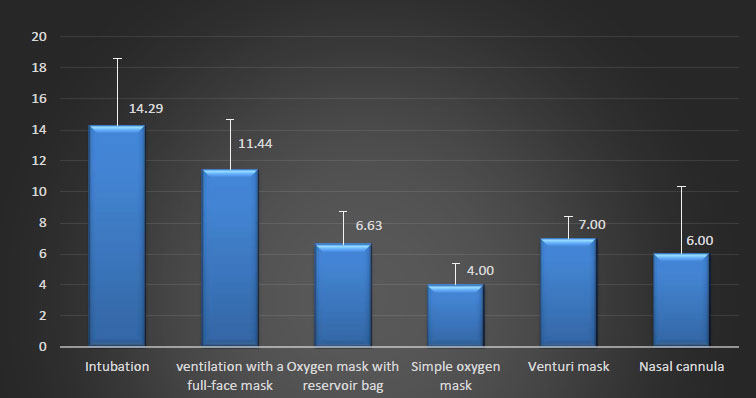
The mean serum levels of IL-6, CRP, and LDH in the patients with SpO2 <93 were greater than in patients with SpO2≥ 93 (p <0.05). The mean serum levels of IL-6, LDH, and CRP were significantly different (p <0.01) between patients receiving various types of respiratory support. The post-hoc analysis revealed that the mean serum concentrations of IL-6, LDH, and CRP were significantly greater in the patients receiving intubation respiratory support than in patients receiving other forms of respiratory support. In addition, the levels were higher in patients using non-invasive ventilation (NIV) full-face masks than in patients using oxygen masks with reservoir bags, simple oxygen masks, venturi masks, and nasal cannulas (p <0.05) (Table 2).
The mean serum concentrations of IL-6 and CRP were lower in patients with no or one underlying disease than those with two or three. Moreover, the mean LDH level in patients suffering from a single underlying disease was significantly lower than in those who had two or three underlying diseases (p <0.05). Recovered patients had lower serum levels of IL-6, CRP, and LDH compared to those who did not survive (p <0.01) (Table 3).
| Variable | Frequency | Percent | |
|---|---|---|---|
| Gender | Female Male |
15 16 |
48.4 51.6 |
| Education level | Illiterate Non-tertiary |
19 12 |
61.3 38.7 |
| Marital status | Single Married |
6 25 |
19.4 80.6 |
| Age (years) | < 40 40-60 > 60 |
12 15 4 |
38.7 48.4 12.9 |
| Occupation | Homemaker Self-employed Retired Unemployed |
15 5 4 7 |
48.3 16.1 12.9 22.6 |
| Hospitalization period | < 3 days ≥ 3 days |
8 23 |
25.8 74.2 |
| Underlying disease | Diabetes Cardiovascular Renal Cancer Respiratory |
25 17 4 1 2 |
80.6 54.8 12.9 3.2 6.5 |
| Number of underlying diseases | None 1 2 3 |
4 9 14 4 |
12.9 29 45.2 12.9 |
| Smoking history | No Yes |
12 19 |
38.7 61.3 |
| History of COVID-19 vaccine injection | No Yes |
16 15 |
51.6 48.4 |
| Patient outcome | Recovered and discharged Death |
23 8 |
74.2 25.8 |



| Variable | IL-6 | CRP | LDH | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| SpO2 | < 93 ≥ 93 |
353.311 ± 04.45 107.156 ± 63.12 |
10.4 ± 65.51 6.3 ± 38.46 |
683.190 ± 35.73 532.153 ± 88.11 |
| P-value based on independent t-test | 0.04 | 0.02 | 0.05 | |
| Type of respiratory support | Intubation Non-invasive ventilation with a full-face mask Oxygen mask with reservoir bag Simple oxygen mask Venturi mask Nasal cannula |
637.242 ± 00.50 397.251 ± 67.82 89.97 ± 75.82 30.10 ± 50.61 53.1 ± 00.41 19.9 ± 33.87 |
14.4 ± 29.35 11.3 ± 44.21 6.2 ± 63.13 4.1 ± 00.41 7.1 ± 00.41 6.4 ± 00.36 |
788.112 ± 71.36 734.202 ± 67.64 582.141 ± 00.09 421.137 ± 00.18 482.42 ± 00.42 461.125 ± 67.64 |
| P-value based on ANOVA test | < 0.001 | < 0.001 | 0.006 | |
| Variable | IL6 | CRP | LDH | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Number of underlying diseases | None 1 2 3 |
38.32 ± 25.87 47.20 ± 67.56 398.238 ± 29.04 705.306 ± 75.25 |
5.1 ± 00.83 6.2 ± 78.68 11.3 ± 00.49 15.5 ± 25.85 |
611.270 ± 50.15 502.141 ± 78.05 145.64 ± 692.25 828.177 ± 00.17 |
| P-value based on the ANOVA test | < 0.001 | < 0.001 | 0.01 | |
| Treatment outcome | Recovered and discharged Death |
172.205 ± 61.88 626.269 ± 38.29 |
8.3 ± 00.64 14.4 ± 00.38 |
593.185 ± 70.31 790.127 ± 63.11 |
| P-value based on the independent t-test | < 0.001 | 0.001 | 0.01 | |
4. DISCUSSION
Understanding the relationships between laboratory findings, the patient's SpO2, and the type of respiratory support administered is crucial to clinical care provision for COVID-19 patients. Knowledge of this relationship can aid in selecting the most appropriate type of respiratory support for patients, allowing them to receive effective care in the shortest possible time and under optimal clinical conditions. This research aimed to learn how SpO2, CRP, and LDH serum levels in COVID-19 ICU patients are related to each other and to the type of respiratory support they receive.
According to the data collected here, males accounted for a greater proportion of COVID-19 ICU patients than females. Consistent with this finding, other studies have reported a higher prevalence of COVID-19 infection in men [30-33]. Males exhibit a higher susceptibility to contracting COVID-19 compared to females, for which several hypotheses have been proposed. Li et al. suggest that the increased prevalence of COVID-19 in males could be linked to sex hormones and the crucial protective function of the X chromosome in innate immunity [31]. However, cultural factors account for the vast majority of this disease among men residing in Iran. There may be a correlation between the greater rate of COVID-19 infection among men and the prevalence of male-to-male contact, as more men than women in Iran work outside the home [32].
The current study found that the most common age range for patients was 40-60 years, with an average age of around 50 years. The observed research findings can be explained by the physiological changes in body tissue that occur with aging and old age. During this period, there are various changes such as muscle wasting, reduced endurance capacity, muscle weakness [34], increased vulnerability to infectious agents, decreased immune system function [35], hormonal changes, and a lower anabolic to catabolic hormones ratio [36]. Older adults are at a higher risk of infection due to various factors, including impaired immune function, nutritional deficiencies, bacterial colonization in mucosal surfaces, decreased physiological defense reflexes, and an increased prevalence of chronic diseases associated with infections [37]. Older adults with multiple diseases exhibit defects in their immune response to pathogens, organ dysfunction, and experience high mortality rates, hospital visits, ICU admissions, and disease-related complications.
The mean age of COVID-19 patients admitted to the hospital ward was around 50 years, which aligns with the results of previous studies conducted by Li et al. [31], Guan et al. [16], and Shahriarirad et al. [32].
The study revealed that a majority (87.1%) of COVID-19 patients admitted to the ICU had an underlying disease. The prevalent underlying diseases were diabetes, cardiovascular disease, respiratory disease, kidney disease, and cancer. The observed phenomenon can be attributed to the weakened immune response in individuals with pre-existing medical conditions. Therefore, these individuals are at a higher risk of contracting COVID-19. Infection can lead to a fatal illness requiring hospitalization [38]. The likelihood of developing a severe form of the disease is increased by the presence of an underlying condition, such as diabetes, hypertension, and cardiovascular or respiratory disease. Diabetes is considered the primary risk factor for contracting severe COVID-19 due to its impact on multiple organs. This is supported by research indicating that diabetes is associated with a higher risk of severe COVID-19 [39].
Corroborating this finding, other research demonstrates that most COVID-19 cases are linked to pre-existing medical conditions. Diabetes, lung disease, hypertension, and heart disease were identified as the most common underlying conditions in COVID-19 patients in the studies conducted by Shahriarirad et al. [32] and Nikpouraghdam et al. [40]. A 2020 cohort study conducted in the United States found that there was an association between type 2 diabetes and the risk of contracting COVID-19, which is consistent with the previous research [41]. Similarly, a cohort study conducted in England reported a positive correlation between diabetes, high body mass indices, and the probability of hospitalization due to COVID-19 [42]. The Chinese Center for Disease Control and Prevention reported in 2020 that people with cardiovascular disease and diabetes were at the highest risk of contracting the virus, after those with chronic respiratory disease, hypertension, and cancer [42, 43].
The study found that 61.3% of the patients had a history of smoking. The correlation between smoking and COVID-19 infection can be attributed to the fact that COVID-19 primarily affects the respiratory system. Individuals who smoke or initiate smoking during the pandemic are at a higher risk of contracting the virus and experiencing severe clinical outcomes, which may require specialized treatment in COVID-19 units. Individuals with a history of smoking or who currently smoke have a higher representation among those who have contracted severe COVID-19 and needed mechanical ventilation in ICUs [16]. This result aligns with previous studies that have established smoking as a risk factor for COVID-19 patient hospitalization [44, 45].
The mean serum concentrations of CRP, IL-6, and LDH were significantly greater in patients with SpO2 <93 than in patients with SpO2≥ 93, as found by the present study. In explaining this research finding, it can be stated that serological techniques are superior to other diagnostic methods for diagnosing infections [16]. Certain blood cells undergo transformations that can reveal the nature and severity of a disease. COVID-19 also causes alterations in the patient's blood cell count. In the study conducted by Chen et al. on 99 hospitalized patients with severe COVID-19, for instance, more than half of the patients had elevated serum LDH levels. In addition, fifty percent of patients exhibited a significant increase in the infection-related biomarkers interleukin 6, serum ferritin, CRP, and erythrocyte sedimentation rate (ESR). Another study on the blood samples of 1,099 patients infected with COVID-19 from different provinces in China revealed that in 83.2% of the patients, the level of lymphocytes was lower than normal, the level of CRP was very high in most of the patients, and the levels of alanine aminotransferase, aspartate aminotransferase (AST), LDH, creatine kinase, and D-dimer were elevated in patients [46]. Another study of clinical serological factors in 140 patients infected with COVID-19 in Wuhan revealed that 90% of patients had elevated levels of CRP, LDH, and serum amyloid [47]. In another study involving 138 patients, it was determined that the serology parameters had changed in these patients, resulting in a significant rise in the serum levels of CRP, creatine kinase, LDH, and blood factors [48]. A further study on the blood samples of 24 asymptomatic carriers with confirmed COVID-19 found that the number of lymphocytes was decreased in 16.7% of patients, and the levels of ALT, AST, IL-6, CPR, D-dimer, and creatine kinase were elevated in the majority of patients [49]. Results from a study of 41 patients with the severe form of COVID-19 indicated that 63% of them had abnormally low lymphocyte counts and elevated levels of certain other blood chemicals, including ALT, AST, D-dimer, bilirubin, creatinine, and LDH [50]. This study's finding, in line with findings from comparable studies, reveals a strong connection between the serum concentrations of IL-6, CRP, and LDH and the condition of COVID-19 patients.
The current study noticed that the mean levels of IL-6, CRP, and LDH differ significantly depending on the type of respiratory support provided to patients. Indeed, the findings revealed that the average serum levels of CRP, IL-6, and LDH were significantly greater in patients receiving intubation respiratory support than other types of respiratory support, as well as in patients receiving NIV with full face mask than patients receiving respiratory support with oxygen reservoir bag mask, simple oxygen mask, venturi mask, and nasal cannulas.
In the elaboration of this research finding, it can be noted that during the acute phase of COVID-19, the infection-related biomarkers such as interleukin 6, serum ferritin, ALT, AST, CRP, red blood cell sedimentation rate, etc. undergo significant deviations from their normal values, which can result in tissue and organ damage. In the acute phase, extensive and widespread damage to lung alveoli results in hyaline membrane formation in lung alveoli. Destruction of type 1 pneumocytes eliminates gas exchange, whereas destruction of type two pneumocytes eliminates surfactant secretion. The production of cytokines by fibroblasts is also increased under these circumstances. Alveolar macrophages secrete proinflammatory cytokines that recruit neutrophils, monocytes, macrophages, and T cells, resulting in extensive lung tissue damage and fibrosis [51, 52]. There are a number of distinct pathophysiological processes at play in the development of lung damage in these patients, such as intravascular thrombosis as a result of endothelial loss and damage, the absence of hypoxic pulmonary vasoconstriction as a result of endothelial dysfunction, and the delivery of an excess of blood to already damaged lung tissue [53].
As explained, higher serum concentrations of the studied markers, namely IL-6, CRP, and LDH, are associated with more lung tissue damage in COVID-19 patients. The patient requires advanced respiratory support in proportion to the increase in these markers. Therefore, it can be stated that patients with a high level of these serum markers are likely to require advanced airway care, such as NIV and intubation, whereas patients with lower levels of these serum markers will require respiratory support with other common methods, including nasal cannula, venturi mask, simple oxygen mask, and oxygen storage bag mask.
Consistent with this finding, Haghighi et al. found that the majority of the patients had SpO2 levels below 93% and were receiving NIV and intubation. In addition, there was a significant increase in LDH, liver enzymes, creatinine, hypoalbuminemia, hyperphosphatemia, hypercalcemia, hypermagnesemia, CRP, and ESR in the tests of these patients [54-56].
In addition, Pimentel et al. demonstrated in their study that there was a significant association between the mean breathing rate and the decrease in blood oxygen saturation in patients with blood markers such as LDH, elevated liver enzymes, positive CRP, and elevated ESR [55].
The current study revealed that the average levels of CRP and IL-6 were significantly lower in patients who had no or only one underlying disease than those who suffered from two or three underlying diseases. In addition, the average serum concentration of LDH was substantially lower in patients who had one underlying disease than in those with two or three cases. The fact that persons with underlying disorders have a less effective immune response and that COVID-19 infection results in significant alterations in blood tests such as CRP, IL-6, and LDH, as well as higher damage to the lung tissue, can both be used to explain this finding.
Other studies' findings support the current study's conclusion that having underlying diseases is one of the biggest risk factors for people with COVID-19. Studies looking at individuals with underlying illnesses have found that not only is the risk of contracting the disease higher in these people but also that they are more likely to pass away from the disease. Patients with COVID-19 who concurrently suffer from underlying diseases have a worse prognosis and experience increased disease symptoms and significant changes in serum liver enzyme levels, longer treatment courses, and a lower likelihood of recovery [16, 56-58].
The current study revealed that the mean serum concentrations of IL-6, LDH, and CRP were significantly lower in patients who recovered and were discharged than in those who perished. The serum levels of IL-6, CRP, and LDH rise during the acute phase of COVID-19, which ultimately causes widespread lung alveolar damage and the development of a hyaline membrane [53]. The research finding suggests that elevated serum levels of markers including IL-6, CRP, and LDH are linked to the decline in patients' health status and their need for invasive and non-invasive respiratory support, ultimately resulting in a high mortality rate among these patients.
In conformity with this result, Haghighi et al. reported a mortality rate of 58.90% among ICU-admitted COVID-19 patients with elevated concentrations of LDH, creatinine, hypoalbuminemia, liver enzymes, hyperphosphatemia, hypercalcemia, hypermagnesemia, CRP, and ESR [54].
In addition, the systematic review by Quah et al. showed that most patients hospitalized in the COVID-19 ICU with high concentrations of IL-6, ESR, liver enzymes, CRP, and LDH required aggressive and non-aggressive mechanical ventilation and finally passed away in ICUs [59].
CONCLUSION AND RECOMMENDATIONS
The present study disclosed a significant association between the initial tests of COVID-19 patients who suffered from underlying diseases and the type of respiratory support these patients required. In the clinical care provision of these patients, awareness of this significant association is one of the most important factors. Understanding the relationship between the serum levels of IL-6, CRP, LDH, and SPO2 and the type of respiratory support can help predict the management of acute respiratory patients, but this decision-making method based on serum levels should be further investigated and compared with the current methods of management of treatment of acute respiratory patients. In the early stages of COVID-19, parameters such as IL-6, LDH, and CRP are significant markers of inflammation and immune response that can significantly aid in the diagnosis of patients with the severe form of the virus. Moreover, researchers need to develop a scoring system that correlates IL-6, LDH, CRP, and SPO2 with the underlying disease in order to help clinicians in the early diagnosis of patients who are at risk of severe disease requiring advanced airway management.
LIMITATIONS OF THE STUDY
This study was hampered by a number of limitations. The first restriction was the incapacity to compute body mass index because the patients' height and weight were not recorded in the files. The second limitation of this study was the lack of examination of the anxiety and stress of patients hospitalized in corona wards, which can affect the results of the study indirectly. Another restriction was the exclusion of some patients from the study because the files did not contain all of the necessary information. Additionally, this study only included patients hospitalized in the 22nd-Bahman Hospital of Khaf's ICU during the first half of 2021. As a result, caution should be exercised when extrapolating the findings. The study was limited by the ICU's restricted medical resources and inability to accommodate all critically ill patients, resulting in the exclusion of this patient population from the study. In order to improve the precision and accuracy of COVID-19 disease characterization, it is advisable to conduct comprehensive and prolonged studies on all critically ill patients requiring special care.
LIST OF ABBREVIATIONS
| IL-6 | = Interleukin-6 |
| LDH | = Lactate dehydrogenase |
| CRP | = C-reactive protein |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This article reports the results of a research project approved by Mashhad University of Medical Sciences with the code of ethics (IR.MUMS.REC.1400.284).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All human procedures followed were per the guidelines of the Helsinki Declaration of 1975.
CONSENT FOR PUBLICATION
In order to comply with ethical considerations in this research, the information of the participants was kept confidential and other people were not able to access this information. The names and surnames of the participants were not used for data collection, and data collection was done after obtaining the code of ethics from Mashhad University of Medical Sciences.
STANDARDS OF REPORTING
STROBE guideline has been followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author [R.R] upon reasonable request.
FUNDING
This research was performed with the financial support of Mashhad University of Medical Sciences.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We would like to express our sincere gratitude to the honorable Vice-chancellery for Research of Mashhad University of Medical Sciences, the honorable officials of 22nd-Bahman Hospital in Khaf, the participants, and all the people who helped us in conducting this research.


