All published articles of this journal are available on ScienceDirect.
Antenatal Care Services Uptake and Associated Factors in Somaliland: Further Analysis of the 2020 Somaliland Demographic Health Survey
Abstract
Purpose
Antenatal care (ANC) is vital to maintain the health of pregnant women and their unborn babies. It was linked to a positive pregnancy experience. However, ANC uptake remained low in Somaliland, and no study has been conducted to assess possible predictors. Hence, the current study aimed to determine the level of ANC utilization and to identify its associated factors in Somaliland.
Materials and Methods
Somaliland Demographic Health Survey (SLDHS) Data 2020 were used. A weighted sample of 3,192 women aged 15-49 years participated in the study. The survey used a two-stage cluster design for sample selection. Descriptive statistics in the form of frequency and percentage and multilevel multinomial logistic regression analysis were carried out to determine associated factors and statistical significance was declared by p< 0.05.
Results
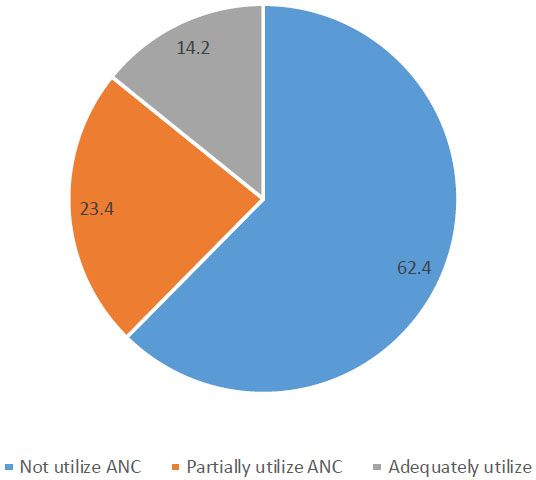
The findings showed that 62.4% (95% CI: 60.7-64.1) of the women did not utilize ANC services, while 23.4% (95% CI: 21.9, 24.9) partially utilized and 14.2% (95% CI: 13.0, 15.4) adequately utilized ANC services. The odds of adequately utilizing ANC service decreased by a factor of 0.88 for women aged 35 and above compared to 15 - 24 year old women (AOR= 0.88, 95% CI: 0.61, 1.26). Women with higher educational levels had significantly higher odds (AOR=4.31, 95% CI: 1.54, 12.02) of adequately utilizing ANC compared to those with no formal education. The employment status, marital status, household wealth index, residence and region were also found to be associated with the utilization of Antenatal care.
Conclusion
The study showed low adequate utilization of ANC services in Somaliland. The variables, including age, education, wealth index, marital status, employment status, residence and region, were significantly associated with ANC utilization. Governmental and non-governmental organizations should enact a strategy with targeted intervention focusing on women from nomadic and rural communities, those from poor households, and low educational levels.
1. INTRODUCTION
Globally, 94% of all preventable pregnancy- and childbirth-related deaths in 2017 occurred in places with limited resources, with an average of 810 women dying per day. High maternal mortality indices were significantly correlated with lack of access to antenatal care [1]. Somaliland is a sub-Saharan African country where the Maternal Mortality Ratio is 396 maternal deaths per 100,000 live births [2].
Antenatal care is a kind of maternal health service with the potential to reduce maternal mortality [3-5]. Improvements in the provision of quality health care during pregnancy and childbirth and increasing the number of ANC visits (≥8) could prevent many of these deaths [6]. The term “antenatal care” (ANC) refers to the care given to pregnant women by trained medical personnel to ensure the mother's and baby's health during pregnancy [7]. This includes risk identification, disease prevention and management, health education, and promotion for pregnant women and adolescent girls [8]. The new ANC model from the World Health Organization (WHO) places an emphasis on more frequent visits, more comprehensive care, and treating pregnancy as a positive experience for women [9].
Prioritizing person-centered healthcare, the well-being of women and families, and favorable perinatal and maternal outcomes, the World Health Organization's 2016 recommendations on antenatal care (ANC) for a positive pregnancy experience emphasize these factors [10]. Recent WHO guidelines have increased the number of ANC contact from four to eight [11].
Evidence shows that 86% of pregnant women worldwide access skilled ANC at least once, and 65% have at least four visits. In sub-Saharan Africa, only 52% of pregnant mothers made at least four visits [12]. According to the 2020 Somaliland Demographic & Health Survey (SLDHS), only 20% of pregnant women made four or more visits, and approximately 52% of the mothers did not receive ANC services [2]. Reports from different countries have shown that sociodemographic characteristics, including level of education, residence, marital status, age, religion, and ethnicity, have an impact on ANC utilization [13]. Lower antenatal care services utilization has been associated with unplanned pregnancies, problems from prior pregnancies, lack of autonomy, lack of support from the husband, greater distance to the medical facility, lack of health insurance, and high service fees [14-16]. Household financial status, setting, media exposure, the number of children currently alive, knowledge of danger signs, prior obstetric history, and level of care are among other factors that affect the utilization of antenatal care [17-24].
Most experts agree that the foundation of maternal and perinatal care is adequate ANC [25]. The healthcare systems in many developing countries, particularly in Africa, still face challenges in providing adequate ANC due to a shortage of trained personnel [26]. Decades of poverty, underinvestment, violence, insecurity, evictions, and natural calamities are significantly challenging factors in addressing the demands of reproductive health through a comprehensive, functional health system in the country [27]. In addition, few studies have assessed ANC uptake and factors affecting its uptake in Somaliland. This might be another challenge when focusing on areas for sectors that work on the subject. Previous studies dichotomized the outcome variable of antenatal utilization as either utilized or not. This study aims to fill these gaps by applying a multinomial logistic regression model. Considering this knowledge gap, the current study aimed to assess antenatal care (ANC) utilization and its associated factors in Somaliland.
2. MATERIALS AND METHODS
2.1. Study Setting
This study was conducted in Somaliland, a self-declared independent country in the Horn of Africa. The estimated population of Somaliland is 4.5 million. Somaliland, bordered by Djibouti, Ethiopia, and Somalia, spans 176,119.2 km2 with 850 km coastline. Its climate combines wet and dry conditions, with hilly northern regions and altitudes ranging between 1,800 and 2,100 m [2]. The Somalilands are inhabited by ethnic Somalis and Muslims. Somaliland’s capital, Hargeisa, is home to more than one-third of the nation's population. There are six regions in Somaliland: Awdal, Marodijeh, Sahil, Togdheer, Sool, and Sanaag, with 22 districts across the country [28, 29]. Somaliland's economy has expanded, with livestock being its main source of exports; however, it remains a poor country with fewer chances for foreign investment and trade [2]. Somaliland’s GDP and GDP per capita are estimated to be 2.5 billion USD and 566 USD, respectively, in 2018, with remittances and livestock exports shipped to the Gulf States (GoSL, 2018). Somaliland's lack of international recognition limits its ability to enter bilateral agreements and attract direct investment from donors.
2.2. Study Design, Data Source and Study Period
This study used data from the 2020 Somaliland Demographic Health Survey (SLDHS) 2020. The survey was cross-sectional and appropriate for investigating the level of ANC uptake and its associated factors. The survey began in August 2018 and was completed in December 2019. The country's first nationally representative demographic health survey, the 2020 SLDHS, reported on it with the aim of enhancing data systems and evidence-based planning [2].
2.3. Sample Size and Sampling
This study used a weighted sample of 3,192 from the 2020 Somaliland Demographic Health Survey (SLDHS) dataset. The participants were women in the reproductive age group (15-49 years old) who had a pregnancy in the five years preceding the survey. The DHS survey used a Geographic Information System (GIS) program to spatially count the number of residential buildings and create enumeration areas (EAs) for the survey. Sample ground verification was performed to adjust the sampling frame as needed.
Two-stage sampling technique was used during the DHS survey. A minimum of 50 and a maximum of 149 dwellings were present in each of the formed EAs. 1,869 EAs in urban areas and 1,054 in rural regions, for a total of 2,923 EAs, also known as primary sampling units (PSUs), were digitalized. The final sampling frame consisted of 2,086 PSUs (1,869 in urban regions and 937 in rural areas). However, owing to security concerns, some sampled EAs were not visited. In the first stage, the probability proportional to the size (PPS) sampling of digitized residential structures was used to select 35 EAs from each stratum of each design domain. The six regions that serve as first-level administrative divisions of the country correspond to the design domain. To determine the total number of households, all households are listed in each of the 35 selected EAs [2].
2.4. Variables of the Study
2.4.1. Outcome Variable
The antenatal care use outcome variable in this study was quantified as not utilized, partially utilized, and adequately utilized. Women who did not visit antenatal clinics while they were pregnant were under the “not utilized” group. Women who attended antenatal clinics less than four times fell into the “partially utilized” category, while those who did so at least four or more times fell into the “adequately utilized” category [30]. This was categorized into three groups and levels as follows:
X = {0 if a woman visits ANC (0 visits)
{1 if a woman attended an ANC (one to three visits)
{2 if a woman attended an ANC (four or more visits)
2.4.2. Explanatory Variables
Various sociodemographic, biological, and environmental factors, including age, education level, religion, wealth index, family size, pregnancy compli- cations, and professional health counseling, have been identified as predictor variables in previously published research articles [31, 32]. By reviewing previous studies, the following independent variables were considered: age, education, household wealth, residence, employment, education, media exposure, parity, health-care decisions, marital status, and region. Women’s reproductive history, including marital status, age at first marriage, current pregnancy, contraceptive use, desire for more children, and total number of children born, were also included as independent variables.
2.4.3. Data Collection Methods
In order to gather information [2] from 30 chosen families in each of the 10 sampled EAs in each region stratum for the 2020 SLDHS, trained interviewers and supervisors were used in urban and rural areas of the country. The chosen households came from a list of all the households in EA. The primary survey began in August 2018 and ran until December 2019. Nineteen teams of one supervisor, three enumerators, and one driver each carried out the fieldwork. The data were gathered using an Android platform created in CSPro. The listing team, which was skilled at reading maps and could recognize the EA boundaries as well as the chosen household, provided assistance to the data collectors.
In nomadic areas [2], there were a total of four teams, each with four members, collecting the SLDHS data. To get a current and comprehensive list of households, nomadic households were listed in each TNS one day prior to the day of enumeration. In each enumeration area, thirty households were chosen.
2.4.4. Data Quality Assurance
During the DHS data collection, 92 employees, including interviewers and supervisors, received training. At the end of each training session, a pretest was conducted using manual questionnaires and computer-assisted personal interviewing (CAPI) to ensure that all trainees had acquired a minimum level of knowledge and skills. The GPS tracking of field operations aids georeferencing to allow geolocated data collection. The data collection was closely supervised. In Kigali, Rwanda, the technical team from the UNFPA national office taught four master trainers for more than a month in October 2017. All of these master trainers were specialists in Somaliland who also contributed to the creation and evaluation of data collection systems. Consequently, the ToTs in Borama, Hargeisa, and Burao trained 92 employees, who were supervisors and interviewers. To make sure that all trainees had attained a minimal level of knowledge and abilities, a pretest using manual questionnaires and the CAPI was carried out at the conclusion of each training session. Based on their performance on both in-class and field pretests, supervisors were selected [2].
2.4.5. Data Management and Analysis
A weighted sample was considered in the analysis to ensure the representativeness of the survey data. Data were exported to STATA software version 14 for analysis. Data cleaning was performed, missing variables were checked, and a multicollinearity test was performed using a variance inflation factor, which was 4, which indicated no multicollinearity. Descriptive statistics such as frequencies, percentages, means, and standard deviation were computed. Moreover, due to significant variation observed as a result of clustering, the association between dependent and independent variables was analyzed using multilevel multinomial logistic regression. Four models, including the null model (containing only the outcome variable), model I (containing only individual-level variables), model II (containing only community-level variables), and model III (containing both individual and community-level variables) were constructed. Based on the model fitness test, the best-fitting model was model III. Hence, this model was selected for final interpretation. The analysis used non-utilization as a reference category and assessed the factors associated with the partial and adequate utilization of ANC services. The variables with adjusted odds ratios with 95% confidence intervals and a p-value of <0.05 were used to declare significance.
3. RESULTS
3.1. Sociodemographic Characteristics of the Participants
Data from 3,192 women in the reproductive age group were included in this study. Table 1 presents the sociodemographic characteristics of reproductive-age women included in the survey. The mean (SD) age of women was 29.74 (±6.86), with a range of 15 to 49 years. The majority of respondents married were 2,971 (93.1%), and the respondents who had no formal education were 2,636 (82.6%). Approximately one-third of the respondents that lived in rural areas were 1070 (33.5%), while the remaining were urban residents,902 (28.2%), and nomadic residents, 1220 (38.2%). Most respondents were unemployed 3002 (94%), and a significant proportion were in the lowest-wealth quintile 1167 (36.6%).
The findings indicated that women aged 15–24 years had the highest percentage of non-utilization, 474 (63.4%). The Sool region had the highest percentage of non-utilization, 538 (76.0%), followed by Sanaag 544 (72.8%), Togdheer 305 (56.7%), Marodijeh 212 (54.8%), Sahil 201 (49.4%), and Awdal 192 (47.4%) (Table 1).
3.2. Reproductive History of the Participants
Regarding the reproductive history of women, more than half, 1,742 (54.6%), married before the age of 20, and only a few, 85 (2.7%) of the respondents married at the age of 31 years and above. Among the total respondents, 533 (17.0%) were currently pregnant, while 2,608 (83.0%) were not pregnant at the time of the survey. Among the women who were currently pregnant, 448 (84.1%) wanted pregnancy and 85 (15.9%) had unwanted pregnancies. In terms of the desire for more children, 1,802 (68.4%) respondents wanted to have more children within two years, while 348 (13.2%) wanted no more children (Table 2).
| Variables | Category | Frequency (%) | Antenatal Care Utilization | P-value | ||
|---|---|---|---|---|---|---|
| Not Utilized n (%) | Partially Utilized n (%) | Adequately Utilized n (%) | ||||
| Age | 15–24 | 748 (100) | 474 (63.4) | 181 (24.2) | 93 (12.4) | 0.143 |
| 25–34 | 1519 (100) | 923 (60.8) | 357 (23.5) | 239 (15.7) | ||
| 35+ | 925 (100) | 595 (64.3) | 210 (22.7) | 120 (13.0) | ||
| Region | Awdal | 405 (100) | 192 (47.4) | 107 (26.4) | 106 (26.2) | < 0.001 |
| Marodijeh | 387 (100) | 212 (54.8) | 104 (26.9) | 71 (18.3) | ||
| Sahil | 407 (100) | 201 (49.4) | 126 (31.0) | 80 (19.7) | ||
| Togdher | 538 (100) | 305 (56.7) | 142 (26.4) | 91 (16.9) | ||
| Sool | 708 (100) | 538 (76.0) | 124 (17.5) | 46 (6.5) | ||
| Sanaag | 747 (100) | 544 (72.8) | 145 (19.4) | 58 (7.8) | ||
| Residence | Urban | 902 (100) | 315 (34.9) | 344 (38.1) | 243 (26.9) | < 0.001 |
| Rural | 1070(100) | 617 (57.7) | 259 (24.2) | 194 (18.1) | ||
| Nomadic | 1220(100) | 1060 (86.9) | 145 (11.9) | 15 (1.2) | ||
| Employment | Employed | 188(100) | 86 (45.7) | 54 (28.7) | 48 (25.5) | < 0.001 |
| Unemployed | 3002(100) | 1904 (63.4) | 694 (23.1) | 404 (13.5) | ||
|
Education |
No Education | 2636 (100) | 1804 (68.4) | 534 (20.3) | 298 (11.3) | < 0.001 |
| Primary | 430 (100) | 160 (37.2) | 162 (37.7) | 108 (25.1) | ||
| Secondary | 83 (100) | 22 (26.5) | 37 (44.6) | 24 (28.9) | ||
| Higher | 43 (100) | 6 (14.0) | 15 (34.9) | 22 (51.2) | ||
| Wealth | Lowest | 1167 (100) | 956 (81.9) | 173 (14.8) | 38 (3.3) | < 0.001 |
| Second | 525 (100) | 385 (73.5) | 92 (17.5) | 48 (9.1) | ||
| Middle | 359 (100) | 221 (61.6) | 79 (22.0) | 59 (16.4) | ||
| Fourth | 519 (100) | 239 (46.1) | 168 (32.4) | 112 (21.6) | ||
| Highest | 622 (100) | 191 (30.7) | 236 (37.9) | 195 (31.4) | ||
| Marital status | Married | 2971 (100) | 1850 (62.3) | 703 (23.7) | 418 (14.1) | < 0.001 |
| Divorced | 149 (100) | 92 (61.7) | 34 (22.8) | 23 (15.4) | ||
| Widowed | 72 (100) | 50 (69.4) | 11 (15.3) | 11 (15.3) | ||
| Listen to radio | At least once a week | 110 (100) | 47 (42.7) | 41 (37.3) | 22 (20.0) | < 0.001 |
| Less than once a week | 38 (100) | 23 (60.5) | 9 (23.7) | 6 (15.8) | ||
| Not at all | 3044 (100) | 1922 (63.1) | 698 (22.9) | 424 (13.9) | ||
| Health care decision | Respondent | 778 (100) | 455 (58.5) | 185 (23.8) | 138 (17.7) | < 0.001 |
| Husband | 1185 (100) | 810 (68.4) | 260 (21.9) | 115 (9.7) | ||
| Jointly | 1172 (100) | 699 (59.6) | 283 (24.1) | 190 (16.2) | ||
| In law | 3 (100) | 1 (33.3) | 2 (66.7) | 0 (0.0) | ||
| Someone else | 9 (100) | 5 (55.6) | 2 (22.2) | 2 (22.2) | ||
| Other | 8 (0.3) | 4 (50.0) | 4 (50.0) | 0 (0.0) | ||
| Variables | Category | Frequency (N) | Percentage (%) |
|---|---|---|---|
| Age at first marriage (years) | < 20 | 1742 | 54.6 |
| 20-24 | 829 | 26.0 | |
| 25-30 | 536 | 16.8 | |
| 31 and above | 85 | 2.7 | |
| Current pregnancy intention (533) | Yes | 448 | 84.1 |
| No | 85 | 15.9 | |
| Contraceptive use (2633) | Yes | 221 | 8.4 |
| No | 2412 | 91.6 | |
| Desire for more children (2633) | Wants within 2 years | 1802 | 68.4 |
| Wants after 2 years | 99 | 3.8 | |
| Undecided | 339 | 12.9 | |
| Wants no more | 348 | 13.2 | |
| Declared infecund | 45 | 1.7 | |
| Currently pregnant (3141) | Yes | 533 | 17.0 |
| No | 2608 | 83.0 |
3.3. Antenatal Care Utilization among Study Participants
Among the participants who gave birth in the five years preceding the survey, 62.4% (95% CI: 60.7, 64.1) did not utilize ANC services, 23.4% (95% CI: 21.9, 24.9) partially utilized ANC services, and 14.2% (95% CI: 13.0, 15.4) adequately utilized ANC services (Fig. 1).
3.4. Factors Associated with Antenatal Care Utilization
Multilevel multinomial logistic regression was used for analysis, and the result was presented in Table 3.
3.5. Partial Antenatal Care Utilization
The results showed that educational level, wealth quantiles, marital status, residence and region are found to be associated with partial utilization of antenatal care. The participants who attained secondary level education (AOR=2.11, 95% CI:1.18,3.79) and primary level education (AOR=2.04, 95% CI: 1.55, 2.68) are more likely to partially utilize ANC compared to women with no formal education. The odds of utilizing ANC partially among women from the richest (AOR= 1.85, 95% CI: 1.27, 2.71) households were nearly two times the odds in the poorest household.
| Variables | Null Model | Model I | Model II | Model II | |||
|---|---|---|---|---|---|---|---|
| Partially Utilized (AOR 95% CI) | Adequately Utilized (AOR 95% CI) | Partially Utilized (AOR 95% CI) | Adequately Utilized (AOR 95% CI) | Partially Utilized (AOR 95% CI) | Adequately Utilized (RR 95% CI) | ||
| Age in years | - | - | - | - | - | - | - |
| 15-24 | - | 1(ref) | 1(ref) | - | - | 1(ref) | 1(ref) |
| 25-34 | - | 1.02(0.81, 1.28) | 1.27(0.95,1.71) | - | - | 0.89(0.70,1.13) | 1.05(0.77,1.44) |
| ≥ 35 | - | 1.08(0.84,1.40) | 1.24(0.88,1.73) | - | - | 0.89(0.68,1.16) | 0.88(0.61,1.26) |
| Education | - | - | - | - | - | - | - |
| No education | - | 1(ref) | 1(ref) | - | - | 1(ref) | 1(ref) |
| Primary | - | 2.16(1.66,2.81) | 2.05(1.52,2.77) | - | - | 2.04(1.55,2.68) | 1.89(1.38,2.58) |
| Secondary | - | 2.49(1.41,4.41) | 2.24(1.19,4.20) | - | - | 2.11(1.18,3.79) | 1.84(0.95,3.56) |
| Higher | - | 3.11(1.16,8.27) | 6.03(2.34,15.53) | - | - | 2.61(0.93,7.29) | 4.31(1.54,12.02) |
| Employment | - | - | - | - | - | - | - |
| Employed | - | 1 (ref) | 1 (ref) | - | - | 1(ref) | 1(ref) |
| Unemployed | - | 0.58 (0.41,0.82) | 0.38(0.26,0.55) | - | - | 0.82(0.56,1.22) | 0.64(0.42,0.98) |
| HH wealth quintiles | - | - | - | - | - | - | - |
| Poorest | - | 1(ref) | 1(ref) | - | - | 1(ref) | 1(ref) |
| Poorer | - | 1.23(0.93,1.64) | 2.98(1.91,4.65) | - | - | 0.92(0.66,1.27) | 1.34(0.80,2.23) |
| Middle | - | 1.75(1.28,2.38) | 5.93(3.82,9.21) | - | - | 0.76(0.51,1.14) | 1.51(0.89,2.56) |
| Richer | - | 3.36(2.58,4.37) | 10.37(6.95,15.48) | - | - | 1.42(0.97,2.07) | 2.95(1.77,4.93) |
| Richest | - | 5.15(3.92) | 19.08(12.81,28.41) | - | - | 1.85(1.27,2.71) | 4.18(2.52,6.93) |
| Marital status | - | - | - | - | - | - | - |
| Married | - | 1(ref) | 1(ref) | - | - | 1(ref) | 1(ref) |
| Divorced | - | 0.69(0.45.1.06) | 0.71(0.42,1.17) | - | - | 0.55(0.35,0.85) | 0.53(0.31,0.91) |
| Widowed | - | 0.58(0.29,1.15) | 0.92(0.45,1.88) | - | - | 0.62(0.31,1.25) | 1.02(0.48,2.19) |
| Listen radio | - | - | - | - | - | - | - |
| Once a week | - | 1(ref) | 1(ref) | - | - | 1(ref) | 1(ref) |
| <once a week | - | 0.33(0.12,0.84) | 0.40(0.13,1.25) | - | - | 0.44(0.16,1.19) | 0.61(0.18,1.97) |
| Not at all | - | 0.58(0.36,0.92) | 0.79(0.44,1.41) | - | - | 0.75(0.46,1.21) | 1.07(0.59,193) |
| Residence | - | - | - | - | - | - | - |
| Urban | - | - | - | 1(ref) | 1(ref) | 1(ref) | 1(ref) |
| Rural | - | - | - | 0.37(0.29,0.48) | 0.38(0.30,0.49) | 0.46(0.36,0.59) | 0.61 (0.46,0.81) |
| Nomadic | - | - | - | 0.12(0.09,0.15) | 0.02(0.01,0.03) | 0.19(0.13,0.28) | 0.05(0.03,0.11) |
| Region | - | - | - | - | - | - | - |
| Awdal | - | - | - | 1(ref) | 1(ref) | 1(ref) | 1(ref) |
| Marodijeh | - | - | - | 0.80(0.56,1.15) | 0.52(0.34,0.77) | 0.73(0.51,1.06) | 0.45(0.29,0.69) |
| Sahil | - | - | - | 1.01(0.71,1.43) | 0.60(0.40,0.89) | 0.92(0.64,1.32) | 0.51(0.33,0.77) |
| Togdheer | - | - | - | 0.77(0.55,1.08) | 0.49(0.33,0.71) | 0.77(0.55,1.09) | 0.50(0.34,0.74) |
| Sool | - | - | - | 0.41(0.30,0.57) | 0.15(0.10,0.23) | 0.41(0.29,0.58) | 0.15(0.09,0.23) |
| Sanaag | - | - | - | 0.41(0.29,0.56) | 0.15(0.11,0.23) | 0.36(0.25,0.50) | 0.12(0.08,0.18) |
Table 4.
| Parameters | Null Model | Model I | Model II | Model III |
|---|---|---|---|---|
| Inter-class correlation (ICC) | 0.282 | 0.124 | 0.012 | 0.012 |
| Log-likelihood ratio (LLR) | -3246.3 | -3239.1 | -3180.7 | -3180.7 |
| Akaike’s information criterion (AIC) | 6498.7 | 6488.3 | 6373.4 | 6363.4 |
| Bayesian information criterion (BIC) | 6516.9 | 6518.7 | 6409.8 | 6369.5 |
The odds of partially utilizing ANC decreased by a factor of 0.46 and 0.19 for women from rural and nomadic communities compared to those from urban residents. The region of residence is significantly associated with the likelihood of partial utilization of ANC compared to non-utilization. Respondents from the Sanaag region were less likely to partially utilize ANC than those from Awdal (AOR: 0.36, 95% CI: 0.25-0.50). Moreover, the odds of partial utilization ANC decreased by a factor of 0.41, 0.77, 0.92 and 0.73 for women from the Sool, Togdher, Sahil and Marodijeh, respectively (Table 3).
3.6. Adequate Antenatal Care Utilization
The variables, including age, educational status, employment status, household wealth quintiles, marital status, residence and region, were found to be associated with adequate antenatal care utilization.
The result showed that women in the advanced age (≥ 35 years) category are less likely to adequately utilize ANC compared to their counterparts (AOR: 0.88, 95% CI: 0.61, 1.26). The higher educational level is also significantly associated with the adequate utilization of antenatal care. Women with an educational level of college and above (AOR = 4.31, 95% CI: 1.54-12.02) and primary education level (AOR = 1.89, 95% CI: 1.38 - 2.58) had a higher likelihood of adequately utilizing ANC compared to those with no formal education.
The results suggest that employment status is associated with antenatal care utilization. The odds of adequately utilizing antenatal care decreased by a factor of 0.64 among unemployed women compared to employed women (AOR = 0.64, 95% CI: 0.42,0.98). The household wealth index was also significantly associated with antenatal care utilization. Compared to the poorest households, those from the richest (AOR = 4.18, 95% CI: 2.52, 6.93) and richer (AOR= 2.95, 95% CI:1.77, 4.93) households were more likely to adequately utilize antenatal care. Marital status is also among the factors significantly associated with ANC utilization. The odds of adequately utilizing ANC among divorced women decreased by the factors of 0.53 compared to married (AOR=0.53, 95% CI:0.31, 0.91).
Regarding community-level factors, both residence and region are associated with uptake of ANC utilization. The odds of adequately utilizing ANC decreased by a factor of 0.61 and 0.05 for women from rural and nomadic communities, respectively, compared to those from the urban residence. The odds of adequately utilizing ANC were decreased by the factor of 0.12 and 0.15 among participants from Sanaag and Sool regions, respectively, compared to Awdal. Similarly, women from Marodijeh, Sahil, and Togdher regions had a significantly lower likelihood of adequate antenatal care utilization (AOR = 0.45, 95% CI:0.29-0.69; AOR = 0.51, 95% CI: 0.33-0.77; and AOR = 0.50, 95% CI:0.34,0.74), respectively (Table 3).
3.7. Random Effect Analysis
Random effect analysis of the null model revealed ICC was equal to 0.282, which indicate that 28.2% of the variability in the ANC utilization was attributed to the difference of cluster. Regarding the model fitness test, model III has insignificant intra-cluster correlation (ICC), lower Akaike’s information criterion (AIC) and Bayesian information criterion (BIC) were selected for final interpretation (Table 4).
4. DISCUSSION
This study revealed the level of ANC utilization and its associated factors. The results showed that 62.4% of women did not utilize ANC services, 23.4% received partial utilization, and 14.2% received adequate utilization. The current report shows a high proportion of non-utilization of antenatal care services in Somaliland. This rate is higher than a report from the study conducted in 31 sub-Saharan African countries that showed non- utilization of ANC in Chad (41.8%), Ethiopia (34.8%) and Nigeria (26.1%). A similar study showed proportions of adequate utilization of antenatal care in Ghana (86%), Gambia (78.1%), and South Africa (78.1%) [30], which is higher than reported in the current study.
The observed difference in the report might be attributed to differences in the sociodemographic characteristics of the study participants, particularly the economic status, the limited access to maternal health services and inadequately trained health personnel in Somaliland [33-36].
Women aged 35 and above had a lesser likelihood of adequate utilization of ANC services. This finding is consistent with studies conducted in Zambia [37] and Nigeria [38]. The possible explanation could be lower education status, lack of awareness of ANC and poor health-seeking behavior of women with advanced age [39]. Regarding marital status, divorced women are less likely to utilize ANC services. This is in line with other studies conducted in Ghana [40] and Botswana [41]. Many factors associated with divorce, including lack of social support, economic status and psychological factors, could affect health-seeking behavior of pregnant women. This possibly reduced the uptake of ANC services among divorced women.
The current study showed significant differences in the utilization of ANC services according to educational level. The higher educational level favors better utilization of ANC services. This finding is consistent with reports from other researches that showed educated women have higher odds of utilizing antenatal care [42-44]. It may be due to the fact that mothers with greater levels of education have better access to information, understanding of it and hence more awareness of the importance of ANC than their counterparts [45]. Additionally, education is more likely to increase their autonomy, self-assurance, and capacity to make independent health-related decisions [46-49].
Place of residence was also found to be a factor influencing the utilization of ANC. Being a resident of a rural and nomadic community negatively affects ANC uptake compared to urban residents. This is consistent with the report from other studies conducted in Ethiopia [50-52], Nigeria [53], Nepal [54, 55] and Malaysia [56]. The reason for less utilization of ANC service among women in nomadic communities might be due to their seasonal movement and lack of permanent residence, which disfavors access to fixed health services, including antenatal care [57, 58]. Low socio-economic status, lack of health service, which is not friendly to the nomadic lifestyle [59] and inadequate community-level medical facilities [57] might also affect the utilization of ANC services.
Regarding region, the study found that women from Marodijeh, Sahil, Togdheer and Awdal were more likely to use ANC services than women from Sool and Sanaag. This finding is consistent with studies that have reported regional disparities in ANC utilization [60, 61]. The low uptake of ANC in Sool and Sanaag might be due to the political crisis in these two regions. In addition, clannism and political conflicts causing a lack of peace and political unrest in the Sanaag region could result in less uptake of ANC in the area. For health services providers, security issues in the Sanaag region become an obstacle to serving the community [62].
The study found that unemployment is associated with poor utilization of ANC services. This finding is consistent with previous studies that reported a significant association between employment status and ANC utilization in Ethiopia [63], South Africa [64], and sub-Saharan Africa [14]. The possible explanation for this can be that employment is closely tied to income and education status. So unemployed women have less exposure to and access to ANC information and inadequate financial capacity for ANC follow-up [65-67].
The study also found that the higher level of household wealth quantiles favors better utilization of ANC services. Similar findings were reported from the studies conducted in Ethiopia [68], 31 Sub-Saharan African countries [69, 70] and Nepal [54]. This could be due to the fact that pregnant women in poor households cannot afford ANC services [71]. There is a direct link between poverty and decreased use of ANC services [71] [72].
4.1. Strengths and Limitations of the Study
This study used nationally representative data from the Somaliland Demographic and Health Survey, the first nationwide survey. The analysis included a large sample size, and it is the first study of its kind being performed in Somaliland.
However, it has some limitations, including social desirability and recall bias, owing to the self-report nature of the survey. Furthermore, some important variables were excluded due to incomplete data.
CONCLUSION AND RECOMMENDATIONS
The ANC utilization in Somaliland is low compared to the international target. The results of the study revealed that more than half of the women (62.4%) did not utilize ANC services, whereas the rest either partially (23.4%) or adequately (14.2%) utilized ANC services. Variables including maternal age, educational status, marital status, household wealth index, employment, residence and region were associated with ANC utilization.
Based on the results of the current study, promoting the education of women, particularly among nomadic communities, those with a poor wealth index, and unemployed women, will help to increase the utilization of ANC services. Hence, governmental and nongovernmental organizations working to promote ANC utilization should focus on creating strategic plans that focus on disadvantaged groups of women like divorced women, poor economic status and those in regions where it is difficult to access ANC services.
AUTHORS' CONTRIBUTION
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
LIST OF ABBREVIATIONS
| ANC | = Antenatal Care |
| SLDHS | = Somaliland Demographic Health Survey |
| PSUs | = Primary Sampling Units |
| PPS | = Probability proportional to the size |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Institutional Review Board of the Ministry of Health in the Republic of Somaliland (Ref: MOHD/DG:2/631/2023) and the Joint Ethics Review Committee of the University of Ibadan and the University College Hospital, Ibadan, Nigeria (UI/EC/22/0459).
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
The data were fully anonymized, and confidentiality was maintained. Written informed consent was obtained from the DHS survey.
AVAILABILITY OF DATA AND MATERIALS
The Manuscript was prepared from DHS data that is owned by the ministry of Health in Somaliland. It is not permitted to deposit whole data on repository so it will be available upon reasonable request from the corresponding author [S.A].
FUNDING
This study is funded by Pan African University (PAU), life and earth science institute (including Health and Agriculture). The funding university had no role in the study design, data collection, analysis, preparation of the manuscript and decision to publish.
ACKNOWLEDGEMENTS
The authors would like to thank Pan African University, Life and Earth Science Institute (including Health and Agriculture) for sponsoring this Research work. Our heartfelt thanks also goes to data collectors, the participants and heads of health facilities for their provision of all the necessities for data collection.


