All published articles of this journal are available on ScienceDirect.
Patient Satisfaction in the Primary Care System of Cyprus: A Pilot Study
Abstract
Background
Patient satisfaction serves as a widely acknowledged metric for assessing the quality of care. Understanding the perspectives of care recipients through patient satisfaction is crucial, as it can function as a valuable tool for quality improvement. The assessment of patient satisfaction becomes particularly imperative following significant healthcare reforms.
Methods
This study represents the first attempt to delineate the level of patient satisfaction with the newly introduced Primary Care system in Cyprus. Employing an internationally validated tool for evaluating general practice care, a cross-sectional online survey was conducted within one of the largest group practices in Cyprus Primary Care. An online questionnaire was dispatched to all registered email addresses within the group practice, totaling 5,000 emails. Patient satisfaction was measured based on the percentage of respondents reporting their level of satisfaction on a 5-point Likert scale for the questionnaire items.
Results
The overall satisfaction percentage emerged at 80.51% (SD 32.36). Notably, the majority of questions received excellent ratings. The aspect rated the least satisfactory was the waiting experience in the waiting room, with a mean (SD) of 4.05 (1.08). Conversely, the highest-rated item pertained to safeguarding the records and confidentiality of the patients, with a mean (SD) of 4.65 (0.70).
Conclusion
This survey, the first of its kind since the inception of the new NHS, conducted in one of the largest primary care centers, indicates remarkably high satisfaction rates comparable to those of other developed EU NHSs. However, to achieve a comprehensive national understanding of patient satisfaction and further support quality improvement initiatives, a larger study encompassing more GP practices is warranted. Such an expanded study would not only supplement ongoing quality improvement interventions but also contribute to fostering patient empowerment in the healthcare system.
1. INTRODUCTION
The significance of the role of primary care in influencing population health outcomes has been extensively researched and substantiated [1]. Individuals who visit their General Practitioners (GPs) regularly and rely on them as the primary source of health-related information tend to exhibit better health outcomes. This holds true irrespective of their initial health status and socio-demographic characteristics. Such individuals are not only less prone to hospitalization but also incur lower annual healthcare expenditures [2]. Furthermore, the presence of a robust primary care system within a healthcare framework has demonstrated a positive impact on patient satisfaction [3]. This highlights the integral role played by primary care in not only maintaining and improving individual health but also in fostering a sense of contentment and approval among healthcare recipients. The interplay between frequent GP visits, informed healthcare decisions, and positive health outcomes emphasizes the pivotal role of primary care in shaping the overall health landscape of a population.
Patient satisfaction stands out as a primary catalyst for ensuring quality in healthcare. It serves as a pivotal metric for evaluating healthcare services and even acts as a predictor for health outcomes. Within the healthcare system, the primary care setting holds particular significance, as interactions with providers within this domain can elicit varied perceptions of care quality and satisfaction.
Since the 1990s, following Donabedian's declaration of quality, there has been a paradigm shift in the assessment of healthcare quality, incorporating patient perceptions into the evaluation process. In recent years, healthcare systems have increasingly embraced approaches from other industries, notably borrowing from the retail market. Patient satisfaction surveys, initially introduced as tools for quality improvement, have gained prominence, mirroring successful practices seen in other sectors. This evolution underscores the commitment of the healthcare sector to adopting innovative strategies and technologies to enhance the quality of care provided to patients.
Historically, most European countries have adopted patient satisfaction as a quality improvement tool. Some examples are as follows: In 1996, the evaluation of patient satisfaction was mandated for all French hospitals [4]. In Germany, measuring satisfaction has been required since 2005 as an element of quality management reports [5]. In England’s NHS, since 2002, the Department of Health (DOH) has launched a national survey program in which all NHS trusts have to survey patient satisfaction on an annual basis and report the results to their regulators [6]. Many other countries have adopted the use of patient satisfaction as a quality improvement tool, indicating that patient satisfaction is a legitimate indicator for improving the services and strategic goals of all healthcare organizations [6, 7].
The literature indicates a number of tools that evaluate primary care. Amongst others are the WHO Primary Care Assessment Tool (PCET), the Primary Care Assessment Survey (PCAS), the Primary Care Assessment Tool (PCAT), the Components of Primary Care Index (CPCI), and the EUROPEP, which measures experiences, views, or satisfaction of patients with GPs [8].
These instruments serve the purpose of assessing primary care comprehensively, encompassing various facets, such as financing, service delivery, and patient satisfaction. While some of these instruments are explicitly designed for the evaluation of patient satisfaction, others incorporate diverse aspects that can be indirectly associated with patient satisfaction but are not exclusively tailored for this purpose. The inclusiveness of these instruments reflects a holistic approach to evaluating primary care, recognizing the multifaceted nature of healthcare quality and the importance of patient perspectives.
The EUROPEP is a validated tool that is widely used for the study of patient satisfaction by measuring their own opinion. It asks patients to assess their GP, which they have visited over the previous 12 months [9]. The tool has been validated and used in about 20 countries and has been translated into 15 languages [9-15]. Using such a widely used tool is of paramount importance in Cyprus, which has undergone a major healthcare reform over the recent years especially in light of the pandemic crisis in Cyprus.
The first mention of a health system in Cyprus was made in 1957, and this was a state-funded health system based on the Beveridge principles. It underwent minor reforms until a major one in 1980, where the provision of care was based on income criteria [16]. This reform has led to what was existing until 2019. Cyprus underwent a major healthcare system reformation in 2019, which implemented a universal healthcare system for all its citizens. The new NHS is a Bismark type of health system and has been implemented in two phases. The first phase of the NHS has been implemented since 1st June 2019. This phase only dealt with outpatient health services. These services include personal doctors for adults and children, outpatient specialists, pharmacies and pharmaceuticals, and medical laboratories. This phase aimed to strengthen primary care with the implementation of the Personal Doctor (PD). In other words, the first phase was the establishment of primary care [17]. The PDs ensure continuous and comprehensive healthcare provision. PDs provide primary care with an emphasis on prevention, navigate the beneficiaries in the system and help reduce unnecessary visits to specialised doctors. They are considered the backbone of the system. PDs in the latest COVID-19 pandemic were at the forefront, and they were the ones that “triage” patients as suspected cases and subsequently referred them for a lab test or took care of them at home via telemedicine.
It is also worth noting that all of the officially recorded population have registered as beneficiaries of the new system. At the beginning, there was a time window for beneficiaries to register to a PD of their choice, but after the deadline, those who did not register were automatically registered to PDs with the least registered beneficiaries. Beneficiaries have the right to change their preferred PD at predefined time intervals or if they are not satisfied with the level of care they are provided with. Beneficiaries have access to contracted providers, as well as public and private entities. Importantly, due to the high numbers of specialized paediatricians and obstetrics and gynaecologists (Obs & Gyn) and the lack of trained GPs, the new system provides primary care services via three distinct specialties; GP service for over 15 yrs old population via PDs, paediatricians for below 18, and Obs and Gyn for all female beneficiaries.
In Cyprus, no study to assess patient satisfaction has been performed since the major healthcare reformation of 2019, which implemented a universal health system and established primary care officially for the first time. Even prior to the establishment of the new National Health System (NHS), there were no such studies, given that primary care mostly operated on a private basis, making it challenging to capture data on patients visiting General Practitioners (GPs). Consequently, Cyprus did not participate in the European primary care comparison, creating a notable gap in knowledge that needed addressing [9]. Recognizing this gap, our study was initiated to assess, for the first time, the satisfaction levels of users of primary care services in Cyprus. The absence of previous studies, coupled with the unique context of the major healthcare reform, underscored the importance of investigating patient satisfaction in this specific healthcare landscape.
Considering the ongoing challenges posed by the COVID-19 pandemic, we conducted a special online survey using the Greek version of the EUROPEP tool. This survey aimed to evaluate patient satisfaction with the primary care services provided through general practice. Importantly, this study represents the first instance in Cyprus where the Greek version of the questionnaire has been utilized after the major healthcare reform, contributing valuable insights into patient satisfaction within the evolving healthcare system.
2. MATERIALS AND METHODS
The research incorporated data from the Apostolos Loukas Medical Centre, one of the largest primary care facilities in Cyprus, catering to both urban and semi-rural populations in our locality. In 2020, the medical center initiated a local quality improvement effort, utilizing the Greek version of the EUROPEP tool. The center, which comprises five GPs, 15 specialist physicians, healthcare administrators, and nurses, aims to enhance the quality of its primary care services.
To ensure the focus on primary care patient satisfaction, the study exclusively included beneficiaries registered on the lists of the GPs within the center. The number of beneficiaries on these lists ranged from 1,000 to 2,500, adhering to the maximum limit stipulated by the Health Insurance Organisation (HIO), the overseeing body of the new Cyprus universal NHS. The GPs involved in the study were aged from 35 to 47, with professional experience spanning 10 to 20 years.
As part of their commitment to continuous quality improvement, registered beneficiaries were invited to express their opinions on the services provided by GPs, thereby reflecting on the quality of primary care and the overall Medical Center. To adapt to the constraints imposed by the pandemic, the survey questionnaire was transitioned to an online platform. The distribution of questionnaires was conducted through emails and the newsletter of the center, with a total of 5,000 emails sent to registered beneficiaries, fostering a comprehensive and inclusive approach to gathering feedback on primary care services.
2.1. EUROPEP Tool
EUROPEP is a multidimensional tool that consists of 23 items concerning five aspects of care: relation and communication, medical care, information and support, continuity and cooperation, facilities, availability, and accessibility. The tool asks the beneficiaries to assess their primary care doctor, taking into account experiences over the last 12 months [10]. The Greek version of EUROPEP was used to survey patient satisfaction with regards to GPs and the primary care centre. The Greek version of the tool was developed and validated by the Clinic of Social and Family Medicine of the University of Crete [13, 18]. The translated version uses the original five-point Likert scale (1=bad=very dissatisfied, 5=excellent=very satisfied) for the 23 items describing patient satisfaction. It should also be noted that there is a Not Applicable (N/A) option available. Additional emphasis on patient satisfaction is provided by two more items; “I strongly recommend the GP to family and friends” and “I have no reason to change my GP” (five-point response scale: 1=strongly disagree to 5=strongly agree). The tool also collects sociodemographic characteristics, such as gender, age, educational level as well as the number of times patients consulted their GP during the last year.
2.2. Statistical Analyses
Data cleaning was performed before data analyses. If participants responded that they had no consultation with their doctor in the preceding year, then that response was omitted from the analysis as the questionnaires clearly stated that they must have had contact with their doctor in the last 12 months. In addition, responses with more than 12 being “not applicable” were excluded from the analysis.
Items were assessed for mean (SD), median (IQR), and floor and ceiling effects. Cronbach’s alpha was used to assess the internal consistency reliability of the questionnaire.
In order to be considered a satisfied patient, we summed those who responded ≥4 per question. A total satisfaction percentage was calculated using the formula below.
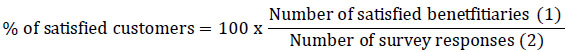
1. The number of satisfied beneficiaries are those who responded with excellent (5) or very good (4)
2. The number of survey responses are the sum of all responses, excluding the “Not applicable”
Potential associations and overall satisfaction were assessed by demographic characteristics collected through the tool, and the appropriate statistical test was used (Mann Whitney, Kruskal-Wallis H test, mean (SD) median (IQR) and χ2). All analyses were performed using STATA 14.1.
3. RESULTS
A total of 501 questionnaires were completed and successfully submitted online. Of those submitted, none had any missing data. Of those 501 responses, 33 answered that they had no contact with their GP in the last 12 months and, therefore, were excluded. The remaining 468 responses underwent a comprehensive analysis, resulting in a response rate of 9.38%. It is important to acknowledge the inherent limitation in assessing the exact reach of the survey, as the emails might have potentially been directed to spam folders and remained unread. Despite this uncertainty, considering a 50% population proportion, our sample provided a 95% confidence level, suggesting that the actual satisfaction value falls within ±4.31% of the measured satisfaction value. This statistical approach helps provide a reliable estimate of the satisfaction levels within the studied population despite potential limitations in email reach and response rate.
3.1. Participant Characteristics
Table 1 shows the participant characteristics. The age of the participants ranged between 18-84, with a mean (SD) age of the responders 45.14 (12.53). The majority of the responders were female 58.97%. The majority of the participants had graduated from tertiary education (79.71%). The vast majority of participants evaluated their state of health as good or very good (77.78%), 17.95% evaluated their health as excellent, and only 4.27% evaluated their health as poor or fairly good. Around one-third of the participants (31.82%) stated that they have a chronic condition. Also, the majority of the patients (52.76%) had two consultations with their doctor in the last 12 months.
3.2. Patient Satisfaction
The participants' satisfaction scores (mean (SD), median (IQR) floor and ceiling effects) for the 23 items are shown in Table 2. All items with the exception of item 22, had a ceiling effect larger than 50% (range: 50.6%-66.3%). All items had a skewed distribution towards ‘excellent’. The reliability of the tool was very high (Cronbach’s alpha 0.98). The overall % satisfaction of all beneficiaries was 80.51% (SD 32.36).
| Beneficiary Characteristic | ||
|---|---|---|
| Age | Mean | 45.14 |
| SD | 12.53 | |
| - | No (%) of patients | |
| Gender | Female | 276 (58.97) |
| Male | 192 (41.03) | |
| Academic education | Primary/ Secondary | 95 (20.29) |
| Tertiary | 373 (79.71) | |
| Self-reported health status | Excellent | 84 (17.95) |
| Very good/good | 364 (77.78) | |
| Fair/poor | 20 (4.27) | |
| Chronic disease | Yes | 148 (31.82) |
| No | 320 (68.38) | |
| Visits to the doctor over the last 12 months | 1 | 106 (22.65) |
| 2 | 169 (36.11) | |
| 3-5 | 170 (36.33) | |
| 6-12 | 23 (4.91) | |
| Question | Mean(SD) | Median(IQR) | “Not Relevant” (%) | Floor(%) | Ceiling (%) |
|---|---|---|---|---|---|
| Making you feel you had time during consultations? | 4.40 (1.01) | 5 (1) | 1.28 | 2.81 | 66.45 |
| Interest in your personal situation? | 4.48 (0.94) | 5 (1) | 1.28 | 2.38 | 69.48 |
| Making it easy for you to tell him or her about your problems? | 4.46 (0.93) | 5 (1) | 1.07 | 2.16 | 68.03 |
| Involving you in decisions about your medical care? | 4.44 (0.90) | 5 (1) | 2.78 | 1.32 | 65.27 |
| Listening to you? | 4.53 (0.92) | 5 (1) | 1.50 | 1.52 | 71.19 |
| Keeping your records and data confidential? | 4.65 (0.70) | 5 (0) | 8.97 | 0.23 | 77.70 |
| Quick relief of your symptoms? | 4.47 (0.89) | 5 (1) | 3.42 | 1.33 | 66.59 |
| Helping you feel well so that you can perform your normal daily activities? | 4.53 (0.84) | 5 (1) | 3.85 | 0.67 | 70.67 |
| Thoroughness? | 4.56 (0.89) | 5 (0) | 1.28 | 1.30 | 75.11 |
| Physical examination of you? | 4.44 (0.94) | 5 (1) | 6.41 | 1.83 | 66.44 |
| Offering you services for preventing diseases? | 4.51 (0.89) | 5 (1) | 4.27 | 1.56 | 71.21 |
| Explaining the purpose of tests and treatments? | 4.51 (0.92) | 5 (1) | 2.99 | 2.20 | 71.81 |
| Telling you what you wanted to know about your symptoms and/or illness? | 4.52 (0.86) | 5 (1) | 1.50 | 0.65 | 70.28 |
| Help in dealing with emotional problems related to your health status? | 4.40 (0.98) | 5 (1) | 12.61 | 1.71 | 65.77 |
| Helping you understand the importance of following his or her advice? | 4.47 (0.90) | 5 (1) | 3.21 | 1.55 | 68.43 |
| Knowing what she/he had done or told you during previous contacts? | 4.42 (1.00) | 5 (1) | 4.27 | 3.13 | 67.86 |
| Preparing you for what to expect from specialist or hospital care? | 4.40 (0.97) | 5 (1) | 13.25 | 2.46 | 65.02 |
| The helpfulness of the staff (other than the doctor)? | 4.45 (0.85) | 5 (1) | 3.21 | 0.66 | 64.68 |
| Getting an appointment to suit you? | 4.36 (0.95) | 5 (1) | 1.28 | 1.73 | 61.47 |
| Getting through to the practice on the phone? | 4.37 (0.95) | 5 (1) | 1.28 | 1.30 | 62.77 |
| Being able to speak to the GP on the telephone? | 4.25 (1.06) | 5 (1) | 1.50 | 3.04 | 57.92 |
| Waiting time in the waiting room? | 4.05 (1.08) | 5 (2) | 2.14 | 3.93 | 43.67 |
| Providing quick services for urgent health problems? | 4.39 (0.92) | 5 (1) | 7.69 | 0.93 | 62.50 |
The lowest mean (SD) score was for the item “Waiting time in the waiting room?” (4.05(1.08)), with the second lowest being “Being able to speak to the GP on the telephone” with a mean(SD) 4.25 (1.06). The highest mean (SD) satisfaction was for the item “Keeping your records and data confidential?” (4.65 (0.70)). There was a heavy skewness towards positive evaluations; the ceiling effects ranged from 43.67% to 77.70%, while floor effects were all less than 4%.
Further analysis of the % satisfaction was performed for the sociodemographic measures collected. A Mann-Whitney test was performed to assess differences in median % satisfaction between genders. The results indicated no statistically significant difference between the two (p-value=0.1323). The same test was used to assess the differences between satisfaction and whether the beneficiary has a chronic disease. Again, the results indicated no statistically significant difference (p value=0.9612). A Kruskal-Wallis H test was performed to determine if % satisfaction was associated with different age groups. This test indicated no statistically significant difference in the satisfaction % between the six groups, χ2 (5)=1.226 p-value=0.9424. The same was true for education χ2 (2)=1.955 p-value=0.3763, the number of GP visits χ2 (3)=5.400 p-value=0.1448, and the health status χ2 (2)=1.494 p-value=0.4738.
4. DISCUSSION
The results of this study identified good satisfaction with the care provided by the GPs and the medical centre. Overall, patients expressed strong satisfaction across all aspects of care, with a notable emphasis on their contentment regarding data confidentiality. However, the areas where patients expressed the least satisfaction were related to the ability to contact their GP by phone and the waiting time during scheduled appointments. It is evident that these concerns are not directly associated with the quality of medical care received but rather with the availability and accessibility of services.
It is crucial to underscore the significance of these findings, as the ability to contact a GP and the waiting time for appointments are integral components of healthcare accessibility and availability. While patient satisfaction was high in general, addressing these specific concerns is imperative to uphold the pillars of quality care. These aspects contribute significantly to the overall patient experience and should not be overlooked in efforts to continually enhance the quality and accessibility of healthcare services.
The primary strength of this study lies in its pioneering nature, being the first of its kind conducted after the significant healthcare system reform in Cyprus. Benefiting from a representative sample obtained from the largest group practice primary care center in Cyprus, the results indicate a notably high level of satisfaction among participants. This study serves as a valuable benchmark, offering insights into patient satisfaction post-reformation.
The management of the center, demonstrating a proactive approach, is actively engaged in identifying areas for improvement. The findings have been swiftly incorporated into the decision-making process, leading to the initiation of targeted actions. This responsiveness not only highlights the commitment of the center to continuous enhancement but also underscores the practical application of research outcomes for tangible improvements in the delivery of primary care services.
Further, the assessment tool needs to be updated as it has traditionally been filled by patients with the help of a researcher at the GP practice. After the pandemic, patient visits decreased, and close interaction between people became strictly prohibited, especially in medical centres. Therefore, we opted for electronic dissemination, which may have decreased our response rate. Our data were heavily skewed towards beneficiaries with tertiary education backgrounds; therefore, there may be some probability of bias in our findings. But this may also be a true representation of the population as Cyprus has the second highest tertiary education % in Europe [19]. Also, the questionnaire asks for patient visits. With the advancement of IT, the current pandemic, the excess demand for service, and the limited time resources, other forms of consultation have increased, such as telephone and video consultations [20, 21].
Patient satisfaction, while not precisely defined, is widely acknowledged as a crucial quality indicator that gauges the success of healthcare services. In our study, we employed an internationally validated patient satisfaction tool to comprehensively assess patient satisfaction in primary care in Cyprus. This marks the first attempt to gauge patient satisfaction after the significant healthcare reform of 2019.
The overall patient satisfaction observed in our study aligns well with the results from a previous study conducted in Cyprus in 2010, specifically examining diabetic and hypertensive patients. This consistency across studies suggests a certain stability in patient satisfaction levels over time, emphasizing the enduring importance of this metric in evaluating the effectiveness and quality of healthcare services [22]. Overall, our study findings are consistent with other international findings of the studies that used the EUROPEP tool [11-15]. Aligning with these global findings, our study highlights that patients express high levels of satisfaction, particularly in the domain of safeguarding confidentiality. However, akin to patterns observed in other studies, the aspect with the lowest satisfaction is typically the waiting time before a consultation with the General Practitioner (GP).
This recurrent trend emphasizes a shared challenge across various healthcare systems worldwide and underscores the importance of addressing waiting times as a critical aspect of enhancing patient satisfaction. Recognizing and targeting this specific concern can contribute significantly to overall improvements in the quality of primary care services.
The original work of the EUROPEP tool categorises primary care into five distinct categories: availability and accessibility, information and support, medical and technical care, doctor-patient relationship, and organization of services [10]. Although internal reliability was very high, we were not able to identify any scales using the data we collected. This inability to identify the five distinct categories may reflect the need for additional indicators based on single items or new refined scales. In addition, this is an aspect that many of the studies analyzing EUROPEPR have identified.
4.1. Limitations
This study identified a “methodological problem” of the large ceiling effects [23], which other international EUROPEP studies have also reported. We found a skewed distribution towards the “excellent” option; therefore, there was a large ceiling effect and a very small floor effect. The high ceiling effect was potentially an indication of the lower responsiveness of the questionnaire. These ceiling effects were not higher than those of other comparable studies [11-15], but it should be noted that there is a great variation in the criteria used to evaluate ceiling and floor effects.
Another limitation of the study is the generalizability of the findings. Although the sample size was good enough to make accurate estimates, it was a single-centre study in our location. Although the healthcare practice serves beneficiaries from both urban and rural areas, the universal electronic health record does not provide the opportunity to extract data to understand the case of the beneficiaries registered with the practice; therefore, we cannot be sure of the generalisability of the findings. In addition, we had a relatively low response rate, which is usually the case in such studies, and this increases the risk of bias. Unfortunately, due to the lack of specific registries and a proper electronic patient record system, it was not possible to compare the characteristics of responders with non-responders. Also, this may be the reason why we did not spot any sociodemographic differences in satisfaction while they exist in the international literature.
CONCLUSION
The findings of this study underscore the potential utility of the Greek EUROPEP tool as a valuable quality assessment and improvement instrument in Cyprus. The implications extend beyond the management of the medical center, reaching national and international health policy leaders. Further, the active participation of patients in shaping health policy is crucial, emphasizing the importance of patient engagement in service assessment and empowering patients to advocate for the acknowledgment of their health needs.
The study has already informed the managers of the medical center, leading to prompt actions to address identified issues. Measures such as increased administrative and IT support aim to enhance communication between beneficiaries and GPs, while improved appointment management seeks to reduce waiting times. The COVID-19 pandemic prompted the cancellation of physical appointments, prompting alternative solutions like emails, live chat, and texting, which have proven to be effective.
The Health Insurance Organisation (HIO) should leverage the findings of this study as a foundation for a nationwide assessment of patient satisfaction across Primary Care. Such an initiative, conducted regularly, could serve as a crucial tool for targeted quality improvement interventions, ensuring transparency and promoting patient empowerment. Given the role of primary care as the gatekeeper in the national health system, variations in patient satisfaction may signal differences in care quality and potential health inequalities. Hence, annual assessments can help maintain a proactive approach to addressing these concerns.
Beyond national implications, a large-scale study employing the EUROPEP tool could provide baseline data for international comparisons. When used as a tool for GP evaluation and quality improvement, patient satisfaction offers valuable insights into good practices and areas requiring enhancement. Therefore, adopting similar approaches on a universal scale within the new National Health System (NHS) can systematically assess Primary Care, addressing quality issues without exacerbating health inequalities.
AUTHORS’ CONTRIBUTION
GS and NS conceived the idea for the study. NS and AS gathered all the data. NS analysed all data and wrote the original manuscript with the assistance from AS and GS. All authors commented on the manuscript.
LIST OF ABBREVIATIONS
| GPs | = General Practitioners |
| PCET | = Primary Care Assessment Tool |
| PCAs | = Primary Care Assessment Survey |
| PCAT | = Primary Care Assessment Tool |
| CPCI | = Components of Primary Care Index |
| PD | = Personal Doctor |
| COVID-19 | = Coronavirus Disease |
| HIO | = Health Insurance Organisation |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Our study received approval from the Cyprus National Bioethics Committee (ΕΕΒΚ ΕΠ 2020 01 156).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.


