All published articles of this journal are available on ScienceDirect.
Understanding and Overcoming Barriers to Admissions and Timely Discharges in a Cancer Hospital: A Case Study of National Centre for Cancer Care and Research, Doha, Qatar
Abstract
Background
Improving access to healthcare is crucial for patient experience, clinical safety, timeliness of care, and reducing staff pressure. The National Centre for Cancer Care and Research (NCCCR), the primary cancer center in Qatar, confronted challenges in delivering quality cancer care and services.
Aim
This project aimed to identify factors limiting patient admissions and discharges at NCCCR to improve the average patient admission and discharge rates by 50%.
Methods
The study was conducted at the National Center for Cancer Care and Research (NCCCR) in Qatar from June 2020 to December 2021. Descriptive statistics were used to analyze the average number of inpatient admissions, discharges, and patient length of stay. The Plan-Do-Study-Act (PDSA) Model for Improvement tool was utilized to test changes at the facility level.
Results
A comparison of baseline data in Quarter 2 (Q2) 2020 with Quarter 4 (Q4) 2021 showed a 37% increase in the average number of inpatient admissions and a 62% increase in inpatient discharges. The number of patients staying 0-10 days increased by 39% from Q2 2020 to Q4 2021.
Conclusion
This project identified several factors affecting patient admission and discharge services. Implementation of strategies such as establishing a physician-led discharge multidisciplinary committee, conducting frequent bed status evaluations by case managers and physicians, and expanding bed capacity led to significant improvements in the admission and discharge process.
1. INTRODUCTION
The demand for cancer care services among patients is increasing due to a rise in new cancer cases, a growing number of cancer survivors in need of follow-up treatment, and a shortage of oncology care providers. These factors impact cancer programs' ability to meet patient demand, and the recent COVID-19 crisis has exacerbated long-standing patient access issues [1].
To demonstrate their commitment to patient-centered care, cancer programs are implementing innovative models to boost their capacity and patient access. They understand that patients who receive a cancer diagnosis but cannot access services promptly may seek care elsewhere. Some techniques involve expanding the workforce or productivity standards to boost capacity, while others are more innovative, like establishing new treatment facilities tailored to specific patient demographics, such as survivorship centers and clinics for benign tumors.
Cancer is a complex medical condition that often requires intervention from multiple healthcare providers over extended periods and at various stages. A study in the UK found that, on average, cancer patients saw 28 different doctors during their treatment, not accounting for other medical professionals involved in their care. This complexity presents significant challenges for healthcare professionals in hospital and community settings to deliver well-coordinated patient care [2].
Qatar, a small nation on the Arabian Peninsula, has experienced rapid development in recent decades. It has a high per capita GDP and a young native population, along with a substantial expatriate community. Cancer has become the second most common non-communicable disease in the country, following cardiovascular disease. Projections suggest that cancer incidence will triple between 2010 and 2030 due to population aging and growth.
A retrospective cohort study based on the Qatar cancer registry (1991-2006) revealed that cancer is a significant public health issue in Qatar, with incidence increasing with age and higher rates among women compared to men [3]. Qatar's population presents unique challenges in disease presentation and spread, with implications not only internationally but also for the Gulf region and the global Arabian diaspora. The country has a robust Cancer Research Infrastructure through academic partnerships, positioning it to contribute significantly to cancer research. Public healthcare is accessible to all residents who have paid a minimum health insurance fee, including coverage for cancer care services [4].
In 2011, Qatar launched its First National Cancer Control Program within the Gulf Cooperation Council. The National Cancer Strategy aimed to transform cancer care in the country over five years, establishing governance frameworks for execution. As Qatar's population is expected to grow significantly, strategic direction is crucial to ensure all healthcare tiers are engaged [5]. The strategy focuses on enhancing cancer care from prevention to treatment quality, aiming to improve patient admission and discharge services at the National Center for Cancer Care and Research (NCCCR) by 50%.
1.1. Statement of the Problem
Cancer is a significant global issue, with an increasing number of people being diagnosed, making it a leading cause of death. The World Health Organization (WHO) has emphasized the importance of all countries developing strategies to control cancer, including prevention, early detection, and effective treatment at all stages, including post-treatment. Qatar responded to this challenge by implementing “The National Cancer Strategy: A Path to Excellence (2011–2016).” WHO data from 2015 indicates that cancer is a leading cause of premature death in many countries, including Qatar.
The National Center for Cancer Care and Research (NCCCR), as Qatar's sole cancer care center, faces various challenges in meeting the growing demand for cancer care while maintaining high-quality services. This project aims to explore the chronic nature of cancer and the increasing number of cancer patients as the primary reasons for delayed admissions at NCCCR in Doha, Qatar. Additionally, limited hospital space has been identified as a bottleneck for admissions.
Delays in the discharge process are primarily due to pre-discharge procedures and payment settlement issues. Furthermore, appointment dates for treatment, such as chemotherapy, are not visible to all healthcare staff in the electronic health record, leading to difficulties in monitoring patient length of stay, payment concerns, and unsafe living conditions that hinder timely discharge.
Patients and their families have expressed dissatisfaction with prolonged waiting times for admission due to bed unavailability, impacting overall patient satisfaction. This, in turn, creates pressure on staff to manage bed resources efficiently, potentially compro- mising patient care. By examining the admission process, identifying root causes of delayed admissions, and addressing barriers to timely discharge, we aim to improve patient access at the cancer hospital by enhancing average patient admission and discharge rates. Therefore, this study aims to identify factors that limit NCCCR patient admission and discharge services and thus improve the average patient admission and discharge by 50%.
1.2. Access to Care - Current State
Care Coordination encompasses numerous aspects of health service provision, including appropriate, timely care provided by a multidisciplinary team comprising medical doctors, nurses, and allied health professionals. Other vital elements intrinsic to cancer care coordination include psychosocial assessment, timely referral, information provision, and individualized treatment personalized to each patient's needs and preferences [6]. Therefore, a lack of coordinated care can lead to fragmented care, patients getting “lost” in the system, and failing to access appropriate services. In addition, it can also cause unplanned visits and utilization of services and staff that can create chaos in the systems [7, 8]. A study conducted in Public Health Institutions in Limpopo Province, South Africa, found shortages in staff for comprehensive cancer care, inadequate patient management and support, and lack of coordination in cancer services. Participants suggested strategies to enhance patient satisfaction and health worker fulfillment by addressing human and system-related issues. They recommended implementing systems to reduce risks from these factors and improve patient satisfaction [9].
The Cause-and-Effect diagram (Fig. 1) illustrates the four factors leading to impaired access and discharge processes in the hospital. A leading problem of delayed health care delivery stems from unresolved and unmanageable pending admissions of cancer patients. At the same time, discharging patients from acute hospitals is challenging, especially in the context of limited resources and an aging population. The below-mentioned contributing factors caused hindrances in accessing care. Mismatches in admission and discharge rates with poor coordination of bed availability to prepare for peak admission time do not favor patient flow in any healthcare situation. To handle the high demand for admissions from the urgent care department, it is suggested to discharge patients early by evaluating patient status [10]. Less critical patients and those who do not require hospital management were assessed by the physicians and hence, were not admitted and were given discharge instructions as per the condition of the patients. Less urgent and non-urgent patients are treated according to the CTAS (Canadian Triage Acuity System) protocol. Since the hospital has only urgent care units and not an emergency department, the urgent care unit of NCCCR receives fewer urgent and non-urgent patients.
The delay in the discharge process was mainly attributed to the pre-discharge procedures and payment settlement issues. These concerns were attended to promote early discharge. The problems of unclear discharge workflow, lack of structured pathways to admission and discharge, and limited bed capacity were the main adversities to early discharge.
1.2.1. Manpower Factors
The following obstacles were identified in the cancer center concerning the workforce: Staff shortage, Unclear physician roles, lack of leadership support, lack of adequate involvement of a multidisciplinary team in reviewing possible discharges, and lack of early involvement of social workers.
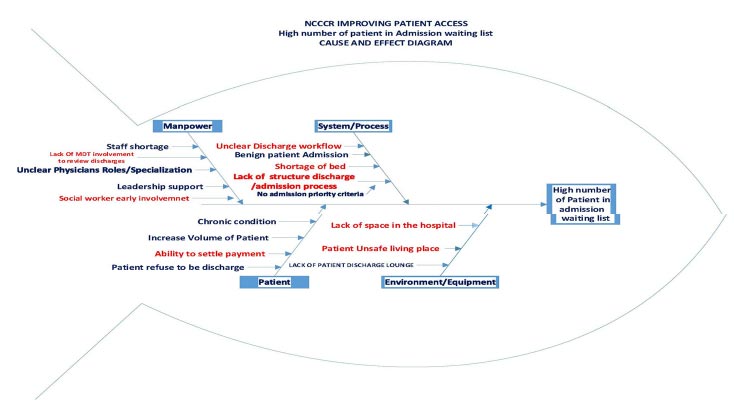
1.2.2. System/process Factors
Shortage of beds, unclear discharge workflow, lack of structured discharge and admission processes, and, most importantly, no admission priority criteria were the major hurdles.
1.2.3. Patient Factors
This includes an increased number of cancer patients, chronic conditions, patient refusal to discharge, and payment settling issues.
1.2.4. Environment/Equipment Factors
Lack of space in the hospital, lack of a patient discharge lounge, and patient unsafe living place were the primary concerns.
Therefore, we initiated a study to identify the factors related to care access and their influences on admission and discharge processes in the cancer hospital.
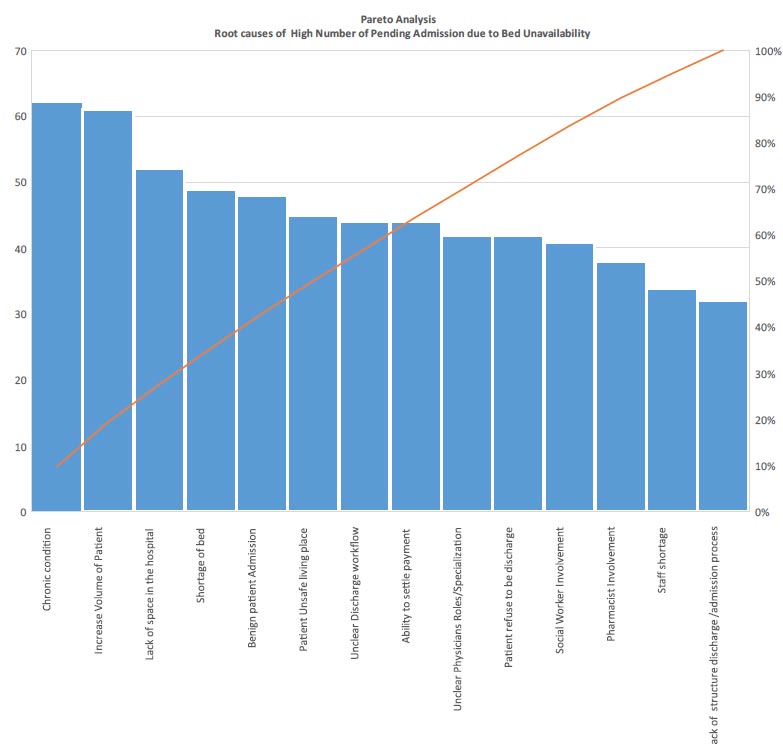
2. METHODS
A Pareto causes rating survey with a rating scale from 1 (lowest impact) to 10 (Highest impact) considering the effects on cost, time, and resources was conducted among hospital staff, including 4 physicians and 7 nurses and 1 Pharmacy supervisor, to prioritize the root causes leading to delayed access to care and the high number of pending admissions. Pareto analysis leads a project team to focus on the vital few problems or causes of problems that significantly impact the quality effect the team is trying to improve [11]. The Pareto analysis Causes Rating Survey regarding a high number of pending admissions is plotted (Fig. 2).
The Plan-Do-Study-Act (PDSA) is used as a model for improvement to test the initiatives with changes, and several initiatives were proposed and tested for improvements. The program seems to work best for identifying implementation challenges and optimizing the implementation of evidence-based intervention into practice [11].
2.1. Inclusion Criteria
• All patients requiring admission to NCCCR. (Elective, patient from UCU, transfer from other HMC facilities)
• All patients in the pending admission/waiting for bed.
2.2. Exclusion Criteria
• Patients with no admission order
• Patients not under Oncology, Hematology, and Palliative care.
• Benign case
• Age less than 14 years
2.3. Measures of Improvement
With the PDSA model for improvement, measures of improvement were stated in terms of the following:
• Outcome measures: The project's outcomes were measured in terms of average inpatient admission per month, average inpatient discharge per month, and percentage of Patient Discharge before 11 am.
• Process measures: This included the percentage of patients with discharge orders written before 9 am.
• Balancing measures: This included Patient / Staff satisfaction and Readmission Rate within 28 days.
2.3.1. PDSA 1
A physician-led multidisciplinary discharge team was established in NCCCR to assess patients' eligibility for discharge. This integrated team, consisting of physicians, nurses, pharmacists, and case managers, has been operational at the hospital. The team's formation resulted in early discharge orders from physicians, timely prescription of discharge medications, completion of care plans, holistic care by nurses, and prompt dispensing of medications by the pharmacy. Multidisciplinary care, with regular team meetings, is considered essential for providing high-quality, coordinated cancer care [12]. Ideally, these meetings should involve clinical, primary, community, and allied health professionals to facilitate efficient treatment planning, streamline referral processes, and prevent unnecessary or duplicate examinations [13].
2.3.2. PDSA 2
Case managers and physicians conducted a daily review of bed availability by examining the discharge coordinators' list of patients expected to be discharged hospital-wide. Additionally, daily meetings were held on the ward with the discharge team to monitor patient progress. Discharging patients from acute hospitals is known to be a complex task [14].
2.3.3. PDSA 3
A survivorship clinic and benign tumor clinics were established in the Ambulatory Care Centre (ACC) for cancer patients at NCCCR to alleviate the patient load at the cancer center. Satellite clinics offering specialized oncology services for hematology and gynecology tumors began operating at HMC, including Al Wakra Hospital, Al Khor Hospital, and Women's Hospital. This expansion aims to improve patient access to cancer services, considering the growing number of cancer survivors in other countries like the United States. In the United States, there are already 16.9 million cancer survivors, and projections indicate that number will rise to almost 22.1 million by 2030 [15].
2.3.4. PDSA 4
Patient access was enhanced through capacity expansion, including increasing the number of beds in the daycare unit from 20 to 50, the urgent care unit from 6 to 9, and short stay unit from 4 to 10. An additional 16 beds were added to the inpatient care facility, along with 56 beds in the Patient Recovery Centre for chronic and long-term cancer patients.
2.3.5. PDSA 5
A pending admission list was incorporated into the daily patient review to identify potential discharge candidates daily, updating as pending admissions are resolved. This initiative was a collaborative effort between the patient flow team and designated discharge coordinators.
2.3.6. PDSA 6
A new admission criteria tool was developed to assist the patient flow team and physicians in prioritizing cases for proper bed allocation upon admission. This tool consists of 11 criteria ranked by priority to determine the most urgent cases for admission, ensuring patients receive timely and appropriate treatment (Table 1).
| S.No. | Patient Category | Priority Rate |
|---|---|---|
| 1. | Newly diagnosed leukemia patient | 1 |
| 2. | Newly diagnosed lymphoma patients with bulky diseases | 1 |
| 3. | Febrile neutropenia patient in UCU | 2 |
| 4. | Leukemia patient for chemotherapy | 2 |
| 5. | Germ cell treatment for chemotherapy | 2 |
| 6. | Post-chemotherapy with multiorgan failure | 2 |
| 7. | Septic patient in UCU | 2 |
| 8. | Post chemotherapy complication | 3 |
| 9. | Ovarian/gestational malignancy for urgent chemotherapy | 3 |
| 10. | Symptomatic palliative patient | 3 |
| 11. | Elective admission for long protocol/chemotherapy (3-5 days duration) | 4 |
Priority 2: Admission within 24 hours from the requested admission date and time
Priority 3: Admission within 1-3 days from the requested admission day
Priority 4: Admission when bed is available within 4-7 days of the requested admission date
2.4. Change Concepts
2.4.1. Improved Admission and Discharge Process
A structured physician-led discharge team developed and implemented an admission criteria tool after reviewing the existing admission/discharge criteria and policies. This tool was created after prioritizing the admission needs of the patients. A list of waiting admissions, discharges per specialty, and discharges per unit served to guide the admission/discharge process. Physicians were encouraged to engage in the continuous evaluation of the discharge process. The HMC discharge policy was reviewed and analyzed to enhance the patient's discharge process. Points of delay in the discharge continuum were identified. Reminder emails were sent to the units and departments to comply with timely discharge. The scope of services in the units has been revised.
2.4.2. Leadership Support
Daily leadership meetings were held to update on the admission/discharge status with an emphasis on the 11 set criteria (given above in table form) of the new admission criteria tool. With an increasing number of cancer patients considering cancer clinics established in ACC, leaders envisioned expanding bed capacity and clinic services outside NCCCR. The number of benign cases and their admission policies were revised. The method of delivering care for them resulted in the formation of satellite clinics in the Ambulatory Care Unit. Patients with benign tumors and cancer survivors started consulting doctors and continued their follow-up in satellite clinics. Therefore, services for cancer patients broadened across HMC.
2.4.3. Patient and Family Involvement
A proactive plan for discharge was initiated, and care providers were asked to identify patients with complex needs. A discharge checklist was developed and tested for early patient discharge. All patients and families were informed of the discharge planning upon admission. Patients and families began to realize the importance of early discharge, and stakeholders adhered to the timely discharge process.
2.4.4. Effective Communication
ISBAR communication was encouraged among healthcare professionals. Discharge planning was added as a primary agenda in safety huddles and physicians' morning reports. Reliable and timely communication was developed with the primary team of doctors to initiate the discharge plan upon admission. Reliable handoffs and hospital safety huddles with a priority on timely discharge facilitated the process.
2.4.5. Multidisciplinary Team Involvement and Collaboration across HMC Facilities
A significant number of cancer patients were followed up by the home health team, and many patients were cared for by the Patient Recovery Centre (PRC) for continued care and follow-up care for cancer patients. This helped reduce the burden on bed occupancy in NCCCR. Patients in need of follow-up blood tests and subcutaneous injections were taken care of by the home healthcare staff. The rehabilitation department of NCCCR was shifted to Qatar Rehabilitation Institute (QRI), which includes physiotherapy and lymphoedema clinics to follow up with cancer patients in need of these services, allowing room to accommodate more patients in the urgent care unit. Mobile health services and patient recovery centers are utilized for cancer patients post-discharge, intending to provide a safe environment and symptomatic care. The involvement of MDT key staff in discharge planning and front-line nurses in notifying physicians to write the expected date of discharge (EDD) upon admission was crucial in determining patient discharge. Workforce and manpower support in achieving the target goals enabled improving access, admission, and discharge processes.
2.4.6. Capacity Enhancement
Factors like faster bed occupancy rate, increased patient volume, unexplained LOS, and minimum bed capacity in the facility led to the establishment of new beds in Ward 4 and the urgent care unit (UCU), expansion of the Day Care Unit, as well as the Short Stay Unit. The utilization of the unit was reviewed, along with other HMC facilities like Rumeillah Hospital, to find space and accommodate more beds for NCCCR hospital.
3. RESULTS
We analyzed the responses of 12 healthcare personnel (Fig. 2), including 4 physicians, 7 nurses, and 1 pharmacy supervisor, using a Pareto Causes Rating Survey scale to identify the root causes of pending admissions in the cancer facility with a rating scale from 1 (lowest impact) to 10 (highest impact) considering the effects on cost, time, and resources. 92% of the respondents reported the patients' chronic condition as the root cause for the pending admission, followed by the increased volume of patients (91%) as the second root cause for the pending admissions. More than 70% of respondents reported a lack of space in the hospital as an essential hindrance to admitting patients. The root cause analysis also showed that the delay in the discharge process mainly occurred due to the pre-discharge procedures and payment settlement issues.
The data on inpatient admissions and NCCCR discharges per quarter from 2020 to 2021 were also evaluated. In Fig. (3), it is evident that the number of patients getting admitted with cancer is increasing in number by each quarter. This shows that the cancer burden is increasing among the population. The average number of cancer patients getting admitted improved by 37% (Fig. 4) and the average number of discharges by 62% (Fig. 4) after implementing the PDSA-tested change concepts such as a physician-led discharge committee, new admission criteria tool, and physical expansion of the hospital focusing on bed capacity. A 39% increase in the number of patients whose LOS was from 0-10 days (Table 2) and a drastic decrease in the Length of Stay of patients staying 20 days because of the introduction of the discharge checklist, daily review of the need for a stay in the hospital, selection of discharge champions among physicians, and timely involvement of social worker and case managers.
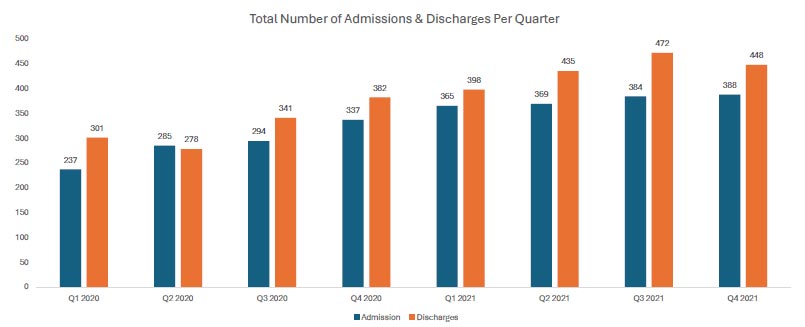
The quarterly number of NCCCR Inpatient Admission and discharges in comparison with the baseline data in Q2 2020 and Q4 2021; Fig. (3) shows that the cancer burden is increasing among the population in Qatar by quarter.
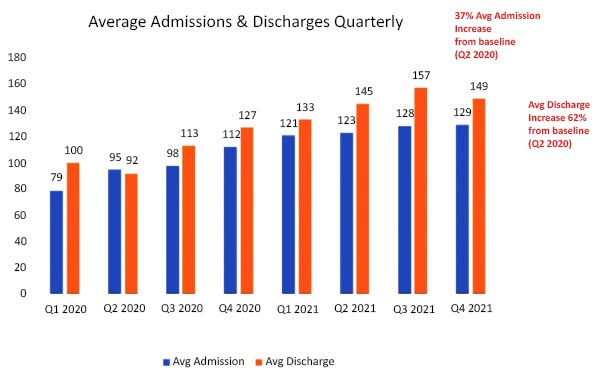
37% increase in the average number of Inpatient patient admission and 62% increase in inpatient discharges. This was calculated using the formula of percent of change. The average number of cancer patients getting admitted improved by 37% (Fig. 4) and the average number of discharges were improved by 62% (Fig. 4) after implementing the PDSA-tested change concepts such as physician-led discharge committee, new admission criteria tool, and physical expansion of the hospital focusing the bed capacity.
This was calculated using the formula of percentage of change which is as below:
Percentage of change = Original Value -New Value x 100 / Original Value
Percent increase = (increase / original value) x 100
or
Total number of discharges in Quarter 4 2021 - Total number of discharges in Quarter 2 2020 x 100 / Total number of discharges in Quarter 4 2021.
| Stay Duration of Patients (LOS) | Q1 2020 | Q2 2020 | Q3 2020 |
Q4 2020 |
Q1 2021 | Q2 2021 | Q3 2021 | Q4 2021 | Percentage of Change from Baseline Q2 2020 |
|---|---|---|---|---|---|---|---|---|---|
| 0-10 Days | 125 | 126 | 156 | 184 | 163 | 190 | 153 | 256 | 11.8 ↑ |
| 10-20 Days | 54 | 56 | 67 | 80 | 77 | 76 | 61 | 80 | 2.3 ↓ |
| 20-30 Days | 46 | 45 | 48 | 48 | 48 | 33 | 27 | 48 | 5.5 ↓ |
| Greater than 30 days | 76 | 51 | 65 | 61 | 55 | 64 | 49 | 64 | 4.1 ↓ |
There was an increase in the admission rate to 100% from the urgent care unit to inpatient units. The average patient waiting per day was reduced by 72%. The number of outpatient visits of oncology survivors in satellite clinics at the Ambulatory Care Centre during the period of September 2020 to December 2021 was 4,104. The number of patients who visited the benign hematology clinics was 7,547.
4. DISCUSSION
There is a wealth of research on the advantages and necessity of care coordination for cancer patients [7, 16]. Research on the present obstacles to effective care coordination, as reported by patients, caregivers, and medical professionals, is, however, lacking. The identification of existing challenges may serve as a roadmap for the creation of new projects aimed at enhancing the quality of coordinated healthcare.
Focusing on the illness experience and its impact on both patients and their families, alongside treating the tumor, is crucial for enhancing cancer outcomes. With the shift towards value-based care over fee-for-service models, understanding what patients consider valuable is essential for improving results. Additionally, systematically monitoring and improving treatment through measurements like patient experience is crucial for progress [17].
Key barriers identified in the admission-discharge process of NCCCR:
- The unavailability of patient appointment dates in the daycare, short stay, and inpatient units.
- Limited number of beds in short stay unit, daycare unit, and inpatient units.
- Payment unable to settle.
- Poor and unsafe living conditions of patients.
- A long list of pending admissions compromising the quality of patient care and satisfaction.
Improvements were achieved by altering the following factors:
4.1. Manpower Factors
With the introduction of a physician-led integrated discharge committee, the need for members with decision-making capacity from all disciplines was added as the main stakeholders of the committee. The case managers and social workers intervene early in the process to make discharges faster. It could also be attributed to recognizing health professionals' roles and responsibilities in healthcare provision. The introduction of discharge advocates among physicians also led to the early discharge process.
4.2. System Factors
It was made essential to communicate with all primary care providers regarding daily patient reviews for discharge readiness. Discharge planning communication was made through safety huddles and clinical staff handoff. The pending admission list is also added along with the patient list to allow for more visibility of patients waiting for admission. A noncompliance report regarding the failure to assess the need for daily discharge review was sent to the concerned physicians.
4.3. Patient Factors
It was made a priority to plan for patient discharge at the time of admission. The team assigned to the patient's care had to review the patient's clinical condition. The patient's family was actively involved in discharge planning upon admission. The patient's needs were identified, and goals were set upon admission to facilitate the discharge process at the earliest.
4.4. Environmental Factors
The facility's capacity and physical layout were redesigned to increase patient services and improve access to care. This was achieved by a massive expansion of the facility. The Urgent care unit was expanded from 6 beds to 9 beds. The Daycare unit was expanded from 20 beds to 50 beds. The short-stay unit was extended from 4 to 10 beds. The inpatient unit Ward 1 was expanded from 24 to 28 beds. The bed capacity of ward 2 was increased from 26 to 28 beds. The patient recovery center is a 56-bed facility that was later handed over to NCCCR for cancer patients to find space for patients discharging from NCCCR, which provides more amenities to enhance the quality of life of patients. Satellite clinics were opened in the Ambulatory Care Center to support and care for specific patient populations, such as benign tumor and survivorship clinics.
5. LIMITATIONS
The Pareto causes rating was done among a few hospital healthcare professionals. Moreover, the percentage of physician orders for discharge before 9 am was viewed as a process outcome, which was significantly lower (<40%). Hence, patient discharge before 11 am is still an unresolved problem, creating no possibility for new admissions. These areas need more research and analysis.
CONCLUSION
Timely morning discharge remains a challenge; however, our interventions were able to mediate improvements. The study's findings demonstrate that a quality improvement intervention based on the PDSA methodology can enhance the admission discharge pathways and lower LOS through helpful strategies like forming a discharge committee and developing a new tool for admission criteria that aims to enable the most effective admission discharge mechanism given the resources at hand. This project aimed to identify factors that limit NCCCR patient admission and discharge services and thus improve the average patient admission and discharge by 50%. Hence, the average number of cancer patients getting admitted improved by 37% and the average number of discharges improved by 62%.
When evaluating intricate operational processes with several stakeholders, the PDSA technique proves to be an efficient means of enhancing quality. To address admission discharge delays, institutions should prioritize implementing the fundamental tenets of PDSA over potentially institution-specific solutions. Further projects that focus on other factors affecting admission and discharge are yet to be studied to enhance further and sustain early admission and timely discharge.
AUTHORS' CONTRIBUTIONS
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| NCCCR | = National Centre for Cancer Care and Research |
| GDP | = Gross Domestic Product |
| PDSA | = Plan-Do-Study-Act |
| Q1 to Q4 | = Quarters 1 to 4 |
| LOS | = Length of Stay |
| UK | = United Kingdom |
| UCU | = Urgent Care Unit |
| HMC | = Hamad Medical Corporation |
| ACC | = Ambulatory Care Centre |
| PRC | = Patient Recovery Centre |
| QRI | = Qatar Rehabilitation Institute |
| ISBAR | = Introduction Situation Background Assessment and Recommendation |
| MDT | = Multidisciplinary Team |
| EDD | = Expected Date of Discharge |
| QoL | = Quality of Life |
ETHICAL STATEMENT
The National Centre for Cancer Care and Research does not require ethical approval for reporting a quality improvement project.


