All published articles of this journal are available on ScienceDirect.
Herbal Medicine Use among Adult Lebanese Patients with Chronic Diseases: A Descriptive Cross-sectional Study
Abstract
Introduction
Herbal products are used for the management of various chronic diseases. This study sought to determine the frequency of herbal medicines use among Lebanese patients diagnosed with chronic diseases, their patterns, underlying causes and perceived efficacy.
Methods
This is a descriptive cross-sectional study that enrolled Lebanese adult patients from the six governorates of Lebanon between February and December 2020. Those who had hypertension, diabetes mellitus, dyslipidemia, chronic constipation, or rheumatoid arthritis were eligible for enrollment.
Results
A total of 300 patients participated in this study. Around 123 participants (41%) reported using herbs. The majority purchased the herbs based on a suggestion (47.2%) from a friend or a family member. The most commonly used herbs were Pimpinella anisum, and Garlic (15.8%) for hypertension, Sage (26.9%) and Stevia (23.1%) for diabetes mellitus, Red Yeast Rice (27%) and Hawthorn (23%) for dyslipidemia, and Senna (43.6%) and Artichoke (25.8%) for chronic constipation, and Curcumin (46.2%) and Allium sativum (30.8%) for rheumatoid arthritis. The majority did not have an idea about the side effects (87.8%), drug-herbal interactions (95.1%), or drug-disease interactions (96.8%) of herbs. Most of the patients (65%) were satisfied with the herbal product use.
Conclusion
The use of herbal medicines is common among adult Lebanese patients diagnosed with hypertension, diabetes, dyslipidemia, arthritis, and constipation. However, herbal products are not risk-free. Hence, further research in this area is warranted.
1. INTRODUCTION
Naturally occurring substances derived from plants, known as herbal medicines, undergo minimal or no industrial processing and are valued for their fragrance, taste, or therapeutic qualities [1]. They represent a popular choice in complementary and alternative medicine [2]. The global consumption of herbal products has risen significantly, addressing various health concerns [3]. Approximately 38% of Americans employ herbal medicines, while in Arab societies, around 80% of the population depends on them for preventing and treating illnesses [4, 5]. In Egypt, 37% of the populace acknowledges using herbal medicines, and in Saudi Arabia, 73% of individuals have reported using herbal products [6, 7]. A Lebanese national study found that 29.87% of the population engages in complementary and alternative medicine, with “folk herbs” being the most prevalent, utilized by 75% of respondents [8].
The primary reasons for the widespread use of herbal products include their application in preventing diseases and managing various conditions, such as dyslipidemia, hypertension, diabetes, constipation, and rheumatoid arthritis, among others [9]. The increasing popularity of herbal medicines can be attributed to several factors, including dissatisfaction with conventional treatments [10], their cost-effectiveness compared to traditional medical care, alignment with patient beliefs, accessibility of health information, and the placebo effect [11, 12].
In contrast to conventional medications, herbal medicines are not required to meet premarketing safety and efficacy standards [13]. Despite the perception of herbal products as harmless, they can lead to a range of side effects, from mild to severe, and may also result in drug or disease interactions [14]. Improper use, inaccurate content, and variations in the quality, purity, strength, or composition of herbal products can contribute to health problems.
With the rising usage of herbal medicines, the incidence of adverse effects and interactions with conventional drugs increases as well [15]. Therefore, it is crucial to conduct studies on the frequency and characteristics of herbal product use, particularly among adult patients with chronic diseases. This is essential for promoting public awareness, addressing health risks associated with herbal use, and establishing stringent governmental policies to ensure consumer safety and uphold product quality [16]. A study in Lebanon focusing on the regulation of complementary and alternative products found that existing frameworks do not adequately ensure public safety or support the integration of these products into the healthcare system [17].
While Lebanon has a rich history of incorporating herbal medicine [18], there is limited information on the prevalence of herbal medicine usage in the context of chronic diseases. Consequently, this research aimed to assess the frequency of herbal medicine utilization among Lebanese adults diagnosed with conditions, such as hypertension, diabetes mellitus, dyslipidemia, chronic constipation, and rheumatoid arthritis. Additionally, the study sought to characterize the patterns, root causes, and perceived effectiveness of herbal products in this population.
2. METHODS
2.1. Study Design and Setting
This is a quantitative descriptive cross-sectional study that enrolled a sample of 300 Lebanese adult patients drawn from the six governorates of Lebanon (Beirut, South, North, Beqaa, Nabatieh, and Mount Lebanon) between February and December 2020. Due to the limitations of conducting face-to-face interviews during the COVID-19 pandemic, the developed questionnaire was distributed online to Lebanese adults. Invitations to participate in the survey were sent by the investigators via social networking platforms, such as WhatsApp, Facebook, and Instagram. The sample was collected using a snowball-sampling technique where participants were encouraged to pass on the questionnaire link to their acquaintances.
2.2. Ethical Considerations
The study was approved by the Ethical and Research Committee at the Lebanese International University under the number 2020ERC-121-LIUSOP. The Helsinki Declaration was followed for involving human subjects in the study, though the study posed no harm to the participants. The participation of members of the Lebanese public was strictly voluntary. Informed consents of the patients were obtained prior to study inclusion, where the participants had to agree to participate in the study before survey access. The anonymity of respondents was preserved in the study, as the names of the participants were not included.
2.3. Eligibility Criteria
The inclusion criteria of this study were set to include Lebanese patients who were at least 18 years of age, currently living in Lebanon, and willing to participate in the study. Patients who had any of the following diseases: diabetes mellitus, hypertension, dyslipidemia, chronic constipation, rheumatoid arthritis, and were able to fill out the survey online, were eligible for enrollment. Excluded were those who did not fit the inclusion criteria or refused to complete the questionnaire.
2.4. Data Collection and Measures
Data collection was carried out using a questionnaire that was developed by the researchers based on questions extracted from previous studies [19, 20]. Opinions of experts, including a sample of the target group and two faculty members, were sought to assess the questionnaire for appropriateness, complexity, attractiveness, and relevance for the items. The items were edited and reworded based on their statements. The survey questionnaire was self-reported and administered in Arabic. Before use, the questionnaire was translated into Arabic (a process involving two independent translations, synthesis of the two translations, back translations, review of the pre-final version, and pretesting). The survey was created via Google Forms and shared through online platforms to collect data from participants. The questionnaire contained close-ended questions. All participants filled out the survey online using the link that was shared with them. The questionnaire was divided into two sections. The first part was dedicated to collecting the socio-demographic data, which included questions regarding age, gender, region of residence, educational level, employment, monthly income, medical diseases, and check-ups. The second section retrieved information regarding herbal products use, reasons for using or not using herbs, the most commonly used herbs in chronic diseases (Hypertension, diabetes mellitus, dyslipidemia, chronic constipation, and rheumatoid arthritis), frequency of use, dosage form of the herbal product, reported side effects, reported interactions, patients' satisfaction and expectations, and counseling about herbs.
3. RESULTS
3.1. Socio-demographic Characteristics
A total of 300 patients were recruited in this study. Males (56.3%) and females (43.7%) were almost equally distributed, with the majority of participants aged between 41 and 60 years (56%). Most of the patients were employed (65.3%) with low income (66.7%). Three-quarters of the participants (75%) reported conventional medication use. The enrolled patients reported having diagnosed hypertension (29.4%), diabetes mellitus (22.3%), dyslipidemia (19.7%), chronic constipation (18.3%), and rheumatoid arthritis (10.3%). The majority (60%) had medical check-ups every 1 to 2 years. The socio-demographic characteristics of the participants are illustrated in Table 1.
3.2. Herbal Products Use
Around 123 participants (41%) reported using herbs or herbal products to treat their disease states, while 59% denied any herbal use. Among those using herbs, 29 patients (31.7%) were consuming them to manage hypertension, 26 patients (21.1%) for diabetes mellitus, 26 patients (21.1%) for dyslipidemia, 39 patients (31.7%) for chronic constipation, and 13 patients (10.6%) for rheumatoid arthritis. The majority purchased the herbs based on a suggestion (47.2%) from a friend or a family member, followed by disappointment with conventional therapy (23.6%), Family traditions (17%), and social media (10.6%). Fig. (1) demonstrates the several reasons why the participants consumed herbs. On the other hand, among those who did not use herbs, the most revealed reasons for not consuming herbs or herbal products included not believing in them (25.4%), not being prescribed by a physician (29.4%), or not needing them (16.4%). Fig. (2) illustrates the reasons reported by the participants for not using herbs.
| Variable | N (%) |
|---|---|
|
Gender Male Female |
169 (56.3%) 131 (43.7%) |
|
Age 18-40 years 41-60 years 61-80 years >80 years |
78 (26%) 168 (56%) 37 (12.3%) 17 (5.7%) |
|
Location Beirut South Lebanon Bekaa Mount Lebanon North Lebanon Akkar |
49 (16.3%) 78 (26%) 36 (12%) 52 (17.3%) 43 (14.3%) 42 (14%) |
|
Employment Employed Unemployed |
196 (65.3%) 104 (34.7%) |
|
Average Monthly Income Low Low-moderate Moderate-high High |
196 (66.7%) 66 (22.4%) 31 (10.5%) 1 (3%) |
|
Educational Level Primary High school University |
184 (61.3%) 59 (19.7%) 57 (19%) |
|
Conventional Medication use Yes No |
225(75%) 75 (25%) |
|
Disease State Hypertension Diabetes mellitus Dyslipidemia Chronic constipation Rheumatoid arthritis |
88 (29.4%) 67 (22.3%) 59 (19.7%) 55 (18.3%) 31 (10.3%) |
|
Medical Check-ups Frequency Every 3-6 months Every 6-12 months Every 1-2 years >5 years |
14 (4.7%) 84 (28%) 180 (60%) 22 (7.3%) |
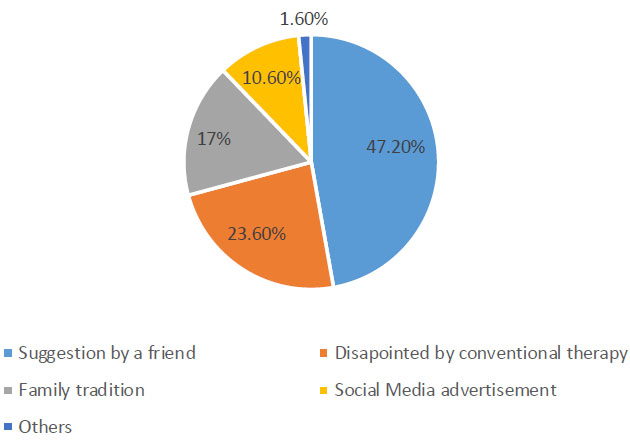
Reasons for using herbs or herbal products.
3.3. Most Commonly Used Herbs
For hypertension, the participants reported mostly the consumption of Pimpinella anisum, Matricaria aurae, and Garlic (15.8%). Sage (26.9%), Stevia (23.1%), and Ginseng (19.2%) were the herbs most reported by the patients for managing diabetes mellitus. The participants revealed mainly the use of Red Yeast Rice (27%) and Hawthorn (23%) for the treatment of dyslipidemia. For the management of chronic constipation, Senna (43.6%) and Artichoke (25.8%) were the most utilized herbs. As for rheumatoid arthritis, the most commonly used herbs included Curcumin (46.2%) and Allium sativum (30.8%). Table 2 demonstrates the herbs utilized by the participants for the management of different chronic diseases.
| Disease | Herb | N (%) |
|---|---|---|
| Hypertension | Pimpinella anisum | 6 (15.8%) |
| Matricaria aurae | 6 (15.8%) | |
| Garlic | 6 (15.8%) | |
| Zingiber officinale | 5 (12.8%) | |
| Hawthorn | 3 (7.9%) | |
| Foeniculum vulgare | 3 (7.9%) | |
| Fenugreek | 2 (5.3%) | |
| Apium celery | 2 (5.3%) | |
| Diabetes Mellitus | Sage | 7 (26.9%) |
| Stevia | 6 (23.1) | |
| Ginseng | 5 (19.2%) | |
| Robas root | 3 (11.5%) | |
| Moringa | 2 (7.7%) | |
| Dyslipidemia | Red yeast rice | 7 (27%) |
| Hawthorn | 6 (23%) | |
| Green tea | 4 (15.7%) | |
| Celery | 3 (11.5%) | |
| Curcumin | 3 (11.5%) | |
| Matricaria aura | 1 (4%) | |
| Berberine | 1 (4%) | |
| Basil | 1 (4%) | |
| Chronic constipation | Senna | 17 (43.6%) |
| Artichoke | 10 (25.8%) | |
| Peppermint oil | 5 (13%) | |
| Aloe vera | 4 (10.3%) | |
| Fenugreek | 2 (5.2%) | |
| Rheumatoid arthritis | Curcumin | 6 (46.2%) |
| Allium sativum | 4 (30.8%) | |
| Ginger | 2 (15.4%) | |
| Eucalyptus | 1 (7.7%) |
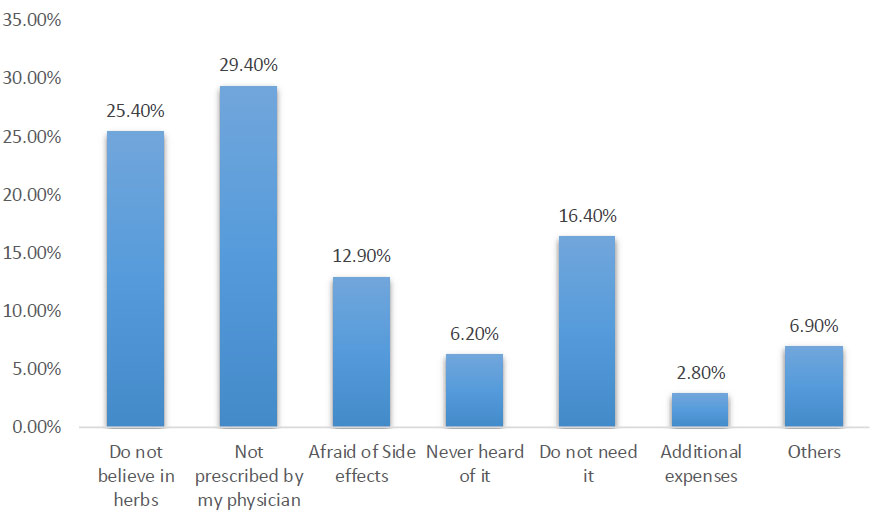
Causes for avoiding herbs or herbal products.
3.4. Administration of Herbs
Most of the patients reported either irregular use (37.4%) or daily use (38.2%) of herbs or herbal products. Only 17.1% had their herbs prescribed by a health care provider (physician or pharmacist). The participants mostly reported consuming the plant as a whole (53.7%), followed by pharmaceutical formulations, such as tablets or capsules (28.5%). Table 3 illustrates the administration of herbs among the participants.
| Variable | N (%) |
|---|---|
|
Frequency Irregularly Daily >once/week Weekly |
46 (37.4%) 47 (38.2%) 26 (21.1%) 4 (3.3%) |
|
Prescribed by Pharmacists Physicians Family tradition Books Neighbours Social media |
14 (11.4%) 7 (5.7%) 23 (18.7%) 14 (11.4%) 46 (37.4%) 19 (15.4%) |
|
Dosage Form Tablet/capsule from pharmacy Herbal mix from pharmacy Distilled extract Plant as a whole |
35 (28.5%) 6 (4.9%) 16 (13%) 66 (53.7%) |
| Variable | N (%) |
|---|---|
|
Have you asked a physician or a pharmacist about the herb/s before use? Yes No |
42 (34.1%) 81 (65.9%) |
|
Do you have any idea if the herb/s you utilize can induce side effects? Yes No |
15 (12.2%) 108 (87.8%) |
|
Have you suffered from side effects caused by herbs? Yes No Undecided |
7 (5.7%) 112 (91.1%) 4 (3.3%) |
|
Do you have any idea if the herb/s you utilize can interact with medications? Yes No |
6 (4.9%) 117 (95.1%) |
|
Do you have any idea if the herb/s you utilize can interact with diseases? Yes No |
4 (5.2%) 119 (96.8%) |
|
Have you suffered from any drug-herb interaction? Yes No Undecided |
4 (3.3%) 117 (95.1%) 2 (1.6%) |
|
Would you use the herb again knowing it can cause side effects and interactions? Yes No Undecided |
10 (8.2) 110 (89.4%) 3 (2.4%) |
3.5. Side Effects and Interactions
Only 34.1% of the participants consulted a healthcare provider prior to herbal use. The majority did not have an idea about the side effects (87.8%), drug-herbal interactions (95.1%), or drug-disease interactions (96.8%) they might suffer due to the consumption of herbs or herbal products. Only 5.7% reported having side effects induced by herbs ranging from mild to severe abdominal cramps to hypoglycemia and insomnia. A minority of 3.3% revealed suffering from a drug-herbal interaction. Around 90% of the patients would not use herbs or herbal products again, knowing they can cause side effects or interactions. The views of participants toward herbal side effects and interactions are shown in Table 4.
3.6. Satisfaction and Expectations
Most of the patients (65%) were satisfied with the herbal products used, with around 33% being moderately satisfied. The majority (74%) would recommend the herb (s) they are consuming to other patients. The participants mainly expected the herbal products to prevent the progression of the disease (32.5%) or improve their health status (20.3%). Table 5 illustrates participants' satisfaction and expectations with herbal product use.
3.7. Sources of Herbs or Herbal Products: Pharmacist vs. Herbalist
The majority of the participants (69.1%) reported purchasing their herbs from the herbalist, while the remaining 38 patients (30.9%) purchased them from a pharmacy. The participants were counselled by the pharmacist regarding the herbal product dose and frequency of use (100%), side effects (84.4%), and interactions (65.8%). Only 54% of the patients were counselled for dose and frequency, 11.8% for side effects, and 2.4% for interactions by the herbalist. Fig. (3) shows the difference in counselling about herbs between the pharmacist and the attar.
| Variable | N (%) |
|---|---|
| Level of satisfaction with the herb/herbal product Not satisfied Moderately satisfied Satisfied Very satisfied |
2 (1.6%) 41 (33.3%) 71 (57.7%) 9 (7.3%) |
| Do you recommend the herb you used to another patient? Yes No Undecided |
91 (74%) 10 (8.1%) 22 (17.9%) |
| What expectations did you have when using the herb/herbal products? No expectations Prevent the progression of the disease Complete cure of the disease Enhance the effect of conventional therapy Better health status Others |
25 (20.4%) 40 (32.5%) 16 (13%) 11 (8.9%) 25 (20.3%) 6 (4.9%) |
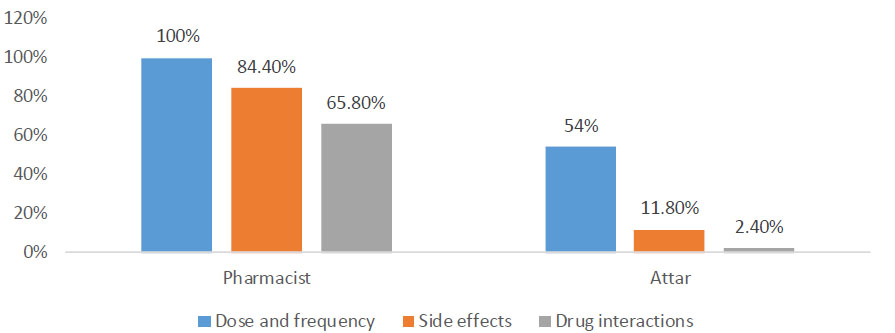
Counseling about herbal products by the pharmacist and the attar.
4. DISCUSSION
Despite advancements in the pharmaceutical industry, herbs continue to be frequently utilized in the management of various diseases either independently or as a complementary therapy to conventional pharma- ceuticals [11]. The utilization of herbal medicines, especially in the treatment of chronic conditions, raises concerns regarding their safe and effective use [21].
Recent global studies, including those in Lebanon, support the widespread and increasing use of herbal medicine [3, 5, 8]. More than one-third of the participants in this study reported using herbal medicine for treating chronic diseases. Similar trends were observed in a Turkish study, where around one-third of participants used herbal medicines for managing chronic conditions, such as hypertension, diabetes, and hyperlipidemia [21]. Studies from Thailand, Jordan, and Saudi Arabia also reported a notable prevalence of herbal medicine use among patients with chronic diseases [16, 22, 23].
The reasons for herbal medicine use in this study were diverse, with family and friends or media acting as primary sources of information, aligning with findings from previous research [24, 25]. The study identified various reasons for not using herbs, including a lack of belief in their efficacy or a perceived lack of need. Similar findings were reported in a Jordanian study, highlighting the importance of disseminating information and conducting outreach and education about herbal products.
The most commonly used herbs in this study varied based on the chronic condition, with Pimpinella anisum and Garlic for hypertension, Sage and Stevia for diabetes mellitus, Red Yeast Rice and Hawthorn for dyslipidemia, Senna and Artichoke for constipation, and Curcumin and Allium sativum for rheumatoid arthritis. The choice of herbs was influenced by heritage and availability, with around 250 plant species still in use in Arab traditional medicine [8].
The study revealed that a majority of participants used herbs either irregularly or daily, with concerns raised about the lack of regulated dosing. Professional healthcare providers, primarily physicians or pharmacists, were the main sources of herbal product recommendations. However, the study highlighted that many participants were unaware of potential side effects, drug-herb interactions, or drug-disease interactions associated with herbal product consumption.
Despite these potential risks, the majority of participants expressed satisfaction with herbal product use and indicated a willingness to recommend herbs to others. The study emphasized the role of pharmacists in providing appropriate counseling on herbal product dosage, frequency of use, side effects, and interactions.
While the study contributes valuable insights into herbal medicine use among patients with chronic diseases in Lebanon, it has limitations, including its local nature, limited sample size, and the subjective nature of self-reported data. The descriptive study design also precludes establishing cause-effect relationships, and the choice and wording of questions may have influenced participant responses [26-31].
CONCLUSION
This study revealed that the use of herbal medicines is common among adult Lebanese patients, specifically among patients with hypertension, diabetes, dyslipidemia, arthritis, and constipation. Family and friends or media were the main sources of information regarding herbal medicines. Further, a vast majority of medicinal plant species are still in use for the treatment of various chronic diseases with satisfactory results. However, it is worth knowing that herbal products are not risk-free, and the risk of drug interactions is not currently well studied. This is especially important since herbal medicines are recommended by professional health care providers. Hence, further research in this area is warranted, and healthcare professionals should suggest caution to patients where appropriate.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Ethical and Research Committee at the Lebanese International University under the number 2020ERC-121-LIUSOP.
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study. The Helsinki Declaration was followed for involving human subjects in the study, though the study posed no harm to the participants.
CONSENT FOR PUBLICATION
Informed consents of the patients were obtained prior to study inclusion, where the participants had to agree to participate in the study before survey access.


