All published articles of this journal are available on ScienceDirect.
Assessment of University Students’ Knowledge, Attitude and Practice Regarding Breast Self-Examination in Bahrain: A Call for Action
Abstract
Background
Breast cancer has become a significant global health concern in recent years, calling for action and intense methods of prevention and early identification.
Aim
To assess the Knowledge, Attitude, and Practice (KAP) regarding Breast Self-Examination (BSE) among university female students.
Methods
A cross-sectional descriptive study was conducted at the University of Bahrain (UoB). A convenience sampling of 375 female students voluntarily completed the questionnaires.
Results
The students’ total percent scores in the three domains were less than 70% (63.25±10.60 for knowledge, 64.47±12.55 for Attitude, 56.03±18.27 for practices). The majority of students had unsatisfactory BSE practices (82.9%), and poor knowledge about BSE (69.6%). However, 28.5% of students had positive attitudes toward BSE.
Conclusion
The results indicate a significant gap in KAP related to BSE among university female students. The knowledge deficiency reflects finite awareness and understanding of the importance of BSE and using proper techniques. At the same time, the limited attitude might hinder students’ engagement and motivation in practicing BSE. Therefore, targeted educational initiatives and community engagement campaigns are essential to improve women’s awareness regarding BSE and enhance personal motivation toward the proper practice of BSE. Disseminating the appropriate practice of BSE in the community is also recommended.
1. INTRODUCTION
Breast Cancer (BC) is a disease in which cancerous cells develop in the breast tissue, primarily in the milk ducts or lobules. It is unclear exactly what causes breast cancer. However, several risk factors have been identified that enhance the likelihood of having the disease. These risk factors include gender, age over 50, history of breast cancer in the family, lifestyle factors, and hormonal factors such as prolonged estrogen exposure [1].
The World Health Organization (WHO, 2020) reports that breast cancer (BC) is the most common type of cancer worldwide, affecting 2.3 million women and responsible for 685,000 deaths in 2020. In addition, 7.8 million women who were diagnosed with BC within the previous five years were still alive as of the end of 2020. In the Kingdom of Bahrain, BC is the most prevalent type of cancer, representing 37.9% of females with cancer [2]. The significance of BC, indeed, is linked to the anatomical location close to important organs including the heart, lungs, and esophagus. So, early detection and management are essential to prevent the risk of metastases to surrounding tissues and organs, allowing for more effective treatment, and preserving the overall health and well-being of the patient [3].
Although it is not possible to eliminate the risk of BC, several measures can help reduce the likelihood of developing the disease [4]. Preventing BC involves a combination of lifestyle modifications, proactive health care practices, and risk-reduction strategies [5]. Adopting a healthy lifestyle can contribute to overall well-being and reduce the risk of BC. This involves eating a balanced diet, exercising frequently, and keeping a healthy weight, in addition to limiting alcohol consumption and quitting smoking. Evidence suggests that breastfeeding may have a protective effect against BC [6]. Long-term use of Hormonal Replacement Therapy (HRT) for menopausal symptoms has been linked to a higher risk of developing BC. Discussing the potential risks and benefits with a healthcare provider and exploring alternative treatments, if appropriate, is essential. Women also can reduce exposure to environmental factors associated with an increased risk of BC, such as radiation and certain chemicals. This may involve taking necessary precautions in occupational settings and avoiding unnecessary radiation exposure [7].
Under the umbrella of early detection, women can adopt many strategies to notice any changes that could happen in their breasts. These methods involve a variety of approaches, such as mammography, genetic counselling, testing, breast self-examination (BSE), and clinical breast examinations (CBE).
Regular breast self-examination can help in the early detection of the disease and lower its prevalence [8]. The BSE is a crucial preventive practice that empowers individuals to detect early signs of abnormalities, including lumps or changes in breast tissue. Evidence suggests that women who properly conduct the BSE once a month are more likely to notice a lump early which is reflected in the early treatment and a better prognosis [9]. Regular and appropriate BSE assists individuals to be familiarised with their bodies and potentially identify any potential abnormalities that may require further medical attention. However, despite the benefits of practicing regularly, still many women are non-compliant in performing BSE and many do not even know the appropriate approach to performing it [10]. While BSE is a crucial component of breast health awareness, women still have a limited awareness of breast self-examination [8]. For that, university students' knowledge, practice and attitude towards BSE have garnered increasing attention recently [4]. Research indicates that when women are instructed by doctors or nurses, they are more likely to conduct BSE properly [10]. Nurses play an important part in the primary, secondary, and tertiary levels of prevention. Nurses take part in creating awareness of risk factors, educating the community about the importance of performing regular BSE, participating in screening programs, and finally, offering essential supportive care, and emotional support, coordinating rehabilitative services and improving the overall quality of life of the affected women [11].
University students represent a diverse and dynamic population often undergoing significant lifestyle changes as they transition into adulthood. This period of personal growth and development provides a unique opportunity to cultivate health-conscious behaviors and attitudes, including adopting regular breast self-examination practices [12]. However, various factors influence university students' knowledge, attitude, and practice (KAP) of breast self-examination, such as education, cultural beliefs, social norms, and access to healthcare information [6].
Recognizing university students' current KAP towards BSE holds immense importance for healthcare pro- fessionals, educators, and policymakers. It allows for identifying potential knowledge gaps, misconceptions, and barriers that may hinder the adoption of breast self-examination practices [7]. There is scarce and limited knowledge available on breast self-examination among Bahraini university students. In order to create educational interventions that are effective, it is necessary to comprehend the extent of their knowledge about the significance of early detection, appropriate self-examination practices, and understanding of breast cancer risk factors is essential.
So, assessing university students' KAP for breast self-examination is essential for advancing breast health awareness for early diagnosis and treatment. Empowering university students with accurate information and cultivating a proactive approach toward breast health will not only benefit their well-being but also contribute to the larger goal of reducing BC morbidity and mortality. Little data is known about the knowledge, attitude and practice of female university students in the Kingdom of Bahrain regarding BSE. Understanding the challenges and factors that influence female university students in practicing BSE is necessary for empowering female university students to maintain healthy practices. So, the aim of this study was to evaluate female university students' knowledge, attitudes, and practices of BSE.
2. METHODS
2.1. Design and Settings
A cross-sectional descriptive study was conducted at the University of Bahrain (UoB).
2.2. Participants
Participants included a convenience sampling of 375 female students enrolled in any undergraduate program of the University of Bahrain in the first semester of the academic year 2023-2024 and did not receive any professional educational program about breast self-examination. After excluding students who did not meet the inclusion criteria, The Epi Info program version 10 was used to estimate the sample size using the following parameters: a population size of 16735, a confidence coefficient of 95%, an expected frequency of 50%, and an acceptable error of 5%. The minimum sample size was 375 students.
2.3. Measurements Tool
2.3.1. Knowledge, Attitudes, and Practice (KAP) of Breast Self-examination Questionnaire
The KAP was developed by Rosmawati (2010) to evaluate the KAP of BSE among women in a suburban area in Terengganu, Malaysia. The questionnaire consists of 35 items divided into three subscales: knowledge (15 items), attitude (13 items), and practice (7 items). For knowledge subscales, participants answered 15 closed-ended questions scored as follows: True scored two, did not know scored one, and false scored Zero. To measure the attitude towards BSE, the participants rated their responses on a 5-point Likert scale from strongly disagree (0) to strongly agree (4). The questions of practice were answered on a 5-point Likert scale: never (0), seldom (1), neutral (2), frequently (3), and always (4). The scores of the negative items were reversed. The total scores for the subscales were summed up, and the percentage score was determined by dividing the obtained scores by the maximum score of each subscale (30 points for knowledge, 52 points for attitude, and 28 points for practice). According to Doshi et al. (2012), a 70% cut-off point was used to categorize the participant's responses of knowledge (poor- good), attitude (Positive – negative), and practice (satisfactory – unsatisfactory). The questionnaire is reliable (α = 0.80) [12].
2.4. Data Collection Procedure
The pilot study was conducted by administering the questionnaire among thirty university students to assess the clarity of the instructions and questions. Samples who participated in completing the questionnaire were excluded from the final sample for the main study to avoid any potential bias or influence on the results.
To make the data collection process more streamlined, the researchers transformed the questionnaires into electronic formats. This allowed them to share a link with female students at UoB, making it convenient for participants to access and complete the questionnaires online. The electronic form began with a clear explanation of the study's aims and objectives, providing participants with a comprehensive understanding of the purpose of the research. Following this, an online consent form was presented, ensuring that participants had the opportunity to give their informed consent before proceeding.
Once participants agreed to take part voluntarily in the study, they were able to proceed with completing the questionnaires. Notably, each participant was restricted to providing only one response to maintain data integrity and prevent duplicate entries.
2.5. Ethical Consideration
Approval was obtained from the Ethical Research Committee at the College of Health and Sport Sciences and the University of Bahrain (CHSS SRPC No: 18/2023-24). To ensure ethical considerations were met, the study complied with The Declaration of Helsinki 7th revision.
2.6. Statistical Analysis
Data analysis was conducted using the SPSS version 23. Descriptions were used to describe students’ KAP of BSE. After testing the obtained data for normality, the Kolmogorov–Smirnov test was not significant which indicated a normal distribution of the KAP of BSE. Hence, Pearson’s Correlation Coefficient was employed to assess the relationship between students' age, family history of BC, and their KAP towards BSE. Statistical significance was determined using a threshold of P < 0.05.
3. RESULTS
Table 1 shows that 62.40% of the participants were less than 20 years and 31.47% were in their first year of study. Results showed that most of the students had no family history of BC (90.93%).
Students’ knowledge about the BSE is displayed in Table 2. Results indicated that the majority of the students reported that they knew the importance of observing the breasts for any unusual change in shape and size (1.88±0.401), using finger pulps for examining any thickening or lumps of the skin (1.87±0.41), using the circular strip vertical BSE technique (1.78±0.50), pressed on the nipple to check for any unusual discharge (1.79±0.52), inspected their breast by using mirror (1.66±0.681). However, most of the students were confused about the timing of the BSE (0.47±0.74), the early signs, and some steps of the BSE techniques, such as raising the two hands simultaneously while inspecting the breast (0.55±0.78) and using different views (0.70±0.85).
Table 3 shows female students’ attitudes toward BSE. The average attitude score was 33.52±6.52 out of 52. Results demonstrated that most of the students agreed that women should do BSE (3.65±0.76), that they care about their breasts (3.27±1.001) and discuss BSE with their friends (2.29±1.331). However, some of them reported that doing BSE is unpleasant (2.63±1.25), embarrassing (2.42±1.34), and wasting time)3.17±1.32).
| Items | No. | % | |
|---|---|---|---|
| Age (years) | < 20 | 234 | 62.40 |
| 20 - 21 | 96 | 25.60 | |
| 22 - 23 | 35 | 9.33 | |
| 24- 25 | 10 | 2.67 | |
| Year of Study (level) | First | 118 | 31.47 |
| Second | 79 | 21.07 | |
| Third | 71 | 18.93 | |
| Fourth | 107 | 28.53 | |
| Family History of BC | No | 341 | 90.93 |
| Yes | 34 | 9.07 | |
| Item | Mean ± SD |
|---|---|
| 1. BSE should be done every two months | 1.02±0.91* |
| 2. BSE must be done between day 7 and day 10 after menses | 0.47±0.74* |
| 3. BSE should be done in front of the mirror | 1.66±0.68 |
| 4. Undress until the waist when doing the BSE | 1.59±0.68 |
| 5. Hands should be raised up alternately above the head when doing the BSE in front of the mirror | 0.55±0.78* |
| 6. BSE should be done from the front view only | 0.70±0.85* |
| 7. BSE can be done in a supine position | 1.14±0.88 |
| 8. Palpate in the right breast while left-sided lying when doing the BSE | 1.26±0.78 |
| 9. Use finger pulps to examine any lumps or thickening of the skin | 1.87±0.41 |
| 10. BSE can be done using the vertical strip and circular technique | 1.78±0.50 |
| 11. Need to press on the nipple to check any unusual discharge | 1.79±0.52 |
| 12. BSE includes arm-pit examination to check for any lump | 1.42±0.79 |
| 13. Need to observe any unusual change in the shape and size of breast | 1.88±0.40 |
| 14. Retraction of the nipple is a warning sign that should be observed | 1.47±0.64 |
| 15. Lump is the early sign for cancer | 1.64±0.70 |
| Total knowledge score | 18.98±3.18 |
| Item | Mean ± SD |
|---|---|
| 1. Doing BSE makes me feel so funny | 2.45±1.25* |
| 2. BSE will be embarrassing to me | 2.42±1.34* |
| 3. Doing BSE is wasting time | 3.17±1.32* |
| 4. Doing BSE makes me feel unpleasant | 2.63±1.25* |
| 5. If there is a lump, I prefer to get treatment from a traditional healer | 1.86±1.27* |
| 6. Feel uncomfortable, cannot do BSE once a month | 1.61±1.25 |
| 7. All women should do BSE | 3.65±0.76 |
| 8. I really care about my breasts | 3.27±1.00 |
| 9. I am not afraid to think about the breast cancer | 2.45±1.41 |
| 10. Avoid BSE because I worry about having breast cancer | 2.30±1.28* |
| 11. Interested in doing BSE | 2.91±1.00 |
| 12. Always search for information regarding BSE on the internet, magazines, and newspaper | 2.50±1.21 |
| 13. Discuss with my friends about BSE | 2.29±1.33 |
| Total attitude score | 33.52±6.52 |
| Item | Mean± SD |
|---|---|
| 1. Do BSE once a month | 1.49±1.23 |
| 2. Avoid learning the correct method of BSE | 2.05±1.22* |
| 3. Parents or partners always advise to do BSE | 1.95±1.30 |
| 4. Advise friends to do BSE | 2.18±1.36 |
| 5. Discuss the importance of BSE with friends | 1.79±1.33 |
| 6. Have been taught on BSE by health staff | 2.37±1.40 |
| 7. If you notice any breast abnormality, directly go to public health care | 2.86±1.12 |
| Total practice score | 15.69±5.12 |

The students' practice of BSE is discussed in Table 4. The overall mean score was 15.69±5.12 out of 28. The mean score of the students who reported doing BSE monthly (1.49±1.23) or discussing the BSE importance with their friends (1.79±1.33). Besides, few students reported that their parents or partners always advised them to do BSE (1.95±1.30).
Fig. (1) reveals that the average of students' total percent scores in the three domains were less than 70% (63.25±10.60 for knowledge, 64.47±12.55 for Attitude, 56.03±18.27 for practices).
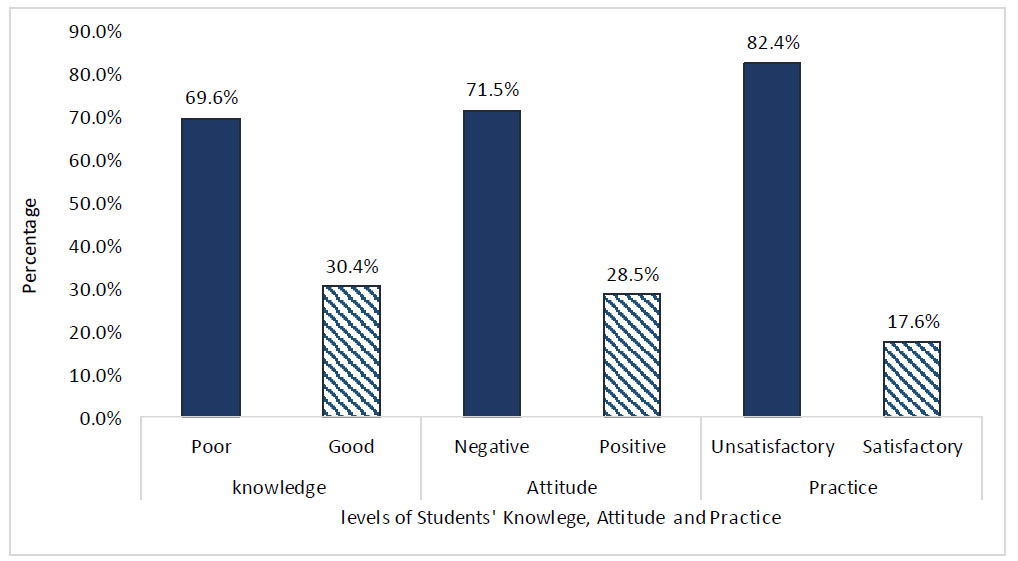
Fig. (2) illustrates that 69.6% of students indicated the student’s further need for better knowledge regarding BSE, and 82.4% of them had unsatisfactory BSE practices. Further, only 28.5% of the students had a positive attitude toward BSE.
Table 5 displays a significant positive correlation between the students’ practice of BSE and their knowledge and attitude (r= -0.167, p= 0.001, and r= 0.482, p<0.001, respectively). The matrix also showed a significant positive correlation between students' age and their practice of BSE (r= .126, p= .015).
| Items | - | knowledge | Attitude | Practice |
|---|---|---|---|---|
| Attitude | r | -0.091 | - | - |
| p | 0.078 | - | - | |
| Practice | r | 0.167** | 0.482*** | 1 |
| p | 0.001 | <0.001 | ---- | |
| Age | r | -0.064 | 0.035 | 0.126* |
| p | 0.220 | 0.501 | 0.015 | |
| Year of Study | r | -0.096 | 0.044 | 0.065 |
| p | 0.062 | 0.398 | 0.211 |
4. DISCUSSION
Breast cancer has increasingly been acknowledged as a growing health concern owing to its high incidence rate across the globe. The startling rise in the incidence of BC cases warrants more investigation of this health problem at multiple levels [13]. In this venue, our study findings have shown considerable updates to the data concerning the KAP of BSE among UoB students.
The existing findings exhibited a poor knowledge level of BSE among students. This result is congruent with many studies conducted in the region, such as the one reported by Albeshan et al., 2023 [14] who claimed that female students enrolled in Saudi universities demons- trated an inadequate knowledge about BSEs and Ghrayeb et al., 2018 who concluded that female undergraduate students at Al-Quds University in Palestine had unsatisfactory knowledge about BSE [15]. At the international level, for example in Cameroon, results showed that female students have reported insufficient overall knowledge related to BSE [16]. A plausible reason for our existing findings may hinge on the participants' age, coupled with most of them not having a family history of BC, which may be attributed to their inadequate knowledge of BSE. Typically, this age bracket of university life is only sometimes eager to seek health information about medical illnesses around them, including BC and BSE [17]. It is especially important that half of the participants are less than 20 years old, and one-third of them are first-year students who may never have heard about BSE. Gedefaw et al. (2020) highlighted that the students' acknowledgment of health literacy issues becomes more apparent as their year of study progresses, prompting them to seek BSE-related information [18]. In this case, BSE should not be unfamiliar to this cohort, which must monitor changes in their breasts. The American Cancer Society suggests that women should be informed and sensitized about the importance of BSE, commencing at the age of 20 [19]. This enterprise calls for urgent actions by the responsible authorities to conduct health educational programs geared toward fostering awareness of BSE in university milieus.
Emerging scientific evidence recommends that the correct time to perform a monthly BSE is 3 to 5 days after the menstruation period starts [2, 20]. Roughly, most of the students are confused about the timing of the BSE, as exemplified by the findings of this study. The respondents displayed that BSE must be done between days 7 and 10 after menses. Contrarily, findings from a Pakistan’s study indicated that only one-third of the females stated that BSE should be performed a week after menstruation [21], which is comparable with an Ethiopian study reported that a third of the female university students declared that the best time to do BSE was two to three days after the menstruation [22]. Moreover, a study done in Eritrea reported that only 14% of female college students knew the appropriate time for performing BSE 2-3 days following menstruation [23]. This discrepancy across the studies might be due to the inconsistencies in the probable source of information regarding BSE that might exist between the geographical and study population differences. The present study was campus-based, while that of African studies was conducted on tertiary education among females who came from diverse cultural, ethnic, and geographic zones across the country. Though beyond the benefits of BSE, a particular concern for prioritizing reliable resources about the correct time women rely on for BSE is warranted [21]. Nonetheless, interpretative caution is hinted, as we did not assess the possible sources of the acquired knowledge related to BSE.
Interestingly, among the respondents of the present study, only more than one-quarter of them endorsed a positive attitude toward BSE. Referring to our findings, the university students recorded that doing BSE is unpleasant, wastes time, and is embarrassing. Similar testimonials from Saudi Arabia concurred with our study’s findings, where more than one-third of females demonstrated a positive attitude toward BSE [24]. This may be an indication that the discussion of specific topics related to the female body, like breasts, is still deeply rooted in shame across the Gulf and Middle Eastern countries [25]. Opposite outcomes were documented by Alomair et al. (2020), who recorded that 64.01% of female students demonstrated a positive attitude toward BSE. In addition, Ahmed et al. (2018) surveyed 1000 female university students and found that most respondents had positive attitudes toward BSE. The authors added that the observed positive attitude signals that they are more inclined to BSE but have yet to receive sufficient knowledge and motivation to perform it [21].
Furthermore, most of the study participants demonstrated an unsatisfactory BSE practice level, with the minority performing BSE monthly. This was not indeed different from previous studies; among Palestinian undergraduate students, only 4.1% reported practicing BSE in the last month, and 62.9% never did so [26]. Additionally, a study of undergraduate students at Ajman University revealed that while 22.7% of the participants practiced BSE, only 3 percent did so in the last month [27].
A multicentre study involving 10,810 undergraduate students from 25 universities across Asia, Africa, and America revealed that 59.3% had never performed BSE [28]. Given that most of the participants do not have a family history of BC, their age and unfamiliarity with BSE may be contributing factors to our current findings.
In contrast, a previous study conducted in Nigeria revealed that 58.51% of community women had good BSE practice, with 11.9% performing it within the last month and 39.4% within two months [29]. In addition, Florence et al. estimated that 85–90% of nursing students at the Institute of Benin perform self-breast examinations every month [30]. The disparity in the results can be attributed to a substantial discrepancy in the knowledge level demonstrated by these studies, in addition to the inconsistent study population. Lack of knowledge, along with the inconsistent source of information, was one of the most frequently reported obstacles to BSE [14]. Similar to the present study, Rosmawati et al. reported a highly statistically significant correlation between overall knowledge and practice of BSE (P = 0.00) [31].
Considering our findings, a small percentage of participants discuss BSE with peers, and their parents do not encourage them to do so. These imply a need for more women's motivational support from parents, family, and community and emphasize one of the most significant challenges to implementing BSE, which is the Arab-specific cultural barriers. Most health behaviors are learned via experience and modified by the influence of culture. Cultural barriers, discomfort over self-examination, and touching one's body were the most significant barriers to not practicing BSE in a previous study [32].
Without questioning cultural stereotypes and how they are reinforced in society, it would be challenging to enable women to overcome obstacles to receive BCS services. Understanding how women define breasts, not only in terms of health but also in terms of their functions and identity, is crucial for successful BSE implementation [32]. Moreover, women’s conceptualization of health as the absence of pain/disease, as well as cancer phobia, are another potential barrier to BSE. This indicates that the women's attitude and beliefs dramatically affect their practice, as shown in the current study, the positive correlation between the attitude towards BSE and practice, and other previous studies as well [31].
5. LIMITATIONS
This was a cross-sectional descriptive study design that does not support causal inferences, which limits the ability to determine cause-and-effect relationships. Using of non-probabilistic method of selection of the population would limit the generalizability of our findings. Future research will overcome these limitations by using more representative sampling methods and increasing sample size to enhance the external validity of the study. However, the data of this study was collected at a specific time, lasting the month of October, during National BC Awareness Month. The facet would provide a credible, updated picture of the existing outcome.
CONCLUSION
The results indicate a significant gap in KAP related to BSE among university students. Knowledge deficiency suggests a need for more awareness and understanding of the importance and proper techniques of BSE, while the limited positive attitude could hinder their engagement and motivation in practicing BSE. In this case, there is a notable lack of regular BSE practice among students, with many not performing BSE monthly as recommended, pointing towards a critical area for intervention to improve practice rates. The facet that warrants the need for targeted educational initiatives and sensitization campaigns to improve awareness regarding BSE ought to be endorsed to address this issue. In addition, the incorporation of BSE knowledge and practice as a part of the university student's curriculum is also of utmost importance in a bid to raise awareness. Equally important, a substantial effort should be intensified to use mass media to increase BC awareness and inculcate knowledge regarding the best time to do BSE. Exploring the impact of cultural beliefs on females’ attitudes towards breast self-examination could provide valuable insight for developing culturally sensitive interventions to address this knowledge gap.
LIST OF ABBREVIATIONS
| KAP | = Knowledge, Attitude, and Practice |
| BSE | = Breast Self-Examination |
| UoB | = University of Bahrain |
| BC | = Breast Cancer |
| BSE | = Breast Self-examination |
| CBE | = Clinical Breast Examinations |
ETHICAL STATEMENT
Approval was obtained from the Ethical Research Committee at the College of Health and Sport Sciences and the University of Bahrain (CHSS SRPC No: 18/2023-24).
To ensure ethical considerations were met, the study complied with The Declaration of Helsinki 7th revision.


