All published articles of this journal are available on ScienceDirect.
Prevalent Clinical Assessments of HIV Positive Infants in a South African District Hospital
Abstract
Background
HIV/Aids continues to be a major factor in the morbidity and mortality of children in South Africa. Despite the implementation of new guidelines to lower mother-to-child transmission in the country, some infants are admitted to hospitals undetected and or in alarming conditions.
Aim
To determine the most prevalent clinical assessments of HIV-positive infants admitted at Odi District Hospital, South Africa.
Methods
This was a cross-sectional study based on a retrospective records review of all HIV-positive infants admitted at Odi District Hospital in Pretoria from the 1st January 2010 to 31st December 2012.
Results
Only 10.2% of the 962 files of infants admitted to Odi Hospital were HIV-positive infants, with the majority (58.2%) in the 7–12-month age range and a high admission rate (57.1%) for males. Twenty-five percent of infants had a diagnosis prior to admission. There were 44.9% lower respiratory tract infections, 25.5% malnutrition and failure to thrive, 2.4% gastroenteritis, 2% meningitis, 2% febrile convulsions, and other diseases like encephalopathy and dehydration.
Conclusion
The current study has presented lower respiratory tract infection as the most prevalent clinical assessment and cause of morbidity among HIV-positive infants admitted at Odi District Hospital in Pretoria, South Africa. In order to provide a comprehensive view of the issue, additional studies with large sample sizes are advised.
What This Study Adds
The study presents the prevalence of associated clinical conditions among infants with HIV/AIDS, listed in descending order at a South African district level of care.
1. INTRODUCTION
In 2021, there were 25.6 million people living with HIV in the world, with the African region being the most impacted. Despite this statistic regarding prevention and management of the infection, there has been an improvement over the previous ten years, with a 44% decrease in new infections and a 55% decrease in AIDS-related deaths. The World Health Organization (WHO) and its partners utilized several platforms to achieve this target, and some of those avenues were access to reasonably priced medications, diagnostics, and health technologies [1]. Yet, HIV/Aids is still a problem in the Sub-Saharan African region, specifically in South Africa, where the prevalence of people living with HIV (adults and children) was 7.5 million, and for children aged 0 to 14 years was around 2.7 million in 2021 [2]. Aligned with the improvement occurring in the management of the situation or HIV infection, since the approval of zidovudine as the first antiretroviral (ARV) medication in 1987, the management of HIV/AIDS has significantly advanced and upgraded [1]. The life expectancy of HIV-positive people has grown as a result of antiretroviral therapy (ART), bringing it closer to that of non-infected people [1]. The development occurring in ARV therapy, specifically for children, has been highlighted by the ODYSSEY trial, published in 2022 [3]. The trial was carried out in a few African nations, including South Africa, Uganda, and Zimbabwe, and children weighing 3 kg to less than 20 kg were enrolled. They received dispersible tablets of dolutegravir in accordance with WHO weight bands. Through this trial, the majority of children weighing 3 kg to less than 20 kg were exposed to dolutegravir. The trial's findings assisted in the modification of the WHO's recommendations for pediatric antiretroviral dosage and formulation, as well as the approval of the dolutegravir dispersible tablets by regulatory bodies. Additionally, children older than 4 weeks will have access to the medication globally once dolutegravir dispersible versions are made available in low- and middle-income countries [3].
Taking into consideration the different efforts made in improving ARVT in children, they are still brought to the hospital and clinics without being tested for HIV, as well as in alarming conditions; as a result, this research study would like to determine the most prevalent clinical assessments of HIV-positive infants admitted in a South African district hospital.
2. LITERATURE REVIEW
It is estimated that approximately 1.8 million children under the age of 15 were living with HIV in 2020 [4]. South Africa has the largest number of people living with HIV worldwide, with 7.3 million adults in 2021 and 270,000 children aged between 0 and 14 years in the same year [5, 6]. Globally, approximately 1.7 million new HIV infections were reported in 2019, of which 9% were in children [4], and of which 84% were children in Sub-Saharan Africa [4]. There were 10,000 newly infected children aged 0 to 14 years in South Africa in 2021 [5], and deaths due to AIDS in this age group were 2800 in the same year [5]. Sadly, only 48% of children with HIV aged 0 to 14 years received anti-retroviral therapy (ART) in South Africa in 2021 [5].
Great progress has been made in the elimination of vertical transmission of HIV in South Africa [7] and therefore, a reduction in the number of HIV-infected infants can be seen [7]. Mother-to-child transmission is, however, still the biggest cause of HIV infection in children under five years in South Africa, and AIDS is the leading cause of death in children under five [6]. ART use by pregnant women may, however positively impact an infant's immune response and birth weight, and the degree of maternal immunosuppression has been shown to be an important predictor of infant survival [7]. In 2021, 277,543 South African pregnant women received ART for Prevention of Mother to Child Transmission (PMTCT), and an estimated 290,000 pregnant women needed ART for PMTCT. Early infant HIV diagnoses were 94%, and the vertical transmission rate and transmission of infections through breastfeeding was 3.51%. New HIV infections averted due to PMTCT were estimated at 40 000, and the number of HIV-exposed children who are uninfected is 4,100,000 [5]. There were, however, an estimated 320,000 children living with HIV in South Africa in 2016, and this resulted in South Africa having the largest pediatric antiretroviral therapy program in the world [8]. According to 2021 WHO updated recommendations on HIV prevention, infant diagnosis, antiretroviral initiation and monitoring, point-of-care nucleic acid testing should be used to diagnose HIV among infants and children younger than 18 months of age should these infants be at risk of vertical HIV transmission [9]. This early testing aids in the diagnosis and initiation of treatment of HIV-positive infants.
The hallmark of HIV is immune suppression [10]. When organisms that don’t normally cause disease become pathogenic due to an impaired immune system, those infections are called opportunistic infections [11]. Alternatively, when common pathogens cause unusually severe infections, this can also be referred to as opportunistic infections [11]. Opportunistic infections can be caused by bacteria, fungi, viruses, or parasites [11]. Advanced opportunistic infections and suboptimal viral suppression resulting from immune suppression are the leading causes of morbidity and mortality in HIV-infected infants [4, 10, 12] and present as pneumonia, chronic diarrhea, and malnutrition.
Globally and in South Africa, lower respiratory tract infections are a common cause of death in infants with HIV infection [7]. Despite early ART, respiratory disease remains the primary cause of hospital admissions in children living with HIV [12], with pneumonia being the most prevalent opportunistic infection in infants [10]. Bacterial pneumonia in HIV-positive infants showed higher mortality rates than viral pneumonia [7]. Streptococcus pneumonia is the leading bacterial cause of pneumonia and related mortality in children under five years in 2015 in South Africa [13]. Other common causative organisms of community-acquired pneumonia in HIV-infected infants include Respiratory syncytial (RS) virus, Pneumocystis jirovecii, Mycobacterium tuberculosis [7], group B Streptococcus, Listeria monocytogenes, Escherichia coli, Klebsiella pneumoniae, and Mycoplasma pneumoniae [13].
HIV and tuberculosis (TB) infection commonly occur together and exacerbate each other [14]. TB is the biggest cause of mortality in HIV-infected people, including infants [15]. Both infections cause a decrease in the CD4 cells and are therefore immunosuppressive. This suppression of the immune system can lead to progression from latent to active TB infection [13]. HIV infection also suppresses the body’s innate response to TB infection. Therefore, these two infections are also known as “the cursed duet”. [14, Culture-positive and –negative TB infections commonly occur in HIV-infected infants [14]. HIV-positive infants commonly develop TB meningitis or military TB, a more severe infection than pulmonary TB [14]. Severe immunosuppression also worsens an infant’s prognosis when they have TB co-infection [15].
Chronic diarrhea (diarrhea with a duration of more than a month) has been documented as the second most common manifestation of infection in infants with HIV [10]. A parasitic infection, Giardia lamblia, is one of the causes of prolonged, chronic diarrhea in HIV-positive infants [13]. Patients present with watery diarrhea and epigastric pain for up to two weeks, but in some, the symptoms may last for months [13]. In infants with prolonged diarrhea, malabsorption and weight loss may result in chronic sequelae such as irritable bowel syndrome, chronic fatigue, failure to thrive, and even cognitive impairment [13].
Although rotavirus is not a cause of chronic diarrhea in infant with HIV, it has been identified as a common cause of acute diarrhea and gastroenteritis in infants [13]. In HIV-positive infants, the clinical presentation of rotavirus is more severe and includes fever and watery stools which may lead to dehydration, shock and death [13]. Rotavirus may also lead to respiratory symptoms in more than 50% of patients and neurological manifestations, including seizures, encephalitis and encephalopathy in 2-3% of patients [13].
Malnutrition also contributes to HIV and AIDS-related morbidity and mortality in infants [1, 16] and up to 40% of HIV-positive children are malnourished [16]. In Sub-Saharan Africa, the combined burden of HIV infection and malnutrition remains a concerning public health issue, as up to 90% of the children who are infected by HIV globally reside in Sub-Saharan Africa [16]. This malnutrition may present as underweight, stunting, wasting and micronutrient deficiencies [16].
When compared to non-HIV-infected children, the energy needs of children with HIV are increased. In asymptomatic infants, there is a 10% increased energy need, and this rises to 20 to 30% in symptomatic children and 50 to 100% in children with severe malnutrition [16]. Malnutrition can worsen the effects of HIV infection through an increased severity and frequency of infections [13, 16]. Recovery from opportunistic and other infections is also delayed by malnutrition [13]. On the other hand, malnutrition can be worsened by opportunistic and other infections that lead to reduced food consumption and cause malabsorption [13, 16]. The vicious interaction between malnutrition and HIV in infants can therefore be seen.
In the current study, different diagnoses, their frequencies among HIV-positive infants as well as an assessment of HIV infants on antiretroviral therapy constituted the main study objectives while aiming to describe the prevalent clinical assessments of HIV-positive infants in Odi district hospital in Pretoria,, South Africa from the 1st January 2010 to 31st December 2012.
3. METHODS
3.1. Study Design
This was a cross-sectional study based on a retrospective records review of all HIV-positive infants admitted at Odi District Hospital in Pretoria from the 1st January 2010 to 31st December 2012.
3.2. Setting
The study was carried out in the 227-bed Odi District Hospital in South Africa's Gauteng province. It is located in a peri-urban setting to the northwest of the capital city (Pretoria). There are numerous services provided, including a wellness center or HIV clinic, eye and dental clinics, a rehabilitation unit with social work, audiology, physiotherapy, dieticians, an outpatient department, an obstetrics unit, and others. According to the researcher's observations, this hospital sees a majority of patients from low socioeconomic backgrounds because of its placement in a township.
3.3. Study Population
From January 1, 2010, to December 31, 2012, every infant (under one year of age) admitted to the pediatric ward of the Odi district hospital in Gauteng province of South Africa constituted the study population. According to hospital records, there were 962 patients overall (including HIV-positive, HIV-negative, and untested individuals).
3.4. Sample Size
A total of 98 HIV-positive infants were admitted to the Odi District Hospital during the study period made up the study sample. With convenience sampling, this indicates that the study sample size (n= 98) was 10.2% of the study population (962).
3.5. Data Collection
The researcher trained a retired nurse as a research assistant (RA). Data gathering from the files of the HIV-positive infants hospitalized at the Odi District Hospital was the responsibility of the RA throughout a 6-week period. From the hospital's records section, medical records or patients' files were retrieved. Using the data collection sheet created for this study, information on demographics, clinical diagnoses, and particular antiretroviral regimens were gathered as the causes of death in case the infants died.
3.6. Data Analysis
As a data gathering sheet, a Microsoft Excel spreadsheet was created. Coding was performed on raw data to obtain categorical data before it was put into Statistical Analysis System (SASA) software release 9.2 for descriptive analysis. Tables and figures with frequencies and percentages were used to present the findings.
3.7. Ethical Considerations
Patients' confidentiality and anonymity were guaranteed throughout the study's duration and data processing. The CEO (Chief Executive Officer) of the Odi District Hospital granted permission for the study to be carried out in the facility, while the Medunsa Research and Ethics Committee (MREC), now known as the Sefako Makgatho Research Ethics Committee or SMUREC (MREC/M/314/2013), also granted research an Ethical approval.
4. RESULTS
The majority of infants (57; 58.2%) were in the age category 7-12 months, while males as a sex had a high participation (56; 57.1%), as displayed in Table 1.
On admission, as displayed in Fig. (1), HIV-positive infants admitted at Odi District Hospital during the study period were diagnosed with lower respiratory tract infection (LRTI) (44; 44.9%), malnutrition and failure to thrive (FTT) (25; 25.5%), gastro-enteritis (21, 21.4%), meningitis (2; 02.0%), febrile convulsions (2; 02.0%), and other conditions such as encephalopathy (1; 0.98%) and dehydration (1; 0.98%).
In Table 2 below, the majority of HIV-positive male infants had lower respiratory tract infections (25), malnutrition and failure to thrive (18), while the majority of female infants were exposed to lower respiratory tract infection (19) followed by gastro-enteritis (11), and meningitis, febrile convulsions, and dehydration (2).
| Demographic Data | Frequency (n) | Percentage (%) |
|---|---|---|
| AGE in Months | - | |
| 1 – 6 (4.00) | 41 | 41.8 |
| 7 – 12 (11.00) | 57 | 58.2 |
| TOTAL | 98 | 100 |
| Sex | - | |
| MALE | 56 | 57.1 |
| FEMALE | 42 | 42.9 |
| TOTAL | 98 | 100 |

| Prevalent Clinical Assessments | Male | Female | Total |
|---|---|---|---|
| LRTI | 25 (25.5%) | 19 (19.3%) | 44 (44.8%) |
| Malnutrition and Failure to thrive | 18 (18.4%) | 7 (7.1%) | 25 (25.5%) |
| Gastro-enteritis | 10 (10.2%) | 11 (11.2%) | 21 (21.4%) |
| Encephalopathy | 1 (10,0%) | 0 | 1 (10,0%) |
| Meningitis, Febrile convulsions, Dehydration | 1(10.0%) | 2 (2,0%) | 3 (3.0%) |
| Others | 2 (2.04%) | 2 (2.0%) | 4 (4.1%) |
Twelve of the twenty-five infants who were known to be HIV + upon admission (25.5%) were taking ART, but seventy-three (74.5%) infants were diagnosed during admission by the use of polymerase chain reaction (PCR). They were all using one regimen, which consisted of Lopinavir-Ritonavir (Kaletra), Abacavir, and Lamivudine.
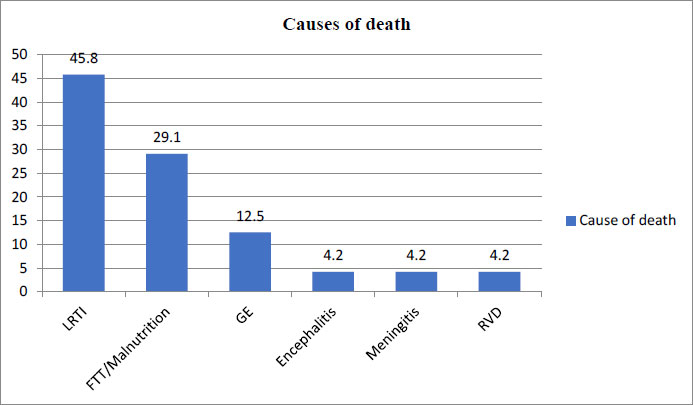
Regarding the causes of death, as seen in Fig. (2), twenty-four infants were demised during hospitalization (24.4%). Among them, 11 were admitted with LRTI, 7 with FTT/ malnutrition, 3 with GE, 1 with encephalitis, 1 with meningitis, and 1 was simply admitted as RVD, not on treatment. Among the deaths, 15 were males and 9 were females. Twelve were in the age category of 0-6 months, and 12 were in the category of 7-12 months.
5. DISCUSSION
Despite the country's new standards to reduce mother-to-child transmission, certain infants are taken to hospitals without a known HIV status and a time in alarming conditions. In the current study, only 25% of the hospitalized infants had been diagnosed with HIV prior to admission. This contradicts the 90/90/90 strategy, which was set to be implemented by 2020. The findings of this study showed that most infants admitted to the Odi District Hospital were male (56% of 98 participants) and aged between 7 and 12 months, in contrast to a retrospective chart review conducted in Ethiopia in 2018 to determine the prevalence of HIV-positive infants born to HIV-positive mothers receiving anti-retroviral therapy, which found that out of more than 230 HIV-positive mothers, 6% of infants were HIV-positive and like the South African study 57% were male. It was advised that decisive action has to be taken by stakeholders, medical professionals, and the general public in order to eliminate baby HIV infection in Ethiopia [17].
Regarding the distribution of sexes, a study conducted in Blantyre, Malawi, which looked at gender-specific risks of mother-to-child transmission (MTCT) at birth and at 6 to 8 weeks among children born to African women with HIV, revealed that the rate of HIV transmission at birth was around 10%. However, girls were HIV-positive at birth at a much higher rate than boys. Nearly 9% of newborns who were HIV-negative at birth had HIV by the time they were 6 to 8 weeks old. Of these infants, more females than boys (10.0%) developed HIV [18], which is inconsistent with the demographic distribution displayed by the current study, where boys are compared to many girls.
The current study has presented lower respiratory infection as the principle l or main clinical assessment among HIV-positive infants admitted at Odi District Hospital; this outcome has been supported by several studies, such as a study done in India highlighting the fact that opportunistic infections continue to be a serious health risk for children with HIV/AIDS. They manifest differently in poor nations than they do in industrialized countries. Along with other bacterial illnesses, tuberculosis is still a serious threat. Infections with fungi and parasites are additional common health risks [19]. The Odi District Hospital’s finding is also supported by the guideline for prevention and treatment of opportunistic infections in children with and exposed to HIV, which stated that serious bacterial infections were the most frequently diagnosed opportunistic infections in children with HIV before combination antiretroviral therapy was available, with pneumonia being the most common. However, since the introduction of ART, bacterial infections in children with HIV have significantly decreased. As a result, the rate of pneumonia has dropped, but bacteraemia is still significantly more common in children in the United States than invasive pneumococcal illness [20].
According to the Odi findings, more than 50% of the deceased had lower respiratory tract infections (LRTI), followed by malnutrition and failure to thrive. According to the findings of an Indian study, LRTI was the leading cause of death among HIV-positive children on ART. Pneumonia, included in LRTI, caused by unknown microorganisms accounted for 17% of deaths, followed by tuberculosis (16%), sepsis (8.0%), and AIDS (6.7%); 12% of deaths had unknown underlying causes [21].
6. LIMITATIONS
Due to the small sample size, the current findings cannot be applied to the full city of Pretoria. Therefore, investigations including more health facilities and larger samples are advised in order to develop a disease profile for the clinical assessment of HIV-positive infants in the city.
Although the data is almost 13 years old, the literature review is current, confirms the data, and therefore supports the study as still being relevant.
As this is a statistical study of age, sex, morbidity and mortality of infants with HIV / AIDS according to the aim of the study, there is no conclusion, test result, or information on viral load.
CONCLUSION
The current study has presented lower respiratory tract infection as the most prevalent clinical assessment and cause of morbidity among HIV infants admitted to Odi District Hospital in Pretoria, South Africa. More studies with substantial sample sizes are advised to give a comprehensive picture of the problem.
AUTHORS’ CONTRIBUTIONS
This article is taken from a master's dissertation in family medicine. KN came up with the idea, gathered information, and wrote the dissertation. KEH oversaw every aspect of the dissertation and engaged in the article writing process. GAO co-supervised the dissertation throughout all phases. CS and TB wrote the article.
LIST OF ABBREVIATIONS
| ARV | = antiretroviral |
| WHO | = World Health Organization |
| PMTCT | = Prevention of Mother to Child Transmission |
| RS | = Respiratory syncytial |
| TB | = Tuberculosis |
| RA | = Research Assistant |
| SASA | = Statistical Analysis System |
| LRTI | = Lower Respiratory Tract Infection |
| FTT | = Failure to Thrive |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Institutional Ethical Committee of the Medunsa Research and Ethics Committee (MREC), now known as the Sefako Makgatho Research Ethics Committee or SMUREC (MREC/M/314/2013).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this current study is not openly available. Data is available from the corresponding author [K.N]. upon reasonable request.
FUNDING
No specific grant from any funding agency was received for this present research.
CONFLICT OF INTEREST
The authors declare that no financial or personal relationship has inappropriately influenced the writing of this article.
ACKNOWLEDGEMENTS
We gratefully recognize the late Professor G.A. Ogunbanjo's important intellectual contribution to the completion of the dissertation that resulted in the current work.
DISCLAIMER
The views and opinions expressed in the manuscript are those of the authors and do not necessarily reflect the official policy or position of any affiliate institution.


